According to many of us, antibacterial drugs can be considered a panacea for most diseases that humanity faces.
After all, everyone knows the confirmed historical facts, according to which antibiotics were recognized as the greatest invention of the last century. These drugs helped save millions of lives during wars and epidemics, and now some modern scientists are in the continuous process of searching for new treatment regimens that will certainly lead humanity, if not to eternal life, then to complete victory over most diseases known to science. It would seem that if antibacterial drugs can save lives, then they will definitely help with the flu. And you won’t need any other treatment, just take a pill and the unpleasant symptoms will go away. But why, with all the successes of such therapy, the question still arises about the advisability of their use for influenza? Let's figure it out.
- Possibility of addiction to antibiotics
- Does it make sense to take it for the flu?
- Can children take it: doctors' opinion
- When is it necessary to take antibiotics?
- Antiviral treatment for influenza
The word “antibiotics” translated from ancient Greek means “against life”. In the modern interpretation, these drugs actually suppress the vital activity of pathogens of many diseases.i Historians claim that the great physician and philosopher Avicenna treated his patients with substances similar to modern antibiotics. But antibacterial drugs received widespread recognition only in 1929, when the British scientist Alexander Fleming reported on a new miracle substance that he was able to isolate from mold colonies. This substance was called penicillin. People also called it “magic bullets”, which hit the target precisely at pathogenic microorganisms. The substance found was able to fight staphylococci, streptococci and pneumococci.
Over time, antibiotics were improved, thanks to which doctors were able to save more and more patients who were previously considered hopeless. Cephalosporins, augmentin, macrolides - all these drugs are probably familiar to everyone who has had to fight infectious diseases or treat children for them.
Every year the arsenal of this type of drugs increases. They are the object of study by millions of scientists from the fields of microbiology, pharmacology, medicine and radiobiology. In recent years, hundreds of drugs with different spectrums of action have been discovered. However, a fairly limited number of drugs are still used in practice. This is explained both by the fact that resistance (immunity) can develop quite quickly to drugs in this group, and by the fact that not all drugs can be used for all groups of patients. We must also remember that antibiotics are useless against some diseases. The list of these diseases includes influenza. In most cases, antibiotics are not needed for this disease. We’ll talk about nuances and exceptions separately.
Accustoming the body to antibiotics for influenza
“Can I take antibiotics for the flu?” This is one of the most common questions patients ask doctors. In some cases, patients with influenza infection decide to self-medicate with antibacterial drugs in order to shorten the period of the disease. They believe that antibacterial drugs can quickly eliminate symptoms of the disease such as fever, runny nose, sore throat, headache and pain in muscles and joints.
Unfortunately, as statistics show, self-medication with this type of medication does not lead to the desired results, but causes an increase in antibiotic resistance of the microflora.
A person who uncontrollably takes antibacterial drugs for viral diseases, without consulting a doctor and choosing the dose on his own, may later face the fact that these drugs will no longer be effective in treating various diseases. Bacterial resistance to drugs is a major obstacle to the treatment of a number of dangerous diseases, which leads to treatment failures.
By taking antibiotics for a flu infection without good reason, you risk one day finding yourself in a situation where these drugs will not help you fight serious bacterial diseases.ii The spread of drug-resistant strains of various diseases can lead to unpredictable consequences for humanity.
University
→ Home → University → University in the media → Pills or bed rest? How to treat colds and flu
Clinical pharmacologist with half a century of experience, Professor Mikhail Kevra recommends not to get carried away with medications for seasonal respiratory infections.
The specialist expressed concern about the growing drug addiction among the population and doctors, and also commented on several myths regarding methods of prevention and treatment of colds and flu. The medicine was created, but the virus has changed
— Mikhail Konstantinovich, during the cold season, people actively buy “anti-cold” pills, that is, antiviral pills that are sold without a doctor’s prescription. A typical request to a pharmacy worker is to advise the best. And judging by the advertising, all the drugs are “powerful and work flawlessly.” As a specialist who has spent his entire life studying the effects of medications on the human body, what do you recommend?
- Today not a single name will come out of my mouth. And not only because of the reluctance to support the commercial interests of producers. The fact is that most of the existing so-called. Antiviral drugs only alleviate the symptoms of the disease, but do not have a detrimental effect on the virus itself. Unfortunately, recently created drugs that inhibit the reproduction of viruses are rapidly losing their effectiveness.
This is primarily due to the rapid variability of the antigenic structure of the virus. For example, it has been established that the influenza virus, under the influence of various environmental factors, can change dramatically within 6–10 months and become resistant to those medications that were recently effective. It is impossible to develop a new drug in such a period of time, and the virus will become different again... And this process is endless.
Lie down - and no work!
—So you want to say that if a cold is treated, it will go away in 7 days, but if not, then you will be sick for a week? — The body itself fights the pathogen of ARI. He needs help. The first thing to do is to ensure complete rest (especially in the first three days of the disease). Previously, in clinical guidelines for the treatment of respiratory infections, the first point was to prescribe bed rest, and only then medications. Why? Because the virus greatly weakens the body, and if a person continues to lead a normal lifestyle or, even worse, exposes himself to increased stress, then there is simply no strength left to fight the pathogen. The weaker the immune system, the more actively pathogenic viruses cling and the more opportunistic flora multiplies. Today, unfortunately, the emphasis in treatment has shifted to the use of drugs. The sick person takes pills and continues to go to work. What does this lead to? To a protracted course and the occurrence of complications. In time pressure, it is very difficult to overcome the pathogen. The second important condition for the fight against the virus is plenty of warming drinks (tea with lemon, honey, raspberries, milk with honey, herbal tea). Toxins produced by the pathogen are removed with the liquid. — To hear such recommendations from a clinical pharmacologist, frankly speaking, is unexpected... — There is a pharmacomania in society: many cannot imagine recovery without pills, injections and droppers. And doctors to whom the patient “indicates” that he was prescribed few medications or the wrong ones that help, is easy to understand: sometimes specialists prescribe the required medications under moral pressure, fearing conflicts and complaints. To some extent, they are right: if a person believes that such a drug is effective, a placebo will help him recover. But this has nothing to do with the real effectiveness of the medicine. We must understand that the body perceives any chemical as foreign and hostile. The first reaction of the cells that meet it is protest and fight. It turns out that instead of conserving the strength the body needs to suppress and destroy the pathogen, we force our body to spend it on adapting to the drugs. A comparative study was conducted in the UK: some patients with a respiratory viral infection were treated with antiviral drugs, while others were treated with hot chicken broth with spices. In the group of those who did not take chemicals, the results were better. This was explained not only by the warming effect of the liquid, but also by the presence of extractive substances in the broth that help the body cope with the infection. — Is drug prophylaxis possible for ARI? One of the medications, according to the instructions, can be taken to prevent infection. “It is very difficult to stop the spread of the virus using the drug. I consider regular hand and face washing a much more realistic option. Most often, we get the virus not through inhaled air, but through our hands. He scratched his nose, rubbed his eyes - and the pathogen penetrated the mucous membrane. When coming from the street, after communicating with a sick person, you should immediately wash your hands - and the risk will decrease. But life shows that pharmacologists cannot be convinced of this! Since ancient times, people have used plants containing phytoncides (garlic, onion) to prevent viral infections. — It is not uncommon for people with ARI to prevent complications to take antibiotics like amoxicillin, which can be bought without a prescription... — If complications have not developed, there is no inflammation caused by bacteria, then what is the antimicrobial drug aimed at destroying? To other flora, including microorganisms that are beneficial in the fight against disease. In addition to pathogens, so-called pathogens live on mucous membranes. saprophytic microorganisms that do not themselves cause disease, but help fight the virus. If they are destroyed, the virus has an additional opportunity to survive. The immune system, which has already survived the blow, weakens even more. The use of antibiotics “for prevention” leads to the fact that microbes become increasingly resistant to antimicrobial drugs. Is there any benefit from immunomodulators - The conclusion suggests itself: it is necessary to support the immune system. There are many drugs that stimulate it... - The best immunity against acute respiratory infection is developed in the body after a person has had it. Therefore, in children and young people, the flu is more “brighter” and more often causes complications, because their immune system has less experience in fighting it. But since there are so many pathogens of ARVI, a person gets sick again and again. The second most effective means is vaccination: a weakened pathogen or its antigenic determinants are specially introduced into the body, thereby “warming up” the production of antibodies. The effect of drugs that are positioned as immunostimulants and immunomodulators is questionable. Clinical trials conducted on small groups of people are not proof! In the West, drugs that supposedly stimulate the activity of the immune system are not prescribed because most insurance companies do not pay for such therapy, not seeing any real benefit from it. There is also an assumption that stimulating the production of lymphocytes and other protective cells can simultaneously activate the growth of cancer cells.
Super-persistent myths about vitamins
— What can you say about the advisability of vitamin support for ARI, primarily ascorbic acid? Many are sure that this promotes a speedy recovery and strengthens defenses.
— If there are not enough vitamins in the blood (the deficiency is confirmed by laboratory tests), then replenishment will have a positive effect. But with the same success, other essential substances - amino acids, sodium, calcium and other microelements - will “stimulate” the immune system!
The use of large doses of vitamin C (up to 3 g per day) to prevent colds was proposed by the famous chemist, two-time Nobel Prize winner Linus Carl Pauling.
First impressions of this use of ascorbic acid were optimistic. However, in more in-depth studies based on a double-blind control method (when neither the patient nor the doctor knows which drug is being used), it turned out that the frequency of colds under the influence of high doses of ascorbic acid does not decrease. And yet, there is still an opinion among the population about the miraculous properties of vitamin C. Unfortunately, such advice can also be found in the media.
Many clinical studies back in the 1970s convincingly proved that the administration of high doses of ascorbic acid to people with normal levels of it in the body does not reduce the incidence and severity of colds in either adults or children.
It should be noted, however, that there are situations with ARI when high doses of vitamins really help. For example, with influenza, scarlet fever, measles with hemorrhagic manifestations. In this case, they help strengthen the walls of capillaries.
Vitamins are essential organic substances. They must be constantly supplied with food, since the human body cannot store them for future use. But few are needed.
Vitamins created artificially are chemical substances with pronounced pharmacological activity. In therapeutic doses (which are 2-3 times higher than preventive doses), vitamin C can cause disruption of capillary permeability, which impairs the nutrition of organs and tissues. You need to be careful when prescribing these drugs to pregnant women and those who are planning to conceive: unreasonable use is fraught with disruptions in the course of pregnancy and even threatens the death of the embryo.
— Mothers and pediatricians really like to turn to vitamins... Are they wrong too?
- The child is lethargic and tired - they start feeding him “to raise his tone”, not knowing the level of these substances in the blood. Meanwhile, the child is overloaded at school and in clubs; he simply wants to relax and be in the fresh air. Synthetic substances will not compensate for this deficiency, but they can cause health problems.
It has been established that long-term intake of vitamin C in high doses (for preschoolers and primary school students this is 100-200 mg per day, i.e. 2-4 tablets of ascorbic acid with glucose) can lead to a decrease in the number of red blood cells and hemoglobin in the blood, an increase leukocyte content and a decrease in the number of lymphocytes. Even a single dose of ascorbic acid can provoke tachycardia (an increase in the number of heartbeats per minute), and a long-term dose can disrupt the nutrition of the heart muscle, which is easily determined by an electrocardiogram.
— At the end of winter, many of us are accustomed to buying vitamin complexes...
— Seasonal fluctuations in the content of vitamins in the blood are the norm, not a pathology. In summer and autumn, the level of vitamins in the blood will certainly increase even without taking complexes, and in winter and spring it will decrease.
Vitamins have been known to mankind for about 100 years, but they learned to obtain them artificially a little over 50 years ago. But summer and autumn, winter and spring have always existed, and with them seasonal fluctuations in the content of vitamins in the body. These are normal natural biorhythms that should not be interfered with. It wouldn’t even occur to anyone to “even out” the level of sex hormones during a woman’s monthly cycle!
If you really need to nourish the body, it is better by eating fresh fruits, vegetables and other foods that contain vitamins. It is almost impossible to create hypervitaminosis through regular food, but it is easy to create with the help of artificially created substances. Elena Kleshchenok Medical Bulletin , January 26, 2017
Share
Antibiotics against influenza: is there any point?
Scientists never tire of reminding us that with an exclusively viral etiology (when the disease was caused by viruses), antibacterial drugs are useless or even harmful, since they disrupt the biocenosis of the respiratory tract.iii This can lead to the fact that unusual flora, for example, intestinal flora, will predominate in the respiratory tract , which leads to additional complications.
One of the greatest dangers in the spread of drug resistance is the widespread use of macrolides, a group of antibiotics whose structure is based on a macrocyclic lactone ring. This type of medicine is able to disrupt the formation of bacterial proteins, due to which pathogenic organisms lose their ability to reproduce and are thus destroyed.
With unsystematic and unjustified use, macrolides accumulate and are very slowly removed from cells, which leads to the emergence of virus strains with drug resistance not only to macrolides, but also to other types of antibacterial drugs.iv To restore the sensitivity of the flora after self-medication and the ability to be effectively treated with antibacterial drugs, it is necessary long period of time. Remember: flu and antibiotics can be combined only after consulting a doctor .
Which antibiotics to choose
The name of the drug depends directly on the organ affected by secondary infection. Each antibacterial drug targets a specific strain of bacteria. If the doctor does not know the name of the bacterium that caused the disease, he can use a broad-spectrum drug aimed at a number of known microorganisms.
The most common drugs used for various bacterial complications of influenza are:
- Sumamed. The active ingredient is azithromycin. Effective for bacterial bronchitis, pneumonia, bacterial tonsillitis, sinusitis, sinusitis and otitis media. The children's form in the form of a suspension allows you to reduce the treatment time to 3 days.
- Amoxiclav. Analogues – Augmentin, Femoklav. This is a combination antibiotic that includes two active components: amoxicillin and clavulanic acid. This is a broad-spectrum antibiotic, effective against bacterial infections of the ENT organs, lower respiratory tract, as well as diseases of the pelvic organs.
- Suprax. The active substance is cefixime. The drug is also a broad-spectrum antibiotic. Effective against diseases of the upper respiratory tract: sinusitis, tracheitis, pharyngitis. They are also used in the treatment of otitis media and acute bronchitis.
- Avelox. The active substance of the drug is moxifloxacin. A broad-spectrum antibiotic, used for bacterial sinusitis, sinusitis, and bronchitis. It is chosen in the treatment of pneumonia if the disease is caused by microorganisms resistant to derivatives of penicillin, cephalosporin and tetracycline.
- Zinnat. The active ingredient is cefuroxime. This antibiotic is prescribed to patients with lesions of the upper and lower respiratory tract caused by bacteria resistant to ampicillin and amoxicillin.
Treatment of influenza with antibiotics in children: doctors' opinion
The scientific literature provides various data on the frequency of use of antibacterial drugs for ARVI, including influenza infection in children. According to research, antibiotics are used much more often in the treatment of children than is actually required. In the minds of many parents, influenza and antibiotic treatment are inseparable concepts. Of course, such therapy is often used without a doctor’s prescription. The widespread desire to treat children with antibacterial drugs, whether there is a serious reason for it or not, is observed in all countries of the world. For example, in Canada, almost 15% of children with signs of ARVI are prescribed antibacterial drugs. In Denmark, more than 60% of children under two years of age receive at least one course of this type of medication during the year. And in China, antibacterial drugs are recommended for almost 97% of children with cold symptoms.
The situation is aggravated by the fact that in some countries, including Russia, the sale of antibiotics in most cases is not regulated. All antibacterial drugs (including those used topically) in Russia are currently prescription drugs. However, since there are no actual regulatory measures at the state level for the dispensing of these drugs, they can be freely purchased in government and commercial pharmacies. The drugs are in most cases available without a prescription and are widely used for self-medication.
Many parents believe that it is easier to give their child antibiotics in the form of powders or tablets and thereby try to prevent the development of complications of influenza infection than to wait for a situation to develop when the child will not attend kindergarten or school for weeks. But doctors remind that no antibacterial drugs taken during self-medication and without the advice of a specialist will help protect the child from the development of complications, but will only increase the risk of side effects, including life-threatening ones.
Recommendations from professional communities of pediatricians, general practitioners, and consensus results from physicians in other specialties emphasize the importance of not using antibacterial agents in children with uncomplicated influenza infection. The following clinical manifestations, which are observed in the first 10-14 days of the disease, do not justify the use of antibiotics without compelling reasons:
- cough;
- runny nose;
- increased body temperature;
- redness of the throat;
- hoarseness of voice;
- wheezing;
- bronchial obstruction;
- labored breathing.
Antibiotics for ARVI, including influenza, in adults are also not needed in most cases.
When are probiotics most effective?
The list of diseases and pathological conditions for which the use of probiotic complexes is recommended is quite extensive. For antibiotic-associated diarrhea, American gastroenterologists, for example, recommend a combination of strains of Lactobacillus plantarum and Bifidobacterium infantis in a “community” with the fungi Sacchromyces boulardii. For infectious diarrhea caused by ARVI pathogens, two types of lactobacilli are indicated - Lactobacillus casei and Lactobacillus rhamnosus.
Of considerable importance to achieve the desired effect is the survival rate of microorganisms that we obtain from probiotic complexes. In other words, how high is their biochemical activity in the gastrointestinal tract. In addition to the above-mentioned lacto- and bifidobacteria, propionic acid bacteria Propionic bacterium are among the most “tenacious”. They not only restore the gastrointestinal tract after the “invasion” of antibiotics, but also act as immunomodulators. In addition, they suppress the development of many mutations, reduce the toxic effects of a number of chemicals and promote the growth and development of fecal bifidobacteria.
Back to list Previous article Next article
When is antibiotic treatment needed for influenza?
There is a very fine line between bacterial infections, for which treatment with antibacterial drugs is indicated, and viral infections, for which antibiotics are not required, which cannot always be quickly established. But there are still certain signals that may indicate that the patient has currently developed a bacterial complication:
- elevated body temperature does not go away for more than 5-6 days and remains at a very high level;
- body temperature dropped, but after 1-2 days it rose again to high numbers;
- after a period of improvement, there was a sharp deterioration in health;
- symptoms are observed that were not there before - increased headaches and cough, ear pain, etc.;
- purulent discharge appears - for example, discharge from the nose has acquired a greenish tint, yellow-white liquid is released from the ear canal, and sputum during expectoration acquires a cloudy grayish tint.
As a rule, bacterial complications in people at risk (children, pregnant women, elderly people) develop rapidly.
All of the above symptoms should alert the patient and force him to immediately consult a doctor. Only a doctor can make the correct diagnosis and decide whether it is necessary to start taking antibiotics. For example, if a viral pathogen of bronchitis is accompanied by a bacterial one and the disease itself is chronic, recurrent or atypical, it is almost impossible to do without antibacterial drugs.
What complications become an indication for taking antibiotics?
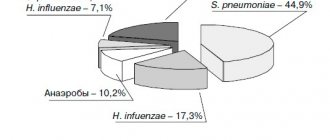
Influenza is often attributed to the development of a bacterial infection, which can cause bacterial:
- bronchitis;
- otitis;
- conjunctivitis;
- lymphadenitis;
- tonsillitis;
- sinusitis.
In addition, pneumonia is a common bacterial complication. The listed diagnoses are a direct indication for the prescription of antibiotics. The drugs will not alleviate the course of the flu itself and will not in any way speed up the process of recovery from a viral infection, but they will be able to overcome a secondary disease of bacterial etiology.