From this article you will learn:
- why do acne appear on the chin, forehead or cheeks,
- reasons for their development in women,
- the most effective remedies for acne on the face,
- use of phototherapy (IPL) and laser.
The article was written by a specialist with higher medical education.
Pimples on the face are inflammatory formations on the skin, which are a consequence of the formation of acne (open and closed comedones) in the hair follicles and their subsequent infection. There are 2 types of acne - the so-called “papules” and “pustules”. Papules look like inflamed bumps on the skin, but they do not contain pus inside. Pustules are classic pimples in which a blister of pus has already formed.
Papules can be independent formations and, persisting for up to 2 months, can then disappear without a trace. However, most often papules turn into pustules. In general, the term “acne” is a colloquial expression, and it is correct to call this disease papulopustular acne. This form is usually preceded by the comedonal form of acne, which is nothing more than acne. The formation of blackheads (sebaceous plugs) in the hair follicles is a necessary basis for the subsequent formation of acne.
Types of acne on the face in teenagers (papules) -
Pimples in the form of pustules -
Pustules and papules are superficial inflammatory elements. Pustules go through their full development cycle in an average of 10-12 days, and after they disappear, a bright hyperpigmented spot remains in their place. As we said above, papules can persist from 10 days to 2 months, and they can either turn into pustules or disappear without a trace (or rather, weakly pigmented spots remain in their place). You probably already realized that it is useless to squeeze out papules, and this can only lead to increased inflammation and suppuration.
Getting rid of acne on your face if you have mild acne (moderate amount of superficial inflammatory elements) is not very difficult. However, in a number of patients, deep inflammatory elements can also form - these include the so-called indurative, abscessing, phlegmonous, draining, and conglobate acne. After the disappearance of such inflammatory elements, superficial or deep atrophic scars remain in their place, less often keloid scars.
The most common location of acne is if we talk about the face, then most often acne appears on the forehead, as well as acne on the chin. No less common localization are pimples on the cheeks or in the area of the ears. Some patients may experience acne on the scalp (in the scalp), as well as in the back and shoulders. This localization is due to the fact that it is in these areas that the skin contains the maximum number of sebaceous glands - about 400 to 800 per 1 cm2.
Acne on the face in teenagers: causes
We have already said above that it all starts with the comedonal form of acne, i.e. since the appearance of acne. The main reason for the formation of acne in adolescence is an increase in the production of androgens during puberty (puberty). The main androgen in girls is androstenedione, and in boys it is testosterone. Puberty for girls begins at approximately 12-13 years of age, for boys at 14-15 years of age. It is during this period that approximately 85% of adolescents experience the first manifestations of the comedonal form of acne (acne).
Let us remember that the main elements of acne are comedones (white or blackheads), which are non-inflammatory formations. In the middle and late teenage period, against the background of comedones, inflammatory elements (papules and pustules) already begin to predominate, which will indicate the transformation of the comedonal form of acne into the papulopustular form. The course of mild forms of acne usually lasts no more than 4-5 years, but the course of moderate-severe forms can last even 10-12 or more years.
The most striking clinical picture of acne (blackheads and pimples) is observed in girls between the ages of 17 and 18, and in boys between the ages of 19 and 21. It should be noted that girls are less fortunate and are characterized by a longer course of acne, which is also due to the presence of the menstrual cycle. In particular, it is known that in the period from 2 to 7 days after ovulation, acne symptoms intensify in girls. This is due to an increase in the concentration of luteinizing hormone during this period, and the conversion of androstenedione (this is the main androgen secreted by the ovaries) into testosterone.
Important: let's look at how androgens are associated with the appearance of acne and pimples... The fact is that the sebaceous glands have receptors for androgens, and therefore an increased concentration of the latter automatically leads to hyperactivity of the sebaceous glands. As a result, they begin to produce too much sebum, which contributes to the formation of fatty plugs in the lumen of the hair follicles, which are called acne or comedones.
Causes of acne and its types
Pimples don't appear on their own. They indicate any changes and (or) disturbances in the body. The most common causes of acne are:
- too active production of sebum;
- accumulation of dead epidermal cells;
- hereditary factor that provokes a tendency to acne;
- combination of external factors with weakened immunity;
- adolescence, during which hormonal changes occur;
- stressful situations that provoke activation of the adrenal glands;
- skin damage causing inflammation;
- exposure to chlorine;
- disruption of the keratinization process, which can result in the formation of plaques that enlarge the sebaceous glands;
- use of products with barbiturates, lithium, halogens;
- long-term use of hormonal drugs;
- acne, which suggests the presence of a parasitic mite in the glands of the epidermis or in the hair follicles.
Note! It is important to find out the original cause of acne. This will significantly affect the speed of treatment and its outcome. Under no circumstances should you try to squeeze acne, regardless of the reason for its appearance. This may make the situation worse.
When diagnosing, not only the causes of the disease, but also its type are taken into account. Acne is classified according to shape, age and stages of development.
The disease can be expressed in inflammatory and non-inflammatory forms. The first option is characterized by the formation of suppuration.
Inflammatory acne is divided into types:
- conglobate. They appear in the form of spherical rashes. With this type of disease there is always a tendency to form cysts and cavities;
- ordinary. They occur in adolescents, usually appear during puberty, mainly on the face. In most cases, such acne goes away on its own, without third-party intervention or treatment;
- mechanical. Formed as a result of damage to the epidermis;
- lightning fast. Once new growths appear, they fester and spread very quickly. Sometimes they are accompanied by a general deterioration in health and even an increase in body temperature. This occurs due to intoxication.
Non-inflammatory acne is a common rash, blackheads that occur due to blockage of follicles by dead cells or sebum.
According to age, acne is classified as: childhood acne, teenage acne, late acne. And by stages of development: mild acne (up to 10 acne elements), moderate (10-20), severe (20-30), very severe (over 30).
Pimples on the forehead or chin in women: causes
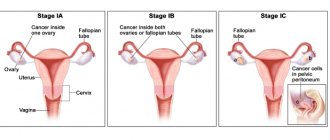
Why do acne form on the chin in women? The reasons here may also be hidden in hormonal background. The fact is that increased concentrations of androgens can occur not only in adolescents. Clinical studies show that 30% of women with acne have laboratory confirmed absolute hyperandrogenism, i.e. increased production of androgens of ovarian or adrenal origin.
Acne in middle-aged women is most often localized in the chin and cheeks; sometimes women also experience acne on the forehead:
We have already said above that in women, in the period from 2 to 7 days after ovulation, current symptoms of acne may arise or intensify. This is due to peak concentrations of luteinizing hormone, which promotes the transformation of androstenedione into testosterone, and the latter, thanks to enzymes, is already converted into dihydrotestosterone. Therefore, taking into account all the above-mentioned causes of acne in women, a remedy for acne on the face, such as oral contraceptives or antiandrogens, can be used as part of complex therapy.
Another cause of acne in women may be the use of oral contraceptives based on pure progesterone. This is due to the fact that sebocytes (these are the cells of the sebaceous glands that produce fatty secretions) have receptors not only for androgens, but also for progesterone. However, the largest group of adult acne patients (both women and men) do not have an increase in androgen production, but they still have overactive sebaceous glands. What this is connected with - read below.
Other causes of acne in adults -
As we said above, the sebaceous glands have receptors for androgens. The fact is that hyperactivity of the sebaceous glands can occur even with normal concentrations of androgens (if these receptors, due to genetics, have increased sensitivity to androgens). The receptors become more sensitive to androgens due to increased activity of the following enzymes: 17-β GSD, 3-β GSD, and 5 α-reductase. The first 2 enzymes convert dehydroepiandrosterone and androstenedione into free testosterone, and 5 α-reductase further converts testosterone into dihydrotestosterone (24stoma.ru).
In general, it is precisely due to the increased activity of these enzymes that in men and women there is an increase in the concentration of dihydrotestosterone (even if the level of androgens is normal). It is dihydrotestosterone that is the main and direct hormonal stimulator of the activity of the sebaceous glands. Studies have shown that in patients with acne and pimples, the synthesis of dihydrotestosterone in the sebaceous glands is increased from 2 to 30 times - compared to patients without acne symptoms. And, by the way, one of the markers of increased activity of these enzymes is the presence of androgenic alopecia in the patient (which occurs not only in men).
The best acne creams
The first category is preventative inexpensive products for acne on the face in the form of creams. In addition to medicinal properties, their additional components promise hydration and softening of the epidermis. They can be used in the initial stages of a rash to prevent relapses. Vyborexperta.ru noted 4 products with high ratings from customers.
Cynovitis
Triple action cream-gel for problem skin from Russian. It has antiseptic, anti-inflammatory and soothing properties. Effective against blackheads.
Active components – bioactive zinc, dipotassium glycyrrhizinate. They fight acne, pimples, and cleanse pores. Sebum production is normalized, skin structure improves. Its irritation and redness are eliminated. The composition does not contain alcohol, salicylic acid, or hormones - the causes of dryness.
Vitamins A and E nourish and saturate the skin. Packaging: 35 ml soft plastic tube with a thin spout for convenient dosing. The texture is dense, viscous, with a slight unobtrusive smell, applied with little effort. The finish is matte.
Advantages:
- Antiseptic, anti-inflammatory components;
- Calming effect;
- Normalization of sebum production;
- Lack of components that cause dryness;
- Mattifying effect;
- Inexpensive.
Flaws:
- Individual intolerance to components;
- Small volume.
The nominee is more suitable for oily and inflamed dermis. Recommended for spot application to problem areas. The effect is noticeable after 14 days if used twice per day. The duration of the course is not limited.
Propeller turbo active cream “SOS”
A domestically produced cosmetic product for emergency control of inflammation on the face within 24 hours. Applied precisely, it reduces acne by drying and reducing irritation.
The active component is cincidone, which affects the causes of inflammation. It controls the production of subcutaneous fat and prevents the development of acne bacteria. Salicylic acid naturally exfoliates, stopping the formation of blemishes. Vitamin E maintains water-lipid balance.
The 50 ml vacuum packaging is maximally protected from bacteria and retains its beneficial properties for a long time. Cream with a snow-white base, rich. When squeezed out, it is dense, but then becomes soft. The smell is cosmetic.
Advantages:
- Emergency help;
- Control of subcutaneous fat production;
- Minimum consumption;
- Hygienic packaging;
- Acceleration of pimple maturation;
- Inexpensive.
Flaws:
- The dispenser requires skill;
- Imperfect composition.
Apply the cream locally to problem areas using beating movements with your fingers. It is recommended to do the procedure before bedtime. Can be repeated throughout the day as needed. If you don't wash it off, the effect will come faster.
Librederm seracin active
Cream-active for oily skin from the Russian brand “Librederm” fights pimples and ulcers in just a few days, suitable for targeted use. Has a powerful antibacterial and anti-inflammatory effect.
Salicylic acid cleanses inflamed pores and soothes. Sulfur and zinc regulate the secretion of the sebaceous glands, reduce redness and discomfort. Allantoin stimulates regeneration processes and opens pores. Xanthan gum retains moisture and forms a protective film.
The 20 ml tube contains a gel-cream consistency with a cosmetic scent. It is absorbed quickly, does not leave a sticky film, and can be applied under daytime makeup. The thin spout saves consumption.
Advantages:
- Pharmacy series;
- Antibacterial components;
- Acceleration of inflammation maturation;
- Drying;
- Convenient packaging;
- Performance.
Flaws:
- Price;
- It dries and irritates healthy skin.
The cream significantly reduces inflammation after 2-3 applications. It can be used not only on the face, but also on the back and décolleté area. It is applied pointwise, so the dermis does not dry out, there will be no peeling or irritation.
Floresan face without problems
Fast-acting cosmetic complex from the Russian brand “Floresan”. It eliminates redness, relieves inflammation, and dries out acne. The antiseptic effect destroys bacteria and blocks the appearance of new acne.
The active component is zinc oxide, which regulates the functioning of the sebaceous glands, it disinfects and has astringent properties. White clay is rich in microelements that contribute to the overall health of the epidermis. Extracts of string and calendula heal abscesses and soothe them.
Plantain extract has a protective effect; it creates a moisturizing and protective barrier. The white cream is packaged in a 50 ml plastic tube with protective foil on the spout. The consistency is thick and takes a long time to absorb. The smell is pleasant.
Advantages:
- Zinc with herbal extracts;
- Quick effect;
- Antiseptic properties;
- Wound healing effect;
- Nice smell;
- Inexpensive.
Flaws:
- Poor absorption;
- Imperfect composition.
Apply the cream to areas of inflammation in the morning and evening, leaving for at least 30 minutes. Residues can be removed with a cotton pad. Reviews confirm a noticeable reduction in abscesses and a gradual elimination of redness.
Key Factors in Acne Formation –
You probably already realized that overproduction of sebaceous gland secretions is one of the main reasons why acne appears on the face. But this factor is far from the only one. This also includes the process of follicular hyperkeratosis, and in addition, the bacteria Propionibacterium acne (P.acne), which live both on the surface of the skin and subsequently in the ducts of the sebaceous glands, are also important.
- Hyperproduction of sebaceous gland secretions – it is caused by increased production of androgens, as well as increased sensitivity of sebaceous gland receptors to androgens. We have already described this process above, but as it turned out, what is important here is not only that there is an increase in the secretion production of the sebaceous glands. A very important point is the change in the chemical composition of the secretion of the sebaceous glands (sebum). In particular, against the background of increased secretion, there is a decrease in the content of linoleic acid in the sebum.
The function of the latter is to regulate the processes of differentiation and desquamation of follicular and epidermal keratinocytes. The stratum corneum of the epidermis of the skin consists of epidermal keratinocytes, and follicular keratinocytes line the lumen of the hair follicle. A decrease in the content of linoleic acid in sebum causes follicular hyperkeratosis, which is one of the most important factors in the development of acne and pimples (we will talk about follicular hyperkeratosis below).Simultaneously with the decrease in the concentration of linoleic acid, the content of unsaturated fatty acids in the sebum increases (from 5 to 20%). Such acids are comedogenic and also contribute to the development of follicular hyperkeratosis and the onset of inflammation. And lastly, an increase in sebum secretion also leads to the fact that follicular keratinocytes begin to release an inflammatory mediator called IL-1α (interleukin-1α). This mediator also promotes follicular hyperkeratosis and the development of inflammation.
- Follicular hyperkeratosis - the lumen of the hair follicle is covered with layers of follicular keratinocytes of varying degrees of differentiation.
When their cell layers are renewed, a constant process of exfoliation of their surface layer occurs. A low concentration of linoleic acid in sebum leads to: 1) hyperproliferation of follicular keratinocytes, i.e. to a sharp increase in the number of their layers and their thickness, 2) to a disruption in the desquamation of keratinocytes into the lumen of the hair follicle. Follicular hyperkeratosis, together with an increase in sebum production, leads to the formation of fatty plugs (comedones) in the lumen of the follicles, obstruction of the follicles and the onset of the inflammatory process. Moreover, at the first stage, inflammation is not associated with a sharp increase in the number of P. acne bacteria in the lumen of the follicle and its damage, but is associated with the production of interleukin-1α by follicular keratinocytes, as well as with an increase in the concentration of free fatty acids. - The presence and activity of the bacteria "P. acnes" - the bacterium Propionibacterium acnes (and to a lesser extent Staphylococcus epidermidis) - are the main microorganisms that are involved in the formation of acne.
These bacteria are representatives of the normal opportunistic skin flora, which is also present on the skin of people without acne symptoms. For a long time, the importance of these bacteria was underestimated; for example, it was believed that they were only responsible for the development of local inflammation in the hair follicle. However, this bacterium also affects the formation of comedones (blackheads) themselves. In particular, the increase in the content of free unsaturated fatty acids in sebum occurs precisely thanks to the enzymes (lipases) of these bacteria. These enzymes break down di- and tri-glycerides contained in the secretions of the sebaceous glands into free fatty acids. And as we said above, free fatty acids are comedogenic and contribute to follicular hyperkeratosis and the development of inflammation. In addition, the listed bacteria secrete enzymes, which subsequently lead to rupture of the walls of the hair follicle - as a result of which the entire contents of the follicle are poured into the surrounding tissue, which leads to a pronounced local inflammatory reaction.
What factors can aggravate the appearance of acne -
- use of comedogenic cosmetics,
- insufficient cleansing of the skin from water- and fat-soluble contaminants,
- medications (prednisolone, steroid hormones, drugs with lithium, anticonvulsants, iodides and bromides),
- active sweating.
Effective methods of dealing with problem skin: advice from a cosmetologist
Acne on the face (acne) can ruin even an ideal appearance. It would seem that in the age of nanotechnology there should be no problems with its treatment, however, millions of people continue to suffer from rashes on the face and body. Acne has different forms, and each of them has its own therapy. The lack of results in the fight against acne in 99 out of 100 cases is due to an incorrectly selected treatment regimen. Daria Sergeevna Bolgova, a dermatovenerologist, cosmetologist, and trichologist at the Face&Body wellness center, talks about the features of acne and how to get rid of it.
Daria Sergeevna Bolgova – dermatovenerologist, cosmetologist, trichologist at the Face&Body wellness club
Daria Sergeevna is a member of the Moscow Society of Dermatovenerologists and Cosmetologists. Participant of the IV and V International training courses for cosmetologists on non-surgical methods of rejuvenation. Member of the Interregional Public Organization of Botulinum Therapy Specialists. Knows everything about the nature of acne and effective methods of treating it.
– Acne is a sore subject for many... Why do they occur and what types are there?
– Let's start with the fact that acne is not a medical term. What we are talking about is called acne, also commonly called acne. This is an inflammatory skin disease, the foci of which are located in the sebaceous glands. Their main function is the production of sebum, which comes to the surface of the skin through the mouth. One of the key factors in the development of the disease is a violation of sebum production, in particular, this concerns its qualitative and quantitative parameters. Depending on the stage of this process, three types of rashes are distinguished:
- Open comedones are the same blackheads that are often talked about in cosmetics advertising. These are nothing more than plugs in the ducts of the sebaceous glands that prevent sebum from coming out. There is no inflammation yet.
- Closed comedones are bumps above the skin with or without blackheads inside. Inflammatory processes can begin in clogged sebaceous ducts - such neoplasms are also called conglobate acne.
- Pustular elements (pustules) are rashes with purulent contents. They appear at the site of inflamed comedones.
The cause of acne is dysfunction of the sebaceous glands
– Do they affect only the face or can they spread to other parts of the body?
– Most often, acne is localized on the face – in the T-zone and on the cheeks. It also appears on the upper back (usually between the shoulder blades) and on the chest. Acne almost never occurs on the stomach, thighs and legs.
– Who suffers from acne more often – women or men?
- There are no differences. Acne occurs equally often in both sexes. It’s just that girls usually perceive it more sharply as an aesthetic problem.
– There is an opinion that acne is characteristic only of teenage skin (there is even a term – juvenile acne), and older people cannot have it. This is true?
– No, adulthood is not insurance against acne. Indeed, acne appears more often in adolescents. It is reliably known that the functioning of the sebaceous glands is influenced by the amount of the hormone testosterone, which begins to be actively produced during puberty, starting at 14–15 years of age. But acne can also occur in adults as a side effect of taking hormonal medications (most often oral contraceptives) and as a symptom of diseases of the endocrine system, when the body’s production of its own hormones is disrupted. Even if your skin was fine in your youth, this does not mean that you will definitely not develop acne in adulthood. Everything is individual.
Acne is not just an appearance problem. To cope with it, it is not enough to remove the rashes themselves. It is important to normalize the amount of testosterone in the body - otherwise the rash will quickly reappear. That is why a good cosmetologist will recommend contacting an endocrinologist and gynecologist. Usually, to get a picture of the pathology, it is enough to take three blood tests - general, biochemical and hormone tests.
– What are the causes of acne and is it possible to somehow prevent it?
– As already mentioned, this problem is of a hormonal nature and is associated with the action of the hormone testosterone. Its excess in the body can be due to heredity (in 90% of cases) or pathologies of internal organs. Acne can occur even if testosterone is normal, but the sebaceous gland receptors are hypersensitive to one of its derivatives, dihydrotestosterone (DHT). The activity of the enzyme 5-α-reductase, which is involved in the synthesis of DHT from testosterone, may also be increased.
External causes of acne include improper selection of cosmetics and skincare procedures. For example, if you have oily skin, you use creams and lotions for dry skin or neglect professional cleansing (if you have hypersecretion of the sebaceous glands, this is definitely necessary).
Another common mistake is using peels with abrasive particles. In the presence of infiltrates (inflammatory elements), they are strictly contraindicated. Abrasive particles open the contents of the rash and spread pathogenic bacteria throughout the face. Therefore, such peelings do more harm than good. For acne, gentle professional gommage peelings without abrasive particles are recommended. They are also called peeling rolls, as they gently roll off the skin, collecting all the excess fat and keratinized scales.
Facial acne treatment at Face&Body. The work of a cosmetologist, dermatovenerologist Daria Sergeevna Bolgova
– Can diet cause acne? After all, they often say: “sprinkled with sweets”...
– Nutrition is a controversial factor. A direct connection between acne and the composition of food consumed has not been established, although some dermatologists do not exclude it. In any case, we can talk about the influence of nutrition on the appearance of acne only if the person himself confirms their relationship. For example, he verified from personal experience that after eating chocolate he developed new rashes. Then, of course, we recommend limiting your consumption of this product.
Daria Sergeevna Bolgova will help cope with various skin problems
– So is it possible to cure acne forever? And how is this happening now?
– It’s possible, but you’ll have to be patient. For grade III and IV acne, when the skin is severely inflamed, drug therapy with isotretinoin-based drugs is prescribed. This is a substance from the group of retinoids (vitamin A derivatives), which regulates the function of the sebaceous glands: reduces the production of sebum and accelerates the exfoliation of dead epidermal cells. The most commonly prescribed drug is Roaccutane - this is an original remedy developed specifically for the treatment of acne. He also has generics (drugs with a similar formula, but from others, etc. They are very effective against acne, but in no case should they be used without a doctor’s prescription. For example, isotretinoin is contraindicated during pregnancy and even during the planning period - it causes fetal deformities.
For acne of degrees I and II, treatment with external preparations containing isotretinoin, antibiotic, zinc, and anti-inflammatory components is recommended. There are enough of them now - there are ointments, creams, gels, and lotions... For stages III and IV acne, the cosmetologist prescribes a combination treatment with Roaccutane and external agents.
Beautiful, clean skin requires high-quality care, but in some cases only a cosmetologist can help.
– How long does drug therapy last?
– I can’t give an exact number in days, but usually at least six months. Isotretinoin has a cumulative effect; it begins to act when a certain amount of it accumulates in the body (measured in mg per kg of body weight). The goal of therapy is to collect this amount from daily doses (12 to 16 mg daily). The dosage is selected strictly individually.
Isotretinoin is a photosensitive substance; when exposed to sunlight, it undergoes undesirable reactions. If burns appear on the skin, the drug will have to be interrupted, and this is unacceptable. Therefore, it is recommended to start treatment after the hot season. The optimal period is from October to May, then you can go on vacation with healthy, clean skin.
Photos “before” and “after” treatment of acne on the back by Face&Body specialist Daria Sergeevna Bolgova
– How can cosmetology help with acne?
– For mild acne, cosmetic procedures accelerate the effect of external therapy. Usually a course of peelings with salicylic acid is prescribed - they perfectly dissolve sebaceous plugs and free the skin of all excess. Hardware therapy also helps. At the Face&Body wellness center there is IPL light treatment using the Italian Deka laser. The effect is based on the antibacterial effect of laser radiation - it destroys acne pathogens and inflammation quickly disappears.
The goal of cosmetic treatment is to remove not only the rashes themselves, but also the traces of them (post-acne). These are stagnant spots of different colors that appear in places of large infiltrates. Injection procedures such as mesotherapy and biorevitalization work well with them. Vitamin cocktails are injected under the skin to improve microcirculation and promote the resorption of stagnant spots. They also contain anti-inflammatory components that prevent new infiltrates from appearing. In the presence of inflammatory elements, mesotherapy and biorevitalization are not prescribed.
Other cosmetic methods of combating post-acne are laser resurfacing (fractional photothermolysis) or a course of acid peelings.
– What recommendations for caring for problem skin will you offer our readers?
– The basic rule is that care should be selected only according to skin type, not based on recommendations from friends, the Internet, etc. The fact is that many people mistakenly determine their skin type: they buy cosmetics for dry skin, but in fact it is oily and dehydrated . In this matter, it is better to trust a cosmetologist. The specialist will select an individual skin care program and recommend specific products. Such a program will necessarily consist of several steps.
First, a two-stage cleansing: remove any remaining makeup with a makeup remover and wash off the sebum with foam or gel cleanser. Next, you need to restore the pH balance - for this we use a tonic. Then comes the turn of nutrition - we apply serum (not oil-based!) and night cream with fruit acids, which dilute sebum and promote its removal. After washing your face in the morning, apply day cream to your skin. Additional care is recommended 1–2 times a week: peeling-gommage and a clay-based mask.
Skin type is the same for life and cannot change, no matter how much we want it. Therefore, any care, no matter whether it is at home or in the salon, should be adjusted to it.
The most effective remedies for acne on the face -
How to remove acne from the face quickly and without complications? The most difficult thing here is to choose the right combination of drugs and draw up a treatment regimen taking into account the specific clinical situation. Below you can see that the approach to treating acne on the face may differ - depending on the predominance of different types of inflammatory elements (papules or pustules), as well as on the severity of the disease. The most effective remedies for acne on the face:
- antibiotics,
- products with benzoyl peroxide,
- topical retinoids,
- oral contraceptives in women,
- phototherapy (IPL), photodynamic therapy and lasers,
- comedones extraction method.
Only a dermatologist or a dermatologist-cosmetologist can professionally treat acne on the face. Unfortunately, in most cases, patients seek consultation with a specialist late, and this leads to complications - the appearance of persistent age spots, as well as superficial atrophic scars. Below you can see a treatment plan for acne, which is based on recommendations from the most famous English-language textbook for dermatologists around the world, Fitzpatrick's Dermatology.
How to get rid of acne on your face (according to Fitzpatrick's Dermatology):
Below we will look at all the types of drugs that are indicated in this scheme, and now you will know for sure which ointment for acne on the face will be the best in your case. Please note that azelaic and salicylic acids are not the main remedy for acne on the face, and can only be used as “second-tier” drugs. You can find out more about them at the link above. At the same link you can learn about the use of oral contraceptives in women.
How to choose the right product for you
To choose a good external remedy for cleansing skin from rashes, you need to consider a number of parameters. The main ones:
- Why do acne appear? If their formation is caused by excessive expansion of pores, you need products that narrow them. When the reason is the presence of certain bacteria on the skin, antibacterial creams and ointments will help.
- Skin type – it is important that the cosmetic product matches your skin type. Drying products are suitable for oily skin, but for dry skin they will be too aggressive. The use of skin care cosmetics that are not suitable for a specific skin type can aggravate aesthetic problems. You should especially carefully select products for sensitive skin types. They must certainly have a soft effect.
- If you have allergies, it is better to give preference to hypoallergenic products.
- Good creams do not contain petroleum products, as well as synthetic additives and artificial flavors. Their presence can further irritate the skin, causing new rashes to appear.
It is important to choose a product that is right for you
It is very important that anti-acne products do not clog pores, otherwise the skin will receive insufficient oxygen, and this worsens its condition, appearance, and contributes to the spread of rashes.
This effective remedy helps against acne because it acts comprehensively. It provides good cleansing, relieves inflammation, has an antibacterial and drying effect. The drugs also reduce sebum production and tighten pores, resulting in the removal of acne. The skin becomes healthy and well-groomed. The main thing is to choose a product that suits your skin type and switch to a balanced diet.
Using topical acne treatments provides only 50-60% of the results. Otherwise, the effectiveness of treatment is determined by the state of health and lifestyle.
Antibiotics for acne treatment –
Antibacterial drugs for the treatment of acne can be used both for external use (usually in the form of gels) and in the form of tablets for oral administration. Modern research shows that antibacterial therapy in patients with acne is not very effective, because Over time, it causes the formation of resistant strains of bacteria and, as a result, leads to more severe acne. But in some cases, antibiotic therapy for acne is still necessary, and in addition, there are ways to reduce the risk of bacterial resistance to antibiotics.
a) Mild to moderate papulopustular acne:
Antibiotics, if prescribed, are only externally. These may be drugs such as Dalacin, Clindovit or Clindatop. These drugs are monocomponent gels containing the antibiotic clindamycin. In addition, there are drugs in the form of solutions for topical use, for example, the drug Zerkalin. This drug is clindamycin based, but it also contains alcohol, which is actually not very good for acne patients (especially if you are also using retinoids and benzoyl peroxide).
Another drug - Zinerit (in the form of a solution that is applied using an applicator) - is based on erythromycin, but there are now many resistant strains of the bacterium P.acnes to this antibiotic. There are also combination preparations that, in addition to the antibiotic, may additionally contain either the retinoid adapalene or benzoyl peroxide. An example of several combination preparations in the form of gels:
- Klenzit-S – contains clindamycin 1% + adapalene 0.1%,
- Indoxyl – contains clindamycin 1% + benzoyl peroxide 5%.
Photos of some drugs –
Important: for papulopustular acne of mild or moderate severity, antibacterial gels are prescribed primarily only in cases where the predominant inflammatory elements in the patient are pustules with pus. In this case, in addition to the external antibiotic, we must simultaneously use + external retinoids, + benzoyl peroxide.
And here you may ask: why is it recommended to also use benzoyl peroxide when prescribing an antibiotic gel? Isn't one antibiotic enough? The fact is that the use of benzoyl peroxide together with an antibiotic greatly reduces the risk of P.acnes bacteria developing resistance to antibiotics. Including the development of such resistance contributes to the transformation of mild forms of acne into forms with a more severe course.
As for patients whose inflammatory elements are represented predominantly by papules (i.e., without pus), it is irrational to prescribe antibiotics in this case. It is optimal to use only a combination of external preparations “benzoyl peroxide + retinoid”.
b) Papulopustular form of severe acne:
For severe papulopustular acne, antibiotics are prescribed only orally (i.e. in tablets for oral administration), plus we prescribe externally retinoids + benzoyl peroxide. For systemic antibiotic therapy, drugs from the tetracycline group will be primarily used - this can be either tetracycline itself or its derivatives - doxycycline and minocycline. Only a doctor can determine the optimal dosage for each individual patient.
As for tetracycline, the average daily dosage is usually 1000 mg, but in serious cases the dose can be increased to 3500 mg per day (such doses can only be used under monitoring of liver function). Tetracycline can be taken only 1 hour before meals or 2 hours after; the duration of administration is determined by the doctor, but not more than 8 weeks. However, this drug has serious age restrictions, and in recent years more resistant strains of P. acnes have been discovered.
Much fewer resistant P. acnes strains have been found to lipophilic tetracyclines (such as doxycycline and minocycline). Doxycycline is taken at a dose of 100 to 200 mg per day orally for no more than 8 weeks, regardless of meals. However, it induces photosensitivity in the summer and therefore in summer it is better to use another antibiotic (azithromycin). Minocycline is also taken at a dose of 100-200 mg per day, but this drug can cause blue-black pigmentation in different areas of the skin. This pigmentation most often occurs in the area of atrophic scars and acne scars.
A good drug of doxycycline is
Antibiotics of the Macrolide group - previously a drug such as erythromycin was widely used, but now there are a lot of resistant strains of P.acnes to it. It is more preferable to prescribe azithromycin in a dose of 250 to 500 mg (taken only 3 times a week). Unfortunately, this drug may have side effects such as diarrhea, and therefore it is best to take it only with parallel medications to restore intestinal microflora. Azithromycin is a good alternative for patients who cannot use doxycycline.
Antibiotics of the Lincosamide group - clindamycin belongs to this group of antibiotics. But its use is justified only for external therapy (with the composition of products for external use), and when taken orally, there is too high a risk of getting a severe form of anibio-associated diarrhea, which is called pseudomembranous colitis. This is such a terrible thing (with a high mortality rate) that don’t even think about taking clindamycin tablets.
Drugs of the sulfone group - these include the drug Dapsone, but it can only be used if the patient develops resistance to other antibiotics (i.e. this drug will not be the first choice drug). Antibiotic resistance should be suspected if there is no response to treatment after 6 weeks of antibiotics. Moreover, in cases where we assume resistance, it is very important for us to exclude the development of gram-negative folliculitis in the patient (usually it occurs precisely after long-term use of antibiotics in the past).
Important: the most painful area of antibiotic therapy in the treatment of acne is the development of resistant strains of P.acnes and S.epidermidis. Concurrent use of topical benzoyl peroxide products with antibiotics, and avoidance of frequent changes between different antibiotics, are the best ways to prevent antibiotic resistance in P. acnes and S. epidermidis. Phototherapy procedures (IPL), photodynamic therapy, and the use of lasers can help reduce the need for antibiotics. We will tell you more about them at the end of the article.
Reviews
There are different reviews of products against skin problems. The best impression on consumers was made by: Synthomycin liniment containing an antibiotic, Benzyl benzoate 20%, Acne-Sept lotion for acne and blackheads, Rohto Acnes 25 cream, Noreva Exfoliac Nc gel, Miracle blackhead removal wipes, Mizon cream and others.
When evaluating medications, consumers rely primarily on the speed of getting rid of the problem, the cost of the product, its composition, and consistency. Only a small part of the reviews mentioned the pleasant smell and packaging.
Preparations with benzoyl peroxide –
Benzoyl peroxide is a bactericidal component and is probably the best remedy for acne (it can even be called the gold standard of therapy). This is a bactericidal component that effectively inhibits the growth of P. acnes bacteria, leading to the development of local inflammation in the area of hair follicles and the appearance of papules and pustules (pimples). It is very important that benzoyl peroxide, unlike antibiotics, does not cause the emergence of antibiotic-resistant microflora.
Professional pharmaceutical preparations with benzoyl peroxide are produced in the form of a gel (usually with a concentration of 2.5 or 5%). For the first month, in order to get the skin accustomed to benzoyl peroxide, it is optimal to use a concentration of 2.5%, and then switch to 5% of the product. If you use more concentrated products at once, irritation will likely appear on the skin. The classic monocomponent preparation with benzoyl peroxide 2.5 or 5% is Baziron-gel.
Combination drugs - but there are drugs where benzoyl peroxide is combined with an antibiotic or retinoid. As you will see below, each of these drugs will be effective in slightly different clinical situations, for example, depending on what type of inflammatory components (papules or pustules) you have. Examples of combination drugs for acne treatment:
- Indoxyl (UK) – benzoyl peroxide 5% + clindamycin 1%.
- Effezel (France) – benzoyl peroxide 2.5% + retinoid adapalene 0.1%.
How to choose the right drugs:
1) For mild to moderate papulopustular acne, the choice depends on the predominance of certain inflammatory elements. If papules predominate (without pus inside), then in this case the combination of “benzoyl peroxide + retinoid” will be optimal. For example, this could be the combination drug Effezel. But for patients with sensitive skin, it is better to use a combination of two monodrugs - benzoyl peroxide in the morning and a retinoid in the evening.
Thus, you can use the drug “Baziron” with benzene peroxide in the morning, and in the evening – one of two drugs “Klenzit” or “Differin” (containing the retinoid adapalene) of your choice. But if you have pustules with pus, then to the above combination of “benzoyl peroxide + retinoid” we also add external use of an antibiotic.
2) For severe papulopustular acne, we also use “benzoyl peroxide + retinoid” for external use, and also add systemic antibacterial therapy. Antibiotics for this form are used only orally, in long courses of up to 6-8 weeks (see above).
Side effects of benzoyl peroxide: Be aware that itching, burning sensation, dryness, tightness, redness, or flaking of the skin may occur after use. But usually these effects are not too pronounced. If you use the drug during active sunny periods, be sure to use sunscreen, because Benzoyl peroxide makes facial skin more sensitive to sunlight.
Kinds
Acne products are available in a wide range. They come in various forms. Both in pharmacies and some stores you can find ointments, creams, gels and other types of products intended for external use.
Creams
This form is the most popular. This is due to ease of use. The creams are easy to apply, quickly absorbed, and do not leave marks on clothes. But it is worth considering that the cream is not able to penetrate into the deep layers of the epidermis, so it is intended more to eliminate external signs of the disease.
Creams containing antibiotics or hormones act quickly and effectively. But they cannot be used uncontrollably. Such drugs are prescribed only by a dermatologist. If used incorrectly, withdrawal symptoms or, even worse, skin atrophy may occur.
The most effective acne remedies in cream form are:
- zenerite;
- clearasil.
- differin;
- baziron;
- skinoren;
Ointments
This form of acne treatment, unlike cream, penetrates into the deep layers of the dermis. Ointments can influence the cause of acne if it is associated with diseases and damage to the epidermis, and not with stress or hormonal imbalance. In the latter cases, additional drug treatment will be required.
An ointment is a preparation based on fat. Therefore, it takes longer to absorb than creams, but lasts much longer. It is applied only to dry skin, but the cream can be used on damp dermis.
Most ointments have a drying effect. But this does not apply to all drugs.
The following ointments are effective in the fight against acne: ichthyol, levomekol, erythromycin, metronidazole.
Gels
This acne remedy is distinguished by the absence of fat and oils. The acid-base indicators of the gels are as close as possible to the skin. They are easy to apply, absorb quickly, leave no residue, and do not clog pores. Some gels, after application, form a film that does not allow air to pass through (Diclofenac). The consistency of the product can be liquid or viscous. If you store the gel in the refrigerator, it will become thicker, but after heating its structure is completely restored.
The best acne gels:
- clindovit;
- Cynovitis
- clensite;
- dimexide;
- metrogil gel;
Other
In addition to creams, ointments, and gels, there are also balms, pastes, and lotions.
The balm is distinguished by the absence of water in its composition. This is a concentrate of active ingredients, usually of plant origin. To enhance their healing properties, modern medicinal substances are additionally added to them.
The advantage of balms is the long period of preservation of properties, as well as the absence of a natural environment for the growth of bacteria, which is water.
The paste is a very thick ointment. It is used in different ways: either gently rubbed in, or applied as a spot treatment directly to pimples.
Lotions are watery. They may contain alcohol, as well as active ingredients: vitamins, organic acids, plant extracts, herbs, antibiotics, antiseptics. Lotions can be used as:
- hygienic cleanser;
- as a medicinal treatment;
- as a cosmetic product for moisturizing and nourishing the skin with vitamins.
The purpose of the lotion depends on the composition of the components.
Topical retinoids (adapalene)
In fact, this is the most important ointment for acne on the face. Topical retinoids are intended for external use. Such drugs are prescribed - 1) for the comedonal form of acne, which means acne, 2) for the papulopustular form of acne (i.e. in the presence of pimples). Previously, the topical retinoid tretinoin was used to treat acne, but it had a lot of side effects, and now there are much safer 4th generation topical retinoids, for example, adapalene.
Such drugs are monocomponent and combined. Monopreparations based on adapalene include Differin, Klenzit or Adaklin. A number of drugs of this type are produced only in the form of gels, but some manufacturers produce drugs with adapalene in both gel and cream form. Gel products will be more effective, but facial acne cream is more suitable for patients with dry and/or sensitive skin (and will help reduce the risk of irritation in such patients).
Examples of combination drugs with retinoids are 1) Klenzit-S, containing adapalene together with the antibiotic clindamycin, 2) Effezel, containing adapalene in combination with benzoyl peroxide. The choice of drug will depend on the severity of the acne, as well as on which inflammatory elements predominate in you (papules or pustules). All this information is schematically reflected in Table 1, which we placed before the description of groups of drugs for the treatment of acne.
How to treat facial acne with retinoids:
- Preparations containing adapalene should be used once a day before bedtime. Before applying a retinoid, you should wash your face with a mild cleanser. Before applying the retinoid, the skin must be completely dry, because... otherwise severe irritation will develop. To get your skin used to it and not be too irritated, start using the drug 3 times a week. After 1-2 weeks, switch to daily use.
When can you expect results: skin oiliness decreases sharply within a few days from the first use. As for acne and pimples, the first noticeable result can be seen only after about 4 weeks of therapy. Good results can be seen after about 8 weeks of using retinoids, but for radical improvement a full course is required, which lasts at least 12 weeks (3 months).
Use of oral retinoids:
In addition to topical retinoids intended for external use, there are also so-called systemic retinoids for oral administration. Such drugs (Acnecutane or Roaccutane) contain the retinoid isotretinoin. These drugs are very effective for treating acne, but they also have very serious side effects. Therefore, such drugs are used only in difficult situations, for example, for the treatment of nodular and conglobate forms of acne.
Use of oral contraceptives in women:
As for the use of oral contraceptives in women, you can read more about this method of treatment in the article at the link below:
→ Oral contraceptives for acne in women
Best Remedies for Acne Spots
The fourth category is effective remedies for acne spots on the face. Their main task is to accelerate the processes of regeneration and cellular renewal. The active components are aimed at healing, resorption of scars, increasing turgor, as well as eliminating pigmentation and spots. 4 nominees have proven their effectiveness.
Heparin ointment
A domestically produced ointment that inhibits the activity of bacteria. It normalizes the production of skin secretions and has an anti-inflammatory effect. Additionally reduces puffiness and evens out facial tone.
The active component is sodium heparin, it improves blood microcirculation, promotes the resorption of hematomas and blood clots. Benzyl nicotinate increases blood circulation, dilates blood vessels, and provides heparin with better penetration. Benzocaine is an anesthetic and reduces pain.
The formula also includes the humectant glycerin and petroleum jelly, which forms a protective film against bacteria. Stearic acid makes the dermis silky. Peach oil nourishes and maintains hydrobalance. Packaging – aluminum tube 25 g.
Advantages:
- Anti-inflammatory properties;
- Reducing puffiness and evening out facial tone;
- Resolves hematomas and blood clots;
- Effective;
- Moisturizing and protecting against bacteria;
- Inexpensive.
Flaws:
- Allergy to some components;
- Not for long term use.
The product is used 2-3 times a day until inflammation disappears (3-8 days). To make the result more effective, it is better to avoid makeup at the time of treatment, and also take a break from using thick creams and medications.
Methyluracil
A domestically produced ointment with an antibacterial effect and a beneficial effect on the immune system. Restores and regenerates the skin. Successfully fights subcutaneous mites and various pathogens.
It is based on the anabolic methyluracil, which promotes the healing of damaged skin areas and stimulates the formation of leukocytes. An auxiliary component is lanolin, which has a rich composition similar to human lard. It softens and nourishes the dermis. Vaseline improves the permeability of substances.
The ointment is safe because it does not enter the body through healthy tissue. At the same time, it helps to accelerate metabolic processes, neutralizes scars. Available in an aluminum tube weighing 25 g. The texture is white and greasy.
Advantages:
- Acceleration of metabolic processes;
- Antiseptic properties;
- Strengthening local immunity;
- Elimination of scars;
- Safety;
- Inexpensive.
Flaws:
- Difficult to absorb;
- Prohibited during pregnancy and lactation.
Before application, cleaning with an antiseptic is necessary. Frequency of application: 2 times daily with a thin layer applied to spots. The duration depends on the amount of inflammation, but no more than 7-8 days. In advanced cases – 15 days.
Clearwin Ayurvedic lotion
A universal cosmetic product from a Russian manufacturer is suitable for combating acne and post-acne. Regular use ensures gentle and thorough cleansing. The lotion is completely hypoallergenic.
Containing turmeric, it brightens the epidermis, relieves irritation, eliminates acne, and smoothes wrinkles. Neem has strong antiseptic properties and is a natural preservative. Licorice relieves irritation, swelling and inflammation. Magnolia prevents the development of pathogenic flora.
Aloe Barbados moisturizes, nourishes and promotes tissue healing. The product is packaged in a 100 ml plastic bottle with a convenient dispenser. The lotion is transparent, the smell is cosmetic, pleasant. Does not leave a greasy film or stickiness.
Advantages:
- Natural composition;
- Gentle, thorough cleansing;
- Hypoallergenic;
- Antiseptic effect;
- Lightening spots, scars;
- Inexpensive.
Flaws:
- Small volume;
- Dries the skin.
The rash areas should be treated locally with a cotton sponge moistened with lotion. After 30-40 minutes, the residues are washed off with running water or left overnight to increase the effectiveness of the procedures.
Zerkalin
A disinfectant that destroys the causative agent of infection, and as a result, acne. It is active against papules, pustules and large, dense nodes. Permitted for use from 12 years of age. Country of origin: Croatia.
The active ingredient is the antibiotic clindamycin hydrochloride, which effectively suppresses acne. It accumulates in the pores and begins to act from the inside. Ethyl alcohol acts as an antiseptic. Propylene glycol is included to moisturize the epidermis and is an absorption enhancer.
"Zerkalin" is suitable for people with reduced immunity. A colorless, transparent liquid with an alcohol odor, packaged in 30 ml dark glass bottles with a dropper and a screw cap.
Advantages:
- Antibiotic included;
- Destruction of infectious agents;
- Performance;
- Antiseptic properties;
- Convenient application;
- Economical consumption.
Flaws:
- Contraindications;
- Smell of alcohol.
It is not recommended to use the drug simultaneously with other drugs of a similar profile. Spot application to pre-cleaned areas 2 times a day. The course of treatment is 5-8 weeks, in advanced cases up to six months.
Squeezing pimples and blackheads (comedone extraction)
For comedonal and papulopustular forms of acne, invasive methods are sometimes used, for example, comedonal extraction. Extraction means their removal/squeezing out - using special comedones extractor tools, or by palpation. Moreover, we are talking about the removal of macrocomedones, i.e. large eels. But squeezing out pimples (papules and pustules) can, at best, lead to the appearance of a hyperpigmented spot in this area in the future.
In the worst case, self-squeezing pimples and blackheads can lead to the spread of inflammation and the formation of deep subcutaneous pimples, which will leave superficial or deep atrophic scars on the skin. Therefore, only comedones (acne) can be squeezed out, and secondly, this should only be done by a dermatologist or a dermato-cosmetologist. The procedure is called “mechanical facial cleansing.”
Mechanical facial cleansing: video
Important: keep in mind that the removal of comedones is much easier and without complications if the patient has previously used topical retinoids for at least 3-4 weeks. The fact is that topical retinoids (adapalene) also have comedonolytic properties.
The main causes of acne
In order for acne treatment to bring maximum results, you need to eliminate the cause that provokes its formation. Skin rashes are caused by:
- emotional shocks, stress, nervous strain, worries;
- frequent contact with hands or phones that have germs on the surface;
- hormonal imbalance, thyroid diseases;
- heredity;
- use of corticosteroids, birth control pills;
- diseases of the gastrointestinal tract, in particular the intestines;
- unhealthy diet - content in the diet of fast food, fatty and fried foods, as well as sweets and baked goods;
- allergic reaction;
- bad habits - nicotine and alcohol provoke metabolic disorders;
- incorrect choice of cosmetics, use of too oily cosmetics.
A doctor will help determine the true cause of the rash. To do this, you can contact a gastroenterologist, endocrinologist, allergist, infectious disease specialist, dermatologist, hematologist. A nutritionist and cosmetologist will also help. By determining the cause of the rash and eliminating it, you can count on the fact that anti-acne products will be effective.
Phototherapy and lasers for acne treatment
Phototherapy and lasers are used to treat acne - either endogenous porphyrins contained in P. acnes, or sources of exogenous porphyrins are additionally applied to the skin before the procedure. Porphyrins have the property of absorbing light in the blue regions of the spectrum (wavelength 415 nm), which leads to the formation of unstable oxygen and, as a result, to the destruction of pathogenic bacteria P.acnes. The FDA recommends Lumenis devices (for example, the IPL module of the M-22 device), which use high-intensity light from the blue part of the spectrum, for the treatment of papulopustular acne, i.e. acne.
Light from the red part of the spectrum can also be useful because... Compared to blue light, it has a stronger anti-inflammatory effect (although it has a lesser effect on porphyrins). Therefore, a combination of light from the blue and red parts of the spectrum will be even more useful. Facial procedures are carried out 2 times a week for 15 minutes. According to the dermatology textbook Fitzpatrick's Dermatology, after a 4-week course of therapy in 80% of patients, the number of acne decreased by 60%. But in the absence of supporting procedures, their number returns to the original level - within 3-6 months.
Photodynamic therapy is even more effective in treating acne. It consists of applying exogenous porphyrins to the skin 1 hour before the procedure (aminolevulinic acid/ALA), after which exposure to a high-power light source occurs. The latter can be pulsed dye lasers, intense pulsed light or a broadband light source in the red part of the spectrum. ALA is metabolized in the sebaceous glands and hair follicle to porphyrins, which when exposed to light lead to the release of unstable oxygen, which damages the sebaceous glands. Several photodynamic therapy treatments can provide improvement for up to 5 months.
Pulsed KTP laser (wavelength 532 nm) - also leads to a reduction in the number of acne by about 40%. Using this laser 2 times a week for 2 weeks, i.e. a total of 4 procedures are required). In addition, some of the non-ablative infrared lasers at 1450 nm and 1320 nm wavelengths may also be useful for treating acne. they cause thermal damage to the sebaceous glands. However, any of these lasers requires a course of several treatments (and the improvement lasts up to about 6 months).
One of the newest acne treatment devices is the Isolaz device (from Solta Medical). The nozzle of the device is made in the form of a photo-pneumatic device, which creates negative pressure that sucks out the fatty secretion from the mouths of the hair follicles. Immediately after this, broadband pulsed light (wavelength from 400 to 1200 nm) is turned on, which acts on the P. acnes porphyrins, destroying these bacteria, and also has an anti-inflammatory effect.
What do phototherapy and lasers do?
Regular use in courses not only improves the course of acne, thereby reducing the number of inflammatory elements. The use of phototherapy (IPL) and lasers in courses often avoids the need for oral medications (antibiotics, isotretinoin), as well as the numerous side effects associated with them. But the cost of such treatment is high. We hope that our article on the topic: How to remove acne on your face was useful to you!
Sources:
1. Higher medical education of the author of the article, 2. Textbook on dermatology “Fitzpatrick's Dermatology” (8th edition), 3. “Modern methods of treatment and rehabilitation of patients with acne vulgaris” (Barinova), 4. “Acne from the position of evidence-based medicine” (Anisimova), 5. “Cellular mechanisms of barrier protective functions of the skin and their disorders in skin diseases” (Medelets).
Features of application
Acne products must be used correctly. Here are some rules:
- The cream is usually applied twice a day: morning and evening. You can steam the skin first. This is done for deeper penetration of the components of the product;
- Do not use medications containing antibiotics or hormones without a doctor’s prescription.
- if the comedones are closed (whiteheads), then you can supplement the course of treatment with a scrub. It is used 1-2 times a week;
- If the acne is isolated, then it is better to apply any drug, be it ointment or cream, pointwise, without affecting healthy skin. The components contained in some products (especially hormonal ones, with antibiotics) are not needed at all for a clean epidermis;
- After 15-20 minutes, remove excess product. Unabsorbed cream or ointment will clog pores;
- if the drug used does not help and positive dynamics are not observed after 10-14 days, it is recommended to replace it. Don't make a decision on your own. Consult a dermatologist or cosmetologist for advice;
- Before using any product, read the instructions. Avoid overdose;
- If you are at risk, test the drug on an inconspicuous area of skin and wait 2 days. If no allergic reaction is observed, the cream can be used;
- do not use several products at once;
Mechanism of action of drugs
When using medications against acne and acne, the following effects occur on the affected epidermis:
- antiseptic effect, by which bacteria are destroyed, the production of pus and the accumulation of polluting particles are suppressed;
- reducing the volume of pores, cleansing the internal contents of pollution, sebum, dead cells;
- elimination of oily shine;
- normalization of the function of the sebaceous glands;
- improving the color and condition of the structure of the epidermis;
- anti-inflammatory, anti-edematous effect;
- smoothing the skin structure, eliminating peeling.
Acne medications can have various side effects that should be taken into account when choosing therapy.
Therefore, before starting use, read the composition to make sure there are no individual intolerances. This will help eliminate inflammation, redness, itching, burning, and allergic rashes. If you use a drug based on antibiotics without a doctor’s prescription, resident microflora may develop and pathology of internal organs may form.
In combination with anti-acne medications, additional types of therapy are used:
- a diet that provides the body with nutrients, vitamins, trace elements and minerals that stabilize metabolism and metabolism;
- the use of sorbents that bind and remove toxic substances before they spread into the systemic bloodstream.
Among sorbents, the greatest effect is observed with Enterosgel. It consists of high-quality components that quickly absorb any toxic substances. They do not have time to spread through the digestive tract, being absorbed into the blood. The product does not cause constipation or allergies. It gradually cleanses the intestinal microflora of pathogenic microorganisms. Long-term use is allowed as part of complex treatment.
Zeneritis for acne
The drug has a composition that causes an antibacterial effect. Therefore, it eliminates pathogenic microflora from the skin, preventing the formation of ulcers. This helps treat small and large acne and prevent its recurrence. The main component is Erythromycin, a broad-spectrum antibiotic that prevents the production of protein in bacterial cells, which gradually leads to their death. It is active against many bacteria.
The composition contains additional components that increase the spectrum of action. For example, zinc. It eliminates inflammatory processes, cleanses the skin from accumulation of dirt and fat, and has an antiseptic effect.
The drug must be applied to the epidermis for the effect to occur. It is usually observed within 2 weeks after initial use. The maximum course of treatment is 3 months, after which the face becomes completely cleansed.
The product must not be used over an excessively long course of treatment, otherwise the bacteria will develop an addiction to the active substance.
They will become resistant, the effect will not occur. Therefore, it is recommended to apply the product no more than once a day and take breaks between courses of treatment.
Treatment with Skinoren
The medicine contains a broad-spectrum antibiotic, which produces an antibacterial effect. The drug has the following properties that distinguish it from other anti-acne products:
- The main form of release is cream, gel;
- penetration into the deep layers of the epidermis;
- the main active component is azelaic acid, which destroys and prevents the development of pathogenic microflora;
- suppression of the activity of the sebaceous glands;
- prevention and elimination of acne;
- removal of traces of connective tissue scars formed from the removal of acne;
- elimination of age spots.
1 month of use is enough for the first result to appear. A lasting effect is observed within 6 months after continuous therapy.
Recommendations for use:
- spot application to areas where pimples and blackheads appear;
- prohibition on contact with the mucous membrane of the eyes, which may cause irritation;
- prohibition on use during pregnancy, since the active component penetrates the placental barrier and causes a toxic effect.
Some patients may develop individual intolerance to the constituent components. It manifests itself in the form of an allergic reaction leading to inflammation, redness, and itching. To eliminate this effect, it is enough to stop taking the drug. If the allergy is severe, antihistamines are used.
Product prices
The table shows the main drugs and their approximate cost in the Russian Federation and other countries.
| Name | Price in Russia, rubles | Price in Belarus, rubles | Price in Ukraine, hryvnia |
| Proactive basic set | 3100 | 86 | 1340 |
| Zenerite | 430 | 15 | 156 |
| Skinoren | 790 | 25 | 367 |
| Baziron AS | 863 | 34 | 386 |
| Roaccutane | 1400-3400 | 56-102 | 686-1310 |
| Differin | 850 | 21 | 310 |
| Curiosin | 420 | 14 | 173 |
In each pharmacy, the listed drugs may vary slightly in price. This is due to the store’s markup, as well as the degree to which the purchase cost increases.
If a patient has acne on his face, they need to be dealt with in a timely manner. Contact a cosmetologist or dermatologist, who will first prescribe a laboratory and instrumental examination. The doctor will evaluate the quality of the pimples, selecting the optimal treatment. It includes local or systemic ointments, gels, creams, tablets. Their choice depends on the woman’s preferences, the possibility of timely treatment, and the presence or absence of side effects. It is necessary to take into account the presence of contraindications, side effects, and overdose. Then the risk of their development will be minimal.
Roaccutane for eliminating acne
This is one of the most effective drugs that fight acne. It has a fairly aggressive composition, so it must be used with caution. The product has the following features:
- Available in the form of capsules containing 10 or 20 mg of the active ingredient;
- the main active ingredient is isotretinoin, it is produced from vitamin A and soybeans;
- oral use of capsules;
- eliminate the increased activity of the sebaceous glands, have an anti-inflammatory effect, which gradually helps to get rid of pimples of any size;
- used only in the most severe cases when local remedies do not help;
- causes many side effects, negatively affects hearing, vision, and the condition of the digestive tract.
If the patient has an individual intolerance to the drug, irritation, inflammation, rash and other negative reactions may develop. Therefore, before use, carefully read the instructions to prevent individual intolerance.
Attention! Capsules should be prescribed by a cosmetologist, dermatologist, therapist or other doctor who conducted the preliminary examination. He assesses the patient's skin condition and his medical history. If there is a risk of developing individual intolerance or other side effects, oral administration of capsules is not recommended.