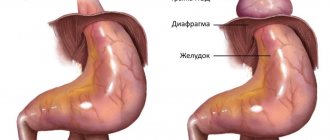
Axial hiatal hernia is a progressive pathology associated with weakening of the ligamentous apparatus of the diaphragm, which is characterized by the movement of internal organs through an enlarged esophageal diaphragmatic opening into the cavity of the posterior mediastinum. The hernia usually involves the terminal segment of the esophagus, parts of the stomach and intestines. The stage of the disease directly depends on the extent of the affected organs. You should find out under what circumstances a hiatal hernia may occur and when you need to see a doctor.
General characteristics of the pathology
Sliding hiatal hernias got their name due to the fact that the posterior wall of the upper part of the cardiac part of the stomach, which is not covered by the peritoneum, participates in the formation of the hernial sac. Initially, the disease is asymptomatic and does not bother the patient at all. After some time, a person may notice symptoms similar to diseases of the gastrointestinal tract and heart. If not treated promptly, symptoms can be so severe that they limit normal life activities.
Nutritional adjustments play a significant role in stabilizing the patient’s condition. This is the use of a gentle diet, which includes:
- exclusion of fatty, fried and spicy foods from the diet;
- avoidance of consuming large amounts of salt;
- lack of smoked meats, marinades, hot seasonings in the diet;
- frequent and small meals.
Proper functioning of the digestive system will be the key to the effectiveness of treatment.
Why does a hernia form?
The causes of hiatal hernia consist of two mechanisms. Changes in the structure of the muscular-ligamentous apparatus of the diaphragm, loss of elasticity, atrophy with pronounced loss of tone and stretching.
This process is typical for old age, people who move little, do not exercise, have lost weight for various reasons, patients with chronic systemic diseases of connective tissue, blood circulation, metabolic disorders (Marfan syndrome, hemorrhoids, intestinal diverticulosis, flat feet, diabetes mellitus), if in children the basis of the disorders is genetic diseases or underdevelopment of muscle groups due to a complicated pregnancy of the mother, anomalies (achalasia, short esophagus).
Another important factor is the increase in intra-abdominal pressure. It grows in people:
Causes of pain in the esophagus
- with chronic diseases accompanied by flatulence and constipation;
- with prolonged uncontrollable vomiting;
- with ascites (abdominal enlargement caused by the penetration of plasma from the vessels into the abdominal cavity during congestion) with cardiac decompensation, liver cirrhosis;
- with a large tumor of a benign or malignant nature located in the peritoneal cavity;
- those who have suffered abdominal trauma;
- doing weightlifting;
- during heavy physical loads;
- with abdominal obesity;
- suffering from chronic diseases of the lungs, bronchi, and larynx with a severe cough.
Physiological pregnancy usually does not lead to a hernia, but if a woman is weakened by one of the listed diseases, then even normal enlargement of the uterus has a serious effect on muscle tone and puts pressure on the diaphragm from below. In case of multiple pregnancy or complicated childbirth, the prognosis worsens.
Impaired peristalsis of the esophagus, causing excessive tension and tightening of the cardial part of the stomach, accompanies inflammatory diseases of the esophagus; it supports peptic ulcer disease, calculous cholecystitis and pancreatitis, chronic gastroduodenitis by a reflex mechanism in 15–20% of patients (spasm of the longitudinal muscles occurs).
Of particular importance are burns of the esophagus (thermal or chemical) with the formation of cicatricial adhesions, narrowing of the lumen, and peptic ulcers.
Degrees and types of pathological changes
In medicine, there are three types of hernia:
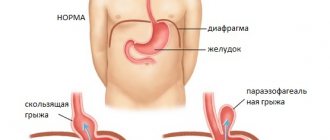
1. Sliding (A).
This type of pathology involves the normal position of the stomach and esophagus. But they can easily move into the esophageal opening. Sliding hernias can be fixed or non-fixed. In the latter case, they are adjusted independently when the patient is in an upright position. Large hernias (cardiofundal and giant), as a rule, are fixed due to the suction effect of the chest cavity and the formation of adhesions in the hernial sac. The scientific name is axial hernia.
2. Paraesophageal (B).
It is characterized by the fact that the cardia does not change its position, and the fundus and greater curvature of the stomach emerge through the enlarged opening. With paraesophageal hernias, the cardia remains fixed under the diaphragm, and one or another abdominal organ is displaced into the mediastinum near the esophagus, which is why the hernia has this name. Thus, it seems as if the stomach has turned over.
3. Combined (C).
Consists of all the signs of the two types of hernia described above.
Consequently, three degrees of hiatal hernia are determined – I, II and III.
The grade of the hernia is based on the level of the protrusion into the chest, as well as the size of the mass.
1st degree
– in the chest cavity (above the diaphragm) there is the abdominal section of the esophagus, and the cardia is at the level of the diaphragm, the stomach is elevated and directly adjacent to the diaphragm.
II degree
– the abdominal section of the esophagus is located in the chest cavity, and part of the stomach is located directly in the area of the esophageal opening of the diaphragm.
III degree
- above the diaphragm are the abdominal esophagus, cardia and part of the stomach (fundus and body, and in severe cases, the antrum).
Operation
The purpose of the operation is to restore the anatomical position and normal function of the cardia. The basic principle is to eliminate the hernial orifice and perform antireflux surgery. This is done by mobilizing and lowering the esophageal-gastric junction into the abdominal cavity, narrowing the esophageal opening of the diaphragm and performing one of the types of fundoplication, which allows you to restore the lower esophageal sphincter, the high pressure zone in it and the angle of His.
- The most common is the operation by Nissen, who proposed a 360° fundoplication for the treatment of a hiatal hernia complicated by esophagitis. It consists of forming a circular cuff from the anterior and posterior walls of the fundus of the stomach, enveloping the mobilized abdominal section of the esophagus, in which a 30-32F1 probe is installed. The edges of the stomach are sutured together with the wall of the esophagus. The width of the cuff is at least 2.5-3 cm. If the hernial opening is wide (more than 3.5 cm), the legs of the diaphragm are sutured together behind or in front of the esophagus (posterior or anterior crurorrhaphy) to the normal size of the POD. When the POD diameter is more than 5 cm, to prevent recurrence of the hernia, it is advisable to strengthen the crurorrhaphy with a mesh prosthesis made of non-absorbable synthetic material.
- Fundoplication according to Nissen-Rossetti also involves a 360° fundoplication with the difference that the gastric cuff is not fixed to the diaphragm (prevention of hiccups and pain during breathing movements), but 1-2 sutures are placed between the esophagus and the gastric cuff on the side opposite from the sutures of the cuff itself (prevention of cuff expansion in the fundus of the stomach). The disadvantage of the Nissen and Nissen-Rosetti operations is the twisting of the esophagus along the axis when the fundus of the stomach is passed under it. This can be avoided by modifying the Nissen operation, in which the first short arteries of the stomach, the posterior (not covered by the peritoneum) wall of the cardia are mobilized, and the anterior and posterior walls of the fundus of the stomach are involved in creating the cuff.
- Toupet fundoplication involves the formation of a symmetrical cuff from the anterior and posterior walls of the fundus of the stomach, enveloping the esophagus at 240-270°, leaving its anterior-right surface free (localization of the left vagus nerve). Used for small stomach fundus. Many authors prefer this method of fundoplication due to the lower incidence of dysphagia in the early postoperative period (compared to the Nissen procedure). This advantage is offset in the future due to a greater number of relapses of reflux disease.
- Fundoplication according to Dor. It also involves partial fundoplication, in which the anterior wall of the fundus of the stomach is placed in front of the abdominal esophagus, fixing it to the right wall of the esophagus. This operation is ineffective; it is rarely used as a forced measure when it is impossible to fully mobilize the esophagogastric junction and perform other types of fundoplication.
- The Cuschieri operation (1991) is the creation of an acute angle of His using the round ligament of the liver, which, after partial mobilization from the navel, is carried out with the free end under the abdominal segment of the esophagus, pulling it to the right and anteriorly (an acute angle of His is formed). Rarely used due to low efficiency.
For hernias combined with pronounced shortening of the esophagus (congenital or due to esophagitis), the Collis-Nissen operation gives the best results. The operation consists of lengthening the abdominal esophagus due to the lesser curvature of the stomach, followed by gastrofundorraphy (enveloping the newly created esophageal tube from the lesser curvature with the walls of the fundus of the stomach according to the Nissen fundoplication type).
The main causes of pathology
The root causes of pathological changes are congenital and acquired. However, all types of hiatal hernia occur under the influence of similar factors.
| Congenital | Purchased |
| During the formation of the chest, the diaphragm was underdeveloped | Injuries and injuries to the chest |
| Hernia pockets formed during embryo development | Insufficient functional load on the diaphragm in people leading a predominantly sedentary lifestyle |
| Elderly age. As a consequence of age-related changes | |
| Repeated longitudinal spastic shortening of the esophagus due to esophageal dyskinesia, as well as reflex and symptomatic esophagospasm | |
| Atrophy of the left lobe of the liver, disappearance of adipose tissue under the diaphragm, which contributes to disruption of the relationships between organs in the area of the esophageal opening of the diaphragm and the formation of its hernia | |
| Constitutional weakness of connective tissue, which is confirmed by their frequent combination with hernias of other localizations, flat feet, varicose veins of the saphenous and hemorrhoidal veins | |
| The difference in pressure in the chest and abdominal cavity. The following conditions lead to increased intra-abdominal pressure: obesity, cough, overeating, constipation, flatulence, ascites, large intra-abdominal tumors, pregnancy, heavy lifting |
Sometimes a patient can combine two factors at the same time - acquired and congenital. For example, a heavy smoker suffers from a cough and the abdominal organs protrude through the esophageal opening.
Forecast
In case of untimely diagnosis and incorrect treatment tactics, a hiatal hernia can provoke the appearance of:
- Peptic ulcers of the esophagus and stomach.
- Reflex angina.
- Perforation of the esophageal tube.
- Various forms (erosive, catarrhal, ulcerative) esophagitis.
- Cicatricial stenosis of the esophagus.
For 30% of patients, untreated hiatal hernia can result in esophageal cancer. With adequate and timely treatment of diaphragmatic hernias, in 80% of cases the condition of patients improves significantly. Stage I diseases are completely cured. Cases of relapse are extremely rare.
What are the symptoms of the disease?
Often, a sliding hiatal hernia is completely asymptomatic and, as a rule, does not require specific treatment. All the symptoms of a hiatal hernia are mainly related to what happens:
- The reflux of stomach acid into an organ such as the esophagus. As a result, 1-4 hours after administration, the patient develops painful heartburn.
- Cramps and frequent bloating begin to occur.
- Aching pain appears in the upper base of the chest, which increases when leaning back or belching due to increased abdominal pressure.
The most common symptoms of an axial hernia.
| Symptom | Main features |
| Pain | Burning at the level of the xiphoid process and the lower third of the sternum, worsening after eating and in a horizontal position, accompanied by other typical signs of gastroesophageal reflux. In some patients, the pain simulates angina pectoris. |
| Heartburn | Usually appears after eating or when there is a change in body position that contributes to the occurrence of reflux. May occur at night. |
| Belching air | Occurs either with air or with acidic contents. It often brings relief, reducing the feeling of fullness in the epigastric region, but in some patients this is followed by burning pain in the chest. In most cases it occurs immediately after eating or after 20-30 minutes. |
| Regurgitation | Reflux of sour or bitter liquid occurs suddenly when the patient is in a horizontal position or when the body is tilted and is not accompanied by nausea. |
| Dysphagia | Patients localize the sensation of food retention at the level of the xiphoid process. Appears periodically, often intensifies with excitement and hasty eating. |
Nausea, vomiting, shortness of breath, hiccups, burning tongue are relatively rare symptoms of an axial hernia.
Diagnostics
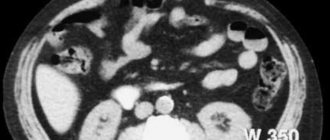
The main signs of the disease are determined by x-ray examination. To identify an abnormal location of the end of the esophagus and stomach, use:
- general visual X-ray examination with contrast of the initial digestive organs - currently rarely used;
- X-ray (series of images) of the esophagus and stomach.
The patient is photographed in the following position:
- lying down,
- standing,
- on the side
- in the knee-elbow Trendelenburg position.
Radiologists take into account, as a direct sign, a clear displacement of part of the stomach into the chest cavity. Indirect ones include:
- disturbed shape of the gas bubble or its absence, change in size;
- increase in the angle of His;
- signs of reflux reflux;
- movements of the esophagus that are the opposite of proper peristalsis.
Ultrasound diagnostic specialists consider it possible to participate in the examination; the picture differs from the radiological signs (right)
Esophagogastroscopy shows:
- non-closing walls of the esophagus in the diaphragmatic area (picture of “gaping of the cardia”);
- the cardiac section is located higher than usual due to shortening of the esophagus;
- gastroesophageal reflux;
- foci of proliferation of foreign epithelium.
Endoscopy helps to identify the severity of reflux influence and possible transition to a neoplasm.
Additional methods include:
- esophagomanometry,
- scintigraphy,
- intraesophageal pH-metry.
Conducting a general clinical examination helps to identify complications:
- stool analysis can detect early signs of bleeding;
- blood test shows anemia, infection;
- An ECG is absolutely necessary to exclude atypical angina.
Differential diagnosis is always carried out:
- with different types of diaphragmatic hernias;
- cicatricial changes in the esophagus;
- peptic ulcer;
- malignant neoplasm;
- disorders associated with increased pressure in the portal vein;
- angina pectoris;
- gallstone disease.
How is the disease diagnosed?
Pathology is often identified when determining the causes of gastric contents reflux into the esophagus, pain in the chest and/or abdomen. To establish a diagnosis, the following is carried out:
- endoscopic examination - will exclude other diseases of the digestive tract, in which similar symptoms may be observed;
- stool test for occult blood - to exclude bleeding in the gastrointestinal tract;
- X-ray examination - may be required to exclude diseases of the respiratory system;
- ECG (electrocardiography) – for the purpose of differential diagnosis with diseases of the cardiovascular system.
Features of treatment
If you had to face a problem such as a hiatal hernia, then there may be two ways out of the situation: surgical or conservative treatment. The main task of classical methods can be defined not as the elimination of the hernia itself, but as a reduction in the symptoms of reflux esophagitis and neutralization of gastroesophageal reflux. That is, doctors strive to relieve pain and prevent possible complications. These goals are achieved through a diet based on small and frequent meals.
| View | Description |
| Drug therapy | It is necessary to take medications that correct the motor process of the stomach and normalize secretory activity. In general, inhibitors, antacids, and prokinetics are used for such therapy. Drug treatment is used only in the early stages without complications. Thanks to the medications, the patient’s vitality increases and he feels relief. If treatment is applied in a timely manner, the likelihood of complications is significantly reduced |
| Surgical treatment | This method is used extremely rarely, only when drug therapy is ineffective or complications arise. |
During this treatment you will have to give up some foods. We are talking about chocolate, carbonated drinks, coffee, animal fats, fresh bread and other flour products. Also, doctors do not recommend resting in a lying position for the next 3 hours after eating during such treatment.
Axial hernia, regardless of the degree and severity, is mainly eliminated by conservative treatment methods.
| Treatment with diet | Drug treatment |
| The patient must switch to fractional meals. That is, food intake should occur in small portions, but much more often. In this case, all food should be crushed to a mushy state and consumed only warm. Some foods will need to be excluded from your usual diet, as they can be irritating to the mucous membrane of the digestive tract. These include all pickles and marinades, spicy foods, smoked meats | The use of antacids is indicated, which suppress the activity of gastric juice (Phosphalugel). Take enveloping medications (Vicalin). To eliminate painful sensations, you can use painkillers (Novocaine). Use of antispasmodics (No-spa) |
Bad habits can complicate the process of fighting the disease, so you will have to give them up. Exposure to pharmacological drugs is also possible. These can be proton pump inhibitors, prokinetics, antacids, etc. As for surgical intervention, it is relevant only if conservative treatment has not given the desired effect. The laparoscopic technique is most often used.
Traditional methods of treatment
Vegetable juices have a beneficial effect on the body and reduce the unpleasant symptoms present with a hiatal hernia:
- potato
– improves the functioning of the gastrointestinal tract, eliminates the symptoms of gastroesophageal reflux; - carrot
– reduces acidity, helps relieve inflammation; - celery juice
– eliminates heartburn, restores the body's defenses.
Medicinal teas for hiatal hernia can be consumed in unlimited quantities. The only contraindication to such treatment is individual intolerance to the components. Chamomile tea is the most effective remedy for diseases of the esophagus. It relieves inflammation and improves the patient's condition. You can use the following recipes:
- For bloating (a common symptom of a hiatal hernia), tea made from crushed cumin or anise seeds (1 teaspoon of raw material per 1 cup of boiling water) will be useful. It is recommended to take the product 50 ml every half hour until the unpleasant symptom disappears.
- Chamomile tea is the most effective remedy for diseases of the esophagus. It relieves inflammation and improves the patient's condition. To prepare it, 1 tsp. inflorescences are brewed with 250 ml of boiling water and left for 10 minutes. You can drink the drink at any time of the day, regardless of meals.
- Ginger will have a positive effect on the body. The root can be used to make tea or simply chewed fresh.
A mixture of dried apricots, figs, prunes, raisins and dates will help cope with the unpleasant symptoms of a hiatal hernia. You need to take 500 g of all components. Prepared dried fruits are soaked in water until softened. After this, the liquid is drained and the mixture is twisted in a meat grinder. Add 5 tbsp to the resulting gruel. l. honey and mix thoroughly. It is recommended to use the medicinal mixture twice a day, 1 tbsp. l.
Possible complications
To the extent that axial hiatal hernia can develop asymptomatically for a long time, the likelihood of untimely diagnosis and treatment increases, resulting in complications:
- Bleeding may begin in the esophagus.
- The hernia is strangulated.
- Esophageal perforation is a common occurrence.
- A peptic ulcer of the esophagus develops.
- Cicatricial narrowing of the esophagus occurs.
But, complications are possible even after surgery during the rehabilitation period:
- Abnormal dilatation of the esophagus may occur.
- Recurrences of axial hernia occur.
- The stomach area becomes pathologically enlarged.
If an axial hiatal hernia is present, a lung problem in the form of aspiration pneumonia may occur. To eliminate this consequence, antibiotics are required, which are introduced into the body without affecting the digestive tract. It is very important to diagnose the complication in time and begin immediate treatment.
Prevention
Preventive measures against hiatus hernia include following simple rules:
- compliance with similar recommendations indicated for conservative treatment;
- timely elimination of diseases or disorders that can lead to such an illness;
- taking regular walks, especially after eating food;
- undergo regular preventive examinations, in particular x-rays.
The prognosis of a hiatal hernia is directly related to the development of complications. After surgery, relapses of the disease are extremely rare. However, patients will need to be followed by a gastroenterologist for the rest of their lives.
What do doctors recommend?
Ignoring or improperly treating a hernia can lead to dire consequences: terrible pain, dependence on painkillers, and limited movement. Not to mention the threat of complete paralysis, when there is no way out.
- rejection of bad habits;
- rational and balanced nutrition;
- healthy lifestyle;
- moderate physical activity;
- body weight control;
- timely and correct treatment of all concomitant diseases.
By following basic rules, you can not only reduce the risk of developing a hernia, but also other diseases of the gastrointestinal tract. In any case, self-medication should be excluded. The sooner a person seeks medical help, the greater the chance of a successful prognosis. Disregarding the fact of the occurrence of a hiatal hernia is a big mistake. If such a diagnosis has been made, then the treatment process must be taken as seriously as possible. Otherwise, the condition may worsen significantly.
How to treat a hiatal hernia without surgery?
To eliminate the clinical manifestations of all concomitant diseases of the digestive system (gastritis, gastroesophageal reflux, ulcers, dyskinesia and erosions), an individual program of complex drug therapy is developed for each patient, including the use of:
- Proton pump inhibitors (esomeprazole, omeprazole, pantoprazole).
- Antacids (represented by Almagel, Maalox and Gastal).
- Prokinetics that improve the condition of the mucous membranes of the esophagus (ganatone, motilium, trimebutine, motilac).
- H2-antihistamines (most often ranitidine).
- B vitamins that can speed up the restoration of gastric structures.
To relieve pain, patients can be prescribed non-steroidal anti-inflammatory drugs (represented by paracetamol, ibuprofen, nurofen). In some cases, taking these medications can provoke an increase in clinical manifestations characteristic of gastroenterological diseases.
To enhance the effectiveness of drug treatment, patients are recommended to:
- adhere to a gentle diet;
- start normalizing your weight;
- during night sleep, take a semi-sitting position (thanks to the raised head of the bed);
- avoid any physical activity.
Indications for the need for surgical intervention are the presence of:
- complete failure of drug treatment;
- complicated forms of diaphragmatic hernia;
- precancerous (also called dysplastic) changes in the mucous membranes of the esophagus.
There are quite a large number of options for surgical treatment of diaphragmatic hernias.