Photo: google.ru
— Nina Alekseevna, how careful should the relatives of a person diagnosed with viral hepatitis B be? Are there any “safety precautions” for family members?
— A person suffering from hepatitis B can be contagious to family and friends. This risk is especially great at the acute stage. It occurs a short time after infection. This is the result of a violent immune response to the virus. During this period, there may be no symptoms or they may resemble a cold: fever, muscle aches, joint pain. Sometimes jaundice occurs in the acute stage. Jaundice is not a diagnosis, but a symptom: yellowing of the skin and sclera of the eyes. It happens not only with viral hepatitis. For example, if a stone blocks the bile duct, then the person will also have jaundice. Jaundice occurs with hepatitis A, B, and C. When a person sees himself yellow, he usually gets very scared, and everyone around him gets scared, because they suspect that it is something contagious. As a rule, in this state a person is admitted to the hospital, where he learns the exact diagnosis, as well as the fact that he is truly contagious.
“It is advisable for everyone to be vaccinated, not just family members of the sick person. Hepatitis B is highly contagious. Many people suffer from it and don’t know it.”
If a person knows about the diagnosis, but remains treated at home, he needs to behave very carefully. Everything related to blood - toothbrushes, nail scissors, razors, towels, pads - should be isolated as much as possible from healthy family members. Sexual contacts at this moment should only be protected. Close contact with children must be avoided, since a mother with jaundice who is breastfeeding is highly likely to infect him. Mothers often infect their children in early childhood, and not only during childbirth, but also in everyday life during the acute stage of hepatitis, when they feed the child, care for him, hug him, kiss him. That is, any situations associated with contact of a patient’s biological fluid with damaged mucous membranes and skin of another person are dangerous.
- But here you can get to the point where you are afraid of everything...
— Yes, of course, it is important not to dramatize and not turn life into constant protection from the virus. For example, there is no need to go crazy with everything related to cooking and eating. The hepatitis B virus is not transmitted through food. It dies when it enters the digestive system. But sometimes the fear of patients goes far: people are afraid to even wash things in the same washing machine, much less eat food prepared by an infected person.
— Is it possible to somehow determine at what point a person is most contagious and when you need to be as vigilant as possible in everyday life?
- Of course, it is possible - with the help of standard and affordable blood tests. The more virus there is in the blood (and therefore in all other human fluids, for example in saliva, semen), the more infectious the person is. When a person’s disease is inactive or artificially inactive under the influence of a drug, then the likelihood of infecting another is negligible. Although there is still a possibility, since in the most inactive state the virus is still present in the body. Therefore, if a person is already being treated, then you cannot say: “Finally, you are not contagious - do what you want!” All family members, all sexual partners, all people who are in close contact with him - one where an exchange of blood particles and biological fluids is possible - should be vaccinated.
— If one of the partners has hepatitis B and the other is vaccinated, can they have unprotected sex?
- Yes. Vaccination, if carried out correctly and confirmed by a blood test that it has had its effect, will definitely protect a healthy person. And partners can have unprotected sex life.
— Is it better to vaccinate as soon as it becomes known that one of the partners is infected?
— Yes, but first you need to undergo tests that will show that your partner has not yet been infected. Then vaccination is done. After this, you need to be tested again to understand whether the healthy partner has received immunity against hepatitis B. If immunity is obtained, you can live peacefully and not worry about anything: this person will no longer get hepatitis B.
— Probably, you need to get vaccinated in any case, even if everyone in the family is healthy?
— It is advisable for everyone to be vaccinated, and not just family members of the sick person, since hepatitis B is very contagious. Many people have hepatitis B and do not know about it, because testing for the disease is usually not carried out. As a rule, we only know about those who got sick and did not recover. These are the minority. But the majority got sick and didn’t notice it. Therefore, before vaccination, it is necessary to find out: has the person already been sick? If he was sick, he received immunity naturally; he no longer needed vaccination. If he hasn’t been sick, then he doesn’t have immunity, and then he needs to be vaccinated.
It happens that an adult has been vaccinated, but it was so long ago that he does not remember about it. The algorithm of actions in this case should be as follows: get checked - get vaccinated - get checked after vaccination. If the vaccination works, you can forget about such a problem as hepatitis B. And even if one of your partners is infected, you should not be afraid to be with him, build a family, give birth to children.
However, minimal household caution must be observed. For example, do not share a towel, toothbrush, nail scissors, razors, and so on. But these hygiene rules must be observed by everyone and always, regardless of the presence of illness in the family.
— Vaccination against hepatitis B is included in the calendar from 0 years. How reasonable is this for people not at risk?
— Those who were born from an infected mother are at risk. Such children are vaccinated in the first hours of life, and the later it is given, the greater the danger that the disease will outstrip the effect of the vaccine. Now they are trying to vaccinate everyone in the first hours of life, even if the mother is healthy. This is not necessary; according to the vaccination calendar, a child can receive them in the first months of life. But even if he receives the vaccine in the first hours of life, this is also very good. The main thing is to get a course of vaccinations. People are usually afraid that they can get hepatitis from the vaccine. This is wrong. You need to know that the hepatitis B vaccine does not contain the virus. It contains an artificial protein, which, once in the human body, causes an immune response. This immune response will protect a person from the hepatitis B virus if infection occurs.
— Who would you recommend to get vaccinated or revaccinated first? Are there any studies that show that it’s time to get vaccinated again?
— Those at risk who need to be vaccinated are those born to a sick mother, those who have a family member with hepatitis, those who cannot give up drugs. A special risk group is medical workers who systematically deal with potentially contaminated material. Here I would include people who are in prison, and those who are interested in salon manicures, pedicures, and tattoos. This is such a large group of people. But since the disease is contagious, we need to remember that we all need to be vaccinated! It is difficult to imagine all the situations in which a person can become infected with hepatitis B. After a successful course of vaccinations against hepatitis B, a person receives lifelong immunity and does not need revaccination (that is, a second course). Even if protective immunity declines over the years, it will still be enough to cope with the infection. In our country it is possible to get vaccinated against hepatitis B for free, so you should not miss this opportunity and do it. Remember that you need to be as responsible as possible towards your health and the health of your loved ones!
— If one of the future parents is sick with hepatitis B, can this somehow affect the child? Maybe such couples need special reproductive programs?
- Children can only be infected with hepatitis B by their mother, because they have contact with her blood during childbirth. The virus cannot be transmitted from a father to a child. Therefore, such couples do not need special reproductive programs; their conception occurs in the same way as everyone else. If this couple needs IVF for other reasons, they will be required to provide a certificate from an infectious disease specialist or hepatologist. But the prospects for the reproductive program do not depend on the severity of hepatitis.
— So a woman with hepatitis B does not transmit the virus to her eggs?
- No. There is no hepatitis virus in human germ cells. Therefore, a child can, as a rule, become infected with hepatitis B only during childbirth.
- Larisa Zelinskaya
- Amurskaya Pravda from 10/18/2018
Hepatitis B: carriage or disease leading to cirrhosis and cancer?
Hepatology, the study and development of new treatments for liver disease, has made incredible progress over the past two decades. Methods for accurate virological assessment of the activity of hepatitis C and B viruses in the human body, which are the most common causes of chronic hepatitis, cirrhosis, and liver cancer, have been developed and implemented. So-called “non-invasive” methods have been developed and are widely used, that is, without the use of liver biopsy, diagnosing the degree of liver damage, or establishing the stage of cirrhosis. Even more impressive progress has been made in the treatment of these diseases. We have discussed the problem of hepatitis C many times. One has only to add that a new era is opening in the treatment of hepatitis C - drugs with a direct antiviral effect have been developed and are already beginning to be used, thanks to which it is believed that within a decade it will be possible to achieve one hundred percent effectiveness of treatment. In this article we will talk about hepatitis B and new advances in its treatment.
Who is susceptible to infection, risk factors
The hepatitis B virus can infect adults, adolescents, children, and infants. But there are risk groups that are more at risk of infection than others, for example, people:
- working in the medical field;
- frequently changing sexual partners;
- having homosexual relationships;
- those suffering from sexually transmitted diseases;
- users of illegal drugs (injection and tablet drugs);
- living with an infected person;
- located in countries at high risk of infection;
- whose parents emigrated from countries with a high risk of infection;
- with dialysis for renal failure;
- in prisons and correctional institutions;
- pregnant women.
The hepatitis B virus is 100 times more contagious than HIV (human immunodeficiency virus).
Despite the widespread introduction of vaccination against hepatitis B, the prevalence of the disease remains high. In different regions of Russia, the prevalence of carriage of the virus ranges from 1.5% to 11.5%. As with hepatitis C, the source of infection is the blood of an infected person. The routes of infection are similar: the use of non-sterile needles, instruments for various medical and non-medical (piercing, tattoos, manicure/pedicure) manipulations, the use of personal hygiene items of an infected person in everyday life (razor, scissors, toothbrush, etc.), unprotected sexual contact, transmission of the virus from an infected mother to her child. The hepatitis B virus is more stable in the external environment and more contagious than the hepatitis C viruses and human immunodeficiency viruses. Therefore, the natural routes of transmission of the B virus (sexual transmission and mother-to-child transmission) are more significant for this virus.
Transfer methods
Most often, patients become infected parenterally, i.e. through blood. In general, any biological fluid can serve as a transmitter: urine, saliva, semen, etc. For infection, it is enough for even a small portion of biomaterial containing the virus to come into contact with an open wound.
Most often, transmission of the virus occurs:
- during any surgical interventions - from opening atheroma to extensive abdominal operations;
- when visiting cosmetic procedures - chiropractic care, manicure, pedicure and the like;
- in tattoo parlors - during tattooing, tattooing, piercing of the earlobe, lip, navel and other areas of the face and body;
- in a dental office - when performing treatment or tooth extraction;
- through an infected syringe;
- with a French kiss and unprotected PA;
- when working with contaminated material in the laboratory.
Household infection with hepatitis B is rare. There is a chance of catching the virus from a patient diagnosed with hepatitis B only when using the patient’s personal hygiene items, such as a comb or razor. In this case, pathogens can be transferred to microcuts on the body of a healthy person.
Another route of infection is transplacental, i.e. from mother to child while the baby is crossing the birth canal. It is also possible for a newborn to become infected by a nursing mother.
How to protect yourself from hepatitis B?
The only means of protection is vaccination against hepatitis B, which is currently administered to all newborn children and adolescents. Adults with risk factors for infection should also be vaccinated. The hepatitis B vaccine is one of the safest vaccines in the world. Three-time administration of the vaccine according to a special scheme leads to the formation of specific antibodies that prevent the development of hepatitis B disease in 98% of those vaccinated. Immunity lasts for at least 8-10 years, but often remains for life.
Prevention
The main method of preventing hepatitis B is vaccination. WHO recommends that all newborns be vaccinated against hepatitis B as soon as possible after birth, within the first 24 hours of life if possible, followed by two or three doses of the vaccine at least four weeks apart to ensure full vaccination. Timely vaccination of children immediately after birth is an effective way to reduce the incidence of mother-to-child transmission of hepatitis B.
According to the latest WHO estimates, worldwide in 2021 the proportion of children under five years of age with chronic hepatitis B has fallen to just under 1%, compared with the decades before the introduction of vaccination (i.e. from the 1980s to early 2000s) this figure was about 5%.
This has achieved one of the Sustainable Development Goal targets for viral hepatitis elimination: reducing the prevalence of HBV infection among children under five years of age to less than 1% by 2021. This success was achieved in a number of regions with the exception of sub-Saharan Africa.
Increasing hepatitis B vaccination coverage worldwide over the past two decades has been a major public health achievement and has contributed to a decline in the incidence of hepatitis B infection among children.
In 2021, three-dose vaccine coverage reached 85% worldwide, up from around 30% in 2000. However, rates of newborn immunization against hepatitis B remain variable. Thus, the average rate of vaccination coverage with the first dose of hepatitis B vaccine immediately after birth is 43% worldwide, but in the WHO African Region it is only 6%.
A full course of vaccination produces protective antibodies in more than 95% of infants, children and young adults. Immunity acquired through vaccination lasts for at least 20 years and probably throughout life. Therefore, WHO does not recommend booster vaccinations for people who have completed the three-dose vaccine.
In countries with low or moderate endemicity of hepatitis B, vaccination is indicated for all unvaccinated children and adolescents under 18 years of age. In these countries, high-risk groups are more likely to become infected and should also be vaccinated. These risk groups include:
- individuals who frequently require blood or blood products, dialysis patients, and solid organ transplant recipients;
- prisoners in places of deprivation of liberty;
- injection drug users;
- persons who have household and sexual contact with people with chronic HBV infection;
- persons with multiple sexual partners;
- healthcare workers and other persons who may have contact with blood and blood products while on duty;
- International travelers who have not completed a full course of HBV vaccination and who are eligible for vaccination before departure to HBV-endemic areas.
The vaccine has an excellent safety and efficacy record and has reduced the proportion of children under five years of age with chronic HBV infection to just under 1% in 2021, compared with the decades before the introduction of the vaccine (i.e. since the 1980s). until the early 2000s), this figure was about 5%.
In addition to infant vaccination, which includes a timely first dose immediately after birth, WHO recommends prophylactic antiviral therapy to prevent mother-to-child transmission of hepatitis B. Pregnant women with a high concentration of HBV DNA (high viral load) and/or the presence of HBeAG in the blood are at high risk of transmitting the virus to their unborn child, even if the child receives the first dose of vaccine immediately after birth and completes the full course of vaccination against hepatitis B. Therefore, pregnant women with high The concentration of HBV DNA during pregnancy may indicate a prophylactic course of antiviral therapy to prevent perinatal HBV infection and protect the unborn newborn from the disease.
In addition to infant vaccination and prevention of mother-to-child transmission, HBV transmission can be prevented through blood safety measures, including quality screening of all donated blood and blood products used for transfusion. Globally, 97% of donated blood units were screened and quality controlled in 2013, but gaps remain. Effective measures to prevent the transmission of hepatitis B virus include ensuring safe injections and avoiding unnecessary injections and injections performed in unsafe conditions. Between 2000 and 2010, the rate of unsafe injections worldwide fell from 39% to 5%. In addition, one of the effective measures to prevent infection is to improve the safety of sexual intercourse, including minimizing the number of sexual partners and the use of barrier contraception (condoms).
Hidden disease
As with hepatitis C, the acute phase of the infection often occurs without jaundice. In the vast majority of cases, patients with acute hepatitis B recover and acquire lifelong immunity to re-infection (protective antibodies to viral proteins are detected in their blood serum). After infection, some people become carriers of the HBsAg virus protein, also called the “Australian antigen.” Carriage most often occurs when infected in childhood. In a small proportion of patients, acute hepatitis drags on and becomes chronic. Chronic hepatitis B, like chronic hepatitis C, often occurs latently and unnoticed for a long time. For many years, a person can feel absolutely healthy, and the first symptoms of the disease appear only at the late stage of liver cirrhosis, when the disease is more difficult to treat and the overall prognosis is unfavorable.
What affects life expectancy
When you find out how long different patients live with hepatitis B with treatment, you will be surprised. Some patients who follow the doctor’s instructions live to old age, others die within 1-5-10 years. The thing is that the development and chronicity of the disease is influenced by several factors:
- The age at which the person was infected. At risk are children and the elderly. In children, the disease especially quickly becomes chronic. The elderly usually have various health problems that aggravate the course of the disease.
- Physical inactivity. With hepatitis, some types of physical activity are limited, but practicing an active lifestyle is mandatory. Low mobility can cause a deterioration in metabolism, which contributes to the development of the disease.
- Overweight. The virus affects the liver, which even without disease in people with a weight exceeding BMI experiences greater stress. Those who want to live as long as possible are advised to lose extra pounds.
- Presence of other diseases. Cirrhosis, cancer, HIV, diabetes, thyroid and gastrointestinal diseases can complicate the course of the disease.
- Non-compliance with the diet. Fried and fatty foods are contraindicated in case of severe liver damage.
- Harmful addictions. Smoking, drug and alcohol use have disastrous consequences for hepatitis patients. Their liver, due to chronic inflammation, is simply not able to neutralize poisons and toxins. Alcoholics and drug addicts live 5-10 years.
- Gender. In women, the disease progresses faster.
What is important to know about the forms of hepatitis B virus infection?
Chronic infection can occur in two main forms:
The first form is inactive carriage of HBsAg. It is characterized by the absence of viral particles in the blood serum or their detection in a low titer, the absence of inflammation in the liver and, as a rule, a non-progressive course. With a decrease in immunity, inactive carriage of HBsAg can turn into the active form of hepatitis B.
The second form is chronic active hepatitis B. It is characterized by the presence of a large number of viral particles in the blood, the presence of inflammation in the liver, which is reflected in changes in the so-called liver tests (or enzymes), and a progressive course with the risk of developing cirrhosis and liver cancer. In recent years, it has been found that the higher the concentration of virus in the blood, or “viral load,” the higher the risk of developing cirrhosis and liver cancer.
It is impossible to distinguish between these two forms based on the patient’s well-being and only clinical signs of the disease (which, as with inactive carriage, may be completely absent in a patient with chronic hepatitis B).
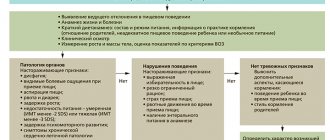
What to do if you are diagnosed with HBsAg?
Unfortunately, hepatologists are often faced with underestimation on the part of the patient, as well as doctors of other specialties, of the seriousness of HBsAg detected over many years. A patient who is diagnosed with HBsAg for the first time must undergo an examination, which will make it possible to make a correct diagnosis - to distinguish between inactive carriage of HBsAg and active chronic hepatitis B that requires treatment. To do this, the hepatologist will suggest that you do a number of studies: - a study of a biochemical blood test, - a study of the viral load using quantitative PCR (polymerase chain reaction) - a study for the presence of another protein (or antigen) of the hepatitis B virus, which characterizes the high infectiousness of the patient, — HBeAg — study for the presence of a companion virus of hepatitis B - delta virus — study of alpha-fetoprotein (tumor marker of a liver tumor) — ultrasound examination of the liver — fibroelastography to clarify the stage of liver fibrosis (other studies are possible according to indications)
Modern treatment of chronic hepatitis B can stop the disease!
If you are nevertheless diagnosed with chronic hepatitis B, it is necessary to prescribe antiviral treatment, that is, treatment using drugs that can block the replication of the virus.
The goal of modern antiviral therapy for chronic hepatitis B is to persistently suppress the replication of the virus, achieve remission of the disease, that is, transfer the process to an inactive state. When this result is achieved, the development of liver cirrhosis and its complications (such as ascites, internal bleeding, liver failure) is prevented, and the risk of developing liver cancer is greatly reduced.
A number of drugs with antiviral effects are currently registered for the treatment of chronic hepatitis B. Among the new generation of drugs there are safe drugs that can be used for several years, drugs to which the virus does not develop resistance. Your attending physician will help you choose a treatment appropriate to the stage and form of your disease.
Treatment
Medical care for hepatitis B is aimed at maintaining comfort and a rational combination of nutrients, including replacing fluid lost as a result of vomiting and diarrhea. People with chronic hepatitis B who need treatment can be treated with medications, including oral antivirals (such as tenofovir and entecavir) and interferon injections. Treatment of hepatitis B may slow the progression of cirrhosis, reduce the incidence of hepatocellular carcinoma, and improve long-term survival. However, in many resource-poor areas, access to such treatment is difficult.
Liver cancer is almost always fatal and often occurs in people who are in their prime productive years and are providing for their families. In developing countries, most people with liver cancer die within months of diagnosis. In high-income countries, surgery and chemotherapy can prolong life by several years. Patients with cirrhosis sometimes undergo liver transplants, with varying degrees of success.
Is it necessary to follow a diet for patients with chronic hepatitis B?
No special diet is required for chronic viral hepatitis, however, you should avoid drinking alcohol even in small doses, since the combined effect of alcohol and the virus on the liver significantly increases the risk of developing cirrhosis and liver cancer. If you are overweight, you should limit your intake of fats and high-calorie foods, since fat deposition in the liver accelerates the development of cirrhosis. Factors that reduce immunity, in particular sun exposure, should be avoided, that is, you should not use a solarium or sunbathe on the beach. It is advisable to quit smoking. You can continue to exercise. Swimming and hardening procedures that support the state of your immunity are useful.