January 20, 2021
Most often in medical practice, pathology caused by type 1 occurs. This is the so-called labial herpes (rash on the lips)
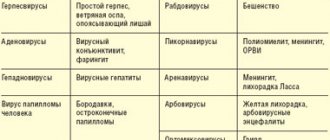
Herpetic infection is a chronic disease; once HSV enters the body, it remains in it, living in the nerve endings, for life. The herpes virus belongs to the Herpeveridae family, includes 8 types and three subfamilies: the Alphaherpesvirinae subfamily consists of herpes simplex viruses 1, 2 and varicella zoster virus; the subfamily Gammaherpesvirinae includes Epstein-Barr virus, HHV-VI, HHV-VII, HHV-VIII; the subfamily Bethaherpesvirinae constitutes type V, the Cytomegalovirus virus.
Most often in medical practice, pathology caused by type 1 occurs. This is the so-called labial herpes (rash on the lips). Its peculiarity lies in its chronic course; with adequate treatment of a patient with symptoms of labial herpes, it is possible to achieve stable remission. However, at this time the virus “hides” in the nerve nodes (ganglia), where it can be stored in an inactive form as long as necessary, and when “favorable” conditions arise, it is activated again.
The herpes simplex virus is present in the body of 95% of people, entering the body in early childhood: at 3 - 4 years, when the antibodies against the herpes virus transmitted to the baby by the mother are depleted. WHO estimates that in 2021, about 3.7 billion people under 50 years of age, or 67% of the world's population, were infected with HSV-1 (have oral or genital herpes). Prevalence rates were estimated to be highest in Africa (88%) and lowest in the Americas (45%). Most HSV-1 infections were oral infections.
Recurrent herpetic rashes occur due to prolonged exposure to the sun, febrile illness, physical or emotional stress, immunosuppression, and unknown causes. In general, recurrent rashes are less severe and less common.
Severe cases of the herpes virus include encephalitis, meningitis, neonatal herpes, and in immunocompromised patients, disseminated infection. Mucocutaneous infections cause clusters of small, painful blisters on an erythematous base.
Herpes is transmitted in the following ways: contact - physical contact with an infected person; airborne - through saliva particles when sneezing and coughing; sexually – genital herpes is most often transmitted this way. During unprotected sexual intercourse; household - through shared items (towels, dishes, bed linen); vertical - from a pregnant woman to a child during pregnancy or childbirth.
Symptoms of the herpes virus
Herpes simplex virus 1 causes oral and, less commonly, genital herpes. Such herpes is characterized by the formation of small blisters in the amount of one to ten pieces, they are located in groups, and inside are filled with serous exudate. Gradually, the blisters open, and in their place crusts form, which disappear on the 6th day of the disease.
After this, subtle pigmentation remains, which goes away independently and without a trace at the end of recovery. Typical clinical picture: the formation of painful blisters filled with serous fluid in the lip area; itching and burning in places where skin elements appear; loss of appetite, increase in body temperature (rare). With adequate treatment, signs of the disease can disappear after 3-4 days.
The formation of blisters is accompanied by severe itching, pain and burning at the site of the pathological process. Systemically, fever and enlarged lymph nodes may occur. With oral herpes, the blisters are localized around the mouth and wings of the nose. The genital form of the disease manifests itself with characteristic symptoms on the mucous membrane of the genital organs.
A typical sign of genital herpes is the appearance of small (2-5 mm), fluid-filled blisters on the genitals, buttocks and anus. The rash is accompanied by itching and/or pain. The rash can be located in the vagina, on the cervix, or in the rectum. Within a few days, the blisters burst, turning into painful sores. After 1-2 weeks, the ulcers become covered with crusts and heal. Other manifestations: pain in the groin or inner thighs, painful urination, vaginal discharge in women or from the urethra in men.
Primary infection lasts about 3 weeks with pronounced manifestations. After the initial episode of the disease, exacerbations occur several times (usually 4–5) during the year. In the future, the number of exacerbations decreases, the severity of manifestations decreases.
What is the best way to treat herpes: effective ointments and tablets for herpes infection
The most well-known antiherpetic drug is acyclovir. Its effectiveness for the treatment of types 1, 2, 3 and 4 of herpes has been proven in clinical studies. Acyclovir is recommended by the World Health Organization to combat HSV.
Acyclovir stops the reproduction of the pathogen and inhibits its activity. It is mainly used in the form of a cream, which is applied several times a day to the affected area of the skin. This drug also exists in tablet form. The rules of admission in each individual case should be discussed with the attending physician.
The drug Penciclovir is considered no less effective. It is also recommended by WHO, as this medication has successfully passed numerous clinical trials. It suppresses the activity of herpes virus types 1 and 2, and is also effective against its strains. Penciclovir can be used in patients who are resistant to acyclovir.
However, Valaciclovir is considered the most effective drug against herpes infection. It is more effective than the previous two medications. In the human body, under the influence of enzymes, valacyclovir is converted into acyclovir.
In almost all antiherpetic drugs, the main active ingredient is acyclovir, penciclovir or valacyclovir.
Drugs for the treatment of oral herpes
There are a wide variety of antiviral medications to treat the symptoms of this disease, which are available in dosage forms for topical use. They begin to act faster than drugs in tablet forms and act directly on the site of infection.
The best creams and ointments for type 1 herpes:
- Pen-Gerpevir;
- Atsik;
- Lipster;
- Gerpevir;
- Zovirax;
- Acyclostad;
- Agerp.
Acyclovir, penciclovir and valacyclovir are also included in medications that must be taken orally, that is, through the mouth.
They are included in the following herpes tablets:
- Gropivirine;
- Valavir;
- Acyclovir-Darnitsa;
- Atsik;
- Lipster.
Drugs for the treatment of genital herpes
Some of the medications listed above are suitable to combat it, but medical experts advise using drugs that contain valacyclovir. This is due to the fact that HSV type 2 has a greater number of negative symptoms and can cause complications, and valacyclovir is stronger than penciclovir and acyclovir.
Effective drugs to combat HSV type 2:
- Proteflazid drops, Proteflazid suppositories;
- Valavir tablets;
- Roller tablets;
- Lipster tablets;
- Valaciclovir-Hetero tablets.
In addition, to treat the viral infection in question, the following auxiliary agents are used:
1. Immunomodulators . They help strengthen the immune system and enhance protective responses against viruses.
Examples of these tools:
- Cycloferon;
- Anaferon.
2. Antiseptics . They are used to prevent re-infections. Antiseptics are used to treat infection sites.
The most famous medicines:
- Chlorhexedine;
- Miramistin.
3. Non-steroidal anti-inflammatory drugs (NSAIDs) . Herpes infection is accompanied by inflammatory processes that help suppress NSAIDs.
Examples of these drugs:
- Ibuprofen;
- Nimesil.
4. Analgesics-antipyretics . With genital herpes, fever may occur. It can be brought down with the help of the most famous analgesic-antipyretic paracetamol.
5. Antihistamines . During HSV, a person experiences itching sensations at the sites of infection. Ulcers and blisters are very itchy, but they should never be scratched, otherwise scars will remain in their place. Antihistamines are used to reduce itching.
Popular products of this group.
- Erius;
- Claritin;
- Eden.
The doctor must decide which remedy to choose for the treatment of herpes simplex virus and which auxiliary medications to take in each individual case. And to prevent the occurrence of the disease or its relapse, you can carry out simple prevention.
Diagnostics
Diagnosis includes visual inspection of the patient's clinical manifestations if an exacerbation is typical. The diagnosis of HSV infection is often based on clinically characteristic lesions. Laboratory confirmation may be necessary if the infection is severe, the patient is immunocompromised, or the patient is pregnant, and the lesions are atypical. Depending on the severity of the clinical picture, a number of necessary auxiliary diagnostic procedures are performed:
- a set of standard laboratory tests (general blood test, urine test, etc.);
- serological tests (ELISA) to detect antibodies to a specific type of virus in the patient’s blood;
- PCR analysis is a highly informative diagnostic method that allows you to detect the presence of a virus in the body with up to 99% accuracy.
Herpes simplex virus must be distinguished from herpes zoster, which rarely recurs and usually causes more severe pain and larger lesions that are distributed along the dermatome and usually do not cross the midline. It should also be noted that collections of vesicles or ulcers on an erythematous basis are uncommon in genital lesions other than those caused by HSV infection.
Treatment and prevention of herpes
The main goal of herpes treatment is to relieve symptoms of the disease and reduce the frequency of relapses. To eliminate the symptoms of oral and genital herpes, ointments and tablets that have a specific antiviral effect are used. The most effective medications for people infected with HSV are antiviral drugs such as acyclovir, famciclovir and valacyclovir. Both tablets and injections, as well as ointments and topical creams are used. To prevent relapses, immunostimulating drugs are prescribed to restore and maintain immunity. They help relieve symptoms and reduce the frequency of their occurrence, but do not lead to a complete cure. It is impossible to completely recover from herpes - the virus remains in the human body for life after the initial infection.
At first glance, it may seem that herpes virus infection is quite harmless. But in fact, it can lead to serious complications:
- In people with weakened immune systems (for example, HIV-infected people), herpes is more severe and often recurs. In rare cases, HSV-1 causes encephalitis (inflammation in the brain), keratitis (inflammation of the cornea of the eye). Herpetic encephalitis leads to death in 30% of cases; after treatment, it leaves serious consequences in the form of persistent paralysis and paresis, and dementia.
- HSV-2 infection increases the risk of human immunodeficiency virus infection.
- In 1 out of 10,000 cases, a child becomes infected during childbirth, and neonatal herpes develops, which leads to severe neurological disorders and death of the newborn. The risks are especially high if the expectant mother becomes infected late in pregnancy.
This is why disease prevention is so important. HSV-1 is most contagious when oral herpes symptoms appear, but it can also be transmitted when no symptoms are felt or observed. Persons with active symptoms of oral herpes should avoid oral contact with other people and sharing household items (dishes, towels, etc.). Patients are also advised to abstain from oral sex to prevent herpes from spreading to the genitals of their sexual partner. People with symptoms of genital herpes should avoid having sex while they have symptoms.
Back to articles
Principles of treatment of herpes simplex
WITH
Among viral diseases, herpes infection occupies one of the leading places, which is determined by the widespread spread
of the herpes simplex virus (HSV)
, more than 90% of its infection of the human population, the lifelong persistence of the virus in the body, the polymorphism of the clinical manifestations of the disease, and its resistance to existing treatment methods.
Unfortunately, modern medicine does not have treatment methods that can eliminate HSV from the human body. Therefore, the goal of therapeutic measures is: a) suppression of HSV reproduction during an exacerbation, b) formation of an adequate immune response and its long-term preservation in order to block the reactivation of HSV in areas of persistence, c) prevention of the development or restoration of those disorders that are caused by HSV activation in the body.
Currently, there are two main directions in the treatment of herpes simplex:
1) use of antiviral chemotherapy
, the main place in which is given to acyclic nucleosides and, first of all, acyclovir;
2) complex treatment method
, including immunotherapy (specific and nonspecific) in combination with antiviral therapy.
Creation of acyclovir
(ACV) opened a new stage in the treatment of herpes. In many countries around the world, the industrial production of acyclovir-containing drugs (ACV drugs) has been established.
Antiviral chemotherapy
Etiopathogenetic therapy is based on the ability of chemotherapeutic drugs to selectively disrupt the process of interaction between HSV and cells, to be included in the development cycle of only HSV at the stages of viral DNA synthesis and assembly of viral particles, inhibiting their reproduction, which ultimately leads to a virusostatic effect. Chemotherapy takes a leading place in acute herpetic infection, which occurs with damage to the central nervous system and other systems and organs, as well as in herpes of newborns. Antiviral drugs are of great importance in the treatment of recurrent forms of herpes simplex with damage to the skin and mucous membranes.
Etiopathogenetic therapy
Acyclovir
- a synthetic acyclic analogue of deoxyguanosine, a natural component of DNA, and today remains the standard of antiherpetic treatment. Acyclovir penetrates predominantly into a cell infected with a virus, where, under the influence of a virus-specific thymidine kinase, it transforms into an active form as a result of phosphorylation with the formation of mono-, di- and triphosphate. Acyclovir has found its use in the treatment of all forms of herpes infection. Pronounced antiherpetic activity, low toxicity, and the presence of several dosage forms (ointment, tablets, cream, suspension, solution for intravenous administration) allow the drug to be widely and effectively used in medical practice.
It has been established that in 5–7% of patients suffering from recurrent herpes (HR)
, during treatment, resistance to acyclovir develops or it initially does not have a therapeutic effect. The mechanism of resistance is associated with a decrease in the activity or absence of viral thymidine kinase, damage to the substrate specificity of this enzyme and the appearance of mutations in the DNA polymerase gene.
valacyclovir, has been developed based on acyclovir.
, which is the L-valine ester of acyclovir. The advantage of valacyclovir in comparison with acyclovir is that its oral administration creates concentrations of acyclovir in the blood serum and other internal media that are equivalent to those achieved only with intravenous administration of acyclovir. This is what allows the patient to reduce the number of doses of the drug during a relapse to 2 times a day (as opposed to acyclovir, which is taken 5 times a day) and take valacyclovir once a day for suppressive therapy.
Famciclovir
is transformed in the body into an active antiviral compound - penciclovir, effective against HSV-1, HSV-2 and other herpes viruses. Penciclovir reaches HSV-infected cells, where it is converted to triphosphate by the action of viral thymidine kinase.
Acyclovir, val acyclovir and famciclovir are “first aid” drugs for any form of herpes. However, ACV drugs exert their indirect virusostatic effect by interacting with the thymidine kinase of herpes viruses, which to a certain extent limits the universality of their action on HSV strains with genetically altered viral thymidine kinase activity. Therefore, the list of specific antiherpetic drugs has been supplemented with foscarnet.
Foscarnet
is a competitive inhibitor of pyrophosphate and has a wide spectrum of antiviral activity, inhibiting the DNA polymerase of herpes viruses. However, it should be noted that this phosphorus-containing drug is more toxic than acyclovir, which may limit its use.
There are a number of drugs with different mechanisms of antiviral action that can be used for herpes: brivudine, ribamidil, metisazone. And yet they are significantly inferior to acyclovir in therapeutic effectiveness.
Immunotherapy for herpes simplex
Impaired immune response is the most important link in the pathogenesis of herpes simplex. As a rule, the disease occurs against the background of suppressed immune reactions: there is a decrease in the total number of T- and B-cells, a change in their functional activity, disturbances in the macrophage component of immunity, in the interferon system. Correction of violations of nonspecific and specific immunity is one of the directions in the complex therapy of herpes simplex.
Nonspecific immunotherapy
includes the use of:
1) immunoglobulin;
2) interferons and interferon inducers;
3) drugs that stimulate the T- and B-links of cellular immunity and phagocytosis.
Mechanism of action of immunoglobulins
For a long time, herpes was explained by a replacement effect against the background of the inherent failure of humoral immunity for this disease. In recent years, it has been found that immunoglobulin preparations also have immunomodulatory and antitoxic effects and activate opson-phagocytic reactions.
Normal human immunoglobulin is used to treat recurrent herpes. The drug contains a sufficient amount of specific antiherpetic antibodies to achieve a therapeutic effect, which is explained by the almost 100% carriage of HSV in the population.
To treat severe forms of herpetic infection (central nervous system lesions, neonatal herpes, primary herpes in pregnant women), human immunoglobulin with a high content of antiherpetic antibodies (Sandoglobulin) or domestic immunoglobulin for intravenous administration can be used.
Wide spectrum of antiviral activity, absence of interferon-resistant (IF)
virus strains predetermined the prospect of using interferon as a means of etiopathogenetic therapy of herpes simplex. Interferons are factors of natural immunity, produced by cells in response to the influence of viruses, bacteria, foreign antigens and cause activation of effector immune cells involved in the reactions of elimination of infectious agents from the body. According to modern concepts, interferons, along with antiviral activity, have antiproliferative and immunoregulatory effects. IF increases nonspecific cell resistance (stimulates phagocytosis, increases the activity of natural killer cells), and the level of interferon formation can be used to judge the general immunological reactivity of the body.
Commercial series of human leukocyte interferon (HLI) produced by the domestic industry are species-specific and are quickly eliminated from the body (with intravenous administration after 4–6 hours, with intramuscular administration - after 20 hours). The high cost and complexity of industrial production of CLI to a certain extent limit its use. In practical healthcare, CLI is currently used in several dosage forms: 1) nasal drops; 2) PLI for injection - a mixture of interferons-a produced by leukocytes of clinically healthy donors, administered intramuscularly, subcutaneously, intravenously; the activity of 1 dose of the drug is 100,000 IU, 500,000 IU, 1000,000 IU; 3) leukinferon (for injection) – a natural complex preparation containing interferon-a and cytokines (1 dose – 10,000 IU); 4) interlock (for injection), 1.0 ml – 50,000 IU; 5) CLI in rectal suppositories (1 suppository contains 40,000 IU of antiviral activity).
The idea of interferon therapy found its development in the creation of genetically engineered interferons and in the use of endogenous interferon inducers.
For the treatment of various forms of recurrent herpes, domestic rectal suppositories Viferon, which contain recombinant a2-interferon, are used. A combined drug, kipferon, has been created (consists of immunoglobulins and recombinant a2-interferon) in the form of suppositories for rectal and vaginal administration.
With the help of interferon preparations (natural or genetically engineered), replacement therapy is carried out, as a result of which the production of the patient’s own endogenous IF can be blocked. This must be taken into account when prescribing long-term (more than 2 weeks) courses of IF therapy, especially genetically engineered forms (Reaferon, Viferon). In cases of long-term administration of IF to patients, they should be discontinued gradually, reducing the dose to 3, then 2 times a week, followed by complete discontinuation of the drug.
The ability to induce the production of endogenous IF
has a large group of natural and synthetic compounds: levamisole, dibazole, vitamin B12, pyrogenal, prodigiosan, which are the drugs of choice for the treatment of herpes.
A synthetic interferon inducer, the domestic drug Poludan (poly A:U), which has been used since the 1970s, has a pronounced therapeutic and prophylactic effect in recurrent herpes. and is still widely used in the form of eye drops and subconjunctival injections for the treatment of ophthalmoherpes and other viral eye diseases. Convincing clinical data have been obtained on the high effectiveness of poludan for the treatment of recurrent herpes affecting the skin and mucous membranes. If smooth skin is affected by recurrent herpes of the buttocks and thighs, the lesion is injected with poludan (200–400 mcg per lesion). Poludan has a general immunostimulating effect, which makes it possible to use it in secondary immunodeficiency conditions caused not only by herpesvirus infections.
IF inductors used per os
, which allows patients to independently carry out preventive and anti-relapse treatment courses recommended by the doctor.
Amiksin, alpizarin, flocazide, arbidol, being inducers of IF, stimulate the production of endogenous IF in the patient's body. This explains the positive therapeutic effect of the listed drugs in many viral diseases (recurrent herpes, influenza, adenovirus infection), which makes it possible to recommend them in the complex treatment of herpesvirus infections, especially in patients suffering from frequent colds and acute respiratory viral infections.
To stimulate the T- and B-links of cellular immunity in patients with recurrent herpes, the drugs taktivin, thymalin, thymogen, myelopid, etc. are successfully used. Treatment must be carried out under the control of an immunogram.
Specific immunotherapy
consists of using a domestic herpetic vaccine (polyvalent, tissue, killed). The therapeutic effect of the vaccine is associated with the stimulation of specific reactions of antiviral immunity, restoration of the functional activity of immunocompetent cells and specific desensitization of the body.
Comprehensive treatment of herpes simplex
Considering the peculiarities of the pathogenesis of herpes simplex, the most appropriate way to achieve a therapeutic effect is to use drugs with different mechanisms of action. Thus, the use of chemotherapy drugs with different mechanisms of antiviral action prevents the emergence of resistant strains of HSV; the use of interferons and their inducers in combination with a herpetic vaccine and immunomodulators makes it possible to comprehensively address the issues of herpes simplex therapy.
Treatment regimens for recurrent herpes can be different, which is determined by the clinical manifestations of HSV infection, the patient’s immune status and the doctor’s choice.
Treatment of recurrent herpes
The most pronounced therapeutic effect is achieved with an integrated approach to therapy
, which includes several stages:
1) antiviral therapy in combination with immunocorrection and interferon therapy, taking into account the data of an immunological examination and the study of interferon status;
2) anti-relapse treatment with a herpes vaccine in combination with immunomodulators and symptomatic use of antiviral drugs;
3) the use of adaptogens, repeated courses of vaccine therapy (re-vaccination), symptomatic use of antiviral drugs.
The duration of observation and the intensity of therapy for patients depend on the severity of herpetic infection, which is determined by the frequency of relapses, the presence or absence of a prodromal period, intoxication, pain, and the involvement of various systems and organs in the infectious process (Table 1).
The effectiveness of the therapy is assessed by reducing the duration and frequency of relapses, as well as the intensity of general symptoms of the disease.
The main remedy for stopping relapses
herpes simplex are ACV drugs (acyclovir, val acyclovir and famciclovir). There are two fundamentally different approaches to prescribing antiherpetic chemotherapy drugs:
a) episodic treatment - taking ACV drugs at the time of relapse, in therapeutic doses, observing the frequency and duration of drug administration.
b) suppressive therapy - long-term, long-term, constant use of ACV drugs without relapse in lower doses.
For episodic treatment during a relapse, patients are recommended to include the drug IF or an oral interferon inducer in the course of treatment in order to strengthen antiviral immunity and prevent possible complications of a viral infection (for example, Viferon and Arbidol).
Treatment of mild forms of RG
is often limited to prescribing ACV-drug in ointment and tablet forms and one or two courses of amixin or alpizarin, multivitamins during a relapse. Considering that the majority of patients with RG have impaired interferon status, it is advisable for them to prescribe an IF inducer or viferon, kipferon during a relapse.
If there is no effect from several repeated courses of nonspecific immunotherapy, vaccine therapy is indicated for patients with a mild form of herpes. The methods of choice are: repeated courses of immunoglobulin (2-3 per year), long-term (up to 1.5 months) administration of amixin or alpizarin in combination with antioxidants, course administration of dibazole with eleutherococcus, multivitamins, prodigiosan, etc.
In the course of treatment of patients suffering from moderate and severe forms
RG, it is necessary to include a herpes vaccine. It is advisable to combine vaccine therapy with immunomodulators (poludanum, myelopid), which increase its immunogenicity. In this case, the antiherpetic vaccine is prescribed after a course of immunomodulator.
Treatment of patients with frequent relapses
(moderate “b” and severe forms) begin with nonspecific immunotherapy, including immunoglobulin, stimulators of T- and B-cell immunity (under the control of an immunogram). Against the background of immunotherapy, patients note an improvement in general well-being, increased performance and a decrease in the frequency and severity of relapses. At the end of nonspecific immunotherapy, patients are prescribed a herpetic vaccine.
Patients with continuously recurring forms of herpes
Vaccination is indicated against the background of a 3-4 month course of suppressive therapy with ACV drugs.
Every 6–8 months, patients suffering from RH need to undergo revaccination. In the intervals between revaccinations, patients in these groups (according to indications) can be prescribed maintenance courses of nonspecific immunotherapy.
Features of local treatment for RG
The problem of local treatment of RH of the skin and mucous membranes was solved with the advent of acyclovir in the form of cream and ointment. With timely use of the drug (at the first signs of relapse or when prodromal local phenomena appear), the relapse is stopped in 1–2 days. Patients with intolerance to ACV or with low effectiveness are prescribed creams, ointments, gels, lotions, and sprays with other antiherpetic drugs.
External administration of antiviral drugs for herpes of the skin and mucous membranes is necessary to reduce clinical manifestations in the lesion, accelerate epithelization and reduce the duration of virus isolation from the lesion.
Without local treatment for herpetic lesions of the genitourinary system in men
It is almost impossible to achieve a significant therapeutic effect. To treat herpetic urethritis, you can use the liniment of cycloferon or poludan, which is injected into the urethra in the form of instillations. For herpetic proctitis, a pronounced therapeutic effect is observed when patients are prescribed Poludan solution in the form of microenemas, as well as with rectal administration of Kipferon suppositories.
Along with medicinal local treatment, men with chronic herpetic diseases of the pelvic organs undergo traditional local manipulations: bougienage of the urethra, massage of the prostate, followed by total instillation of Poludanum solution or Cycloferon liniment. To achieve a more pronounced anti-inflammatory, absorbable and analgesic effect, such patients should include low-frequency laser therapy in the course of treatment.
Local treatment of urethritis and proctitis in women
carried out in the same way as for men. For the treatment of herpetic cervicitis and colpitis, Kipferon suppositories (vaginally) and Cycloferon liniment are used.
However, even with such an integrated approach to the treatment of GC, there are cases with low therapeutic efficacy
, manifested:
1) torpidity to the therapy, when despite the ongoing antiviral and immunocorrective treatment (including vaccine therapy), the frequency and intensity of relapses of herpes in patients remains the same;
2) persistence of symptoms of persistent impairment of general well-being (weakness, malaise, psychoasthenia) and decreased ability to work against the background of a pronounced improvement in the clinical course of RG achieved as a result of treatment (reduction in the frequency and duration of relapses).
Virological examination of patients with low therapeutic efficacy often reveals an association of two herpes viruses: HSV and CMV
, which requires correction in the therapy.
Conclusion
Modern international standards for the management of patients with herpesvirus infections determine the following requirements for doctors:
1. The minimum standard for monitoring a patient is to establish an accurate diagnosis. To do this, it is necessary to examine the patient, take a smear from the site of skin or mucous membrane lesions and conduct a virological examination.
2. The patient should receive reasoned advice on a healthy lifestyle and recommendations on antiviral therapy. The doctor must be aware that the patient needs complete information about the disease.
3. As with other STDs, for genital herpes it is necessary to obtain biological materials for the diagnosis of other genital infections, and this should be discussed jointly between the doctor and the patient.
4. The doctor’s responsibility is:
- diagnosing a patient with clinical symptoms of herpes;
- familiarizing the patient, based on the diagnosis, with the prognosis of the disease, the risk of transmission of infection and the possibilities of antiherpetic treatment;
- involving the patient in deciding on the choice of method (episodic or preventive) and treatment program for recurrent forms of genital herpes.
| Historical reference . , symptomatic therapy occupied an important place in herpetic lesions of the skin and mucous membranes . Treatment consisted of local use of antiseptic drugs to help disinfect and limit the spread of foci of infection, reducing subjective sensations. During the 60-80s. In the 20th century, Soviet scientists created a number of antiviral drugs with different mechanisms of action, allowing for etiotropic therapy . The most numerous group of antiviral drugs includes nucleoside analogues, similar in structure to intermediate products of DNA and RNA biosynthesis. The mechanism of the antiviral action of purine and pyrimidine analogues is that they are included in the viral DNA molecule, replacing thymidine, and this leads to the formation of defective viral nucleic acid, devoid of infectious properties. A pronounced inhibitory effect against DNA-containing viruses, including HSV, is exerted by a group of chemical compounds - halogen derivatives of deoxyuridine: 5-bromo-2′-deoxyuridine (IDU), 5-bromouridine, 5-fluorouracil, cytosine arabinoside, adenine arabinoside (vidorabine , Ara-A). Ribavirin, which exhibits antiviral activity against 20 RNA and DNA viruses, was used for systemic therapy. Clinically, the most studied of these drugs are IDU and AZUR (6-azauridine). They have found application in ophthalmology, mainly for superficial forms of keratitis. However, drugs in this group do not have the ability to cross the blood-brain barrier, which did not allow their use in cases of HSV lesions of the central nervous system. For external use for herpetic lesions of the skin and mucous membranes, domestic scientists have created: oxolin, florenal, tebrofen, bonaftone, riodoxol, adimal, gossypol, megosin, etc. |