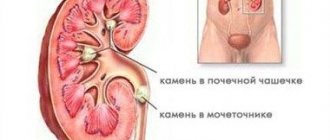
Types of kidney stones
Kidney stones vary in shape and composition. In form they can be:
- flat;
- rounded;
- angular;
- coral-shaped (have the size of the renal pelvis and imitate its internal shape - this is the most complex and rare type of the disease).
Depending on the composition, the following stones are found:
- Phosphate. They are formed from salts of phosphoric acid. Such stones have a grayish color and a soft consistency, due to which they crumble easily. They can be either smooth or rough.
- Cystine. They arise from cystine compounds (a sulfur-containing amino acid). The stones are round, smooth, soft, yellowish in color.
- Oxalate. They are formed from salts of oxalic acid. The stones are dense, with a very rough, uneven surface.
- Urate. They are formed from salts of uric acid. The stones are smooth or slightly rough, dense.
- Carbonate. They arise from salts of carbonate acid. With a smooth surface, soft consistency, they come in different shapes.
- Cholesterol. They arise from cholesterol. They are black in color, soft in consistency, and crumble easily.
- Protein. They are formed from fibrin protein and salts. These are flat and soft stones, painted white.
Carbonate, cholesterol and protein formations in their pure form are rare. There is another type of stones - mixed. This means that they have a heterogeneous structure and different composition in individual areas. The most commonly mixed stones are coral stones.
Urolithiasis (kidney stones): complications
It is impossible not to pay attention to the discomfort the disease brings, and most often it is impossible, since the disease is accompanied by severe pain. The consequence of lack of treatment is multiple complications. And urolithiasis can not only develop into chronic kidney disease, but also cause such consequences as:
- chronic renal failure;
- chronic pyelonephritis;
- chronic cystitis (hypertrophic);
- paranephritis and pyonephrosis;
- anemia, etc.
Nephrolithiasis, urolithiasis, kidney stones: what is it?
Kidney stones occur due to abnormal functioning of the body's genitourinary system. The kidneys perform a large amount of work to cleanse the body of waste and toxins, and when stones appear, the intensity of the work and its quality decreases, which leads to the development of other diseases.
Kidney stones (sometimes only in the right or left, sometimes in both) are a hard mass that is the result of crystallization of salts in the urine. The resulting stones can vary in shape and size, but even the smallest kidney stone can cause excruciating pain.
Nephrolithiasis of the kidney: forms and classification:
- a mild form of the disease, which manifests itself in the form of sudden pain or discomfort in the kidneys and lower back (may intensify when pressing on the kidneys or shaking);
- an acute form of the disease, which manifests itself as very severe and most often constant lumbar and kidney pain, for which even painkillers do not help;
- a chronic form of the disease that “behaves quietly” but manifests itself during external “provocations”.
All forms of the disease are treatable, but the timing and methods vary and also depend on each specific case. First of all, the doctor will eliminate pain and discomfort when urinating.
Causes of kidney stones
Factors that provoke the formation of stones are internal and external. Internal reasons are:
- genetic predisposition;
- pyelonephritis, urethritis, cystitis and other inflammatory diseases of the urinary system of infectious origin;
- metabolic disorders: hyperparathyroidism (hyperfunction of the parathyroid glands), gout;
- infectious diseases not related to the urinary tract (angina, osteomyelitis, furunculosis, salpingoophoritis, etc.);
- excess, deficiency or increased activity of certain enzymes in the body;
- diseases of the liver and biliary tract;
- congenital anomalies of the kidneys, ureters;
- gastrointestinal diseases (gastritis, pancreatitis, etc.);
- lack of physical activity due to bed rest (due to injuries, illnesses).
External reasons include:
- adverse environmental impacts;
- characteristics of the soil, climate, chemical composition of the water used in the area of residence (the presence of some salts in the composition);
- sedentary lifestyle;
- harmful working conditions (hard physical work, high temperatures, chemical fumes, etc.);
- abuse of foods rich in purines (nitrogen compounds that are converted into uric acid in the human body): such products include meat and offal, fish (especially river fish), asparagus, cauliflower, broccoli;
- drinking too little fluid.
Causes
Factors influencing the development of ICD are varied. These are exogenous (external) and endogenous (internal, physiological) forces, the combined impact of which leads to the gradual formation of stones.
- Hereditary predisposition to metabolic disorders is one of the most important reasons. Metabolic disorders lead to the formation of insoluble salts, which cause the growth of stones.
- Another common cause is primary and secondary disorders of the kidneys and/or genitourinary tract (infections, inflammatory processes).
- No less significant factors are congenital and acquired malformations of the urinary tract, hidden urogenital infectious processes and general health (ICD often develops against the background of other pathologies of the body).
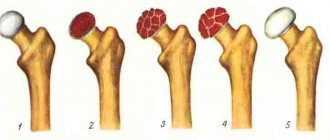
- Overactivity of the parathyroid glands (in postmenopausal women with osteoporosis, excess calcium may occur).
- Long-term use of medications.
- Deficiency of vitamin D (affects the absorption of calcium), B vitamins and other hypovitaminosis.
- Urodynamic disturbances due to pregnancy (the uterus grows and puts pressure on neighboring organs).
- Composition and salt content of drinking water: drinking hard water saturated with minerals leads to pathology.
- Insufficient water intake. The need for fluid increases in hot climates and during physical activity.
- Nutritional errors: spicy, pickled, sour, salty foods increase the risk of illness.
- Lack of movement.
Symptoms
The following signs indicate the presence of kidney stones:
- Pain in the lumbar region, side or lower abdomen (can also radiate to the groin area). Unpleasant sensations usually intensify during physical activity, movement, driving on uneven roads, and also after drinking large quantities of liquid or alcohol. The pain can be periodic or constant (in this case, it intensifies for periods, then subsides, but does not go away completely). A common type of stone pain is renal colic. The attack lasts from several hours to several days. The cramping pains wax and wane, and at times can be so severe that the patient cannot stop screaming.
- Blood in urine. Urine may be intensely red or pinkish. And in some patients, blood in the urine is detected only by test results.
- Delayed urination when there is an urge. This is a dangerous condition that requires immediate medical attention. It is caused by blockage of the urinary tract with stones. The patient is unable to empty the bladder independently; a catheter is required. Urinary retention may be accompanied by vomiting, itching, diarrhea, cramps, headache, cold sweat, chills, and fever.
- Sand in urine.
- Frequent urge to urinate.
- Nausea and/or vomiting.
- Cloudy urine.
- Pain when urinating.
- Increased temperature and blood pressure.
Signs usually appear when the disease is advanced. In the early stages, the pathology can be asymptomatic for a long time. Therefore, it is important to undergo annual preventive examinations with a urologist.
Diagnostics
Diagnosis of the disease is carried out by a urologist, who, if necessary, refers the patient to a surgeon. First, a history is taken and the patient is examined. Then the following mandatory studies are prescribed:
- general and biochemical urine and blood tests;
- urography (x-ray examination of the urinary tract);
- Ultrasound of the urinary system.
Additionally, the following may be assigned:
- computed tomography of the kidneys (to assess the size and density of the stone and the condition of the surrounding tissues);
- radionuclide kidney scan (to assess kidney function);
- urine culture for microflora (to detect infection in the urinary system).
Treatment
Surgical treatment is prescribed in the following cases:
- if conservative therapy is ineffective;
- in the presence of complications.
Before surgery, the patient is prescribed antibiotics, antioxidants and drugs that improve blood microcirculation.
Surgical intervention can be:
- minimally invasive (low-traumatic, the operation is performed through small punctures or natural holes);
- traditional (open surgery is performed through incisions).
Minimally invasive methods include:
- Laparoscopic operations. A small incision (1-2 cm) is made in the lumbar region, through which a special instrument, a trocar (a tube) and a probe, are inserted into the kidney. If the stone is small, it is removed immediately; if it is large, it is first crushed.
- Endoscopic operations. Such surgical treatment is carried out through natural routes or through small punctures using an endoscope.
Traditional surgical methods include:
- Nephrolitomy is an operation in which a stone is removed from the pelvis or calyces of the kidney;
- Ureterolithotomy – surgical removal of a stone from the ureter;
- Pyelolithotomy – removal of a mass from the renal pelvis.
Traditional surgical methods are resorted to if the stone is large or the patient has kidney failure.
Prevention
After surgery, it is important to take preventive measures. Otherwise, stones may recur. Prevention includes:
- Drinking enough water (1.5-2 liters per day). And in hot weather or during active physical activity, it is recommended to drink once or twice an hour (100-150 ml of water).
- Dieting. The development of the diet should be carried out by a doctor, taking into account the composition of the stones, as well as the characteristics of the body and the patient’s medical history.
- Daily physical activity to improve blood flow. Walking will be enough. However, they must be regular and include at least 10,000 steps per day (it is not necessary to take that many steps at a time).
- Limit the amount of alcohol consumed (or better yet, give it up altogether).
- Reducing the amount of salt consumed - to reduce the load on the kidneys.
- Avoiding hypothermia.
- Refusal to drink drinks that are too cold (especially those containing yeast: kvass, beer).
- Timely treatment of diseases, especially infectious ones.
- Annual general urine test.
- Spa treatment. A patient who has undergone surgery to remove kidney stones is recommended, if possible, to visit mineral water resorts annually (1-2 times).
The doctor may also prescribe drug therapy aimed at preventing the recurrence of stones.
Types of Kidney Stones
Table 1. Characteristics of various kidney stones
| Types of stones | Color | Structure | Density |
| Phosphates | White, light gray | Smooth | Soft |
| Oxalates | Grey, black | With sharp edges | Dense, hard |
| Urats | Brick color | Smooth | Dense |
| Cystines | Yellowish, light brown | Smooth | Soft |
| Protein stones | White, light | Smooth | Soft |
Cystine stones
. Diagnosed in 1% of patients.
- Causes: congenital defect resulting in impaired absorption of cystine (amino acid).
- Treatment: The basis is a diet that limits cystine and methionine. Penicillamine, which forms soluble compounds with cystine, can be administered.
- Diet: the basis should be milk and its products, as well as plant products. You need to drink plenty of fluids. Consumption of meat and meat products should be limited.
Phosphate stones (struvite)
. Diagnosed in 5-10% of patients.
- Causes: Frequent urinary tract infections with urease-producing bacteria, that is, Proteus, Klebsiella and Pseudomonas. Urease is the breakdown of urea into ammonia and the alkaline reaction of urine.
- Treatment: The most important is acidification of the urine. However, this cannot be achieved through diet alone. It is necessary to take acidifying drugs.
- Diet: consists of avoiding foods rich in calcium and phosphates, that is, legumes, potatoes, large amounts of vegetables, fruits, milk and eggs. Recommended are fish, cereals, pasta, bread, butter, meat.
Oxalate urolithiasis (calcium oxalate).
Diagnosed in 70-80% of patients with urolithiasis.
- Reasons: it may be hyperparathyroidism, an overdose of vitamin D3, excessive excretion of calcium, citrates and oxalates from the body.
- Treatment: increase fluid intake to 4-5 liters per day. Drugs that retain calcium in the digestive tract and reduce urinary excretion.
- Diet: Mainly consists of limiting oxalate intake. You cannot eat chocolate, cocoa, spinach, rhubarb, sorrel, lemons, beets, hot spices, alcohol, oranges. Coca-Cola, coffee and tea are prohibited. In very small quantities you can eat potatoes, tomatoes, peas, plums, and strawberries. Recommended foods include yeast, eggs, wholemeal bread, cereals, lean meats, fish, poultry, cucumbers, lettuce, butter, onions and fruits.
Cholelithiasis gout. Diagnosed in 5-10% of patients.
- Causes: Occurs when the urine pH is acidic or the body produces excess uric acid. This also affects patients with lymphoma, leukemia and bone marrow diseases.
- Treatment: These stones can be dissolved by taking appropriate tablets. Agents that change the acidity of urine to alkaline are also used.
- Diet: it is necessary to reduce the acidity of urine. This can be achieved by consuming dairy products and plenty of vegetables and fruits. The second rule is to limit foods that are sources of purine (purine bases), which are found in offal (liver, lungs, tongues, kidneys, brain and heart), decoctions, jellies, meat sauces, sardines and herring. Legumes (peas, beans, lentils and beans) and mushrooms are rich in purines. They also contain cocoa, coffee and tea. Pork, beef and lamb should be avoided. It is best to cook meat by steaming and in plenty of water. Lean poultry and veal are recommended. However, their amount in the daily diet should not exceed 100-150 g. Vegetables, fruits, sugar, butter in small quantities, milk, low-fat cheese, and potatoes are recommended. The total daily calorie content of foods should not exceed 2000-2200 kcal.
Plants that are advisable to take for this form of lithiasis: leaves of lingonberry, black currant, leaves and buds of birch. A glass of decoction of this mixture should be drunk at least 3 times a day between meals.
Decoction