Often grandmothers, neighbors and even online forums come to the rescue, and sometimes a young mother has to rely only on herself. What, for example, should you do if your baby refuses to eat or eats very reluctantly? After all, a baby only needs to lose 10% of its weight (which is 500-700 grams) to be on the verge of death! How to deal with the problem yourself or understand that the baby needs the help of a doctor, says the book of the famous pediatrician, 1st category doctor Yuri Belopolsky, “Emergency Care at Home. Mom makes a diagnosis.” We are publishing an excerpt from this book.
Should I worry?
A person’s appetite depends on a number of factors, primarily determined by individual metabolic characteristics. A child's appetite is controlled by the body's needs. The growth process of a child is not uniform: in the first year of life, in adolescence, growth hormone, thyroid and parathyroid hormones, sex hormones are produced in larger quantities, the child grows actively, and appetite increases. Appetite also depends on the level of energy expenditure: the more energy a child spends, the better his appetite. Changes in appetite are normal as long as your child is active and growing normally. However, a lack of appetite in a child who appears unhealthy or is growing slower than expected should be a cause for concern and a visit to the doctor.
Child masturbation and child masturbation: psychological or medical problem?
The problem of masturbation in a child may have one or more reasons, and it is important to find out what order they are: psychological or medical? If you clearly and correctly determine the source of symptoms, then this problem is almost always solved quite quickly and effectively.
Types of masturbation in children:
Infant masturbation occurs in the first year of life. It is unconscious in nature and is more common in girls than in boys. It involves stretching and crossing the legs, strong muscle tension followed by relaxation.
Symptomatic masturbation in children - in response to itching or pain in the groin area caused by various reasons, such as helminthiases, dermatoses, infectious somatic diseases, as well as failure to maintain the necessary body hygiene.
Frustration childhood masturbation - in situations of emotional deprivation (expressed in the child as a feeling of helplessness and rejection) and discomfort associated with pathological relationships in the family.
Neurotic masturbation in a child can be associated with neuroses of varying degrees. Also in cases of organic pathology of the brain (increased intracranial pressure, consequences of birth/intrauterine hypoxia or trauma). Obsessive masturbation is possible as a consequence of damage to higher mental functions and insufficient inhibition of primary excitation.
Inculcated masturbation is when a child imitates one of the children in kindergarten and subsequently uses this habit while at home.
Pseudo-masturbation - if it is not permanent and pathological, then such masturbation in children is a completely normal phenomenon in the process of a child learning about the world and his body.
You can also identify the following types of masturbation according to the degree of its intensity:
- Episodic (occurring rarely, most often under the influence of some disturbing situations and stress)
- Regular (constant, obsessive, regardless of external circumstances)
- Excessive (about several times a day)
Symptoms and causes
Boys often rub their genitals on pillows, place a blanket between their legs, can “spring” their genitals while lying on their stomachs, play and fiddle with their genitals.
Girls bring their thighs together and apart, rub against wool or fur, and use a stream of water from the shower. They may also rub their genitals with their hands, pull on and pull down their panties or trousers.
A child touches his genitals and can masturbate from the first months of life, regardless of gender. In this way, the child can “extinguish” increased nervous excitability due to various reasons.
Masturbation may be due to medical problems: increased intracranial pressure, hypoxia and birth trauma in the past or epilepsy. In short, any neurological pathology associated with increased excitability and anxiety. Because the child unconsciously finds the genitals and uses masturbation as a tool to relieve nervous excitement. After masturbation, the child temporarily recovers from the state of psychological discomfort and repeats masturbation a certain number of times a day, thus making it a habit.
Also, child masturbation can be caused by psychological problems, such as: separation from mother in infancy and early age, a very tense psychological situation in the family (even in the first year of life), lack of tactile and emotional contact with mother, too strict parenting style and harsh punishments , emotional or physical overload, or some organic precondition.
Precocious sexual development (PPD) is often accompanied by early pre-pubertal masturbation. Often, in this case, a congenital or acquired at an early age lesion of the deep structures of the brain, or a mental pathology that requires treatment or correction, is diagnosed.
Who should I contact about masturbation in a child: a psychologist or a doctor? First you need to determine what are the reasons for this “bad” habit? If these behavioral factors and symptoms appear only occasionally, causing concern to parents, then a child psychologist or neuropsychiatrist can help. Timely correction with the help of psychotherapy or the creation of behavioral rules and the correct response, as well as changing the psychological situation in the family to the most harmonious for the child, will bring positive results quite quickly. If a medical factor is present, it is recommended to contact a pediatric neurologist or child psychiatrist, who will prescribe correct and effective treatment that is suitable for your child. In case of a controversial situation, we advise you to go through a consultation of three doctors who, in one visit, will find the true cause of the problem and give recommendations from several specialists at once.
Possible causes of poor appetite
► Lack of a constant feeding schedule. If the child is not used to eating at a certain time.
► Sweet snacks. The more sweets your baby eats between meals, the harder it will be to get him to eat a bowl of soup or a vegetable dish.
► Illnesses of the child. When an illness occurs, a child’s appetite decreases significantly, as all the body’s strength is spent fighting the disease. In this case, you should not force food on your baby.
► Emotional experiences. During these periods, parents' attention should be focused on the child's condition, and not on the amount of soup he has eaten.
Experts' opinion
Pediatricians clarify that in most cases, parents do not complain about a complete lack of appetite, but only about its selectivity.
Children refuse porridge and soup, are reluctant to eat meat, and demand cookies or candy. This situation can be dealt with without medication. There is no need to force the child to eat or give in to the child and allow him to have a snack. You should wait until you truly feel hungry. There is no need to constantly remind you about food. After some time, the baby himself will ask for food and will happily eat the offered dish.
Is there a risk of malnutrition?
There is little risk that a child who restricts his diet will lack nutrients. The child's body will not starve if food is available. The need for a certain amount of food is expressed in thermal units - calories (the amount of heat that can increase the temperature of 1 liter of water by 1 ° C). The Institute of Nutrition of the Academy of Medical Sciences of Russia recommends caloric expenditures for children of different ages:
► From 3 to 5 years - 1500 kcal.
► From 5 to 8 years - 1800 kcal.
► From 8 to 12 years - 2000 kcal.
► From 12 to 16 - 2400 kcal.
Additional recommendations
There are tricks that will help establish normal nutrition for even the most picky baby.
Experienced mothers advise purchasing bright children's dishes for their children. Children are more likely to eat from a plate with characters from their favorite cartoons. If the problem is the taste of some products, then it is recommended to grind them. The child will not notice small pieces of onion in soup or stir-fry. The main thing is not to try to impose your personal taste preferences and regime on children. Try different ways to increase appetite, offer children a choice, respect their opinion, and positive results will not keep you waiting.
Children and vegetarianism
Most experts believe that a child's food should be mixed (meat-dairy-vegetable) with sufficient amounts of vitamins and minerals, and do not recommend vegetarianism for children. Plant foods have a number of advantages, but cannot replace meat, fish, milk, and eggs in a child’s diet. These products contain substances necessary for the child that are not found in plant foods. First of all, these are complete animal proteins, some vitamins and minerals: B vitamins, vitamin D, calcium, iron, zinc. Fish is a source of vitamins PP, group B, as well as phosphorus. A lack of these substances threatens the child with anemia and decreased hemoglobin, which in turn leads to a deterioration in the supply of oxygen to tissues. Vegetarianism is contraindicated for children with low hemoglobin levels.
Proponents of vegetarianism believe that a growing body feels better in the absence of meat food. It has been proven that people who adhere to vegetarianism are less likely to develop diseases of the cardiovascular system and certain types of cancer. Vegetarians practically do not suffer from obesity. A vegetarian diet is high in dietary fiber, vitamin C and beta-carotene. This diet does not contain animal fat - a source of cholesterol and saturated fats, which cause the formation of specific deposits on the walls of blood vessels - atherosclerotic plaques, which narrow the lumen of the vessel and impair blood circulation in tissues and organs.
Families that embrace vegetarianism should take special care to ensure that the child’s body receives all the necessary substances.
A lack of any nutrients can affect growth retardation, physical and mental development, as well as disruption of the formation of the bone skeleton and teeth. This is especially true for children of primary school age.
Relevance
Feeding difficulties and decreased appetite in children are common complaints from parents at pediatric appointments.
However, in many cases, malnutrition remains beyond the attention of pediatricians and leads to the development of nutritional status disorders. Lack of awareness among pediatricians about eating disorders in early and preschool age prevents the timely detection and correction of these conditions. The problem of children's eating behavior has been actively studied in the last decade; the causes of eating disorders in children are being sought and approaches to their correction are being developed. Feeding difficulties (R63.3) – a spectrum of conditions that is characterized by impaired feeding in a child without neuropsychiatric disorders. It is diagnosed both in healthy children and in children with pathology of internal organs and/or the central nervous system (CNS). In most cases, difficulties when feeding a young child are the norm, are mildly transient in nature and disappear as they grow older - often without consequences for the health and development of the child. Feeding difficulties that persist for more than 1 month are of clinical significance [1–3].
Eating disorder in children of early and preschool age (F98.2) is of a neuropsychic nature with features of refusal and extreme selectivity on their part in food without pathology of internal organs and the central nervous system in response to the offer of adequate food by a reasonable and competent person carrying out caring for him. It may be diagnosed if a child exhibits unusual eating behavior or has lost or failed to gain weight for at least 1–3 months [1–3].
Etiology
The occurrence of difficulties with feeding a healthy child does not depend on gender, ethnicity and family income level [4–6].
The main causes of eating disorders and difficulties in feeding young children [1, 4, 7, 8]:
- misunderstanding by parents of eating behavior and the child - the so-called. “imaginary” violations;
- behavioral disorders, incl. neuropsychiatric disorders;
- pathology of internal organs or central nervous system;
- use of forced feeding tactics by parents.
Prevalence
Due to the lack of uniform classification and diagnostic criteria, the true prevalence is unknown. More than 50% of parents of healthy young children believe that their child eats poorly and about 90% of parents of children with developmental disorders of various origins experience difficulties feeding their child [7, 9, 10].
Long-term (more than 1 month) persistent feeding difficulties are observed in 20–30% of healthy children of early and preschool age [7]. In most of them, they are caused by mild transient forms of eating disorders or misinterpretation by parents of the child’s eating behavior, and only in 1–5% by a severe form of eating disorder: eating disorder in infancy and childhood [11].
Implications for child development and health
Chronic deficiency of macro- and micronutrients. Characteristic for children with selectivity in food. These children show reduced intake of almost all macro- and micronutrients, especially folic acid, dietary fiber, vitamins D, E and C [10, 12, 13].
Retarded physical development. Children with decreased appetite or food selectivity typically have lower body weight than children without feeding problems [14]. As people get older, the incidence of stunting and underweight can reach 50% [12].
Decreased cognitive function.
At an older age, children with reduced appetite or selectivity in food often have a reduced ability to learn, attention, memory and visual perception suffer [12].
Chronic stressful situation in the family. Insufficient food intake by a child causes a feeling of anxiety and fear in parents, who often try to force feed him. If parents exert constant psychological pressure on the child, forcing him to eat, a vicious circle is created that aggravates existing feeding difficulties [14].
Diagnostics
The diagnostic algorithm is presented in the figure. The first step is to determine the leading deviation in the child’s eating behavior: decreased appetite, selectivity in food or fear of eating [1]. Further tactics are aimed at excluding pathologies of internal organs, the central nervous system or neuropsychic disorders characteristic of this deviation in eating behavior. Their presence is indicated by warning signs - specific symptoms, the identification of which requires immediate referral of the patient for additional examination or specialized treatment. The absence of warning signs indicates the presence of mild transient eating disorders [1].
When collecting anamnesis, it is necessary to find out information about the pace of physical and psychomotor development, the presence of chronic diseases and functional disorders, past illnesses, hospitalizations, medical procedures (tube feeding, interventions in the oral cavity and/or pharynx). The nutritional history should include information about the child’s nutrition from the moment of birth (types and mode of feeding, their duration and reasons for change; age of introduction of complementary foods, its types, sequence of administration, tolerance, methods and methods of administration), about the mode and composition of nutrition at the present time, about the presence of unusual eating behavior.
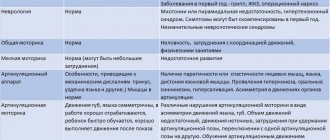
Clinical examination should begin with anthropometric measurements and assessment of nutritional status according to World Health Organization criteria [15]. A physical examination of the child includes an assessment of the condition of organs and systems, neurological status and the level of psychomotor development, aimed at identifying warning signs - symptoms of diseases of the respiratory system, cardiovascular and endocrine systems, gastrointestinal tract, neurological pathology, atopy and developmental abnormalities. It is also necessary to pay attention to the presence of clinical signs of deficiency of macro- and microelements.
Children with a normal level of physical and psychomotor development, the absence of clinical symptoms of diseases, and signs of macro- and micronutrient deficiency do not need laboratory tests [1].
Eating disorders and their correction
Decreased appetite
Imaginary decreased appetite.
This category includes children with normal indicators of physical development, whose parents show excessive concern about poor appetite and the amount of food the child eats [1]. In such children, the appetite and amount of food consumed meet their needs for normal growth and development, but do not meet the expectations of their parents.
In this regard, parents of such children resort to incorrect feeding methods (forced, long-term, mechanistic - feeding strictly according to a schedule, regardless of whether the child is hungry, etc.), which causes difficulties in feeding [1, 16].
Children in this category do not require correction or nutritional support [1]. The child's parents need to explain growth patterns and teach the basic principles of feeding infants and preschool children. If parents are excessively anxious, consultation with a clinical psychologist is recommended.
Active children with little interest in food (infantile anorexia). Children in this category are characterized by a sharply reduced appetite, refusal to eat, delayed physical development and/or severe malnutrition in the absence of any pathology of the organs or central nervous system [1].
Diagnostic criteria [16]:
- an infant or young child refuses to eat an adequate amount of food for at least a month;
- refusal of food often begins during the transition to independent feeding - (6 months - 3 years);
- the child does not show feelings of hunger, interest in food and the process of eating, but at the same time is actively interested in the environment and communicates with parents;
- there is a delay in physical development;
- refusal to eat is not a consequence of trauma of any origin;
- refusal of food is not associated with pathology of internal organs and the central nervous system.
Children with infantile anorexia are active, easily excitable, often hyperactive, they have a reduced hunger threshold, and are satisfied with small portions [14]. They are characterized by inconsistent refusal of food (they may show interest in food on one day and refuse on another). Parental concerns about child development and force feeding further increase feeding difficulties [14].
Children in this category need the help of a child psychotherapist and/or clinical psychologist to eliminate a conflict situation and normalize parent-child relationships, as well as a nutritionist to correct nutritional status [1, 14]. The goal of therapy is to help the child recognize feelings of hunger and satiety and respond appropriately to them. Nutritional recommendations should focus on feeding pattern and duration of feeding [1]:
- The diet should include no more than 4 meals a day, in between them only water can be offered;
- the duration of a meal cannot exceed 20–30 minutes;
- Shared meals should be recommended, during which parents should be an example of the right attitude towards food and healthy eating, and also firmly set boundaries for the child’s behavior at the table.
If there is a deficiency of body weight, it is necessary to prescribe specialized products for nutritional support in order to enrich the diet with basic macro- and micronutrients and vitamin-mineral complexes. Specialized products should not replace meals, but complement them. It is advisable to use hypercaloric products (about 150 kcal per 100 ml of mixture).
Pathology of organs and systems as a cause of decreased appetite. The most common causes of decreased appetite [1, 7–9]:
- structural anomalies - anatomical defects in the structures involved in chewing and swallowing food. These include developmental anomalies of the nasopharynx and oropharynx, larynx and trachea, esophagus;
- pathology of the gastrointestinal tract: esophagitis, incl. eosinophilic, gastritis, gastroesophageal reflux, food allergy, celiac disease, intestinal motility disorders, intestinal form of cystic fibrosis;
- chronic heart and lung diseases;
- diseases of the nervous system – pathology of the central nervous system and diseases of the neuromuscular system: cerebral palsy, muscular dystrophy, damage to the cranial nerves, disorders of mental and psychomotor development;
- endocrine and metabolic diseases - hypothyroidism, fructosemia, etc.
In cases where decreased appetite and refusal to eat are a consequence of pathology of the internal organs or the central nervous system, treatment of the underlying disease is necessary.
Selective appetite
Imaginary selective appetite.
This category includes children whose food selectivity is associated with an age-related feature of eating behavior – food neophobia [1]. Most often, such children refuse to eat vegetables and fruits [17]. The reason for refusal to use is the appearance, not the taste of the product. Children in this category do not require correction or nutritional support. Feeding and nutrition recommendations should focus on a neutral psychological environment during feeding, constant introduction of new foods and shared meals. Each new product should be offered 10–15 times without forcing the child to try it [1, 7].
Moderate selectivity in food. This category includes a large group of healthy children, who are commonly called “little children” [1]. Most young children have normal physical development.
General features of eating behavior of young children [1, 18]:
- eating a limited number of foods;
- refusal to eat both familiar foods and new foods and dishes;
- refusal to eat food of a certain consistency, smell, appearance;
- preference for sweet or fatty foods;
- preference for liquid foods;
- slow pace of eating;
- holding food in the mouth for a long time.
Young children have persistent food preferences and unloved foods, which they reject with anger or irritation [18]. Unlike children with food neophobia, repeated offers of rejected food do not produce the desired result [1]. Parents also often describe conflicts with their children during and about meals [16]. The conflict situation during meals is given key importance in the development of feeding difficulties for a small child.
If the child’s diet is not sufficiently balanced, vitamin and mineral complexes are indicated [1]. The introduction of specialized products into the diet is necessary if changes in the child’s nutritional status are detected. If parents express concern about the child’s malnutrition, it is possible to use isocaloric mixtures containing complete protein and micronutrients in addition to the daily diet as “food insurance.” This helps reduce parental anxiety and maintain normal nutritional status. In most cases, the assistance of a clinical psychologist is required. Feeding recommendations should focus on a neutral psychological environment during feeding and the constant introduction of new foods.
Parents should be recommended the following activities [7]:
- offer new food in minimal quantities and repeatedly (10–15 times);
- place new dishes within the child’s reach without offering to try them;
- if, when offered a new dish, the child shows signs of sensory aversion (the appearance of vomiting, etc.), this product should be excluded from the diet;
- involve the child in the cooking process;
- give dishes an attractive and “appetizing” appearance.
A high degree of food selectivity is currently considered an avoidant/restrictive food intake disorder (ARFID). This disorder was first identified in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013 [19]. The International Classification of Diseases, 11th Revision, provides for the introduction of AFRID as a separate disease under the eating disorders section.
The disorder is most typical for children of early and preschool age, but can persist into later age periods.
Diagnostic criteria for AFRID include:
- An eating/feeding disorder (eg, marked lack of interest in food; avoidance of food based on sensory characteristics; worry about adverse effects of food intake) that results in persistent dietary energy and nutrient deficiencies and is associated with one or more of the following consequences:
- significant loss of body weight (or inability to achieve the expected increase in body weight, or insufficient dynamics of physical development in children);
- significant nutrient deficiency;
- dependence on enteral nutrition or oral nutritional support;
- marked change in psychosocial functioning.
- Malnutrition cannot be explained by a lack of available food or cultural/religious dietary practices.
- Eating disorders are not associated with the presence of anorexia nervosa or bulimia and are not accompanied by a distortion of body image and a desire to lose weight.
- Malnutrition is not caused by a concomitant somatic illness or other mental disorder. In the case of AFRID development against the background of an intercurrent disease that makes it difficult to eat/assimilate food, the degree of malnutrition is more severe than usual for these diseases [20].
Treatment of such patients requires a multidisciplinary approach with the involvement of a neuropsychiatrist, psychotherapist, clinical psychologist, gastroenterologist and nutritionist in a specialized center.
Pathology of the central nervous system. Selective food consumption can be observed in neurological diseases of hypoxic, hereditary, metabolic and unknown origin [1, 7, 9]. Selectivity in food can be associated with both increased or decreased sensitivity of the oral mucosa to the tactile properties of food, and with a delay in the formation of oral motor skills [7]. Children with a selective appetite of organic origin try to accept food put in their mouth, but have difficulty eating it, regardless of its consistency [1]. Treatment of such patients requires a multidisciplinary approach with the involvement of a neuropsychiatrist, psychotherapist, clinical psychologist, speech therapist, gastroenterologist and nutritionist in a specialized center.
Fear of eating
This condition is defined as “post-traumatic feeding disorder” (I. Chatoor, 2007) [16]. There are three main causes of fear of food: a one-time negative experience in the form of some kind of trouble while eating (most often choking on food), painful manipulations in the oral cavity or intubation, prolonged feeding through a tube and/or little experience of feeding by mouth. , and/or the child experienced a feeling of fear when starting oral feeding [16]. The purpose of the correction is to reduce the child’s level of anxiety and restlessness associated with food intake. At the stage of initial consultation with a pediatrician, it is necessary to prescribe nutritional support.
Conclusion
Thus, the problem of difficulties in feeding children of early and preschool age seems to be very relevant due to its high prevalence, tendency to a long course and high risk of disruption of the physical and mental development of children. To solve the problem, joint work of pediatricians, gastroenterologists, nutritionists, clinical psychologists and psychotherapists is necessary. Treatment should be comprehensive with nutritional correction to achieve and maintain normal nutritional status.
Should I force my child to eat?
Never, under any pretext, force your child to eat. If you force your child to eat something he doesn't like, conflict may occur. Continue to offer him a variety of foods, but don't get angry or upset if he refuses it.
Check whether the child eats additional sweets, etc. between meals. If your child looks sick or is growing slower than expected, consult a doctor. It should be remembered that what is much more dangerous for health is not a temporary refusal to eat, but an excessive or monotonous diet.
Child pulls out and eats hair (Trichotillomania)
In case of manifestation of trichotillomania syndrome, we recommend that you consult a neurologist or a pediatric psychoneurologist. Medical and psychological assistance will be effective, and the faster the causes are found, the faster and more effective the treatment will be to eliminate these symptoms.
One of the most serious and profound neuroses in a child is when he tears out his hair. Most often, children tear out hair on their heads, but in some cases it is even possible that eyelashes and eyebrows are pulled out and eaten. Trichotillomania, in most cases, is a type of obsessive-compulsive disorder.
Hair pulling occurs mainly on one area of the head that is convenient for pulling out hair. Neighboring areas of the head are not subject to this procedure, but after regrowth the hair is pulled out again. Sometimes a child can pull out hair from the entire surface of the head, which leads to total baldness.
One of the versions of the psychological reasons for hair pulling is a protective-adaptive reaction, similar to the “lizard tail” phenomenon: pull out what is in the way in order to return to your normal state renewed.
In early preschool age, hair pulling occurs as an involuntary action. The first interaction with hair - twisting and tugging it - begins in newborn children, at the time of breastfeeding or at the moment of falling asleep in the mother's arms, that is, at the moment of their psychological comfort. Emotional stress, anxiety and fear, as primary neurotic reactions, can prompt the child to try to perform these actions more often in order to regain a state of trust and relaxation.
During school and adolescence, awareness of the habit comes and attempts are made to get rid of the habit of pulling out (pulling out and eating) hair. There is a tendency towards an obsessive state. A whole ritual of twirling the hair on the finger is created, with pulling, chewing and even swallowing the torn hair bulb. If a child eats plucked hair, this is a signal of worsening trichotillomania syndrome.
In some cases, trichotillomania is a manifestation of auto-aggressive actions among obsessive-compulsive disorders (obsessive states). In this case, it can be combined with low self-esteem, feelings of inferiority, guilt and self-flagellation, and self-rejection.
Also, hair pulling can be a defensive reaction to any irritation in the head area, especially in combination with increased anxiety.
The causes and provoking factors of trichotillomania may be:
- obsessive states
- schizophrenia
- itching or pain in the head area
- increased intracranial pressure
- diseases associated with brain damage (consequences of birth or intrauterine hypoxia, birth trauma, consequences of concussion, increased intracranial pressure)
- lack of iron and copper in the body
- deep mental traumas and neuroses
- cysts and neoplasms in the brain
- autism manifested as stereotypies
How to distinguish baldness with trichotillomania from baldness with true alopecia (hair loss)
Trichotillomania is a type of alopecia (true endocrine, autoimmune or neurotrophic baldness), but is caused not by internal physiological reasons, but by artificial means.
There are main signs by which trichotillomania can be distinguished from alopecia:
- With trichotillomania, the surface of the baldness is uneven and located in one area.
- With alopecia, the surface of the bald areas is very even and smooth, or is covered with evenly growing hair in remission.
Baldness due to trichotillomania can be distinguished from alopecia due to alopecia using dermatoscopy and trichoscopy. These are studies of skin and hair using an optical instrument with various options of polarizing light. In our clinic, dermatoscopy and trichoscopy are performed by dermatologists.
How to improve a child's appetite?
► Intensify the child’s energy expenditure: he benefits from physical education, active games, walks in the fresh air, and it is also necessary to prevent overheating.
► Do not overfeed. Do not force him to eat, so as not to cause a feeling of aversion to food. Should I force my child to eat?
► Parental example is the best remedy for a child’s poor appetite. If possible, have lunch as a family. Eat with appetite the same food you offer him.
► Sweets and snacks are the enemy of good nutrition. Offer your child sweets only after the main course, for tea. If your child gets hungry between meals, offer him fruit, nuts or dried fruit.
You can read the author of the book, pediatrician Yuri Belopolsky in the CONFERENCES section >>>
Ways to instill in children a love of healthy food
A child will eat with pleasure if he is introduced to light and healthy foods from an early age.
Lead by example
Only parents can show the correct attitude towards food.
All family members, especially adults, should eat according to a schedule, avoid unhealthy snacks, and not be distracted from eating at the table.
Don't let it be manipulated
Promising your baby sweets, cartoons or gifts after meals is a mistake. The child will quickly understand that parents can be blackmailed. It will be difficult to correct behavior in the future.
Show that healthy food can be tasty
Healthy eating isn't just about unsightly cereal and tasteless vegetables. Creativity is important. Don't limit yourself to standard recipes. It’s better to use your imagination and involve your child in the cooking process.
It is recommended to involve your child in cooking together.
Little Conservatives
Young children are extremely conservative in their eating habits and preferences. For this reason, expanding their diet must be done very carefully. In particular, if you are going to offer your baby a new type of food, try to wait until the baby is hungry to do so. This approach will significantly increase the likelihood that the new food will be favorably received by the child.
Young parents should be prepared for the fact that starting from the second year of life (or from the end of the first), many babies like to actively demonstrate their refusal to eat some food. For this age, it is quite typical to love only a few dishes. A child may eat, for example, exclusively fruit or kefir for several days or weeks, and then suddenly “switch” to meat and cheese. At the same time, parents should not be too strict and demanding, trying by all means to ensure that the baby consumes types of food that he does not like. None of the food products can be considered absolutely irreplaceable and therefore almost any of them can be successfully replaced by another. It will be much more productive to focus your efforts on trying to diversify your baby’s diet as much as possible. This will, to a certain extent, ensure the supply of most of the nutrients a growing child needs.
The real problem arises only if the child for a long time and systematically completely refuses all types of foods necessary to ensure the completeness of his diet - for example, any vegetables, fruits or grain foods. In this case, it makes sense to change the culinary features of preparing dishes or to be creative (cutting food in the form of unusual geometric shapes, etc.), which young children really like.
Leave the choice to the child
Food cannot serve as a way to manipulate a baby. The basic rule that determines the strategy for approaching feeding young children can be formulated as follows: “If you don’t like it, don’t eat it!” Back in the early 1980s, American pediatrician Clara Davis conducted a famous experiment by allowing a group of one-year-old children to freely choose food from a large selection of food options. It must be said that the parents did not take the slightest part in the process of feeding the babies. The results of this experiment were simply stunning. It turned out that all the children consumed a so-called “well-balanced diet.” By this term, pediatricians understand a diet that includes foods from the four main food groups every day.
Typically, children who have reached the age of one are already able to independently build their own diet, ensuring the physiological consumption of all nutrients necessary for the body. In this case, it is not so important at what time of day or at what feeding the specified products are given.
It is important to regularly monitor such indicators of the baby’s physical development as body weight and height. If you are at a loss because you don’t know how to interpret the child’s physical development, ask your pediatrician to evaluate his parameters (using special tables). At some stage of development, many young children are “poor eaters,” but in most cases the problem comes from the baby's parents expecting the child to follow certain eating patterns (which he temporarily rejects). With a flexible and natural approach, this problem usually disappears soon.
Loss of appetite due to illness
Some recommendations when a child is sick:
- The child should be given plenty of fluids to drink, especially if the disease is accompanied by vomiting or diarrhea. The liquid should not be too cold or hot. Carbonated drinks and liquids with strong tastes that irritate the mucous membrane of the stomach and intestines should not be given.
- Do not give cow's milk or other dairy products if your child has signs of gastroenteritis.
- Although there is usually no need to follow a strict diet, avoid heavy, protein-rich foods when your child has an upset stomach.
- Offer your baby some of his favorite foods (to encourage him), but the amount of food should be much less than usual. Although, since the child’s body is weakened during this period, it is likely that he himself will not want to eat too much.
- Unfortunately, decreased appetite does not always reflect harmless and completely natural characteristics of a growing child’s body. A decrease or loss of appetite is often one of the first signs of ill health. Nevertheless, you should not dramatize the situation and show excessive concern about this, since usually the illness (usually a trivial cold, called acute respiratory infections) does not drag on for too long.
- If you suspect that the child is unwell, you need to carefully monitor him for several hours. In this case, special attention is paid to pallor, changes in behavior (this can be either excessive excitability or excessive apathy), and fatigue that is unusual for a baby. Of course, it would be useful to measure the child’s body temperature (preferably more than once). If necessary, you should promptly consult a pediatrician.
- In some cases, loss of appetite can be explained by some specific health problems of the child, including conditions of food intolerance or allergies to certain foods that parents “stuff” the baby with. Contact your pediatrician instead of trying to identify and eliminate the food allergen yourself. As a result of such amateur actions, you can deprive the child of some essential nutritional components necessary for the full development of the baby.