What is hepatic colic?
The content of the article
Hepatic colic, also known as biliary colic, is a condition characterized by severe abdominal pain in the right hypochondrium or middle epigastrium (upper abdomen).
Hepatic colic usually occurs when you eat heavy or fatty foods. The condition is very unpleasant, the pain can extend to the back, and associated symptoms may include gas, heartburn or vomiting.
Heartburn
The pain of hepatic colic comes on suddenly and disappears slowly, sometimes lasting up to several hours. Hepatic colic is not a disease in itself, but may indicate more serious diseases, such as the gallbladder. Ignoring the problem can lead to serious complications.
Why do gallstones form?
The exact cause of cholelithiasis has not yet been fully elucidated. Only a few factors are known that increase the likelihood of its occurrence.
- Genetic: family predisposition increases the risk of cholelithiasis by 4-5 times;
- Congenital anomalies of the biliary tract;
- Gender - the risk of developing gallstones in women is approximately 2-3 times higher, which is associated with the influence of estrogens on the ability to form gallstones;
- Age - the maximum frequency of clinical manifestations of cholelithiasis is recorded at the age of 40-69 years;
- Dietary (high-calorie diet, poor in plant fiber, as well as with an excess of simple carbohydrates, animal proteins, foods containing cholesterol);
- Use of medications (oral contraceptives, fibrates, ceftriaxone, somatostatin, nicotinic acid);
- Concomitant diseases and conditions (obesity - a tendency to form gallstones in persons with a body mass index of more than 30 is 3 times higher, type 2 diabetes mellitus, hypothyroidism, cirrhosis of the liver, etc.);
- Pregnancy - the risk of developing cholelithiasis increases during pregnancy, especially with repeated pregnancies (the likelihood of stone formation increases by 10-11 times). During pregnancy, bile heterogeneity, or the so-called biliary sludge, develops in 20-30% of patients, stones - in 5-12% of cases.
There is a so-called 5F rule that describes patients at greatest risk of developing stones:
1. Female (female);
2. Fat (overweight/obesity);
3. Forty (age 40 years or more);
4. Fertile (fertile women - that is, pregnant and giving birth);
5. Fair (light-skinned blondes).
Hepatic (biliary) colic - causes
Eating large amounts of foods containing animal fats is associated with high cholesterol levels. This, in turn, causes the formation of deposits that accumulate in the gallbladder and interfere with its function. The function of the gallbladder is to push out the bile needed to digest food - if something interferes with the contraction of the gallbladder, it must contract more intensely. This is the direct cause of hepatic colic and the severe pain associated with it.
Colic occurs when accumulated bile has difficulty moving due to deposits in the gallbladder or bile ducts.
How does the liver work?
The liver is the largest gland in humans. It is located in the upper floor of the abdominal cavity on the right. It consists of two main lobes - right and left, which in turn are divided into 8 segments.
In an adult, it weighs about 1/40 of the total body weight (approximately 1.6 kg in men and 1.2 kg in women). The liver has a dual blood supply: approximately 80% of the blood entering the liver comes from the portal vein (venous blood collected from all unpaired abdominal organs), the rest (oxygenated arterial blood) comes from the hepatic artery. Having entered the portal of the liver, both vessels give rise to multiple branching smaller vessels. At the exit from the liver, 3-4 hepatic veins are formed, which flow into the inferior vena cava.
The main structural unit of the liver is the hepatic lobule, which consists of liver cells - hepatocytes. This cell is one of the most important biochemical laboratories of the body. The hepatocyte takes part in the metabolism of proteins, carbohydrates, fats, bile acids, and vitamins. Neutralizes toxic substances coming from the intestines, followed by the release of associated products into the intestinal lumen. An important function of the hepatocyte is the synthesis of bile, which is involved in digestion.
Cholelithiasis
Gallstones are nothing but the presence of deposits in the gallbladder or bile ducts. Gallstones are more likely to affect women, obese people, older adults, diabetics, and patients taking oral contraceptives or other estrogen medications.
Gallstones
Gallstones can occur at the same time as duct stones because deposits in the gallbladder are tiny and can travel with bile into the bile ducts, blocking their narrow lumen. In addition to hepatic colic, jaundice indicates urolithiasis, which is additionally accompanied by a change in the color of the stool and unpleasant itching of the skin.
Main symptoms of liver diseases
A variety of symptoms, many of which have a rather characteristic manifestation, will help the doctor to promptly identify the problem and prescribe treatment. However, there remains a danger that some diseases in the early stages are practically asymptomatic. To eliminate the risk of developing the disease and diagnose the liver in a timely manner, gastroenterologists and hepatologists recommend paying attention to some points.
Liver dysfunction can manifest as one symptom or a combination of them, which depends on the specific disease and the presence of associated complications.
Pain and discomfort
Painful sensations are usually concentrated in the right hypochondrium. In some cases, they can radiate to the area between the shoulder blades, separately to the right shoulder blade. Pathology can be assessed based on the type and intensity of pain. For example, minor discomfort with aching pain, which complements the feeling of heaviness, may indicate the presence of an inflammatory process, including that caused by toxins. It is very difficult for the patient to clearly show the place where the pain is concentrated.
Intense and severe pain in the hypochondrium is characteristic of severe inflammation, including purulent inflammation. It is present in cases of stones in the bile ducts, liver injuries. Painful sensations are also typical for hepatic colic, which is caused by the movement of stones in the bile ducts.
There are pathologies that do not manifest themselves as unpleasant sensations. These are indolent processes, such as hepatitis C or cirrhosis of the liver. The patient does not notice them for a long time, which is why liver diagnosis and treatment may be delayed. Often these diseases are detected already in the later stages of development.
Vomiting and nausea
Feelings of nausea and vomiting are quite common with gastrointestinal diseases. If the problem affects the liver, these symptoms will be much more severe.
With the appearance of nausea, problems with appetite begin - it becomes dull or disappears completely. There is an aversion to specific foods, usually high in fat. In some cases, an attack of nausea ends with vomiting, after which relief occurs for a while. An admixture of bile in vomit indicates liver problems.
Manifestation of symptoms in the oral cavity
A characteristic symptom is the appearance of a yellow coating on the tongue. The intensity and color depend on the disease. For example, slight jaundice closer to the tip of the tongue may indicate an early stage of hepatitis. The appearance of a yellow-green coating is characteristic of serious pathologies of the gastrointestinal tract, biliary tract or liver. Stagnation of bile manifests itself in the form of a rich yellow coating. At these stages, tests may be prescribed to check the gastrointestinal tract.
An unpleasant bitterness may also be present. It occurs when bile enters the esophagus. The presence of a pronounced taste may be a symptom of viral hepatitis, liver tumor or cirrhosis, gastrointestinal tract disease or gall bladder. Sometimes bitterness is caused by severe stress and taking certain medications. To accurately determine the disease, doctors prescribe a comprehensive diagnosis of the patient’s body.
In addition to bitterness, a sweetish or “fishy” aroma may appear in the mouth, which is accompanied by constipation or diarrhea, bloating, and vomiting. This symptom indicates problems with the digestive system caused by liver problems.
Increased body temperature
A symptom indicates the presence of a pathogenic agent that the body is fighting. When the temperature rises to 38°C and fluctuates between 37-37.5°C, liver cirrhosis and hepatitis can occur.
In diseases of the biliary tract, the temperature remains at 39°C and above. In this case, the patient experiences twitching of facial and skeletal muscles.
Change in color of urine and stool
Due to the increased volume of bilirubin, characteristic of hepatitis or cirrhosis, the urine acquires a dark tint. When shaken, a rich yellow foam appears in it.
Some diseases are characterized by discoloration of stool, which is accompanied by fever and discomfort in the right hypochondrium. Vomiting may be present.
Changes in skin and mucous membrane color
Due to the accumulation of bile pigments in the tissues, the color of the mucous membranes and skin changes. This may indicate the presence of cirrhosis or hepatitis, especially if there is dark urine and light-colored stool. Yellowness of the skin is present in cholelithiasis. To clarify the diagnosis, the doctor may prescribe additional laboratory tests.
Problems with bile secretion sometimes appear as brown pigment spots with varying degrees of intensity. They usually occur in the groin, armpits or palms of the hands.
Other skin manifestations
An additional symptom that is observed in liver pathologies are spider veins. They usually appear on the back or cheeks. They are caused by metabolic problems and increased fragility of capillary walls. At an advanced stage, the patient immediately develops bruises with slight pressure on the skin.
Autoimmune diseases and hepatitis caused by infection are accompanied by allergic rashes and inflammation. At the next stage, atopic dermatitis and psoriasis may appear.
A characteristic symptom is “liver palms,” in which red spots appear on the feet and palms. They become paler when pressed. When the pressure stops, their color turns red again.
Hormonal changes
Chronic liver diseases cause hormonal imbalance. In this case, patients experience hair loss on the pubis and armpits. Men suffer from testicular atrophy and enlarged mammary glands - this is caused by an excess of female hormones. In women, the volume of estrogen increases, which is why a rash appears throughout the body, PMS becomes very pronounced, and the menstrual cycle is irregular.
Intoxication of the body
Since the liver is responsible for filtering and eliminating toxins from the body, liver damage interferes with these functions. Severe intoxication and accompanying symptoms occur. These include discomfort in muscles and joints, problems with appetite, fatigue and weight loss.
Diagnosis of hepatic colic
As already mentioned, hepatic colic usually indicates gallstone disease, so this disease should not be ignored. In any case, you should visit a gastroenterologist who will perform a physical examination and imaging.
The most useful test for diagnosing hepatic colic (due to gallstones) is an abdominal ultrasound. This test can detect stones in the gallbladder and sometimes even in the bile ducts.
Abdominal ultrasound
However, endoscopic retrograde cholangiopancreatography or EUS (endoscopic ultrasound) is more sensitive. These two studies are performed when choledocholithiasis is suspected and allow visualization of the bile ducts from the inside and removal of deposits or dilation of the bile ducts to the duodenum.
Differences in flow between men and women
Symptoms in women and men during the development of an attack are the same. The provoking factors are slightly different:
- in men, the appearance of hepatic colic is more often provoked by alcohol consumption and physical exertion;
- In women, an attack usually occurs when taking contraceptives, during menstruation, or in late pregnancy.
The symptoms that occur with hepatic colic in women are similar to the manifestations of some gynecological pathologies and, before starting treatment, a differential diagnosis is carried out. In addition to undergoing tests and being examined by a surgeon, the woman is sent for a consultation with a gynecologist.
Hepatic (biliary) colic - treatment
Treatment for hepatic colic is specialized because, as mentioned above, it is not a disease in itself, but a symptom of another ongoing disease. Colic goes away as soon as its cause is eliminated.
Thus, the treatment of this disease consists of the following measures:
- Taking painkillers such as non-steroidal anti-inflammatory drugs or paracetamol. Patients should not be given morphine as it may worsen symptoms;
- Administration of drugs that relax the smooth muscles of the gastrointestinal tract, such as papaverine, scopolamine or drotaverine;
- Using the procedure – gallbladder removal when we are dealing with symptomatic gallstones;
- The use of endoscopic retrograde cholangiopancreatography with prosthetics of the biliary tract or expansion of the outlet into the biliary tract.
Taking painkillers
Further treatment
During an attack, the patient is hospitalized in a hospital. Treatment of hepatic colic is carried out by conservative or surgical methods. If the symptom is caused by cholelithiasis, a therapeutic diet is prepared and physical therapy is prescribed. In case of prolonged attacks (more than 8 hours) and frequent relapses, they resort to cholecystectomy - removal of the gallbladder along with choleliths. In case of isolated episodes of colic, doctors observe the patient.
Diet and lifestyle
Dietary nutrition is prescribed after the condition has stabilized. To restore the functioning of the biliary system, limit the consumption of animal products. The daily energy value of food should be 2200-2500 kcal. It is recommended to consume 90 g of protein, up to 300 g of carbohydrates and 70 g of fat per day.
The diet after hepatic colic includes:
- limiting table salt to 7 g per day;
- drinking up to 2 liters of water per day;
- fractional meals in small portions up to 6 times a day;
- refusal of fatty meats and dishes;
- consumption of heat-treated vegetables.
For a speedy recovery, adhere to a healthy lifestyle. A person must stop smoking and drinking alcohol. To improve the motility of the bile and intestines, physical therapy, breathing exercises, and swimming help well.
Pharmacy products
Cramping colic is treated with symptomatic drugs. To relieve attacks and improve well-being, the following are used:
- antispasmodics (Mebeverine, Drotaverine) – relax the muscles of the hepatic ducts and bile ducts, relieve spastic pain;
- analgesics (Baralgin, Morphine) – eliminate pain;
- antiemetic drugs (Promethazine, Metoclopramide) - relieve nausea, suppress the gag reflex.
Drug treatment of colic involves taking medications aimed at eliminating the underlying disease. For cholelithiasis, lipotropic (Ursohol, Holacid, Destolit) and choleretic (Nicodin, Artichol, Chofitol) drugs are prescribed. The former are used to break down cholesterol stones, and the latter are used to improve the flow of bile from the cystic duct.
Surgery
Surgical intervention is indicated for frequent relapses of attacks and complications of cholelithiasis.
With timely treatment, the prognosis is favorable. Otherwise, the development of serious pathological processes in the liver is possible.
The most effective surgical techniques include:
- Retrograde cholangiopancreatography. During the operation, the surgeon dissects the area where the duodenum and the bile duct connect. Due to the expansion of the opening, choleliths easily penetrate the intestines and are excreted with feces.
- Shock wave lithotripsy. A shock wave energy generator is focused on the area of the gallbladder. It remotely destroys stones in the liver canals and bladder without damaging soft tissue.
- Laparoscopic cholecystectomy. The procedure to remove choleliths is performed through small holes in the abdominal wall. The surgeon inserts medical equipment and a video camera into them. Under visual control of digital technology, he captures the choleliths with a special instrument and removes them.
- Open surgery. Radical intervention is indicated for ongoing attacks and severe complications of cholelithiasis. The surgeon removes stones from the biliary system through large incisions (length up to 30 cm) in the abdomen.
Cholecystectomy eliminates the main cause of colic – a bladder with stones. But due to the absence of an organ, patients must take choleretic drugs, enzymes, and follow a strict diet throughout their lives.
Folk remedies
It is impossible to relieve severe colic with folk remedies. But many of the medicinal herbs prevent relapses, inflammation of the bile ducts, and stagnation of bile:
- angelica;
- immortelle;
- chamomile;
- sagebrush;
- peppermint;
- thyme;
- buckthorn;
- calamus;
- Oak bark;
- sage;
- Birch buds;
- juniper;
- dog-rose fruit.
For liver pathologies and cholelithiasis, it is recommended to replace ordinary water with mineral water - Borjomi, Essentuki-19, Burkut, Narzan, etc. They are recommended to take probiotics and preparations with lactobacilli to restore intestinal microflora.
Other methods
Paroxysmal colic is a consequence of impaired hepatic metabolism and an increase in the density of bile in the bladder. To restore metabolism and transport of bile acids into the small intestine, it is recommended:
- do diaphragmatic breathing exercises;
- take daily walks in the fresh air;
- give up fast food and carbonated drinks;
- avoid stressful situations.
Physiotherapeutic procedures during periods of remission are used:
- inductometry – restores liver function using electromagnetic fields;
- ozokerite and paraffin applications - reduce spasm of smooth muscles, improve blood circulation in the hepatic and cystic ducts;
- electrophoresis - stimulates the flow of bile into the intestines, normalizes intestinal motility.
Heat therapy, that is, applications, is resorted to only in the absence of infectious inflammation in the affected organs.
Hepatic colic and diet
A properly selected diet can not only cure hepatic colic, but also relieve the symptoms of cholelithiasis. The diet should be low-fat and easily digestible.
Patients should eliminate or limit the consumption of foods such as cheese, lard, mayonnaise and cream. In addition, frying should be avoided; it is better when you cook the dish in the oven or steam.
Patients who are obese should reduce their body weight, and those who additionally suffer from hypertriglyceridemia should reduce their levels of simple sugars and disaccharides.
Weight loss in obesity
Prevention
With timely assistance, the prognosis is favorable. Preventive measures can prevent the process of stone formation in the biliary tract and reduce the risk of colic. These include:
- early diagnosis of diseases of the digestive system;
- proper nutrition;
- dosed physical activity;
- giving up alcohol;
- normalization of body weight;
- avoiding long periods of hunger.
The recommendations listed are quite simple and do not require effort to follow. They make it possible not only to normalize bile flow, but also to improve the functioning of the entire digestive system.
Complications of hepatic colic
Ignoring the disease of hepatic colic can lead to unpleasant consequences requiring hospitalization. Among the complications of untreated hepatic (biliary) colic, we note:
- acute pancreatitis;
- acute cholecystitis;
- inflammation of the bile ducts;
- in rare cases, secondary cirrhosis of the liver may occur;
- chronic inflammation of the walls of the gallbladder.
Acute pancreatitis and acute cholecystitis are diseases for which it is necessary to immediately hospitalize the patient, as they are life-threatening! Therefore, it is very important that patients do not ignore hepatic colic and in any case consult a gastroenterologist. This will help to recognize the disease in a timely manner and prevent possible complications.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
First aid
The first point of the medical care plan should be to call doctors. Next, you will have to try to calm the victim. But you should not use medications for this, as they can distort the clinical picture during subsequent diagnosis. To slightly reduce pain, the person is placed on a flat surface, turning on his right side.
Doctors conduct an initial examination by interviewing the patient or the people around him. This is necessary for drawing up a subsequent detailed treatment program. To reduce discomfort, experts use antispasmodic drugs. To increase effectiveness, injectable medications are used as a basis. They are administered intramuscularly.
You should not try to inject a patient yourself, as there remains a high risk of developing an allergic reaction to the components of the medicine. The ambulance team has in stock funds aimed at neutralizing the onset of anaphylactic shock in case of urgent need.
After providing assistance on the spot, doctors will hospitalize the victim if the severity of the disease is confirmed. In a hospital setting, specialists will conduct detailed diagnostics using ultrasound and other modern instrumental techniques.
Complications after laparoscopic cholecystectomy
The most common intraoperative complications are the intersection of the cystic artery and the common bile duct.
Bleeding from the transected cystic artery is stopped by clipping and does not cause technical difficulties for an experienced surgeon.
Damage to the common bile duct requires reconstructive intervention, which is associated with significant difficulties. In the long term, such a surgical injury can lead to a significant decrease in quality of life and disability.
Performing cholecystectomy using minimally invasive and high-tech equipment can significantly reduce the risks of intraoperative complications.
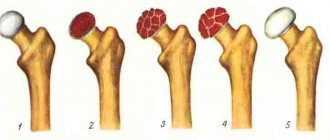
How are gallstones formed?
The process of stone formation is quite well studied. The key links are:
- An increase in the lithogenicity of bile (the ability to form stones) means an increase in the content of cholesterol and bilirubin in it.
- Impaired contractile function of the gallbladder.
- Increased pressure in the bile duct system.
Mucin is a natural gel, constantly secreted by the wall of the gallbladder; when lithogenicity increases, it begins to “absorb” cholesterol crystals, thereby forming a “fossilization nucleus.” The formed suspension, with impaired contractile function, continues to attach salt crystals encrusted with calcium salts. Thus, gallstones can grow up to 5-7 mm per year.