Gastroesophageal reflux disease (GERD) - This is one of the most serious and complex pathologies of the esophagus. The disease can significantly impair the patient's quality of life. As it progresses, it leads to dangerous complications, including Barrett's esophagus and adenocarcinoma. GERD affects both men and women equally often and is difficult to treat. Experienced specialists at the ACMD clinic will help you get rid of the unpleasant manifestations of GERD once and for all. Do not delay your visit to the doctor, contact us at the first symptoms!
Reflux esophagitis: etiology and pathogenesis
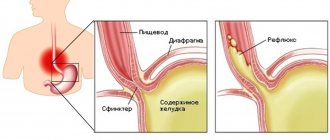
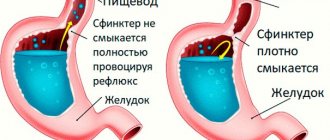
GERD is a chronic disease that occurs when the lower esophageal sphincter, also called the “muscle valve,” does not function properly. Gastroesophageal reflux occurs when stomach contents (undigested food, acid) reflux into the esophagus. Frequent contact of the esophageal mucosa with the contents of the stomach causes inflammation. Gastric juice literally dissolves the esophageal mucosa.
Important information! The World Organization of Gastroenterologists has recognized GERD as the most common disease of the 21st century. According to official data, about 50% of the world's population faces this disease.
The main cause of GERD is insufficiency of the lower alimentary sphincter, which develops due to a general decrease in tone or excessively frequent relaxation of the LES not associated with swallowing. Relaxation of the LES (lower esophageal sphincter) can be provoked by increased pressure in the peritoneum or subthreshold pharyngeal stimulation.
Prokinetics
These drugs restore the normal physiological state of the esophagus by increasing the tone of the lower sphincter, improving clearance and enhancing peristalsis. The main means of pathogenetic therapy for GERD is the prokinetic drug Motilium. It normalizes the motor activity of the upper digestive tract, restores active gastric motility and improves antroduodenal coordination. Motilium is well tolerated when long-term therapy is necessary and reduces the percentage of disease relapses.
Why does reflux disease develop?
Very often, the exact cause of the development of GERD cannot be determined. The disease can be provoked by a combination of different factors, namely such as:
- weight gain;
- overeating fatty foods, unhealthy diet;
- excessive coffee consumption;
- alcoholism and energy drink consumption;
- smoking and other bad habits;
- taking certain medications.
Medicines that reduce the tone of the lower esophageal sphincter include:
- anticholinergic medications;
- antihistamines;
- tricyclic antidepressants;
- calcium channel blockers;
- progesterones and nitrate-containing agents.
Important information! American scientists associate GERD with a hereditary predisposition. The development of the disease can also be affected by: stressful situations, hormonal imbalances, and injuries to the esophagus.
Gastric reflux may be temporary. It is considered pathological only in cases where the frequency of attacks is more than 50 per day, as well as when the pH in the esophagus reaches 4.0 or lower. An attack of pathological reflux can be provoked by: a change in body position, increased abdominal pressure, or disruption of the usual diet.
Proton pump inhibitors
If GERD with esophagitis is diagnosed, treatment with prokinetics is carried out in combination with proton pump inhibitors. As a rule, the new generation drug “Pariet” is used. Due to its use, acid secretion is reduced, and there is a positive dynamics in the clinical manifestations of the disease. Patients report a decrease in intensity or even complete disappearance of heartburn and a decrease in pain.
For GERD, the treatment regimen with prokinetics and proton pump inhibitors is as follows: 20 milligrams of Pariet and 40 milligrams of Motilium are prescribed per day.
Esophagitis: symptoms
The most striking and specific symptom of GERD is heartburn with or without the penetration of stomach contents into the oral cavity. Feelings of heartburn:
- “chill” at the bottom of the throat;
- burning and stinging in the throat;
- bitter or sour taste in the mouth;
- lump in the throat;
- nausea and stomach pain.
Frequent attacks of heartburn can lead to irritability, insomnia, anorexia, and chronic aspiration of stomach contents into the respiratory tract. Signs of chronic aspiration: cough, hoarseness, sore throat.
Distal reflux esophagitis may be accompanied by:
- pain when swallowing;
- esophageal bleeding;
- pain in the chest area;
- an unpleasant taste in the mouth that does not go away even after brushing your teeth.
Due to constant throat irritation, patients with GERD may develop chronic pharyngitis or laryngitis. At the same time, symptoms characteristic of the listed diseases are added (pain when swallowing, swelling of the throat, intoxication).
GERD: classification and features of different forms
There are two main forms of GERD:
- Non-erosive - the most common, characterized by swelling and inflammation of the esophageal mucosa, but does not lead to the formation of wounds.
- Erosive - leads to the appearance of ulcers and erosions on the surface of the esophageal mucosa under the influence of an aggressive gastric environment.
The Los Angeles classification distinguishes the following degrees of GERD:
- A – one damage to the mucosa, limited to the esophageal folds, with a diameter of no more than 5 mm;
- B – one or more lesions of the mucous membrane, limited to the esophageal folds and not merging with each other, with a diameter of more than 5 mm;
- C – numerous lesions of the mucous membrane, occupying less than 70% of the circumference of the esophagus;
- D – numerous confluent lesions of the mucous membrane of the esophagus, occupying over 70% of its circumference.
Surgical intervention
Sometimes, to restore normal function of the cardia, it is necessary to resort to surgery aimed at eliminating reflux. Indications for surgical treatment are as follows:
- complications of GERD (repeated bleeding, strictures);
- ineffectiveness of conservative therapy;
- frequent aspiration pneumonia;
- diagnosing Barrett's syndrome with high-grade dysplasia;
- the need of young patients with GERD for long-term antireflux therapy.
Reflux is often treated by fundoplication. However, this method is not without drawbacks. Thus, the result of the operation entirely depends on the experience of the surgeon; sometimes after surgery there remains a need for drug treatment, and there is a risk of death.
Currently, various endoscopic techniques have been used to influence foci of metaplasia: electrocoagulation, laser destruction, photodynamic destruction, argon plasma coagulation, endoscopic local resection of the esophageal mucosa.
How is GERD diagnosed?
If symptoms of reflux pathology appear, you should contact your family doctor or directly a gastroenterologist. First of all, the doctor carefully studies the clinical picture and complaints of the patient. Often the diagnosis can be made only by the clinical picture, without additional research. Sometimes the patient is prescribed additional diagnostic procedures, namely:
- endoscopy is the most informative way to diagnose GERD , which consists of visually studying the structure of the esophagus (helps determine narrowing, the presence of erosions and ulcers, changes in the composition of the epithelium);
- daily monitoring of the pH level in the esophagus - helps to assess the nature and synchronicity of the reflux of stomach contents into the esophagus;
- X-ray examination of the esophagus with barium - allows you to identify narrowings and hernias of the esophageal passage of the diaphragm.
Interesting fact: a healthy esophagus is able to push food into the stomach when swallowed in any body position, even when a person is lying upside down. And all thanks to proper peristalsis (muscle contractions).
Antisecretory drugs, H2 receptor blockers
This is the first-line treatment for mild to moderate GERD and grade I-II esophagitis. Four H2 blockers are commonly used in clinical practice: ranitidine, famotidine, cimetidine, and nizatidine. They are more effective in suppressing unstimulated secretion of gastric juice with food and are therefore recommended on an empty stomach or at night.
H2 blockers are effective in the treatment of mild esophagitis (70-80% of patients recover), as well as in antirecessive treatment and prevention of relapses. The effectiveness of H2 blockers decreases with long-term use, leading to tachyphylaxis. An H2 blocker is recommended for patients suffering from nocturnal reflux symptoms, especially in Barrett's temple.
GERD in children
Reflux esophagitis in children with diseases of the gastrointestinal tract is detected in 17% of cases (approximately). The exact prevalence of GERD in childhood is unknown, due to the variety of clinical manifestations of the disease.
Important information! The process of GERD itself can be quite natural for a child under one year of age. Due to the insufficient length and immaturity of the esophagus, stomach contents regularly enter it, and from there into the throat and oral cavity. In common parlance this is called regurgitation.
Signs of GERD in childhood are varied and numerous. You can suspect a disease in a child by:
- regular severe vomiting after eating;
- frequent belching with a sour aroma;
- prolonged hiccups;
- morning cough;
- a feeling of bitterness in the mouth;
- chest pain;
- night snoring;
- attacks of difficulty breathing;
- thinning and darkening of tooth enamel.
Treatment of gastroesophageal reflux disease in children is not much different from therapy for adults. Often the child outgrows the disease on his own, and it disappears without a trace, forever.
Antacids
Until the 1980s, antacids were the standard treatment for mild forms of GERD. They are still used to reduce symptoms of mild reflux. Antacids are taken after each meal and before bed.
Taking antacids before bed
Antacids are also useful for side effects: they relieve constipation (aluminum antacids: ALternaGEL, Amphojel), they can increase loose stools (magnesium antacids: Phillips Milk of Magnesia). Aluminum hydroxide increases the pH of the stomach contents to >4 and inhibits the proteolytic activity of pepsin, reducing the symptoms of indigestion. Antacids do not reduce the frequency of reflux, but they do reduce the acidity of the fluid.
Magnesium hydroxide suppresses the symptoms of acidosis and improves digestion. Magnesium hydroxide antacids osmotically retain fluids in the intestine, which distends the intestinal wall, stimulates intestinal motility, and softens stools (laxative effect). When interacting with hydrochloric acid of gastric juice, magnesium hydroxide is converted into magnesium chloride.
Modern treatment of gastroesophageal reflux disease
Treatment for GERD is aimed at combating symptoms and preventing consequences. It can be conservative and medicinal. First, doctors suggest the patient try to change their lifestyle:
- get rid of excess weight;
- switch to a normal regime of wakefulness and rest;
- give up bad habits (smoking, alcohol);
- switch to a balanced, gentle diet.
Diet is the main method of non-drug treatment of GERD. You need to eat small portions 5 times a day. It is recommended to avoid evening overeating (the last meal should be at least 2 hours before bedtime). You need to include more vegetables in your diet. Meat should be consumed after boiling or steaming. Spices, fatty foods, fried foods, carbonated drinks, and sour fruits are excluded from the diet. Dishes should not be too hot or cold.
Patients should avoid situations that increase abdominal pressure. You cannot wear tight trousers, belts, corsets, sweaters, or bandages. It is not recommended to jump, lift weights, or perform intense exercises that strain the abdominal muscles. Ideal sports for people with GERD: swimming, cycling, walking.
If heartburn attacks occur only when lying down, it is recommended to raise the head of the bed or choose a larger pillow. You should not lie down immediately after eating or drinking.
The patient will have to give up medications that can provoke attacks of GERD. Such drugs include:
- nitrates and nitrate-like agents;
- nifedipine, Theophylline, Progesterone;
- antidepressants and antispasmodics;
- non-steroidal anti-inflammatory drugs.
If symptoms of GERD persist, you need to switch to drug therapy. Help to get rid of the manifestations and complications of the disease:
- drugs from the group of proton pump inhibitors;
- combined antacids;
- dioctahedral smectite;
- prokinetics.
Drug treatment for GERD lasts from 4 to 8 weeks. After the main course, you need to undergo maintenance therapy lasting 6-12 months.
Complicated and advanced forms of GERD are treated surgically. To correct a defect in the esophagus, antireflux surgery is performed. In case of a hiatal hernia, a fundoplication is prescribed - suturing the stomach to the diaphragm around the opening of the esophagus, thereby creating a cuff that regulates the passage of food.
"AiF Health" recommends
GERD is a chronic disease, but anyone who suffers from it can prevent its exacerbation. To do this you need:
► normalize body weight (if it is excess); ► stop smoking (especially on an empty stomach); ► reduce the consumption of alcohol, carbonated drinks, coffee, chocolate, fatty foods; ► try to eat regularly and in small portions; ► after eating, do not lie down or bend over for 1–2 hours; ► sleep on a high headboard; ► do not wear tight belts, trousers and skirts that are a size smaller than necessary.
Complications of GERD
Gastroesophageal reflux disease can lead to the development of many dangerous complications. The most common complications are:
- chronic esophagitis;
- peptic ulcer of the esophagus;
- esophageal strictures;
- Barrett's esophagus;
- adenocarcinoma of the esophagus.
Especially often, patients with advanced forms of GERD encounter Barrett's esophagus syndrome. Abnormal columnar epithelium appears in the lower esophagus. Complications can be provoked by: lack of treatment for GERD, asymptomatic course of the disease, old age over 50 years. Barrett's esophagus has no specific symptoms. It is diagnosed during endoscopy with a biopsy of the esophageal mucosa.
GERD can cause narrowing of the esophagus as a result of scarring of the damaged lining. This complication develops mainly in older people with a long course of reflux disease. It is treated through surgery, during which an endoscopic dilation of the esophagus is performed.
Diagnostics
Until GERD is diagnosed by a gastroenterologist, there is no point in starting treatment, because treatment methods should be selected based on the characteristics of the pathological process. To identify reflux disease and determine the mechanism of its development, the following methods are used:
- X-ray of the esophagus. With such a study, erosions, strictures, ulcers, and hernias can be detected.
- Endoscopy of the esophagus. This procedure also reveals inflammatory changes.
- Scintigraphy with radioactive technetium. The study involves taking ten milliliters of egg white with Tc11: the patient takes sips of this drug every twenty seconds, and at this time a picture is taken on the halo-chamber every second for four minutes. This method makes it possible to assess esophageal clearance.
- Manometric examination of the esophageal sphincters. This procedure allows you to detect changes in sphincter tone.
- Monitor pH in the lower esophagus. Such a study is necessary in order to select individual therapy and monitor the effectiveness of medications.
Prevention of GERD
It is impossible to predict the development of gastroesophageal reflux disease in a particular person. Therefore, the disease is difficult to prevent. If there is a hereditary predisposition, it is recommended for prevention:
- eliminate physical activity that increases pressure in the peritoneum;
- lead a healthy lifestyle without bad habits;
- harden the body;
- promptly treat gastrointestinal diseases;
- regularly diagnose parasitic infestations and, if necessary, undergo treatment;
- eat properly, in portions, regularly and in a balanced manner;
- avoid stress, severe nervous shock;
- treat psychoemotional diseases.
Interesting fact: every day, more than 10% of all energy expended is spent on digesting food. It is most difficult for the gastrointestinal tract to digest alcoholic products and animal proteins. You can relieve the gastrointestinal tract by giving up alcohol and changing the way you prepare meat dishes. It is strictly not recommended to combine alcohol with fatty snacks!
Not all patients can boldly say: “I cured GERD.” An innovative approach to treatment at the ACMD clinic will help you achieve a complete recovery!
Therapy with folk remedies
In the initial stages of GERD, alternative treatment can be very helpful. In general, at these stages you can cope with the disease simply by following an antireflux regimen and changing your lifestyle. If the disease is mild, instead of antacids to relieve heartburn, you can use various traditional medicines that strengthen and protect the esophageal mucosa, improve sphincter tone and reduce the acidity of gastric juice. In severe cases of the pathological process, it will not be possible to do without drug therapy, and in the presence of complications, surgical intervention is generally required. Therefore, treatment of GERD with folk remedies is rather an auxiliary and preventive method. It can be used as an adjunct to highly effective drug therapy regimens.
Herbal medicine is very popular among people. Here are several traditional medicine recipes for the treatment of reflux disease.
- Combine crushed dry herb yarrow (20 grams), St. John's wort (20 grams), celandine (10 grams) and chamomile (20 grams). Pour a tablespoon of the mixture into a glass of boiling water and leave for fifteen minutes. Take the strained solution one to two glasses per day.
- Mix calendula flowers (20 grams), chamomile flowers (5 grams), coltsfoot leaves (20 grams). Pour two tablespoons of the mixture into a glass of boiling water and leave for thirty minutes. Take the strained infusion before meals (twenty minutes before) one tablespoon three or four times a day.
- Combine St. John's wort herb (20 grams), chamomile flowers (5 grams), plantain leaves (20 grams). Pour two tablespoons of the mixture into a glass of boiling water and leave for thirty minutes. Take the strained decoction before meals (twenty minutes before) one tablespoon three to four times a day.
- Pour two tablespoons of flax seeds into two glasses of boiling water and leave for eight hours. Take the strained infusion before meals, half a glass three to four times a day for five to six weeks.
- Squeeze the juice out of potatoes and take it before meals (twenty minutes before) a quarter glass four times a day for three weeks.
- Fry the buckwheat until it turns dark brown. Crush the resulting mass into powder and consume it three to four times a day, a pinch at a time.
- You can quickly stop heartburn by chewing a piece of horse sorrel or calamus root. These plants have the ability to reduce the acidity of gastric juice and thus reduce its damaging effect on the esophageal mucosa. Also, horse sorrel and calamus protect the mucous membrane from the harmful effects of hydrochloric acid.