Author:
- Elena Vitalievna Naumova, otolaryngologist, leading doctor of the clinic
5.00 (Votes: 2)
It is difficult to cure a sore throat without antibiotics, so otolaryngologists often supplement the usual treatment regimen with antibacterial drugs. Antibacterial drugs differ in chemical composition and mechanism of action, so only a specialist can choose the best drug. It is important to note that uncontrolled self-administration of antibiotics only harms the body - dysbiosis develops, and the causative agent of sore throat remains and develops resistance to the medication.
To prevent this, you should consult with an ENT doctor, get tested, and only then begin treating tonsillitis with antibiotics.
Indications for use
Tonsillitis, accompanied by the following clinical picture, requires antibiotics:
- A clear white coating on the tonsils, visible to the naked eye.
- Consistently high temperature (above 38°C).
- Enlarged lymph nodes near the neck.
Antibiotics are effective only for tonsillitis caused by bacteria - fusobacterium Fusobacterium necrophorum, group A streptococcus, beta-hemolytic streptococcus Streptococcus pyogenes, staphylococcus, aerobic and anaerobic bacteria. To verify the bacterial etiology of the disease, the ENT doctor gives a referral for a bacterial culture from the back of the throat.
Important to remember! If a bacterial pathogen is not confirmed, then antibacterial therapy is not needed - antibiotics have no effect against viruses.
University
→ Home → University → University in the media → Does a sore throat need to be treated with antibiotics?
Sore throat, chronic tonsillitis - thousands of people are familiar with these diagnoses. Is it possible to get rid of a sore throat forever? How long should you take antibiotics? Is it possible to prevent this disease?
Assistant of the Department of Infectious Diseases of the Belarusian State Medical University, Candidate of Medical Sciences Nikita Solovey answered these and other questions from Komsomolskaya Pravda readers on a direct line
— I have chronic tonsillitis. For the last year, my sore throats have gone away without fever, but with stomatitis. Maybe some kind of prevention can be done?
— How does stomatitis manifest itself?
- Very painful ulcers appear in the mouth.
- Perhaps this problem is not related to your chronic tonsillitis. Stomatitis can be caused by other causes; you need to be examined by specialists who deal with the mucous membranes of the oral cavity, for example, dentists.
— And I also have constant traffic jams.
- If you do not have a fever or severe sore throat, topical medications with anti-inflammatory and antimicrobial effects may be effective, for example, evidence of effectiveness in studies has been obtained for nanocolloidal silver, extracts of certain algae and herbs. These remedies can also be useful for stomatitis.
— Why does chronic tonsillitis occur in general? Is this all due to reduced immunity?
- No, this is a feature of inflammation of the tonsils, which develops in response to the influence of certain microorganisms, often with not entirely correct treatment of repeated episodes of sore throat.
— If sore throats occur two or three times a year, is this an indication for tonsil removal?
— To date, research results show that in adults, removal of tonsils often does not lead to a reduction in the number of recurrent inflammations of the oropharynx. In fact, the final decision on indications is made by otolaryngologists during long-term observation of the patient.
Antibiotics must be taken for at least 10 days
— My son is already in the 8th grade, and since the 5th grade he has been tormented by sore throats. Now they are literally every two weeks, he practically does not go to school. Sore throat manifests itself only with a high temperature, up to 38 degrees. He was already in the hospital. Constantly takes antibiotics. The analysis showed that he had staphylococcus. What should we do?
— Recurrent tonsillitis is a common situation. It is extremely important to adequately treat each exacerbation with the correct course of antibiotics. It is not necessary to use injections; today, most antibiotics are highly effective when taken orally. It is important to carry out 10-day courses of antibacterial therapy. Otherwise, you get a clinical effect - the sore throat goes away, the temperature drops, but the pathogen on the tonsils remains.
— Is it possible to undergo any other examination besides the smear that revealed staphylococcus?
“Unfortunately, most studies do not show the real picture, since we can only examine the microflora from the surface of the tonsils. And in patients with chronic tonsillitis, as studies show, deep in the tonsils there may be a completely different microflora. Therefore, it is more important to adequately treat each episode of exacerbation.
- I'm already desperate. Taking antibiotics so often is also harmful.
— Even frequent use of antibiotics used in modern outpatient practice does not have any long-term consequences. It's a delusion. They can of course have side effects during treatment, just like any other medicine. But those drugs that are approved in our time do not have serious long-term consequences.
- I am 40 years old. The throat is constantly inflamed. Maybe I should have my tonsils removed? My doctor says that problems with the heart and joints may begin.
- At your age, removing your tonsils will not do any good. Problems with the heart and joints can be caused by frequently recurring tonsillitis caused by streptococcus pyogenes. This pathogen is more typical for children and adolescents and is rarely found in older people. In the case of chronic pharyngitis, during exacerbations, drugs with local antimicrobial and anti-inflammatory effects, for example, containing nanocolloidal silver or medicinal plant extracts, can be used.
A virus can also cause a sore throat
— Is it possible to do without antibiotics for a sore throat?
— It all depends on what kind of sore throat the patient develops. There are sore throats that are caused by bacterial pathogens, most often streptococcus pyogenes. But there are sore throats that are caused by respiratory viruses, and then antibacterial therapy is not needed. There are symptoms that practically exclude the bacterial nature of a sore throat: if, in addition to complaints of sore throat, plaque on the tonsils, and fever, there is also conjunctivitis, or a cough, or diarrhea, or a rash. This most likely indicates the viral nature of the disease and requires the use of only agents with a local anti-inflammatory effect.
— I had my tonsils removed when I was a child. And now, as I understand it, doctors are in no hurry to prescribe such an operation.
— First, you always need to adequately treat a sore throat. If this is not done, an acute, frequently recurring process can become chronic.
— I heard that tonsils are not completely removed, but only trimmed.
— There is no scientific evidence of the effectiveness of this procedure. We must understand that by removing the tonsils, we prevent frequent relapses of sore throat, but we open the path of infection to the upper respiratory tract. The tonsils are a barrier organ of the immune system. Recent studies show that the rate of recurrence of acute respiratory viral infections in children whose tonsils were removed is two and a half times higher than in those children who were not operated on. Therefore, tonsils should be removed when there is a real threat of the formation of acute rheumatic fever with consequences in the form of damage to the heart and joints, or when tonsillitis often recurs and ongoing antibacterial therapy becomes ineffective. In addition, not all patients are predisposed to rheumatic complications. Therefore, if we generalize the world experience, there are no clear instructions under which it is definitely necessary to remove tonsils. Everything is decided individually.
Do exercises and don't get too cold
— I am 46 years old, and I have had chronic tonsillitis since childhood. Maybe you can recommend some drug that needs to be taken constantly?
— How does your tonsillitis manifest itself?
— There are seasonal exacerbations, when the throat gets sore and congestion appears.
— Is the temperature rising?
- Not anymore.
— If an exacerbation occurs with a high fever and severe sore throat, it is important to be treated with a 10-day course of oral antibiotics. This course cannot be shortened, even if the patient begins to feel well. Together with the antibiotic, you can use local agents with antimicrobial action. In case of erased exacerbations, it is permissible to use only local remedies.
— Are there methods for preventing or preventing angina?
— Of the methods that have proven effectiveness in treating frequent sore throats, the only effective one is the long-term use of antibiotics with prolonged action. Injections of such antibiotics are given to the patient once a month for a long time. But such prevention is prescribed for very serious reasons, when a person has more than six sore throats per year or there is a threat of rheumatic complications.
In other cases, you just need to carry out general preventive measures: observe a rational work and rest schedule, eat right, develop physically, take multivitamins.
— Does hypothermia affect the occurrence of sore throat?
- Certainly. Hypothermia can lead to an acute or exacerbation of a chronic process. Tonsillitis pathogens live in our oral cavity anyway, but often they cannot realize their pathogenic potential until some predisposing factor occurs. And hypothermia is just that.
— Do rinsing with herbs help?
- Perhaps only at the very initial stage and with viral sore throats. If a real bacterial sore throat has developed, you cannot do without antibiotics. Komsomolskaya Pravda , November 24, 2015
Share
Features of antibiotic therapy in children
When treating tonsillitis in children, the ENT doctor prescribes predominantly local antibiotics, because Systemic medications have a detrimental effect on beneficial bacteria.
Basically, penicillin drugs or macrolides are used, since streptococcus or staphylococcus most often causes sore throat in children. The course of antibiotics is 7-10 days, and treatment cannot be stopped if the condition improves.
Important to remember! It is necessary to get tested before taking an antibiotic, because... symptoms of the initial stage of bacterial tonsillitis are similar to those of infectious mononucleosis.
Many parents are wary of taking antibiotics at a young age, but there is no need to worry. A properly selected drug prevents complications of tonsillitis such as rheumatic fever, purulent-inflammatory process, and peritonsillar abscess. The child tolerates the disease more easily and will not infect others.
It is important to know! If a child gets tonsillitis again, you should not take the same antibiotic again.
Severe stages of tonsillitis are treated with suspensions, an antibiotic in the form of a dry powder for oral administration.
Therapeutic tactics for tonsillitis
If we consider that chronic tonsillitis is only a long-term inflammatory process in the tonsils, then it is unlikely that this disease should have received so much attention from other medical specialties. Therefore, the very definition of tonsil disease as chronic tonsillitis requires clarification. This will make the motivation for different types of conservative or surgical treatment clearer. So, chronic tonsillitis is a process of constant interaction between lymphoid tissue and the contents of the lacunae of the palatine tonsils (purulent detritus with elements of foreign protein, toxins as a result of the vital activity of pathogenic flora, microorganisms themselves, dead epithelial cells from the walls of the lacunae of the palatine tonsils, nutritional particles). The discharge in the lacunae can be purulent, caseous, accumulate in narrow lacunae convoluted with spurs, and form so-called fetid plugs. This process, which takes place in the lacunae of the palatine tonsils, is under the control of the body until a certain time, i.e. There is constant active and passive drainage of tonsil lacunae along with the activity of macrophages, which, preventing inflammation of the palatine tonsil, contributes to the development of immunity to many microorganisms that enter the oral cavity and pharynx along with air and food.
This kind of balance between the vital activity of pathogenic active flora and the protective capabilities of the body can be disturbed for many reasons, as a result of which inflammation of varying intensity develops (it captures only the covering epithelium of the oral surface of the tonsils without its destruction), which passes to the epithelial cover of the lacunae of the tonsils with its destruction and formation necrotic plaques; suppuration of the tonsil follicles. Catarrhal, lacunar or follicular tonsillitis develops
.
In foreign literature, they tend to combine two diseases of the oropharynx and designate inflammation of the tonsils and pharyngeal mucosa as “tonsillopharyngitis.” However, experts in Russia quite reasonably believe that such a combination of two nosological units is possible only in cases of a combination of acute catarrhal pharyngitis and catarrhal tonsillitis. Lacunar and follicular tonsillitis have their own clearly defined clinical, morphological and microbiological aspects
, and they cannot be confused with manifestations of pharyngitis, especially from the point of view of the approach to treatment.
According to modern concepts, angina is an acute infectious-allergic disease, and it is necessary to approach the treatment of a patient with angina from this point of view.
As was said, the presence and persistent preservation of purulent detritus in the lacunae of the palatine tonsils is a determining factor both in making the diagnosis of “chronic tonsillitis” and in choosing the appropriate method of treatment - conservative or surgical.
A sore throat with destruction of the integumentary epithelium of the lacunae promotes the formation of scars in their lumen, which subsequently complicates the drainage of the lacunae of the tonsils. A kind of vicious circle arises - sore throat develops under the influence of pathogenic flora against the background of sensitization by a foreign protein due to a violation of the epithelial cover of the lacunae. Moreover, a sore throat can occur both under the influence of a pathogenic infection and as a result of nonspecific irritation (general hypothermia, drinking cold water).
Each previous angina, especially lacunar, follicular, can contribute to the development of conditions for relapse of inflammation, accompanied by otitis, sinusitis, and bronchitis.
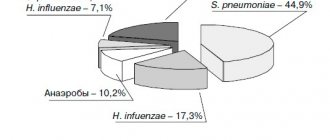
The main reason for this is the viruses that cause most respiratory tract infections, which can weaken the body's defenses. Viruses reduce the ability of macrophages and granulocytes to absorb infectious agents. In this way, the epithelium of the mucous membrane is damaged, which impedes the activity of the epithelial villi and leads to stagnation of mucus. Weakening of local protective mechanisms in many cases leads to infection of the upper and lower respiratory tract with bacteria Haemophilus influenzae, Streptococcus pneumoniae and Staphilococcus aureus, which are usually found in the oral cavity and trachea.
The chronic nature of infections is an indicator that the body's immune system is unable to cope with its functions. Constant but insufficient activation of nonspecific defense mechanisms often causes an inflammatory response, but this is not enough to suppress infectious agents.
Undoubtedly, the nature of the pathogenic flora plays a big role in the occurrence of a particular sore throat,
but the background against which it occurs also influences the clinical picture of the disease. Therefore, therapy should be prescribed and carried out taking into account all identified features in each case (time from the onset of angina, age of the patient, frequency of exacerbations, concomitant diseases: general and from the ENT organs, clinical manifestations, including in the oropharynx, nature of the flora , previous treatment, its effectiveness).
Currently, much attention is paid to the role of group A streptococcus in the occurrence of acute tonsillitis and pharyngitis, although b-hemolytic streptococcus still occupies a leading position among bacterial pathogens. Thus, it is believed that in late autumn and spring it is group A streptococci that cause disease in 40% of children and 10% of adults. Along with this, there is an opinion that in the vast majority of cases, the incidence of the lymphadenoid ring of the pharynx in children is determined by a viral infection, the features of which are a protracted and recurrent course, insufficient effectiveness of conservative anti-inflammatory measures, and a tendency to hyperplasia of the palatine and pharyngeal tonsils. Usually, the doctor diagnoses a sore throat “by eye,” only on the basis of clinical experience, and prescribes antibacterial treatment without taking into account the advisability of antiviral therapy. This not only slows down the healing process, but can also contribute to a decrease in the protective properties of the pharyngeal mucosa, since under the influence of antibiotics a-hemolytic streptococcus, which produces bactericin, a natural antibiotic, disappears. It is penicillins
to a greater extent than cephalosporins, they suppress this beneficial flora of the oropharynx and allow pathogenic streptococci to take its place on the epithelium of both the tonsils and the entire pharynx. Therefore, irrational (too early and without taking into account the flora) prescription of antibiotics leads to a decrease in antibacterial immunity and contributes to relapses of sore throat.
Based on the foregoing, the treatment tactics for patients with acute and chronic tonsillitis should consist of an accurate determination of the nature of the inflammatory process (acute, exacerbation of chronic or its sluggish course), justification of the type of inflammation (catarrhal, purulent, phlegmonous), determination of the type of pathogen (streptococcus, spirochete, bacillus , virus, mushrooms). To this it is necessary to add that all sore throats can be divided into two groups
- primary tonsillitis, as a self-developing acute inflammatory process in the tonsils, and secondary tonsillitis, as a symptom of the underlying disease, for example, in blood diseases. Only the correct diagnosis, taking into account the general condition of the patient, determines the choice of treatment tactics.
Acute sore throat
Catarrhal tonsillitis is the mildest form of tonsillitis, which affects the mucous membrane of the tonsils, sometimes in combination with inflammation of the mucous membrane of the oropharynx (mainly the area of its posterior wall), which gives a mixed picture of tonsillitis and pharyngitis. The main complaint is pain when swallowing food and saliva (with pharyngitis, swallowing saliva is more painful - “empty swallow”). The general condition is satisfactory, the disease lasts 6-7 days, body temperature is within the subfebrile range. Treatment involves the widespread use of physiotherapeutic procedures, frequent rinsing with warm disinfectant solutions, a gentle diet, plenty of warm drinks, and the use of salicylates. Prescribing antibiotics for identified catarrhal tonsillitis is considered inappropriate, especially without a clear idea of the causative agent
.
Due to the fact that even without the use of antibiotics all the symptoms of the disease disappear quite quickly (on the 2-3rd day), early prescription of antibiotics in cases of catarrhal tonsillitis leads to the fact that patients stop taking them without observing the course dose. In addition, complete suppression, for example, by phenoxymethylpenicillin, amoxicillin (the most commonly used antibiotics), group A streptococci (and with them a-hemolytic streptococcus, which resists pathogenic flora) leads to the fact that the person returning to the normal environment (home, school and etc.) the recovered patient again encounters this flora, but already capable of transmission, i.e. the possibility of relapse of inflammation of the tonsils increases - natural immunity is suppressed. When prescribing antibiotics in the first days of a sore throat, it is also necessary to remember about the possible resistance of a number of strains of streptococci to the prescribed antibiotics, for example, to macrolides such as erythromycin, clarithromycin. Therefore, the most rational prescription of antibiotics in the treatment of mild forms of sore throat is after laboratory confirmation of the sensitivity of the flora to them
. These provisions are classics, but in practice, for many reasons, they are not always observed, which will ultimately lead humanity to complete disarmament in the face of transforming strains of pathogens, including those that cause sore throat.
Severe forms of angina - lacunar, follicular
- require the prescription of antibiotics, but also in compliance with the rules for combating infection and taking into account all factors: diagnosis, flora, somatic status, the need to prevent complications, the full course of taking an antibiotic.
Chronic tonsillitis
What are the treatment tactics for recurrent tonsillitis, recurring 2 times a year or more often?
In these cases, the disease is defined as “chronic tonsillitis,” however, for it, the frequency of relapses of tonsillitis may not always be the determining factor, since the concept of “chronic tonsillitis” also includes other parameters that support the diagnosis. These are, first of all, complications clearly associated with it from other organs and systems of the body.
For a practicing physician, both a general practitioner and an otorhinolaryngologist, after making a diagnosis of “chronic tonsillitis,” it is important to choose the tactics of treating the patient and decide the question: in which cases is surgery indicated, and in which - conservative therapy.
We divide chronic tonsillitis into only two forms: chronic tonsillitis I and chronic tonsillitis II
. In the first case, conservative treatment is required, in the second - surgical treatment. The determining factor is the combination of local signs of tonsillitis with complications and features of the course.
Conservative treatment
Conservative treatment involves, first of all, systematic sanitation of the lacunae of the palatine tonsils while preserving the lymphoid tissue of the tonsils.
as an immune, to a certain extent, organ. Conservative treatment is indicated for uncomplicated chronic tonsillitis in cases where surgery can be delayed due to the general condition of the patient; if the patient has not previously received any therapy or is mainly concerned about local manifestations of tonsillitis - purulent plugs in the tonsils, bad breath, etc.
Among the methods of conservative treatment for chronic tonsillitis, the most effective are the following: washing the lacunae of the tonsils and removing purulent plugs and detritus (carrying out repeated courses using the “Tonsilor” apparatus, when simultaneously washing the lacunae of the tonsils with a disinfectant solution, suctioning out the pathological contents from them and ultrasonic exposure with low-frequency ultrasound on the tonsil tissue), as well as the introduction of various medications into the tonsil using phonophoresis. Physiotherapeutic treatment – KUF, “Yakhont-F”.
Both for sore throat and for accompanying pharyngitis, gargling, inhalation, and irrigation of the mucous membrane with disinfectant solutions are indicated.
Increasing the effectiveness of treatment can be achieved by prescribing immunostimulating plant extracts. Tonsilgon N
is a combination preparation of plant origin. The chamomile, marshmallow and horsetail components included in its composition stimulate the body's defense mechanisms by increasing the phagocytic activity of macrophages and granulocytes. The drug has anti-inflammatory, immunostimulating, anti-edematous and antiviral effects, accelerates the healing process and shortens the duration of the disease; can be used in the future to prevent relapse of the disease. There were no side effects when using the drug.
Tonsilgon N is available in two forms: in the form of drops for oral administration and in the form of tablets. For adults, the drug is prescribed 25 drops or 2 tablets 5-6 times a day, for children under 5 years old - 5-10 drops, for children 5-10 years old - 15 drops, for teenagers 10-16 years old - 20 drops 5-6 times a day. day. After the disappearance of acute manifestations of the disease, the frequency of taking Tonsilgon N is reduced to 3 times a day. The duration of basic therapy is 4-6 weeks.
The prescription of systemic antibiotic therapy for uncomplicated forms of tonsillitis of non-streptococcal etiology is not always justified. In this case, local prescription of antimicrobial drugs is more rational (from the first day of the disease until the results of a microbiological study are obtained). The main requirements for local antibacterial agents are a wide spectrum of antimicrobial action, including the most typical pathogens, lack of absorption from the mucous membrane, and low allergenicity.
Fusafyungin (Bioparox) has the most optimal combination of the above requirements.
- inhaled antibiotic with anti-inflammatory properties. The wide spectrum of antibacterial action of fusafyungin, the absence of resistant strains of microorganisms, and the drug’s own anti-inflammatory properties make it especially effective in the treatment of tonsillitis of non-streptococcal etiology. The most optimal is to use 4 doses of the drug every 4 hours for 10 days.
Other drugs used in the treatment of sore throats and exacerbations of chronic tonsillitis are:
Clarithromycin
- 1 tablet 2 times a day.
Coldrex
- 2 tablets 2 times a day. Children 6-12 years old - 1 tablet 4 times a day.
Tonsillotren
(lozenges) - 1 tablet every hour.
Treatment of tonsillitis such as agranulocytic and monocytic requires the participation of a hematologist.
Surgery
Indications for surgical intervention:
1. Frequent (2-4 times a year) sore throats, accompanied by high body temperature; pathological purulent detritus is noted in the lacunae; there is one or another complication associated with an exacerbation of the process (polyarthritis, pyelonephritis, etc.).
2. Frequent sore throats (2-4 times a year or more often), accompanied by high body temperature, local signs of chronic tonsillitis are observed, without identified complications. Frequently recurring sore throats indicate a weakened immune system.
3. As a result of one of the rare cases of tonsillitis (once every 5-7 years), some complication of the heart, joints, etc. developed. Local signs of chronic tonsillitis, adenitis of the lymph nodes in the area of the angle of the lower jaw.
4. There were no cases of tonsillitis, however, against the background of emerging diseases of the heart, joints, etc., local signs of chronic tonsillitis are revealed, mainly the accumulation of purulent contents in the lacunae of the tonsils.
Fuzafyungin –
Bioparox (trade name)
(Servier)
Combined preparation of herbal origin –
Tonsilgon N (trade name)
(BIONORICA Arzneimittel GmbH)
| Applications to the article |
| Chronic tonsillitis is a process of constant interaction between lymphoid tissue and the contents of the lacunae of the palatine tonsils. |
| After making a diagnosis of chronic tonsillitis, it is important to choose a treatment strategy for the patient and decide the question: in which cases is surgery indicated, and in which - conservative therapy. |
Features of antibiotic therapy in adults
Most often, an otorhinolaryngologist prescribes tetracycline or penicillin antibiotics. Acute pain goes away within 12 hours after the first dose of the drug. If the effect is not noticeable after 2-3 days, then the doctor prescribes a second-generation antibiotic from the group of cephalosporins or lincosamides. For tonsillitis caused by Staphylococcus aureus, third generation aminoglycosides are effective. Depending on the severity of the disease, the ENT doctor prescribes the drug in tablet form or by injection.
The course of treatment is 7-10 days. The doctor individually indicates the frequency of administration, dosage and name of the medication in accordance with the symptoms, age, and weight of the patient.
Antibiotics prevent the accumulation of purulent exudate in the lacunae of the tonsils and its further spread through the respiratory tract. For the treatment of adults, local antibiotics complement general therapy.
ANTIBACTERIAL THERAPY FOR STREPTOCOCCAL TONSILLITIS AND PHARINGITIS
L.S. Strachunsky, A.N. Bogomilsky
"Children's Doctor", 2000; 3:32-33
Terminology
In accordance with the International Classification of Diseases, X revision, “Streptococcal pharyngitis” (J02.0) and “Streptococcal tonsillitis” (J03.0) are distinguished. In foreign literature, the interchangeable terms “tonsillopharyngitis” and “pharyngitis” are widely used. In the future, the term streptococcal tonsillitis will be used, which means tonsillitis (sore throat) or pharyngitis caused by b-hemolytic streptococcus group A
(
Streptococcus pyogenes
,
GABHS
).
Etiology
Among the bacterial pathogens of acute tonsillitis and pharyngitis, GABHS is of greatest importance. Much less commonly, acute tonsillitis is caused by group C and G streptococci, Arcanobacterium haemolyticum
,
Neisseria gonorrhoeae
,
Corynebacterium diphtheria
(diphtheria), anaerobes and spirochetes (Simanovsky-Plaut-Vincent angina), extremely rarely - mycoplasma and chlamydia. The cause of viral acute pharyngitis and tonsillitis can be adenoviruses, rhinovirus, coronavirus, influenza and parainfluenza viruses, Epstein-Barr virus, Coxsackie A virus and others.
Epidemiology
GABHS is transmitted by airborne droplets. Sources of infection are patients and, less commonly, asymptomatic carriers. The likelihood of infection increases with a high degree of contamination and close contact. Streptococcal tonsillitis occurs more often in children aged 5-15 years, the highest incidence is observed in the winter-spring period. Viral pharyngitis occurs mainly in the winter months.
Sensitivity of GABHS
GABHS are highly sensitive to penicillins
and
cephalosporins
.
β-lactams remain the only class of antibiotics to which GABHS has not developed resistance. The main problem is resistance to macrolides
, which in Russia is 13-17%, while the M-resistance phenotype, characterized by resistance to macrolides and sensitivity to lincosamides (lincomycin and clindamycin), has become widespread.
Resistance to tetracyclines and sulfonamides
in Russia exceeds 60%.
In addition, tetracyclines, sulfonamides, co-trimoxazole do not provide eradication of GABHS and, therefore, they should not be used for the treatment of acute streptococcal tonsillitis caused even by
strains in vitro
Goals of antibiotic therapy
The goal of antibacterial therapy for acute streptococcal tonsillitis is the eradication of GABHS in the oropharynx, which leads not only to the elimination of symptoms of infection, but also prevents the development of early and late complications.
Indications for prescribing antibacterial therapy
Antibacterial therapy is justified only for known or suspected streptococcal etiology of acute tonsillitis. Unjustified antibacterial therapy contributes to the development of antibiotic resistance and can also be complicated by adverse drug reactions. Antibacterial therapy can be started before receiving the results of a bacteriological study if there are epidemiological and clinical data indicating a streptococcal etiology of acute tonsillitis.
Choice of antibiotics
Given the high sensitivity of GABHS to b-lactams, the first-line drug (of choice) for the treatment of acute streptococcal tonsillitis is penicillin
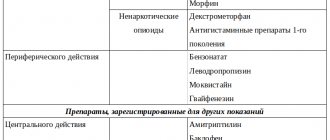
(phenoxymethylpenicillin). Oral cephalosporins are used less frequently. In patients allergic to b-lactams, macrolides or lincosamides should be used. Recommended drugs, doses and dosage regimens are presented in Table 1.
When carrying out antibacterial therapy for acute streptococcal tonsillitis, the following factors must be kept in mind:
- to eradicate GABHS, a 10-day course of antibacterial therapy is required (the exception is azithromycin, which is used for 5 days);
- early administration of antibiotics significantly reduces the duration and severity of symptoms of the disease;
- Repeated microbiological examination at the end of antibacterial therapy is indicated for children with a history of rheumatic fever, in the presence of streptococcal tonsillitis in organized groups, as well as in cases of high incidence of rheumatic fever in a given region.
Ineffectiveness of therapy for acute streptococcal tonsillitis
Inefficiency means:
- persistence of clinical symptoms of the disease for more than 72 hours after the start of antibacterial therapy,
- release of GABHS at the end of a course of antibiotic treatment.
Failures are most common in children treated with phenoxymethylpenicillin, which may be due to
- insufficient patient compliance in complying with the prescribed therapy regimen (premature discontinuation of the drug, reduction of the daily dose, etc.); in such situations, a single administration of benzathine benzylpenicillin
(Table 1), - the presence in the oropharynx of co-pathogens that produce b-lactamases, for example, during exacerbation of chronic tonsillitis; in such cases, a course of treatment with amoxicillin/clavulanate or other drugs from table 2
.
When the clinical symptoms of acute tonsillitis are eliminated and the release of GABHS continues, repeated courses of antibiotic therapy are advisable only if the patient or his family members have a history of rheumatic fever.
Mistakes in the treatment of acute streptococcal tonsillitis
- neglect of microbiological examination
- unreasonable preference for local treatment (rinsing, etc.) to the detriment of systemic antibiotic therapy
- underestimation of the clinical and microbiological effectiveness and safety of penicillins
- prescription of sulfonamides, co-trimoxazole, tetracyclines, fusidine, aminoglycosides
- reduction of the course of antibiotic therapy with clinical improvement
Differential diagnosis of recurrent streptococcal tonsillitis and carriage of GABHS
Recurrent streptococcal tonsillitis should be understood as multiple episodes of acute tonsillitis over several months with positive results of microbiological studies and/or rapid methods for diagnosing GABHS antigens.
Criteria for recurrent streptococcal tonsillitis:
- the presence of clinical and epidemiological data indicating streptococcal etiology;
- negative results of microbiological studies between episodes of the disease;
- increase in titers of antistreptococcal antibodies after each case of tonsillitis.
Antibiotics recommended for use in recurrent streptococcal tonsillitis are given in Table 2. On average, about 20% of school-age children are carriers of GABHS in the spring-winter period. Carriers are characterized by the absence of immunological reactions to the microorganism. Considering the low risk of developing purulent and non-purulent complications, as well as the insignificant role in the spread of GABHS, chronic carriers, as a rule, do not need antibacterial therapy.
Table 1.
Doses and regimen of antibiotics for acute streptococcal tonsillitis.
| phenoxymethylpenicillin1 | 0.375 g in 2 divided doses (<25 kg); 750 mg in 2 divided doses (>25 kg) | 1 hour before meals | 10 |
| benzathine benzylpenicillin2 | 600 thousand units intramuscularly (<25 kg) 1.2 million units intramuscularly (>25 kg); | — | once |
| amoxicillin | 0.375 g in 3 divided doses (<25 kg) 750 mg in 3 divided doses (>25 kg) | regardless | 10 |
| Cephalosporins | |||
| cefadroxil | 30 mg/kg in 1 dose | regardless | 10 |
| For b-lactam intolerance | |||
| Macrolides | |||
| erythromycin3 | 40 mg/kg in 3 divided doses | 1 hour before meals | 10 |
| azithromycin | 12 mg/kg in 1 dose | 1 hour before meals | 5 |
| clarithromycin | 15 mg/kg in 2 divided doses | regardless | 10 |
| midecamycin | 50 mg/kg in 2 divided doses | before meals | 10 |
| roxithromycin | 5 mg/kg in 2 divided doses | 15 minutes before meals | 10 |
| spiramycin | 3 million units in 2 doses | regardless | 10 |
| For intolerance to macrolides and b-lactams | |||
| Lincosamides | |||
| lincomycin | 30 mg/kg in 3 divided doses | 1-2 hours before meals | 10 |
| clindamycin | 20 mg/kg in 3 divided doses | drink plenty of water | 10 |
Notes:
- It is recommended mainly for the treatment of children, given the presence of the dosage form in the form of a suspension.
- It is advisable to prescribe for:
- questionable compliance (diligence) of the patient with regard to oral administration of antibiotics;
- a history of rheumatic fever in the child or immediate family;
- unfavorable social and living conditions;
- outbreaks of streptococcal infection in preschool institutions, schools, boarding schools, colleges, etc.
- Erythromycin is characterized by the most frequent development of adverse reactions, especially from the gastrointestinal tract, compared to other macrolides.
Table 2.
Antibacterial therapy for recurrent streptococcal tonsillitis, as well as when natural penicillins are ineffective.
| at the beginning of a meal | 10 | ||
| Cefuroxime axetil | 20 mg/kg in 2 divided doses | immediately after eating | 10 |
| Clindamycin | 20 mg/kg in 3 divided doses | drink plenty of water | 10 |
| Lincomycin | 30 mg/kg in 3 divided doses | 1-2 hours before meals | 10 |
*Calculate based on amoxicillin
Literature
- Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH Diagnosis and management of group A streptococcal pharyngitis: a practical guideline. Clin Infect Dis 1997;25:574-83.
- Belov B.S., Nasonova V.A., Grishaeva T.P. Rheumatological aspects of acute streptococcal tonsillitis and modern approaches to its antibacterial therapy. Clinical Antimicrobial Chemotherapy 2000;2:4-10.
- Nasonova V.A., Belov B.S., Strachunsky L.S. and others. Antibacterial therapy of streptococcal tonsillitis and pharyngitis. Clinical Microbiology and Antimicrobial Chemotherapy 1999;1:78-82.
| © 2000-2009 NIIAH SGMA | ||