Pharmacological properties of the drug Velaxin
Venlafaxine ((±)-1-[dimethylamino-1-(methoxy-phenyl)-ethyl] cyclohexanol hydrochloride) is an antidepressant with a new chemical structure that cannot be classified as tricyclic, tetracyclic or other known antidepressants. It is a racemic mixture of two active enantiomers. The mechanism of the antidepressant effect of venlafaxine is associated with increased neurotransmitter activity of the central nervous system. Venlafaxine and its main metabolite O-desmethyl venlafaxine (ODV) are potent inhibitors of neuronal reuptake of serotonin and norepinephrine, and also inhibit dopamine reuptake. In addition, both single and chronic administration of venlafaxine and EDV attenuates β-adrenergic reactions. They are equally effective in influencing the reuptake of neurotransmitters. Venlafaxine does not inhibit MAO activity. Venlafaxine has no affinity for opiate, benzodiazepine, phencyclidine, or N-methyl-d-aspartate (NMDA) receptors; it also does not affect the release of norepinephrine from brain tissue. With repeated use of the drug, equilibrium concentrations of venlafaxine and its only active metabolite in the blood plasma are achieved within 3 days. Venlafaxine and EDV have linear pharmacokinetics with total daily doses ranging from 75 to 450 mg. Absorption of venlafaxine after taking a single dose of the drug orally is almost 92%, absolute bioavailability is about 45%. After administration of Velaxin extended-release capsules, maximum plasma concentrations of venlafaxine and its active metabolite EDV are achieved within approximately 6 and 8 hours, respectively. The rate of absorption of venlafaxine released from extended-release capsules is less than the rate of its elimination. Therefore, the average half-life of venlafaxine from the body after taking Velaxin (15±6 hours) is actually the half-life in the absorption phase, and not the half-life in the distribution phase (5±2 hours), which is observed after the use of tablets. After administration of venlafaxine in equivalent doses in tablet or extended-release capsule form, venlafaxine AUC exposure and EDV were similar in both dosage forms, and their plasma concentrations were slightly lower after administration of venlafaxine in capsule form. Thus, extended-release capsules provide slower absorption but the same extent of absorption (i.e., AUC) as Velaxin tablets. Venlafaxine is extensively metabolized during the initial passage through the liver, mainly with the participation of CYP 2D6, with the formation of the main metabolite EDV. It is also metabolized to N-desmethyl venlafaxine and some other metabolites with the participation of CYP 3A3/4. Venlafaxine and its metabolites are excreted mainly by the kidneys. Approximately 78% of the administered dose of venlafaxine is determined in the urine over 48 hours in the form of unchanged venlafaxine, unconjugated EDV, conjugated EDV or other metabolites. In case of renal and hepatic insufficiency, the half-life of venlafaxine and its active metabolite EDV increases. Taking the drug with food does not affect the absorption of venlafaxine and the further formation of EDV. The age and gender of the patient do not affect the pharmacokinetics of the drug. The drug does not accumulate in the body. Velaxin extended-release capsules contain microspheres that, when entering the gastrointestinal tract, slowly release the active component. The insoluble part of these microspheres is excreted in the feces.
Psychiatry Psychiatry and psychopharmacotherapy named after. P.B. Gannushkina No. 09 2003
Introduction
Since the introduction into clinical practice of the first thymoanaleptics—tricyclic antidepressants (TCAs) and nonselective, irreversible MAO inhibitors (MAOIs), the constant search for new drugs for the treatment of depression continues. Today, there is a wide variety of thymoanaleptics that differ in chemical structure and mechanisms of action, which makes it very difficult for a doctor to choose the most adequate antidepressant for the treatment of a specific depressive condition. In accordance with the recommendation issued by the British Association for Psychopharmacology in 1993, the following factors are essential when choosing an antidepressant: severity of side effects, effectiveness, risk of overdose, price. Taking into account these 4 factors is complicated by their significant differences in individual drugs, especially in the traditionally used TCAs and MAOIs, as well as in new groups of antidepressants that have appeared in recent years - selective serotonin reuptake inhibitors (SSRIs) and reversible selective MAO type A inhibitors (RSMAs). This primarily relates to the significant difference in the occurrence of psychomotor and cognitive impairment caused by TCAs and SSRIs, especially in patients undergoing treatment in an outpatient setting and maintaining their daily and work activities. The results of numerous studies of adverse side effects have shown that cognitive and psychomotor impairment, as well as sedation caused by TCAs, significantly limit their use, since many of them develop at therapeutic doses (M. Dukes, L. Beeley, 1998) and require transfer of the patient to suboptimal dosages, which leads to prolongation of therapy. SSRIs are better tolerated than TCAs, however, in numerous studies (J. Edwards, 1992; P. Finley, 1994; S. Montgomery, S. Kasper, 1995), confirmed by a meta-analysis of 55 published papers (J. Anderson, B. Tomenson, 1994 ), SSRIs have been convincingly shown to be inferior to TCAs, especially in the treatment of severe depression. In this regard, there is a need to develop a new antidepressant that combines the mechanisms of action of TCAs (non-selective inhibition of monoamine reuptake) and SSRIs (selective inhibition of serotonin reuptake without affecting postsynaptic receptors). The integrative mechanism of action of such a thymoanaleptic allowed us to hope for a new, more advanced drug in the arsenal of antidepressants. One of these drugs is the thymoanaleptic Ixel (milnacipran hydrochloride), a non-selective serotonin and norepinephrine reuptake inhibitor, produced by Pierre Fabre Medicament, France. Unlike most TCAs, Ixel has no affinity for cholinergic (muscarinic), adrenergic, or histaminergic H1 receptors. However, Ixel also has no affinity for dopaminergic receptors D1 and D2, benzadiazepine and opioid receptors. Ixel is well absorbed when taken orally. Bioavailability is about 85%, does not depend on the nature and diet. The maximum plasma concentration (Cmax) is reached approximately 2 hours (Tmax) after administration. After a single dose of 50 mg, it is approximately 120 ng/ml. The concentration in the blood plasma increases in proportion to the dose taken, reaching up to 200 mg after a single dose. After repeated doses, equilibrium is achieved within 2–3 days with an increase in concentration from approximately 70 to 100% relative to a single dose (Cmax = 216 ng/ml). Interindividual differences are weak. Plasma protein binding is weak (13%) and is not accompanied by saturation. The volume of distribution of Ixel is approximately 5 l/kg with a total excretion coefficient of 40 l/h. Renal and non-renal clearances are equal. The metabolism of Ixel is limited primarily to conjugation with glucuronic acid. There is no active metabolite. The half-life is 8 hours. It is excreted primarily by the kidneys (90% of the dose taken) with secretion of unchanged drug by the renal tubules. After repeated doses, Ixel is completely eliminated from the body 2-3 days after discontinuation of the drug. At a therapeutic dose, the concentration of the drug in the blood plasma is constantly at a level corresponding to the inhibition of the reuptake of norepinephrine and serotonin from 50 to 90%. The pharmacological effects observed in the digestive and genitourinary systems appear to be associated with inhibition of norepinephrine uptake, which has an antagonistic effect on acetylcholine (indirect anticholinergic effect). Ixel does not cause changes in repolarization or cardiac conduction system. It does not affect the patient's responses to cognitive tests and has a mild sedative effect. Depressed patients treated with Ixel note a decrease in sleep disturbances. The period of falling asleep is shortened, the number of night awakenings is reduced, and the latency period for the onset of REM sleep increases, as well as the duration of sleep itself.
Material and treatment methods
At the Department of Psychiatry, Federal University of the Russian State Medical University, an open, simple clinical study was conducted to study the therapeutic effectiveness and safety of the use of the drug “Ixel” (capsules of 25 and 50 mg of active substance) in patients with depressive disorders.
The duration of studying the effect of the drug in each patient was 60 days. The duration of the study was planned to be 6 months, starting from the date of initiation of drug use in the first patient. The study was carried out using the clinical method and standardized rating scales. The dynamics of the patients' condition, the effectiveness and tolerability of treatment were assessed on the basis of clinical data using adequate statistical methods. Ixel was prescribed as monotherapy or, if necessary (see below), in combination with other psychotropic drugs 7 days (“washout” period) after discontinuation of previous treatment. The patients' condition was assessed on the day of Ixel prescription, 3, 10, 20, 30, 45 and 60 days of therapy. The effectiveness of ixel was assessed using unified rating scales: • the Clinical Global Impression Scale (CGI), • the Montgomery-Åsberg Depression Rating Scale (MADRS), • the Hamilton Depression Rating Scale, n-17 (CHDRS), as well as adverse event registration cards (AE) and side effects (AE). Patients who were unable to accept the conditions of the protocol and those with a high probability of refusing to comply with them were excluded from the study. Ixel was also not prescribed to patients with signs of the following disorders according to ICD-10 at the time of the study or within 3 months before the start of the study: • delirium, dementia, amnestic or other cognitive disorders (F.0); • alcoholism, drug addiction (F1); • anxiety-phobic disorders (F40, F41); • obsessive-compulsive disorder (F42); • reaction to severe stress and adaptation disorders (F43); • persons suffering from liver and kidney failure; • patients with prostatic hyperplasia; • patients with arterial hypertension and cardiopathy; • pregnant and breastfeeding women; • persons with hypersensitivity to Ixel; • persons under 18 and over 65 years of age. Ixel was prescribed for moderate or mild depression at a dose of 50 mg (25 mg 2 times a day) or 100 mg (50 mg 2 times a day), increasing the dosage to 100–150 mg/day. To correct anxiety or prevent anxiety disorders at the beginning of therapy, treatment with Ixel was combined with tranquilizers (phenazepam 0.001 g 3 times a day - n=2; seduxen 0.005 g 3 times a day - n=1) and hypnotics (imovan 0.0075 g at night – n=2). Ixel was not combined with the following drugs: • MAO inhibitors, especially non-selective ones (risk of serotonergic syndrome); • lithium salts (risk of serotonergic syndrome); • adrenaline and norepinephrine (hypertensive crisis and heart rhythm disturbances are possible); • clonidine and its derivatives (possible inhibition of the hypotensive effect of clonidine); • sumatriptan (possible increase in blood pressure, suppression of coronary arterial vasoconstriction with suppression of serotonergic effects); • digoxin (risk of potentiation of hemodynamic disorders). As can be seen from the data in table.
1 , the present study included a large group of patients with depressive disorders in terms of diagnostic criteria and characteristics of clinical symptoms. For greater purity of the experiment, patients with current somatic disorders were excluded from the number of outpatients (n=14) and those receiving Ixel in the clinic (n=16). This made it possible to focus more attention on the purely thymoanaleptic effect of Ixel, followed by a multifaceted assessment of it as an antidepressant.
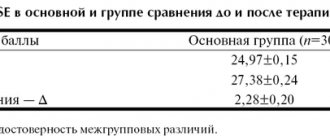
The present study included mainly middle-aged (most able-bodied) individuals, which made it possible to evaluate Ixel not only as a true antidepressant, but also as a drug that can have a positive impact on the quality of life of patients. Ixel was prescribed to 31 patients. Due to the fact that 1 patient stopped taking the drug after 3 days of therapy without explanation and did not show up for subsequent appointments, he was excluded from the study. Thus, the total number of patients receiving Xel is 30 patients. Of the 30 patients included in the study, 14 combined treatment with Ixel while maintaining their work, family, and social status (outpatients). More than half of the patients (53.3%) were patients with bipolar affective disorders with predominantly moderate current depressive episodes (30%). The second largest group consisted of people with a depressive episode (30%), in contrast to the first group, it was slightly dominated by people with a mild depressive episode (16.6%). The number of patients receiving Ixel also included patients with recurrent depressive disorder (16.6%). The criteria for assessing patients were based on the concepts of the International Classification of Diseases (10th revision) “Classification of Mental and Behavioral Disorders”, and therefore the specification of diagnostic criteria does not require more detailed justification. In the process of assessing the condition of the patients, we did not note any significant differences in their status. However, the syndromological characteristics require some clarification, which is essential for assessing the pharmacodynamics of Ixel. In all patients (n=30), the condition was determined by a decrease in mood to a distinct, previously unusual level, which was observed for most or the whole day for at least 2 weeks and did not significantly depend on external circumstances. Along with this, all patients noted a loss of interest and satisfaction from previously usually pleasant or everyday habitual activities, a decrease in motivation, energy, or increased fatigue with psychomotor impairment and the appearance of lethargy (n = 16). In addition, subjectively perceived and/or objectively determined decreases in concentration, uncertainty and/or indecision were noted. Unexpressed suicidal thoughts were noted in 9 patients, sleep disturbances (mainly pre- and intrasomnic disorders) - in 12, and decreased appetite - in 23 patients. In addition, against the background of predominantly asthenoadynamic disorders in the structure of the depressive state, a feeling of slight anxiety was revealed in 8 patients, which influenced the subsequent results of Ixel therapy and the occurrence of side effects. According to the severity of depressive disorders (severity of depression), their condition was considered within the framework of a mild depressive episode (46.7% of cases), as well as a moderate depressive episode (53.3% of cases). Results of using the drug “Ixel” The results of long-term (D60) use of the drug “Ixel” indicate its high therapeutic effectiveness. Analyzing the dynamics of the patients’ condition and the results of Ixel therapy, reflected in the Clinical Global Impression (GCI) scale, the following conclusions can be drawn ( Table 2
).
As can be seen from the data in table. 2
, “disease severity” decreased from 3.8 to 0.6 points over 60 days of therapy.
However, by the 20th day of treatment, we noted a statistically significant decrease in the severity of depressive disorders. Accordingly, these days, both objectively when assessing the condition of patients and when carrying out statistical calculations, a significant “general improvement” was noted, which underwent dynamics from 4.1 to 0.8 points over 60 days of therapy. In this regard, the patients’ condition was categorized as “great improvement” and/or “very great improvement.” Only 3 patients with moderate depression had results indicating “slight improvement.” The therapeutic effect in 78.1% of patients was assessed as “significant; significant improvement or complete remission.” In 21.9% of cases, the therapeutic effect did not go beyond “moderate; improvement; partial remission.” Despite the fact that SHOKV reflects the total data made up of the multi-directional effects of Ixel, we did not determine a significant difference between the effect of the studied drug on patients with different diagnostic criteria (bipolar affective disorder, depressive episode, recurrent depressive disorder), as well as patients whose depression was assessed as moderate and/or mild. The pharmacodynamic effects of Ixel were recorded and assessed using specialized unified rating scales, in particular the Montgomery-Asberg Depression Rating Scale (MADRS). As can be seen from the data in table.
3 , the reduction in the average total MADRS score begins from the first days of taking Ixel.
Already in D10 we can state a statistically significant decrease in the average total MADRS score. At the same time, it should be noted that the most intense reduction occurs in the first (D1–D10) days of therapy. This indicates the rapidity of the therapeutic effect of the drug. In addition to the rapid onset of the therapeutic effect, Ixel is also distinguished by its high therapeutic effectiveness. By the end of treatment (D60), the average total MADRS score decreased from 25.2 to 4.7. When analyzing data on the dynamics of individual psychopathological signs observed in patients, different rates of normalization of individual signs taken into account were noted. Lethargy and associated asthenic and adynamic disorders decreased most intensively (D10 – p<0.005). Subsequently (D20 – p<0.001), an intense positive effect of ixel on a whole group of disorders was noted: visible and described sadness; internal tension; sleep disturbance; inability to feel; pessimistic and suicidal thoughts; lack of concentration. Such a harmonious effect on the reduction of individual depressive disorders indicates the complex integrative mechanisms underlying the intimate action of Ixel. In the first days of treatment (D1–D3), in a number of cases, increased internal tension and deterioration in sleep were noted, which required drug correction (see below). More detailed results were obtained when assessing the effectiveness of Ixel using the Hamilton Depression Rating Scale (HDRS). As can be seen from the data in table.
4 , the total HDRS score decreased from 26.3 to 3.5 during the Ixel treatment period. Thus, the therapeutic effectiveness of this drug after D60 is 86.7%.
These data further confirm the previously obtained idea of the high therapeutic activity of Ixel, as well as the speed of onset of the therapeutic effect (D10 - p<0.001). A detailed analysis of the dynamics of the patients' condition using HDRS allows us to conclude that Ixel has an activating effect. This is evidenced by the intensive reduction of inhibition (D10 – p<0.005), as well as the rapid normalization of the patients’ performance (D10 – p<0.001). An indirect criterion for the activating effect of Ixel can be a short-term and slight increase in agitation, mental anxiety and early insomnia (D3). These symptoms were easily relieved by the administration of hypnotics and daytime tranquilizers (see below). Subsequently, dissomnia disorders underwent intensive reverse reduction and almost all groups of sleep disorders (pre-, intra- and post-somnia disorders) were not observed after D20. Equally intense was the positive dynamics of suicidal tendencies, feelings of guilt, lethargy, agitation and general somatic symptoms. When using Ixel, an uneven reverse dynamics of the severity of somatic anxiety was noted. At D30, 2 patients experienced an increase in gastrointestinal disorders, which required a reduction in the dose of the drug. In all likelihood, this is due to the serotonergic effect of Ixel. The activating effect of Ixel was one of the factors in the normalization of sexual disorders (libido in men and women; normalization of the menstrual cycle in women). In parallel with the improvement in the general condition of patients, due primarily to the normalization of depressed mood and self-esteem of patients, an improvement in appetite and an increase in low body weight were noted. The least favorable results were obtained in the treatment of hypochondria. This is explained by the fact that 3 patients (persons with anxious and suspicious character traits in premorbid), regardless of their condition (phase-remission), treated their health with a certain degree of supervaluation, constantly listening to the sensations in the body, and were actively searching for new drugs and methods treatment. In general, the data on HDRS practically do not differ from the results obtained using MADRS, and confirm previously made conclusions about the speed of therapeutic action and the high effectiveness of the drug “Ixel”.
Adverse events (AEs) and side effects (AEs)
With long-term (D60) use of Ixel, a number of AEs and AEs were noted. A total of 12 AEs were identified in 8 (26.7%) patients. In the first days of therapy, an increase in anxiety was noted in 3 patients, which in 2 patients was accompanied by sleep disturbances (primarily presomnia disorders), as well as the appearance and/or intensification of irritability. Increased feelings of anxiety and irritability were relieved by the prescription of tranquilizers, which were discontinued after 2 weeks; dyssomnic disorders normalized after the administration of Imovan, which the patients took for 7–10 days. On D10 and D20, a slight increase in blood pressure (both systolic and diastolic) was noted, and on D30, 3 patients developed a feeling of nausea. In all 5 cases, the method of leveling AEs was to reduce the dose of Ixel to 100 mg/day. It should be noted that Ixel not only causes a small number of AEs, but the severity of these events in all patients was assessed as mild.
Discussion
A long-term (D60) study of the drug “Ixel” in capsules of 25 and 50 mg in 30 patients, as well as subsequent analysis of the results obtained, indicate its high therapeutic effectiveness.
Patients with depressive disorders that could be classified as moderate (average total MADRS score of 25.2 and HDRS of 26.3) received Ixel in doses of 50–150 mg per day. Based on the mechanism of action of Ixel (potentiation of serotonin-noradrenergic structures of the brain and the absence of an effect on a number of postsynaptic receptors), it was possible to assume possible pharmacodynamic features of the action of this drug. In the dynamics of treatment with Ixel, first of all, its general activating effect is revealed, including its effect on the psychomotor sphere. This therapeutic effect is associated with the noradrenergic properties of the antidepressant under study. The general activating effect of Ixel also caused the appearance of a number of AEs in the first days of therapy ( Table 5
).
The pronounced thymoanaleptic effect of Ixel, revealed during therapy, is the result of potentiation of serotonergic structures of the brain. It should be noted that there was a fairly uniform decrease in all depressive disorders, which indicates the harmonious effect of Ixel on the complex integrative processes that underlie the pathogenetic mechanisms of depression. This, in all likelihood, determines the speed of onset of the therapeutic effect identified when taking Ixel. A small number of AEs are most likely determined by the lack of affinity of Ixel for cholinergic (muscarinic), adrenergic, histaminergic H, as well as dopaminergic D1 and D2 and benzodiazepine receptors. This determines not only the low frequency and severity (degree) of AEs, but also the absence of a sedative effect in Ixel.
conclusions
Ixel (milnacipran) in capsules of 25 and 50 mg is an effective, well-tolerated antidepressant with a mild activating effect, without sedation. The remaining conclusions are formulated in the article “Ixel (milnacipran): generalized results of a clinical study of a selective serotonin and norepinephrine reuptake inhibitor (SNRI) in Russia” with our participation.
Use of the drug Velaxin
Capsules should be taken whole with a meal with liquid. Capsules should not be divided, crushed, chewed or dissolved. The daily dose should be taken in one dose (morning or evening) at the same time. Depression The recommended dose is 75 mg/day in one dose. If, taking into account the course of the disease, a higher dose is necessary, for example, in case of severe depression or inpatient treatment of the patient, the recommended initial dose may be 150 mg/day in one dose. After this, the daily dose can be increased by 37.5–75 mg at intervals of ≥2 weeks, but not less than 4 days until the required therapeutic effect is achieved. The recommended maximum dose of Velaxin is 225 mg/day for moderate depression and 350 mg for severe depression. After achieving the desired therapeutic effect, the dose should be gradually reduced to the minimum effective, taking into account the individual response and tolerability of each patient. When used in high doses, the risk of developing side effects of the drug increases. Generalized anxiety disorders and social anxiety disorders (social phobia) The recommended dose of Velaxin is 75 mg/day in one dose. If after 2 weeks of treatment there is no noticeable improvement in the condition, the daily dose can be increased to 150 mg/day in one dose. When used in a daily dose of 75 mg, an anxiolytic effect is observed after 1 week. Prevention of relapses or new episodes The effectiveness of venlafaxine has been established with long-term therapy (up to 12 months for depression and social phobia; up to 6 months for generalized anxiety disorders). Treatment of acute episodes of depression must be continued for at least 6 months. The doses typically used to prevent a relapse or new episode are similar to those used to treat patients with a primary episode. It is necessary to regularly (at least once every 3 months) examine the patient to monitor the effectiveness of long-term therapy with Velaxin. Transfer of patients receiving therapy with Velaxin in the form of tablets to taking a capsule form of the drug Patients with depression receiving Velaxin tablets in a therapeutic dose can be transferred to taking the drug in the form of long-acting capsules with the appointment of the nearest equivalent dose. Sometimes individual dose adjustment may be required. Renal failure When the glomerular filtration rate is 30 ml/min, no dose adjustment is required. With a glomerular filtration rate of 10–30 ml/min, the dose should be reduced by 50%. Due to the increased half-life of venlafaxine and its active metabolite in these patients, the daily dose should be taken in one dose. It is not recommended to use venlafaxine if the glomerular filtration rate is ≤10 ml/min, since there is insufficient data on therapy in these patients. For patients on hemodialysis, the daily dose of the drug should be reduced by 50% and, if possible, used after completion of the hemodialysis procedure. Liver failure In mild liver failure (prothrombin time ≤14 s), no dose adjustment is required. In case of moderately severe liver failure (prothrombin time - 14–18 s), the dose should be reduced by 50%. It is not recommended to use venlafaxine in severe hepatic impairment (prothrombin time 18 s), as there is insufficient data on this therapy. Elderly patients Caution should be exercised when prescribing the drug to elderly patients (due to the possibility of renal dysfunction), and the drug is prescribed in the minimum effective dose. When increasing the dose, the patient should be under regular medical supervision. Cancellation of Velaxin Abrupt cessation of Velaxin therapy, especially after taking the drug in high doses, can cause the development of withdrawal syndrome, and therefore a gradual dose reduction is recommended before complete discontinuation of the drug. If the drug has been used in high doses for 6 weeks, a dose reduction period of at least 2 weeks is recommended. The length of the period required to reduce the dose depends on the dose size, duration of therapy, as well as the individual sensitivity of the patient.
Contraindications to the use of the drug Velaxin
Hypersensitivity to any component of the drug. Simultaneous use of any antidepressant from the MAO inhibitor group, as well as for 14 days after discontinuation of irreversible MAO inhibitors. After complete discontinuation of venlafaxine, therapy with MAO inhibitors can be started no earlier than 7 days later. Diseases of the cardiovascular system (heart failure, coronary artery disease, ECG changes - pre-existing increase in the QT on the ECG), hypertension (arterial hypertension), electrolyte imbalance. Age up to 18 years. During pregnancy and breastfeeding.
Side effects of the drug Velaxin
Side effects are divided by body system and frequency of occurrence: very often (1/10); often (≤1/10, but 1/100); sometimes (≤1/100, but 1/1000); rare (≤1/1000); very rare (≤1/10,000). General symptoms: very often - asthenia, headache; often - abdominal pain, chills, increased body temperature; rarely - anaphylaxis. Gastrointestinal tract: very often - constipation, nausea; often - loss of appetite, diarrhea, vomiting; sometimes - bruxism, reversible increase in the activity of liver enzymes; rarely - gastrointestinal bleeding; very rarely - pancreatitis. Cardiovascular system: often - tachycardia, hypertension (arterial hypertension), dilatation of blood vessels; sometimes - hypotension/orthostatic hypotension, loss of consciousness, arrhythmias, tachycardia; very rarely - pirouette-type tachycardia, increased QT on ECG, ventricular tachycardia, ventricular fibrillation. Respiratory system: often - difficulty breathing, yawning; very rarely - eosinophilic infiltrates in the lungs. Nervous system: very often - dizziness, dry mouth, insomnia, anxiety, drowsiness; often - unusual dreams, agitation, anxiety, confusion, increased muscle tone, paresthesia, tremor; sometimes - apathy, hallucinations, myoclonus; rarely - ataxia with impaired balance and coordination of movements, speech impairment, including dysarthria, mania or hypomania, as well as manifestations that resemble neuroleptic malignant syndrome (NMS), seizures, serotonergic syndrome; very rarely - delirium, extrapyramidal disorders, including dyskinesia and dystonia, psychomotor agitation/akathisia. Genitourinary system: very often - anorgasmia, erectile dysfunction, impaired ejaculation and orgasm; often - frequent urination, decreased libido, menstrual irregularities; sometimes - urinary retention, menorrhagia; rarely - galactorrhea. Sense organs: often - blurred vision and accommodation, mydriasis, noise and ringing in the ears; sometimes - a change in taste sensations. Skin: very often - sweating; often - skin rashes and itching; sometimes - angioedema, maculopapular rash, urticaria, photosensitivity, alopecia; rarely - erythema multiforme, Stevens-Johnson syndrome. Blood system: sometimes - ecchymosis, bleeding from the mucous membrane; rarely - increased bleeding time, hemorrhage, thrombocytopenia; very rarely - agranulocytosis, aplastic anemia, neutropenia, pancytopenia. Metabolism: often - increased cholesterol levels in the blood serum, increase or decrease in body weight; sometimes - hyponatremia, increased activity of liver transaminases; rarely - hepatitis; very rarely - increased prolactin levels. Musculoskeletal system: often - arthralgia, myalgia; sometimes - muscle spasms; very rarely - rhabdomyolysis.
Special instructions for the use of the drug Velaxin
In patients with depression, the likelihood of suicide attempts should be considered before starting any therapy. Therefore, to reduce the risk of overdose, the initial dose of the drug should be as low as possible, and the patient should be under medical supervision. Aggressive behavior of the patient has been reported during the use of venlafaxine (especially at the beginning of the course of treatment and after discontinuation of the drug). The use of venlafaxine is associated with the development of psychomotor agitation, which is characterized by subjectively unpleasant restlessness with a need to move. Most often this occurs during the first weeks of treatment. If such symptoms occur, increasing the dose may not be appropriate, so the question of whether it is advisable to continue taking venlafaxine should be decided. In patients with mood disorders, hypomanic or manic states may occur when treated with antidepressants, including venlafaxine. Velaxin should be prescribed with caution to patients with a history of mania. These patients require medical supervision. Velaxin should be prescribed with caution to patients with a history of epileptic seizures. If epileptic seizures occur, treatment must be stopped. The patient should be warned about the need to immediately consult a doctor if a skin rash, elements of urticaria or other allergic reactions occur. In some patients, during the period of use of venlafaxine, a dose-dependent increase in blood pressure is possible, and therefore it is recommended to regularly monitor blood pressure, especially during the period of dose adjustment or increase. An increase in heart rate is possible, especially when taken in high doses. In this case, medical supervision of the patient's condition is necessary. Occasionally, orthostatic hypotension was observed during use of the drug. Patients, especially the elderly, should be warned about the possibility of dizziness. Velaxin may increase the risk of hemorrhages in the skin and mucous membranes in patients predisposed to these conditions. Patients should be warned about this and advised to exercise caution while using the drug. During the use of Velaxin, especially in conditions of dehydration or decrease in blood volume (including in elderly patients and in patients taking diuretics), hyponatremia and/or syndrome of insufficient secretion of antidiuretic hormone is possible. During the period of use of the drug, mydriasis may occur, and therefore it is recommended to monitor intraocular pressure in patients with a tendency to increase it, in patients with angle-closure glaucoma. When treating patients with impaired renal or hepatic function, caution and careful medical monitoring of the patient's condition is necessary (dose reduction is possible). In patients who have recently suffered a myocardial infarction and with signs of decompensated heart failure, the drug should be prescribed with caution under constant medical supervision. The safety and effectiveness of the combined use of venlafaxine and drugs used for weight loss, including phentermine, have not been established, so their simultaneous use is not recommended. With prolonged use of the drug, it is advisable to monitor the level of cholesterol in the blood serum. After stopping the use of Velaxin, especially suddenly, withdrawal syndrome often occurs. The risk of developing withdrawal syndrome depends on the duration of treatment, the dose used, and the rate of dose reduction. With withdrawal syndrome, dizziness, paresthesia, sleep disturbance, agitation, anxiety, nausea, vomiting, tremor, sweating, headache, diarrhea, tachycardia, and emotional disorders appear. These symptoms are usually observed in the first days after discontinuation of the drug and disappear on their own within 2 weeks. Therefore, the drug should be discontinued gradually, reducing the dose of venlafaxine gradually over several weeks or months, depending on the patient's condition. Velaxin does not cause the development of symptoms of tolerance or dependence. Despite this, as with other drugs that act on the central nervous system, patients need to be monitored for signs of drug abuse (especially patients with a history of similar problems). While using Velaxin, women of reproductive age should use adequate methods of contraception. The drug may negatively affect the ability to drive vehicles and operate potentially dangerous machinery. Therefore, doses at which driving vehicles and working with machinery are possible are determined for each patient individually.
Instructions for use VELAXIN® tablets
Suicide/suicidal ideation or clinical worsening
Depression is associated with an increased risk of suicidal ideation, self-harm and suicide (suicide-related events). This risk persists until significant remission occurs. Since improvement may not occur during the first few weeks of treatment or longer, patients should be closely monitored until such improvements occur. Clinical experience suggests a possible increased risk of suicide in the early stages of remission.
Other psychiatric conditions for which venlafaxine is prescribed may also be associated with an increased risk of suicidal events. In addition, these conditions may be comorbid with major depressive disorder. The precautions observed when treating patients with major depressive disorder should also be observed when treating patients with other psychiatric disorders.
It is known that patients with a history of suicidal symptoms who exhibit a significant degree of suicidal ideation before treatment are at greater risk of suicidal ideation and suicide attempts; During treatment, such patients should be closely monitored. A meta-analysis of placebo-controlled clinical trials of antidepressants in adult patients with psychiatric disorders showed an increased risk of suicidal behavior in patients under 25 years of age taking antidepressants compared with age-matched patients taking placebo.
Patients, incl. those at high risk of suicidal ideation and suicide attempts require careful monitoring during drug treatment, especially at the beginning of treatment and when changing doses. Patients (and caregivers) should be warned to monitor for clinical worsening, suicidal behavior or ideation, or unusual changes in behavior, and to seek prompt medical attention if these symptoms occur.
Use in children and adolescents under 18 years of age.
Velaxin® immediate release tablets should not be used to treat children and adolescents under 18 years of age. Suicidal behavior (suicide attempt and suicidal ideation) and hostility (primarily aggression, hostile behavior and anger) were observed more frequently in children and adolescents treated with antidepressants compared with those taking placebo in clinical studies. If, despite this, a decision is made to carry out treatment, careful monitoring of the patient is necessary in order to identify suicidal symptoms. In addition, there are no long-term safety data on growth, maturation, and cognitive and behavioral development in children and adolescents.
Serotonin syndrome
As with other serotonergic drugs, venlafaxine may cause serotonin syndrome or neuroleptic malignant syndrome (NMS)-like reactions, a potentially life-threatening condition, particularly when co-administered with other serotonergic drugs (including triptans, serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), amphetamines, lithium preparations, sibutramine, preparations containing St. John's wort ( Hypericum perforatum
), fentanyl and its analogues, tramadol, dextromethorphan, tapentadol, pethidine, methadone and pentazocine), with drugs that inhibit serotonin metabolism (MAO inhibitors, such as methylene blue), with serotonin precursors (for example, with supplements containing tryptophan), and also with other antipsychotic drugs and dopamine antagonists (see sections Contraindications and Drug Interactions).
Serotonin syndrome may include the following symptoms:
- mental status changes (eg, psychomotor agitation, hallucinations, coma), autonomic nervous system disturbance (eg, tachycardia, unstable blood pressure, hyperthermia), neuromuscular disturbances (eg, hyperreflexia, incoordination), and/or gastrointestinal symptoms (eg, nausea, vomiting, diarrhea).
In its most severe form, serotonin syndrome is similar to NMS, with symptoms such as hyperthermia, muscle rigidity, instability of the autonomic nervous system with possible rapid changes in the patient's vital signs and mental status.
If there is a clinical need for the combined use of venlafaxine with other drugs that affect the serotonergic or dopaminergic neurotransmitter system, it is recommended to carefully monitor the patient's condition, especially at the beginning of treatment and when increasing doses.
Concomitant use of venlafaxine with serotonin precursors (eg, tryptophan-containing supplements) is not recommended.
Narrow-angle glaucoma
Mydriasis may occur in connection with taking venlafaxine. Close monitoring of patients with elevated intraocular pressure or patients at risk of developing angle-closure glaucoma is recommended.
Arterial pressure
A dose-dependent increase in blood pressure is often reported when taking venlafaxine. In the post-marketing period, several cases of severe increases in blood pressure requiring immediate treatment have been observed. Before starting treatment, all patients should undergo a thorough evaluation for high blood pressure, and control of pre-existing hypertension is also necessary. Periodic monitoring of blood pressure is necessary after starting treatment, as well as after increasing the dose. Caution should be exercised when prescribing the drug to patients whose underlying disease may be accompanied by an increase in blood pressure, for example, with impaired cardiac function.
Heartbeat
An increase in heart rate is possible, especially when taking the drug in high doses. Caution should be exercised when prescribing the drug to patients in whom an increase in heart rate may have an adverse effect on the underlying disease.
Heart disease and risk of arrhythmia
There is insufficient experience with the use of venlafaxine in patients who have recently had a myocardial infarction or have unstable cardiac disease. Therefore, it should be used with caution in such patients. In the post-marketing period, cases of QTc prolongation, torsade de pointes (TdP), torsade de pointes (TdP), and fatal cardiac arrhythmias have been observed with venlafaxine, especially in overdose or in patients with risk factors for QTc prolongation or torsade de pointes (see Pharmacology). action). The risk-benefit ratio must be assessed before prescribing venlafaxine to patients at high risk of serious cardiac arrhythmias (see Pharmacological Actions).
Convulsions
During treatment with venlafaxine, seizures may occur. As with all antidepressants, venlafaxine should be used with caution in patients with a history of seizures; such patients should be closely monitored. Treatment with the drug should be discontinued in patients who develop seizures.
Hyponatremia
When taking venlafaxine, cases of hyponatremia and/or syndrome of impaired antidiuretic hormone secretion are possible. This phenomenon was most often observed in patients with hypovolemia or dehydration. Elderly patients, patients taking diuretics, and patients at increased risk of hypovolemia are at greater risk for this phenomenon.
Abnormal bleeding
Medicines that inhibit serotonin reuptake may lead to decreased platelet function. Patients taking SSRIs and SNRIs, including venlafaxine, may have an increased risk of bleeding, ranging from ecchymoses, hematomas, epistaxis and petechiae to gastrointestinal and life-threatening bleeding. Patients receiving venlafaxine may have an increased risk of bleeding. As with other serotonin reuptake inhibitors, venlafaxine should be administered with caution to patients predisposed to bleeding, including patients taking anticoagulants and platelet inhibitors.
Serum cholesterol
In placebo-controlled clinical studies, a clinically significant increase in serum cholesterol was observed in 5.3% of patients receiving venlafaxine and 0.0% of patients receiving placebo for at least 3 months. With long-term use of the drug, it is advisable to monitor the cholesterol level in the blood serum.
Combined use with weight loss agents
Safety and effectiveness of combining venlafaxine with weight loss agents, incl. phentermine, not established. It is not recommended to use venlafaxine and weight loss agents together. Venlafaxine should not be used as a means of weight loss and is not recommended in combination with other drugs.
Mania/hypomania
In a small number of patients with mood disorders receiving antidepressants, incl. and venlafaxine, mania/hypomania may occur. As with other antidepressants, venlafaxine should be prescribed with caution to patients with a personal or family history of bipolar affective disorder.
Aggression
In a small number of patients during treatment with antidepressants, incl. venlafaxine, aggression may occur. These symptoms were observed at the beginning of treatment, with increasing doses and discontinuation of treatment.
As with other antidepressants, venlafaxine should be prescribed with caution to patients with a history of aggression.
Stopping treatment
After stopping treatment (especially abruptly), withdrawal symptoms often appear (see section Side effects). In clinical studies, adverse events observed after treatment discontinuation (dose taper and post-dose reduction) occurred in approximately 31% of patients receiving venlafaxine and 17% of patients receiving placebo.
The risk of withdrawal symptoms may depend on several factors, including: on the duration of treatment and doses used, as well as the rate of dose reduction. Dizziness, sensory disturbances (including paresthesia), sleep disturbances (including insomnia and vivid dreams), psychomotor agitation or anxiety, nausea and/or vomiting, tremor and headache are the most common reactions. In general, these symptoms are mild or moderate, however, in some patients they can be severe.
Typically, symptoms appear within the first few days after stopping treatment, but in very rare cases, similar symptoms have been reported in patients who accidentally missed a dose. These symptoms usually go away on their own, usually within 2 weeks, but in some patients they may persist for a longer period of time (2-3 months or more). Therefore, if it is necessary to discontinue treatment, it is recommended to gradually reduce the dose (over several weeks or months, depending on the patient's response (see Dosage Regimen).
Akathisia/psychomotor restlessness
The use of venlafaxine is associated with the development of akathisia, characterized by a subjectively unpleasant and disturbing restlessness for the patient, with a need to move, often combined with the inability to sit or stand still. This is most likely to occur during the first few weeks of treatment. In patients with such symptoms, increasing the dose may have an adverse effect.
Dry mouth
Dry mouth occurs in 10% of patients receiving venlafaxine. This may increase the risk of dental caries and patients should be advised of the importance of dental hygiene.
Diabetes
In patients with diabetes mellitus, the use of selective serotonin reuptake inhibitors or venlafaxine may lead to changes in glycemic control. It may be necessary to change the dose of insulin and/or oral antidiabetic medications.
Sexual dysfunction
SSRIs and SNRIs can cause sexual dysfunction. There have been reports of long-term impairment of sexual function despite discontinuation of SSRIs or SNRIs.
Impact on the results of laboratory tests for the presence of narcotic drugs
False-positive urine immunoassay results for phencyclidine (PCP) and amphetamine have been observed in patients receiving venlafaxine. This is due to the lack of specificity of immunotests. False-positive test results are possible several days after venlafaxine is discontinued. Confirmatory tests such as gas chromatography or mass spectrometry can differentiate venlafaxine from phenylcyclidine and amphetamine.
Velaxin® tablets contain lactose
Patients with rare hereditary diseases such as galactose intolerance, complete lactase deficiency and glucose/galactose malabsorption should not take this drug.
Sodium content
All Velaxin® tablets with varying levels of active substance contain less than one millimole (23 mg) of sodium, so the tablets are practically sodium-free.
Preclinical safety studies
Studies of venlafaxine in rats and mice showed no evidence of tumorigenesis. In numerous in vitro
and
in vivo
, venlafaxine demonstrated no mutagenicity.
Reproductive toxicity studies in animals have shown decreased body weight of pups, increased rates of stillborn pups, and increased pup mortality during the first 5 days of lactation. The cause of these deaths is unknown. These effects were observed at a dose of 30 mg/kg/day, which is 4 times higher than the daily dose of venlafaxine for humans - 375 mg (based on mg/kg). The dose at which these effects were absent is 1.3 times the human dose. The potential risk to humans is unknown.
Decreased fertility was observed in a study in which both male and female rats were given EFA. The dose administered in this case was approximately 1-2 times higher than the human dose of 375 mg/day. The clinical significance of this interaction is unknown.
Impact on the ability to drive vehicles and operate machinery
Any psychotropic drug can affect thinking, judgment and motor skills. Therefore, patients receiving venlafaxine should be warned about the possible effect of the drug on their ability to drive vehicles or operate dangerous machinery.
Interactions of the drug Velaxin
The use of Velaxin in combination with MAO inhibitors is contraindicated: tremor, myoclonus, sweating, nausea, vomiting, flushing, dizziness, fever, convulsive seizures, and death are possible. The use of Velaxin can be started no earlier than 14 days after the end of MAO inhibitor therapy. If a reversible MAO inhibitor is used, this interval may be shorter (24 hours). After discontinuation of Velaxin, you should take a break of at least 7 days before starting therapy with MAO inhibitors. Particular caution is required when using Velaxin with drugs that affect the central nervous system. The mutual influence of Velaxin and the following drugs should be taken into account: Lithium: there are reports of interaction between lithium and venlafaxine, as a result of which the level of lithium in the blood increases. Imipramine: the pharmacokinetics of venlafaxine and its metabolite EDV do not change, so a dose reduction of venlafaxine is not required when these drugs are used in combination. Haloperidol: its effect may be enhanced. Diazepam: the pharmacokinetics of the drugs and their main metabolites do not change significantly. Clozapine: an increase in the level of clozapine in the blood and the development of its side effects (for example, epileptic seizures) were noted. Risperidone: with the simultaneous use of these drugs (despite the increase in the AUC of risperidone), the pharmacokinetics of the sum of the active components (risperidone and its active metabolite) does not change significantly. Alcohol: depression of psychomotor activity under the influence of alcohol after taking venlafaxine does not increase, however, during the period of use of the drug Velaxin, the consumption of alcoholic beverages is not recommended. Electroconvulsive therapy: when conducting electroconvulsive therapy while taking selective inhibitors of neuronal reuptake of serotonin, an increase in the duration of epileptic activity was noted. It is necessary to exercise caution and ensure careful medical monitoring of the patient's condition when combined with this type of therapy and the use of Velaxin. Drugs metabolized by cytochrome P450 isoenzymes : the CYP 2D6 enzyme of the cytochrome P450 system converts venlafaxine into the active metabolite EDV. Unlike many other antidepressants, the dose of Velaxin does not need to be reduced when used once with drugs that inhibit CYP 2D6 activity, or in patients with a genetically determined decrease in CYP 2D6 activity, since the total concentration of the active substance and metabolite (venlafaxine and ODV) does not change. The main route of elimination of venlafaxine involves metabolism with the participation of CYP 2D6 and CYP 3A4, so special caution should be exercised when prescribing venlafaxine in combination with drugs that inhibit both of these enzymes. Venlafaxine is a relatively weak inhibitor of CYP 2D6 and does not inhibit the activity of CYP 1A2, CYP 2C9 and CYP 3A4 isoenzymes; therefore, it should not be expected to interact with other drugs in which these liver enzymes are involved in the metabolism. Cimetidine: inhibits the metabolism of venlafaxine during its initial passage through the liver, but does not have a significant effect on its conversion to EDV or the rate of elimination of EDV, the concentration of which in the circulating blood is much higher. Therefore, there is no need to change the dose of Velaxin and cimetidine when used in combination. This interaction may be more pronounced in elderly patients or with impaired liver function, therefore, in such cases, the combined use of cimetidine and Velaxin requires medical supervision. Antihypertensive and antidiabetic agents: no clinically significant interactions of venlafaxine with antihypertensive (including beta-adrenergic receptor blockers, ACE inhibitors and diuretics) and hypoglycemic agents have been identified. Drugs that bind to plasma proteins: Plasma protein binding is 27% for venlafaxine and 30% for EDV. Therefore, interactions due to their binding to proteins should not be expected. Warfarin: the anticoagulant effect of the latter may be enhanced; at the same time, prothrombin time increases. Indinavir: When used concomitantly with this drug, the pharmacokinetics of indinavir changes (with a 28% decrease in AUC and a 36% decrease in maximum concentration).
Velaxin 75 mg 28 pcs. pills
pharmachologic effect
Antidepressant.
Composition and release form Velaxin 75 mg 28 pcs. pills
Tablets - 1 tablet:
- active substance: venlafaxine (in the form of venlafaxine hydrochloride) 25 mg, 37.5 mg, 50 mg or 75 mg;
- excipients: lactose monohydrate (56.62 mg per 25 mg tablet; 84.93 mg per 37.5 mg tablet; 113.24 mg per 50 mg tablet and 169.86 mg per 75 mg tablet), cellulose microcrystalline, sodium starch glycolate (type A), colloidal anhydrous silicon dioxide, magnesium stearate.
Tablets of 25 mg and 50 mg: 10 tablets in a blister made of PVC/PVDC/alfoil. 1, 2, 3 or 6 blisters along with instructions for medical use in a cardboard box.
Tablets of 37.5 mg and 75 mg: 14 tablets in a blister made of PVC/PVDC/alfoil. 1, 2 or 4 blisters along with instructions for medical use in a cardboard box.
Description of the dosage form
White or almost white, flat round tablets, with a bevel, on one side of the tablet with engraving: E 744 - on 25 mg tablets, E 741 - on 37.5 mg tablets, E 742 - on 50 mg tablets, E 743 - on tablets of 75 mg; odorless or almost odorless.
Directions for use and doses
Velaxin® tablets are recommended to be taken with meals.
The recommended starting dose is 75 mg in two divided doses (37.5 mg) daily. If after several weeks of treatment there is no significant improvement, the daily dose can be increased to 150 mg (2 x 75 mg per day).
If, in the opinion of the doctor, a higher dose is necessary (major depressive disorder or other conditions requiring hospital treatment), 150 mg in two doses (2 x 75 mg per day) can be prescribed immediately. After this, the daily dose can be increased by 75 mg every 2-3 days until the desired therapeutic effect is achieved.
The maximum daily dose of Velaxin® is 375 mg. After achieving the required therapeutic effect, the daily dose can be gradually reduced to the minimum effective level.
Maintenance therapy and relapse prevention:
Maintenance treatment can last 6 months or more. The minimum effective doses used in the treatment of a depressive episode are prescribed.
Renal failure: in case of mild renal failure (glomerular filtration rate (GFR) more than 30 ml/min), no dosage adjustment is required. In case of moderate renal failure (GFR 10-30 ml/min), the dose should be reduced by 25-50%. Due to the prolonged half-life of venlafaxine and its active metabolite (EAM), these patients should take the entire dose once daily. It is not recommended to use venlafaxine in severe renal failure (GFR less than 10 ml/min), since there are no reliable data on such therapy. Patients on hemodialysis may receive 50% of the usual daily dose of venlafaxine after completion of hemodialysis.
Liver failure: in case of mild liver failure (prothrombin time (PT) less than 14 seconds), no dosage adjustment is required. In case of moderate liver failure (PT from 14 to 18 seconds), the dose should be reduced by 50%. The use of venlafaxine in severe hepatic impairment is not recommended as reliable data on such therapy are lacking.
Elderly patients: The elderly age of the patient itself does not require a dose change, however (as with other drugs) caution is required when treating elderly patients, for example, due to the possibility of impaired renal function. The lowest effective dose should be used. When increasing the dose, the patient should be under close medical supervision.
Stopping taking Velaxin®
Upon termination of treatment with Velaxin®, it is recommended to gradually reduce the dosage of the drug over at least a week and monitor the patient's condition in order to minimize the risk associated with drug withdrawal (see below).
The period required to completely stop taking the drug depends on its dosage, duration of treatment and the individual characteristics of the patient.
Pharmacodynamics
Venlafaxine is an antidepressant that does not chemically belong to any class of antidepressants (tricyclic, tetracyclic or others) and is a racemate of two active enantomers.
The mechanism of the antidepressant effect of the drug is associated with its ability to potentiate the transmission of nerve impulses in the central nervous system (CNS). Venlafaxine and its main metabolite O-desmethylvenlafaxine (ODV) are strong serotonin norepinephrine reuptake inhibitors (SNRIs) and weak dopamine reuptake inhibitors. In addition, venlafaxine and O-desmethylvenlafaxine reduce beta-adrenergic reactivity both after a single dose and with chronic use. Venlafaxine and EDV are equally effective in inhibiting the reuptake of neurotransmitters.
Venlafaxine has no affinity for muscarinic, cholinergic, histamine (H1) and α1-adrenergic receptors in the brain. Venlafaxine does not inhibit monoamine oxidase (MAO) activity. Has no affinity for opiate, benzodiazepine, phencyclidine, or N-methyl-d-aspartate (NMDA) receptors.
Pharmacokinetics
Venlafaxine is well absorbed from the gastrointestinal tract. After a single dose of 25-150 mg, the maximum plasma concentration reaches 33-172 ng/ml within approximately 2.4 hours. Subject to intensive metabolism during the first passage through the liver. Its main metabolite is O-desmethylvenlafaxine (ODV). The half-life of venlafaxine and EDV is 5 and 11 hours, respectively. The maximum concentration of EDV in blood plasma of 61-325 ng/ml is achieved approximately 4.3 hours after administration. The binding of venlafaxine and EDV to plasma proteins is 27% and 30%, respectively. EDV and other metabolites, as well as unmetabolized venlafaxine, are excreted by the kidneys. With repeated administration, equilibrium concentrations of venlafaxine and EDV are achieved within 3 days. In the range of daily doses of 75-450 mg, venlafaxine and EDV have linear kinetics. After taking the drug with food, the time to reach maximum concentration in the blood plasma increases by 20-30 minutes, but the values of maximum concentration and absorption do not change.
In patients with liver cirrhosis, plasma concentrations of venlafaxine and EDV are increased, and their elimination rate is reduced.
In moderate or severe renal impairment, the total clearance of venlafaxine and EDV is reduced and the half-life is prolonged. A decrease in total clearance is mainly observed in patients with creatinine clearance below 30 ml/min.
The age and gender of the patient do not affect the pharmacokinetics of the drug.
Indications for use Velaxin 75 mg 28 pcs. pills
Depression of various etiologies, treatment and prevention.
Contraindications
Hypersensitivity.
Concomitant use of MAO inhibitors.
Severe renal and/or liver dysfunction (glomerular filtration rate (GFR) less than 10 ml/min).
Age up to 18 years (safety and effectiveness for this age group have not been proven).
Established or suspected pregnancy.
Lactation period.
With caution: recent myocardial infarction, unstable angina, arterial hypertension, tachycardia, history of convulsive syndrome, increased intraocular pressure, angle-closure glaucoma, history of manic states, predisposition to bleeding from the skin and mucous membranes, initially reduced body weight.
Application of Velaxin 75 mg 28 pcs. pills during pregnancy and breastfeeding
The safety of venlafaxine during pregnancy has not been proven, so use during pregnancy (or intended pregnancy) is possible only if the potential benefit to the mother outweighs the possible risk to the fetus. Women of childbearing age should be warned about this before starting treatment and should immediately consult a doctor if they become pregnant or plan to become pregnant during treatment with the drug.
Venlafaxine and its metabolite (EFV) are excreted into breast milk. The safety of these substances for newborns has not been proven, so taking venlafaxine during breastfeeding is not recommended. If it is necessary to take the drug during lactation, the issue of stopping breastfeeding should be decided.
If maternal treatment was completed shortly before delivery, the newborn may experience drug withdrawal symptoms.
special instructions
Discontinuation of the drug Velaxin®: As with treatment with other antidepressants, abrupt cessation of venlafaxine therapy - especially after high doses of the drug - may cause withdrawal symptoms, and therefore it is recommended to gradually reduce its dose before discontinuing the drug. The length of the period required to reduce the dose depends on the dose size, duration of therapy, as well as the individual sensitivity of the patient.
When prescribing Velaxin® tablets to patients with lactose intolerance, the lactose content should be taken into account (56.62 mg in each 25 mg tablet; 84.93 mg in each 37.5 mg tablet; 113.24 mg in each 50 mg tablet, 169.86 mg each tablet contains 75 mg).
In patients with depressive disorders, the possibility of suicide attempts should be considered before starting any drug therapy. Therefore, to reduce the risk of overdose, the initial dose of the drug should be as low as possible, and the patient should be under close medical supervision.
In patients with mood disorders, hypomanic or manic states may occur when treated with antidepressants, including venlafaxine. Like other antidepressants, venlafaxine should be used with caution in patients with a history of mania. Such patients require medical supervision.
Like other antidepressants, venlafaxine should be administered with caution to patients with a history of epileptic seizures. Treatment with venlafaxine should be interrupted if epileptic seizures occur.
Patients should be warned to seek immediate medical attention if rash, urticaria, or other allergic reactions occur.
Some patients experienced a dose-dependent increase in blood pressure while taking venlafaxine, and therefore regular monitoring of blood pressure is recommended, especially during the period of adjustment or increase in dosage.
An increase in heart rate may occur, especially during high doses. Caution is recommended for tachyarrhythmia.
Patients, especially the elderly, should be warned about the possibility of dizziness and impaired balance.
Like other serotonin reuptake inhibitors, venlafaxine may increase the risk of bleeding into the skin and mucous membranes. Caution is necessary when treating patients predisposed to such conditions.
While taking venlafaxine, especially in conditions of dehydration or decreased blood volume (including in elderly patients and patients taking diuretics), hyponatremia and/or syndrome of insufficient secretion of antidiuretic hormone may occur.
Mydriasis may occur while taking the drug, and therefore it is recommended to monitor intraocular pressure in patients prone to increased pressure or suffering from angle-closure glaucoma.
Venlafaxine has not been studied in patients with recent myocardial infarction and decompensated heart failure. The drug should be prescribed to such patients with caution.
Clinical trials conducted to date have not revealed tolerance or dependence to venlafaxine. Despite this, as with other drugs that act on the central nervous system, the physician should closely monitor patients for signs of drug abuse. Careful monitoring and observation is necessary for patients with a history of such symptoms.
Women of childbearing potential should use appropriate contraception while taking venlafaxine.
Although venlafaxine does not affect psychomotor and cognitive functions, it should be taken into account that any drug therapy with psychoactive drugs may reduce the ability to make judgments, think or perform motor functions. The patient should be warned about this before starting treatment. If such effects occur, the degree and duration of restrictions should be determined by a physician. Drinking alcohol is also not recommended.
Overdose
Symptoms: ECG changes (prolongation of the QT interval, bundle branch block, expansion of the QRS complex), sinus or ventricular tachycardia, bradycardia, hypotension, convulsive states, changes in consciousness (decreased level of wakefulness). Death has been reported in overdoses of venlafaxine when taken concomitantly with alcohol and/or other psychotropic drugs.
Treatment: symptomatic. Specific antidotes are unknown. Continuous monitoring of vital functions (respiration and circulation) is recommended. Prescribing activated carbon to reduce drug absorption. Inducing vomiting is not recommended due to the risk of aspiration. Venlafaxine and EDV are not eliminated by dialysis.
Side effects Velaxin 75 mg 28 pcs. pills
Most of the side effects listed below are dose dependent. With long-term treatment, the severity and frequency of most of these effects decreases, and there is no need to discontinue therapy.
In order of decreasing frequency: frequent ≥ 1%, infrequent ≥ 0.1% -
General symptoms: weakness, increased fatigue.
From the gastrointestinal tract: loss of appetite, constipation, nausea, vomiting, dry mouth, rarely hepatitis.
Metabolism: increased serum cholesterol levels, decreased body weight; Uncommon: changes in laboratory tests of liver function, hyponatremia, syndrome of insufficient secretion of antidiuretic hormone.
From the cardiovascular system: arterial hypertension, hyperemia of the skin; Uncommon: postural hypotension, tachycardia.
From the nervous system: unusual dreams, dizziness, insomnia, increased excitability, paresthesia, stupor, increased muscle tone, tremor, yawning; uncommon: apathy, hallucinations, muscle spasms, serotonin syndrome; rare: epileptic seizures, manic reactions, and symptoms resembling neuroleptic malignant syndrome (NMS).
From the genitourinary system: disorders of ejaculation, erection, anorgasmia, dysuric disorders (mainly difficulties at the beginning of urination); Uncommon: decreased libido, menorrhagia, urinary retention.
From the senses: disturbances of accommodation, mydriasis, visual impairment; Uncommon: disturbance of taste.
From the skin: sweating; uncommon: photosensitivity reactions; rare: erythema multiforme, Stevens-Johnson syndrome.
From the hematopoietic system: infrequent: hemorrhages in the skin (ecchymosis) and mucous membranes, thrombocytopenia; rare: prolongation of bleeding time.
Hypersensitivity reactions: uncommon: skin rash; very rare: anaphylactic reactions.
After abrupt withdrawal of venlafaxine or a reduction in its dose, the following may be observed: fatigue, drowsiness, headache, nausea, vomiting, anorexia, dry mouth, dizziness, diarrhea, insomnia, anxiety, increased irritability, disorientation, hypomania, paresthesia, sweating. These symptoms are usually mild and go away without treatment. Because these symptoms are likely to occur, it is very important to gradually reduce the dose of the drug.
Drug interactions
The simultaneous use of monoamine oxidase inhibitors (MAOIs) and venlafaxine is contraindicated. Taking Velaxin® can be started no less than 14 days after the end of therapy with MAO inhibitors. If a reversible MAO inhibitor (moclobemide) was used, this interval may be shorter (24 hours). Therapy with MAO inhibitors can be started no less than 7 days after discontinuation of Velaxin®.
Venlafaxine does not affect the pharmacokinetics of lithium.
When used simultaneously with imipramine, the pharmacokinetics of venlafaxine and its metabolite O-desmethylvenlafaxine (ODV) do not change.
Haloperidol: the effect of the latter may be enhanced due to increased blood levels of the drug when used together.
When used simultaneously with diazepam, the pharmacokinetics of the drugs and their main metabolites do not change significantly. There was also no effect on the psychomotor and psychometric effects of diazepam.
When used simultaneously with clozapine, an increase in its level in the blood plasma and the development of side effects (for example, epileptic seizures) may be observed.
When used simultaneously with risperidone (despite the increase in risperidone AUC), the pharmacokinetics of the sum of the active components (risperidone and its active metabolite) did not change significantly.
Strengthens the effect of alcohol on psychomotor reactions.
While taking venlafaxine, special caution should be exercised during electroconvulsive therapy, as there is no experience with the use of venlafaxine in these conditions.
Drugs metabolized by cytochrome P 450 isoenzymes:
The enzyme CYP2D6 of the cytochrome P 450 system converts venlafaxine into the active metabolite O-desmethylvenlafaxine (ODV). Unlike many other antidepressants, the dose of venlafaxine does not need to be reduced when administered simultaneously with drugs that inhibit CYP2D6 activity, or in patients with a genetically determined decrease in CYP2D6 activity, since the total concentration of the active substance and metabolite (venlafaxine and EDV) will not change.
The main route of elimination of venlafaxine involves metabolism by CYP2D6 and CYP3A4; therefore, special caution should be exercised when prescribing venlafaxine in combination with drugs that inhibit both of these enzymes. Such drug interactions have not yet been studied.
Venlafaxine is a relatively weak inhibitor of CYP2D6 and does not suppress the activity of the CYP1A2, CYP2C9 and CYP3A4 isoenzymes; therefore, it should not be expected to interact with other drugs that are metabolized by these liver enzymes.
Cimetidine suppresses the first-pass metabolism of venlafaxine and does not affect the pharmacokinetics of O-desmethylvenlafaxine. In most patients, only a slight increase in the overall pharmacological activity of venlafaxine and O-desmethylvenlafaxine is expected (more pronounced in elderly patients and with impaired liver function).
Clinically significant interactions of venlafaxine with antihypertensive drugs (including beta blockers, ACE inhibitors and diuretics) and antidiabetic drugs were not detected.
Drugs bound to plasma proteins: Plasma protein binding is 27% for venlafaxine and 30% for EDV. Therefore, it does not affect the concentration of drugs in the blood plasma that have a high degree of protein binding.
When taken simultaneously with warfarin, the anticoagulant effect of the latter may be enhanced.
When taken concomitantly with indinavir, the pharmacokinetics of indinavir changes (with a 28% decrease in the area under the AUC curve and a 36% decrease in the maximum concentration Cmax), but the pharmacokinetics of venlafaxine and EDV do not change. However, the clinical significance of this effect is unknown.
Velaxin overdose, symptoms and treatment
Symptoms: ECG changes (increased QT , bundle branch block, expansion of the QRS ), sinus and ventricular tachycardia, bradycardia, hypotension, convulsions, impaired consciousness. In some cases, fatalities due to overdose have been reported when high doses of venlafaxine were taken concomitantly with alcohol and/or other psychotropic drugs. Treatment: there is no specific antidote. Gastric lavage and the use of activated carbon are indicated. Inducing vomiting is not recommended. It is necessary to ensure airway patency, adequate ventilation and oxygenation. Monitoring of ECG and vital body functions is recommended, as well as supportive and symptomatic therapy. In case of overdose, the possibility of the patient taking several psychotropic drugs simultaneously should be taken into account. Venlafaxine and EDV are not eliminated by dialysis.
Velaxin (Venlafaxine)
In most patients, an overdose of Velaxin manifests itself only in mild symptoms. However, severe toxicity has been reported, with the most common symptoms including CNS depression, serotonin toxicity, seizures, or cardiac conduction disturbances. The toxicity of Velaxin appears to be greater than that of other SSRIs, and the lethal toxic dose is closer to that of tricyclic antidepressants than to SSRIs. Doses of 900 mg or more are likely to cause moderate toxicity. Deaths have been reported only after taking very large doses. Plasma concentrations of Velaxin during overdose in survivors range from 6 to 24 mg/L, while levels leading to fatalities are often in the range of 10-90 mg/L. On 31 May 2006, the UK Medicines and Healthcare Products Regulatory Agency (MHRA) completed its review of the latest safety data relating to Velaxin and in particular the risks associated with overdose. They suggest the need for specialist supervision in cases of severe depression or hospitalization for patients who require a dose of 300 mg or more; cardiac contraindications are more focused on high-risk groups; patients with uncontrolled hypertension should not take Velaxin and regular blood pressure monitoring is recommended for all patients; In addition, it is necessary to monitor updated recommendations regarding possible drug interactions. On October 17, 2006, Wyeth and the FDA notified health care professionals of changes to the overdose/human study information for the drug Effexor (Velaxin) for the treatment of major depressive disorder. During post-marketing research, there have been reports of Velaxin overdose, mainly in combination with alcohol and/or other drugs. Published retrospective studies suggest that overdose with Velaxin may be associated with an increased risk of death compared with SSRI antidepressants, and a reduced risk compared with tricyclic antidepressants. Healthcare professionals are advised to prescribe Effexor and Effexor XR in the smallest number of capsules possible and monitor the patient closely throughout treatment to reduce the risk of overdose. An article published in 2002 in the British Medical Journal by Dr. Nicholas Buckley and colleagues from the Department of Clinical Pharmacology and Toxicology at Canberra Hospital, Australia, who studied the fatal toxicity index (deaths per million prescriptions) suggests that the fatal toxicity of Velaxin is higher than that of Velaxin. than the toxicity of other serotonergic antidepressants, but similar to some of the less toxic tricyclic antidepressants. Overall, scientists say there is a serious risk of toxicity from an overdose of Velaxin, with reports of death, arrhythmias and seizures. They argue, however, that these data are open to criticism, noting that mortality data may be influenced by previous data and that "less toxic" drugs may be prescribed predominantly to patients at high risk of poisoning and suicide, but are also less likely to should be reported as the sole cause of overdose death. It is also assumed that drugs in case of overdose are taken with the same frequency and in equal quantities. The scientists suggest that "clinicians consider all factors in their patients that reduce or offset these risks before prescribing Velaxin." On February 27, 2007, the Vancouver Sun reported that the BC Drug and Poison Information Center issued a warning to doctors that the drug poses a significant risk of overdose death, stating that Velaxin "is more toxic than originally thought." A physician in the Department of Pharmacy Services, College of Pharmacy, Medical University of South Carolina, Charleston, South Carolina, reported the death of a 39-year-old patient from a 30-g overdose. To understand what we're talking about, imagine if a patient were to take 66 infrequently prescribed high-dose 450 mg tablets, or 400 commonly prescribed 75 mg tablets.