Causes
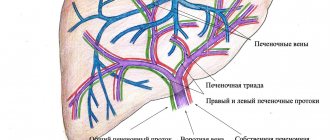
The leading role in the formation of pathology is played by the traumatic factor. Both frequent injuries of the same type and excessively high physical activity can lead to the development of osteochondropathy. The result of systematic local injury or strong muscle contractions is compression, and then complete failure of the function of the vessels that feed the bone.
There are also a number of factors that increase the risk of osteochondropathy:
- Hereditary predisposition. Cases of osteochondropathy of the hip joint are described, which were recorded in representatives of several generations of the same family.
- Metabolic disorders, for example, vitamin deficiencies.
- Hormonal factors. Osteochondropathies occur more often in patients with endocrine pathologies.
The action of pathological factors leads to the development of subchondral necrosis of certain areas of the bone. Gradually, destruction of bone tissue occurs, and then a change in the shape of the affected area, which is often accompanied by deformation of the nearest joint.
Prevention
To prevent the development of osteochondropathy, the following recommendations should be followed:
- Monitor children who have a hereditary tendency to develop this disease. At the first suspicion, consult a doctor.
- Provide children with a balanced diet high in vitamins and microelements (phosphorus, calcium, magnesium).
- Timely diagnose concomitant diseases and pathologies, in particular metabolic disorders, blood supply to bone tissue, etc.
- Control body weight, preventing obesity , treat eating disorders (anorexia, bulimia).
- If you are prone to osteochondropathy, exclude participation in traumatic sports, as well as those sports activities that require prolonged stay in anatomically unnatural positions.
- Wear properly fitted shoes that do not pinch or cause discomfort.
- Engage in physical exercise aimed at strengthening the muscle corset. It is recommended to swim more often and conduct preventive massage sessions.
Distinctive signs of osteochondropathy
All pathologies that belong to this group of diseases have a number of common manifestations:
- They are detected only in children and adolescents (with the exception of two rare pathologies: Koenig's disease and Kienbeck's disease).
- All osteochondropathy go through certain stages of development, which are accompanied by characteristic anatomical manifestations and X-ray signs.
- Benign course and relatively favorable prognosis.
- The average duration is 1-5 years.
The pathological process affects the epiphyses (expanded terminal areas) and apophyses (tendon attachment areas) of tubular bones. Less common is osteochondropathy of the spine and spongy bones.
Treatment and Prognosis
Treatment of aseptic necrosis of the epiphyses of bones in children due to high reparative capabilities during the growth period should be conservative, with unloading of the affected limb and the use of physiotherapeutic procedures. If O. in children and adults results in deformation of the articular end, in some cases surgical intervention is indicated: corrective osteotomies (see), arthroplasty (see), etc.
The prognosis for life is favorable. The prognosis of Osteochondropathy in relation to the restoration of limb function is determined by the timeliness of treatment. Self-healing is rare. Due to late or irrational treatment, complete restoration of the bone shape and function of the limb usually does not occur - consequences in the form of arthrosis remain.
Bibliography:
Volkov M. V. Bone diseases in children, M., 1974; Kosinskaya N. S. Degenerative-dystrophic lesions of the osteoarticular apparatus, L., 1961; Multi-volume guide to orthopedics and traumatology, ed. N. P. Novachenko and D. A. Novozhilova, vol. 1, p. 516, M., 1967; Multi-volume guide to pathological anatomy, ed. A. I. Strukova, vol. 6, p. 60, M., 1962; Revenko T. A., Astakhova E. I. and Novichkova V. G. On the etiology of aseptic necrosis of the femoral head in adults, Orthop, and trauma. No. 10, p. 38, 1978; Reinberg S. A. X-ray diagnosis of diseases of bones and joints, book. 1-2, M., 1964; Rubasheva A. E. Private X-ray diagnostics of diseases of bones and joints, p. 57 and others, Kyiv, 1967; Startseva I. A. and Lensky V. M. Morphological changes in aseptic necrosis of the femoral heads in adults, Orthop. and traumat., No. 12, p. 56* 1977; Shumada I.V. et al. About aseptic necrosis and racemose restructuring of the epiphyses of bones in adults, in the same place, No. 7, p. 33, 1980; Bely M. Histological differential diagnosis of aseptic bone-necrosis, Acta morph. Acad. Sci. hung., v. 27, old 95, 1979; Campbell's operative orthopedics, ed. by J. Speed, v. 11, p. 1171, L., 1956; Colas M., Carret JP et Fischer L. Contribution a Petude de la vascularisation intraosseuse de l'astragale, Bull. Ass. Anat. (Nancy), t. 59, p. 819, 1975; Edeiken I. a. Hodes P. Roentgen diagnosis of diseases of bone, Baltimore, 1973; Lichtenstein L. Diseases of bone and joints, St Louis, 1975; Melsen F. a. Nielsen HE Osteonecrosis following renal allotransplantation, Acta path, microbiol. scand., v. 85A, p. 99, 1977; Orthopedic surgery and traumatology, ed. by J. Delchef ao, p. 438, Amsterdam, 1972; Puls P. Die Primarlasion und Pathogenese der idiopathischen Hiiftkopfnekrose, Z. Rheumatol., Bd 35, S. 269, 1976; Wade S. E. ao Incidence of dysbaric osteonecrosis in Hawaii's diving fishermen, Undersea Biomed. Res., v. 5, p. 137, 1978.
E.P. Mezhenina; N. K. Permyakov (pat. an.), V. V. Kitaev (rent.).
Development of the pathological process
The course of all osteochondropathy is characterized by 5 successive stages:
- Aseptic necrosis. This stage lasts up to several months and is manifested by pain in the affected area. The onset of the disease is not accompanied by changes on x-ray, but at 2-3 months of progress a weak local compaction of the bone substance is revealed.
- Impression fracture. It is characterized by further disruption of the structure of the bone area and its compaction. The expansion of the joint space begins. The stage lasts on average until the end of the 6th or beginning of the 7th month of the disease.
- Resorption. The dead area of bone is divided into small fragments. The articular surface of the bone is deformed. The duration of the stage is from six months to 2-3 years.
- Reparative (restorative), during which dead bone tissue is replaced by newly formed rough bone substance. This process takes from 6 months to 2 years.
- At the final stage, the affected area is completely replaced by altered tissue.
The development of aseptic necrosis is usually preceded by either mechanical trauma or prolonged ischemia (lack of blood supply). As compensation, an inflammatory process occurs. But if the traumatic effect continues, as for example in the case of high sports loads, or ischemia persists, and even more so if it is aggravated by taking anti-inflammatory drugs that block compensatory inflammation, the stage of necrosis occurs. In other words, the death of bone or cartilage tissue occurs.
The pathological process often ends with deformation of the affected area, the severity of which will depend on the correct choice of therapy and complete unloading of the joint during the illness. Lack of treatment or incorrect patient management tactics can lead to the development of persistent bone deformation and secondary osteoarthritis in the child.
Pathogenesis
To date, the pathogenesis of some forms of the disease remains poorly understood. Scientists have put forward numerous theories about the mechanism of development of the disease and its causes. Currently, the development of the disease is explained by the influence of a number of pathological factors. These include the resulting microtraumas, metabolic disorders, dysfunctions of the nervous and cardiovascular systems, too much mechanical stress, etc. In the pathogenesis of aseptic necrosis, local circulation is impaired due to mechanical damage to blood vessels, embolism , thrombosis , etc.
During the development of the disease, a dystrophic-necrotic process occurs, which is conventionally divided into five stages. At the first stage, as a result of circulatory disturbances in the area of the epiphysis or apophysis, necrosis occurs. At the second stage, at the slightest load, a secondary impression fracture occurs. At the third stage, fragmentation is noted due to the resorption of some areas of the cancellous bone that has undergone necrosis. At the fourth stage, repair occurs due to the fact that the connective tissue grows. The fifth stage - consolidation - develops as a consequence of ossification. In this case, the epiphysis is deformed or completely restored subject to timely and correct therapy.
Stages of osteochondropathy
Characteristics of individual osteochondropathy
Let's look at the symptoms and characteristics of the most common variants of the disease.
Legg-Calvé-Perthes disease
Osteochondropathy of the femoral head occurs in young children and adolescents before the onset of puberty. The disease occurs much more often in boys than in girls. The pathological process is characterized by a long course: the average duration is 3 years, but sometimes the disease drags on for up to 5 or even 6 years. Pathological changes are usually unilateral (most often detected on the left), but in some cases the joints on both sides are affected.
The main reasons for the development of Perthes disease are previous trauma to the affected area or excessive sports activity in combination with local congenital vascular disorders. The following factors are also allowed:
- Hereditary predisposition.
- Foci of infection.
- Dysplastic nature of the disease.
The pathological process develops slowly. Symptoms at the first stage of the disease are mild: children complain of paroxysmal pain in the joint, which, as a rule, radiates to the knee. Further development of the disease leads to the child quickly getting tired when walking and limping. In the absence of medical care or inadequate treatment, the possibility of free movements in the joint becomes difficult, and then the leg on the affected side becomes shorter than the healthy one. The most unfavorable outcome of the disease is the development of osteoarthritis of the hip joint in children with impaired function and severe pain.
Osteochondropathies of the knee joint
Osteochondropathy of the tibial tuberosity, or Osgood-Schlatter disease, is typical for boys over 13 years of age. The lesion may be unilateral or bilateral.
Osgood-Schlatter disease sometimes develops in adolescents who are otherwise healthy. In other cases, the patient may note a connection between the pathological process and high loads on the legs during intense sports training or classes at a ballet school.
An objective manifestation of the pathology is a painful swelling located just below the kneecap. In Osgood-Schlatter disease, the main complaint of patients with the disease is knee pain, which intensifies when walking and running. The functionality of the joint is not impaired or suffers slightly.
Another variant of osteochondropathy of the knee joint is Sinding-Larsen-Johansson disease. It is also diagnosed mainly in boys over 10 years of age who are actively involved in sports. The pathology is manifested by osteochondropathy of the lower or (less often) upper part of the patella. Subjectively, the disease manifests itself as pain in the anterior part of the knee joint, its intensity increases with fast walking, running, and climbing stairs. Larsen's disease can be combined with Osgood-Schlatter disease.
Keller's disease-II
Osteochondropathy of the metatarsal bone predominantly affects teenage girls. The disease has a gradual onset. In the area of the 2nd or 3rd metatarsal bone of the foot, paroxysmal pain appears, which provokes lameness. When the period of severe pain subsides, the patient stops limping.
There is slight swelling at the site of the lesion. In the absence of treatment or improper therapy, shortening of the corresponding finger is observed, which is accompanied by limitation of movements and severe pain on palpation.
Keller's disease-I
Osteochondropathy of the scaphoid is a rare pathology that occurs in preschool-age boys. The cause of the disease is trauma, as well as bone deformation caused by a lack of vitamin D.
Keller's disease I is accompanied by pain that worsens while walking and swelling in the area of the inner surface of the foot. As the disease progresses, lameness develops.
Scheuermann-Mau disease (Schoermann-Mau)
A fairly common disease, which is accompanied by damage to the apophyses of the vertebrae, occurs in adolescents, most often males. With Scheuermann-Mau disease, kyphosis of the middle and lower part of the thoracic spine occurs. A cosmetic defect develops: the back takes on a rounded appearance. As a rule, this is a reason to consult a doctor, since pain in this pathology is mild.
Calvet disease
Osteochondropathy of the vertebral body is a rare disease that is usually observed in young boys. The reasons for the development of the disease are unclear; the role of hereditary predisposition is assumed.
In most cases, Calve's disease involves damage to the thoracic vertebra. The child suddenly begins to complain of pain and fatigue in the back. Pain and swelling in the area of the affected vertebra are objectively determined.
Schinz's disease
The disease is osteochondropathy of the calcaneus. Schinz's disease develops in children during adolescence, more often in girls. Provoking factors are increased sports loads and constant injury to the heel tubercle area (for example, when wearing uncomfortable shoes). The calcaneal tuberosities on both sides are often affected.
Schinz's disease is accompanied by heel pain, which intensifies after a long walk, jumping, or running. A dense swelling forms in the area of the heel tubercle without signs of inflammation.
Partial osteochondropathy
These variants of the disease are characteristic of adolescent males and young men. Most often, partial osteochondropathy is localized in the knee joint. Local necrosis forms on one of the articular surfaces, which can lead to the formation of the so-called “articular mouse” - a freely located intra-articular body. Partial osteochondropathy is also accompanied by pain, the severity of which intensifies after physical activity.
Clinical picture
O.'s course is usually long-term (2-3 years). D. G. Rokhlin (1952) distinguishes 3 phases wedge, the course of aseptic necrosis: the necrosis phase, the degenerative-productive phase, or the fragmentation phase, and the outcome phase. In the first phase, the patient complains of fatigue, vague painful sensations; slight functional impairments appear, local pain, lameness (if the lower extremities are affected), then compression of the necrotic area of the bone occurs. In the second phase, the pain intensifies, the patient spares the affected limb. By the end of the second phase, the pain may disappear, but the function of the limb is not restored. In the third phase, a recovery process or the development of deforming arthrosis with the resumption of pain is observed.
In children during the growth period, aseptic necrosis leads to impaired osteogenesis—inhibition of enchondral ossification. With the development of secondary ischemic disorders, premature closure of the growth plate and deformation of the articular end of the bone are observed.