Chronic cholecystitis. Causes
Bacterial cholecystitis develops when pathogenic microorganisms penetrate into the gallbladder from the intestine when the microflora is disrupted (ascending path) or from the stomach when the acidity of the gastric juice is low and the outlet from the stomach is open (gaping). Routes of infection can be:
- through blood and lymphatic vessels (descending route),
- the source of infection can be chronic infectious foci in the body (chronic tonsillitis, sinusitis, chronic adnexitis - inflammation of the appendages in women, chronic appendicitis, etc.).
An infection in the gallbladder often has a “dormant” character and is clinically asymptomatic or without manifestations, but can cause allergic reactions in patients.
For microbial damage to the mucous membrane of the gallbladder, inflammation, the presence of bacteria is not enough; they often pass through “transit”, being excreted along with bile (bacteriocholia). Additional conditions for the development of inflammation in the gallbladder are stagnation (stasis) of bile, impaired contractile function of the gallbladder, and the state of local immune mechanisms in the mucosa, causing changes in the epithelial cover of the gallbladder.
Inflammation of the gallbladder mucosa may be associated with changes in the quality of bile (thick bile, sludge of bile, stone formation), when pancreatic enzymes flow into the common bile duct (“enzymatic cholecystitis”).
In a third of patients, the cause of chronic cholecystitis remains unclear. In these cases, they speak of “aseptic” chronic acalculous cholecystitis, in the development of which neither bacterial or viral infections, nor helminthic infestations, nor pathogenic fungi play a role. The state of the immune mechanisms is of decisive importance in this case.
Thus, inflammatory processes in the gallbladder develop as a reaction of the mucous membrane to various damaging factors (infection, helminthic invasion of the sphincter apparatus, fungi, trauma to the gallbladder), decreased blood supply to the mucous membrane (with ischemic disease of the abdominal cavity). In the development of chronic acalculous cholecystitis, dyskinesias of the gallbladder and biliary tract are important. They are dangerous because they lead to stagnation of bile and disrupt its physicochemical and biochemical properties. They disrupt the oxidation of fatty acids and bile phospholipids, causing allergic and immunological reactions.
The drug Creon® 25000 for chronic pancreatitis
Find out more
Decreased pancreatic function inevitably leads to a lack of digestive enzymes in the body, so-called enzyme deficiency. As a result, the quality of digestion suffers, and the body does not receive the necessary energy and nutrients for full functioning. Creon® is designed specifically to compensate for the lack of its own enzymes through their delivery from the outside and belongs to the group of enzyme preparations. The drug contains enzymes identical to those produced by the pancreas. The key feature is that the active ingredient Creon® is small particles - minimicrospheres, which are collected in a capsule. The fact is that science has been studying enzyme preparations for more than 100 years in order to increase their effectiveness. To date, scientific advances indicate that preparations with particles whose size does not exceed 2 mm4.5 can most accurately recreate the natural process of digestion. Moreover, it has been scientifically proven that the smaller the particles of the drug, the more effective it can be4,6.
Creon® is the only drug whose capsule contains hundreds of small particles - minimicrospheres7. Their size does not exceed 2 mm, which is recorded as recommended in world and Russian scientific works4,5,6.
Symptoms of chronic cholecystitis in the acute stage, forms of the disease
Chronic cholecystitis has two forms:
- acalculous cholecystitis,
- calculous cholecystitis (GSD - cholelithiasis).
In 60% of cases, chronic acalculous cholecystitis is observed. It is more common in women after 40 years of age. There are stages of the disease: exacerbation, subsiding exacerbations and remission.
Exacerbations of the disease can occur after heavy and fatty meals, in connection with psycho-emotional states, physical activity, and shaking. They usually manifest themselves as pain in the right hypochondrium with irradiation to the right collarbone, scapula, and the left half of the chest. There may be pain in the heart area, palpitations, interruptions in heart function (extrasystole) - the so-called cholecystocardial syndrome.
The pain can be dull, constant, but not cramping, accompanied by fever and chills. The pain is accompanied by dyspeptic complaints, primarily nausea (nausea), vomiting less often, which usually does not bring relief. With repeated vomiting, the vomit acquires a bitter taste and contains an admixture of bile. Another common complaint is bitterness in the mouth and bitter belching.
Appetite, as a rule, is reduced, there is a tendency to constipation, alternating constipation and diarrhea. Patients usually do not lose weight despite poor appetite and dietary restrictions.
Abdominal bloating (flatulence) is often a concern due to the presence of microflora disturbances in the intestines. Dyspeptic symptoms more often occur with chronic cholecystitis caused by Escherichia coli. With streptococcal infection, intoxication and asthenia of the body (weakness, anxiety, depression, psycho-emotional manifestations) are more common.
The pain may intensify with movement and take on the character of biliary colic, which is more often observed in the presence of stones in the gall bladder.
In chronic cholecystitis, patients often experience discomfort in the right hypochondrium after consuming fatty, fried foods, hot sauces and seasonings, and alcohol. Often there is nausea, empty (airy) belching, less often bitterness in the mouth, bloating and rumbling in the abdomen, bowel problems (usually constipation).
Acute calculous cholecystitis
Acute calculous cholecystitis is an acute inflammation of the gallbladder containing stones. Prevalence. Acute calculous cholecystitis ranks second in frequency among acute surgical diseases of the abdominal organs. In 12-24% of cases it is complicated by choledocholithiasis, in 26-49% by obstructive jaundice, in 23-47% by cholangitis.
In the development of acute calculous cholecystitis, the leading role is played by the penetration of infection into the gallbladder and disruption of the outflow of bile. Microbial flora (intestinal, Pseudomonas aeruginosa, staphylococci, enterococci) enters the gallbladder ascending (from the duodenum) or descending (from the liver) by hematogenous or lymphogenous route. The outflow of bile is disrupted when stones obstruct the neck of the gallbladder or cystic duct, common bile duct, or pathological processes in the periampullary zone. The development of calculous cholecystitis is facilitated by changes in the vessels of the gallbladder wall during atherosclerosis, damage to its mucous membrane by pancreatic enzymes during pancreatobiliary reflux.
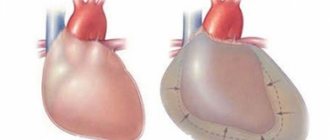
Morphologically, three types of acute calculous cholecystitis are distinguished: catarrhal, phlegmonous and gangrenous. With catarrhal cholecystitis, the gallbladder is slightly enlarged, its wall is thickened due to edema and swelling of the mucosa. The mucous membrane is cloudy due to desquamation of the epithelium and its infiltration with leukocytes. Inflammation also spreads to the submucosal layer. With phlegmonous cholecystitis, the wall of the gallbladder is significantly thickened as a result of abundant impregnation with inflammatory exudate. The mucosa is sharply hyperemic, with fibrin deposits. The bladder is much enlarged in volume, filled with purulent exudate, and covered with fibrin on the outside. In case of occlusion of the cystic duct by a stone or due to swelling of its wall, acute empyema of the gallbladder develops. With gangrenous cholecystitis, which occurs against the background of cystic artery thrombosis, partial or total necrosis of the gallbladder wall occurs. Gangrene usually occurs on the 3-4th day of the disease. Often there is perforation of the bladder wall (gangrenous-perforated cholecystitis) with the flow of bile into the abdominal cavity and the development of biliary peritonitis. Perforation occurs more often in the area of the neck of the gallbladder or Hartmann's pouch, i.e. in the places where stones are most often localized. All described pathomorphological forms of acute calculous cholecystitis are accompanied by pericholecystitis, which is characterized by a local or widespread adhesive process that limits the spread of infection to the area of the right hypochondrium.
Signs of acute calculous cholecystitis are pain in the right hypochondrium, vomiting, nausea. The pain occurs suddenly, most often after a diet violation, and radiates to the right shoulder, collarbone, lower back, and iliac region. The intensity of pain increases with the slightest physical stress. Vomiting in patients with acute calculous cholecystitis is of a reflex nature, often repeated, and does not bring relief. During an objective examination of patients, dryness of the tongue, some bloating of the abdomen and limitation of its participation in the act of breathing, severe pain and muscle tension in the right hypochondrium, especially at the point of projection of the gallbladder: the intersection of the outer edge of the right rectus abdominis muscle with the costal arch (Ker's point) are revealed. . In the absence of pronounced muscle tension in the abdominal wall in patients, an enlarged, tense, sharply painful gallbladder is often palpated (Parturier's symptom). At the same time, characteristic symptoms are determined in patients: the appearance or intensification of pain when lightly tapping the inner edge of the hand along the right costal arch (Grekov-Ortner symptom); pain on palpation in the right hypochondrium, increasing with inspiration (Keur's symptom); pain when pressing on the xiphoid process (Pekarsky's symptom); pain on palpation between the legs of the sternocleidomastoid muscle on the right above the collarbone (Mussy symptom, phrenicus symptom); the appearance or intensification of pain in the right hypochondrium when pressing with the index finger between the legs of the sternocleidomastoid muscle on the right above the collarbone (Georgievsky’s symptom); pain on palpation to the right of the navel and slightly higher in the projection of the common bile duct (Janover's symptom); pain when pressing on the right near the spinous processes of the VIII-X thoracic vertebrae (Boas symptom); irradiation of pain to the heart area (Botkin’s cholecystocardial symptom). The body temperature in patients with acute calculous cholecystitis is elevated. Neutrophilic leukocytosis and increased ESR are observed in the blood.
The severity of clinical manifestations of the disease is directly proportional to the degree of morphological changes in the gallbladder. Thus, the most rapid course is observed with gangrenous cholecystitis. However, in elderly patients, acute calculous cholecystitis occurs atypically, which is due to the lack of a clear relationship between structural changes in the gallbladder and the existing clinical manifestations. This is due to a decrease in the overall reactivity of the body and the presence of concomitant diseases. Acute calculous cholecystitis in this category of people occurs with erased local symptoms and is accompanied by rapid generalization of the main process, symptoms of intoxication, and a high incidence of complications. The body temperature of patients is usually low-grade. Tachycardia is pronounced. A discrepancy is determined between heart rate and temperature. Moderate leukocytosis with a shift to the left is detected in the blood.
The duration of acute calculous cholecystitis ranges from 3-5 days to several weeks. In most cases, the disease becomes chronic or is accompanied by complications: obstructive calculous cholecystitis - empyema or hydrocele of the gallbladder; perforation of the gallbladder (perforative, calculous cholecystitis) with the development of bile peritonitis, subhepatic and subphrenic abscesses; cholangitis; liver abscesses, etc. Complications, as a rule, accompany phlegmonous and gangrenous forms of acute calculous cholecystitis.
Empyema of the gallbladder in acute calculous cholecystitis occurs due to blockage of the cystic duct with a stone in the presence of a virulent infection in the gallbladder. Due to the progression of inflammation, pus accumulates in the lumen of the bladder. The bladder increases in size, becomes tense, and sharply painful on palpation. In the right hypochondrium, patients feel intense, constant pain that lasts for several days. The temperature rises to 38-40 °C, often taking on a hectic character with chills and frequent heavy sweating. During intensive therapy, most symptoms disappear, but patients continue to be bothered by a feeling of heaviness and pain in the projection of the gallbladder (chronic empyema). Violation of the diet and physical stress lead to an increase in body temperature to 38-39 ° C and increased pain. Hydrocele of the gallbladder most often forms after an attack of catarrhal acute calculous cholecystitis caused by microbial microflora with little virulence and preserved occlusion of the neck of the gallbladder or cystic duct. In such cases, due to the absorption of bile pigments and the death of microorganisms, colorless mucous contents are formed in the gallbladder. In the projection of the gallbladder, an elastic formation with a smooth surface is determined, which moves with inhalation along with the liver. Dropsy can exist for a long time, accompanied by a feeling of heaviness in the right hypochondrium, nausea, and vomiting. When the stone blocking the duct comes out, it disappears. In some cases, gallbladder rupture is possible.
The diagnosis of acute calculous cholecystitis is based on data from a physical examination, general and biochemical blood tests, the results of ultrasound examination of the gallbladder, liver, biliary tract, less often - laparoscopy, etc. When acute calculous cholecystitis is complicated by obstructive jaundice, ERCG is informative. Differential diagnosis of acute calculous cholecystitis. Most often, acute calculous cholecystitis is differentiated from a perforated ulcer, acute pancreatitis, right-sided renal colic, Botkin's disease in the preicteric period, and biliary dyskinesia. An attack of right-sided renal colic develops suddenly and is characterized by intense pain in the lumbar region, radiating to the groin. Urine tests determine hematuria. An ultrasound examination of the kidneys and a plain radiograph of the abdominal cavity reveal stones in the projection of the kidneys and urinary tract. In the pre-icteric period of Botkin's disease, general weakness, loss of appetite, nausea, a feeling of heaviness in the epigastrium and right hypochondrium, and an increase in body temperature up to 38 ° C prevail. Then parenchymal jaundice gradually increases: first, the sclera, soft palate, and later the skin become jaundiced. The liver and spleen enlarge. In the blood, the content of direct bilirubin is increased and cholesterol is decreased, and the activity of transaminases is increased. Urobilinuria is detected. Manifestations of biliary dyskinesias are varied, which is associated with the existence of several of their forms: 1) atony and hypotension of the gallbladder; 2) hypertensive gallbladder; 3) spasm of the sphincter of Oddi; 4) atony of the sphincter of Oddi. The atonic gallbladder is accompanied by a constant feeling of heaviness, pain in the right hypochondrium, and vomiting mixed with bile.
Ultrasound and X-ray contrast studies revealed a sharply enlarged gallbladder. With a hypertensive gallbladder, attacks of hepatic colic are frequent. By increasing the muscle tone of the wall, the gallbladder acquires a spherical shape. Hypertension of the sphincter of Oddi occurs in four forms - icteric, painful with colic, febrile and asymptomatic. Atony and insufficiency of the sphincter of Oddi are characterized by weak contrast of the bile ducts during a conventional X-ray contrast study of the biliary system with the simultaneous accumulation of a large amount of contrast in the duodenum. However, after subcutaneous administration of morphine, the shadow of the gallbladder projection becomes clear. When diagnosing acute calculous cholecystitis, one should remember some similarity of the clinical manifestations of the disease with those of acute intestinal obstruction, thrombosis of mesenteric vessels, myocardial infarction, pneumonia and pleurisy.
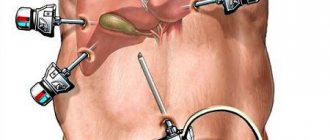
The question of tactics for managing patients with acute calculous cholecystitis should be decided individually based on the existing clinical picture and the general condition of the patients. Most surgeons adhere to active expectant tactics, the essence of which is as follows. In case of acute calculous cholecystitis complicated by peritonitis, the operation is performed immediately after the patient’s admission or short-term preoperative preparation (emergency surgery). Also, urgent cholecystectomy (in the vast majority of cases laparoscopic) is performed if the duration of the disease, from the moment of the attack, does not exceed 72 hours. In all other cases, intensive complex drug treatment is prescribed with the aim of performing the operation in the cold period, i.e. after acute inflammation in the gallbladder and bile ducts has subsided, eliminating intoxication and metabolic disorders, functional changes in vital organs and systems (planned surgery) . However, if the treatment is ineffective, jaundice increases, or signs of destructive cholecystitis occur, the operation is performed 48-72 hours after admission (urgent surgery). However, cholecystectomy, especially when the disease lasts more than 3-5 days, is associated with certain technical difficulties due to inflammatory tissue edema in the area of the gallbladder and hepatoduodenal ligament, and the formation of a dense infiltrate in the subhepatic space. They disrupt topographic-anatomical relationships and increase tissue bleeding in the surgical area, increasing the risk of developing intraoperative and postoperative complications of cholecystectomy.
For the conservative treatment of acute calculous cholecystitis, analgesics, antispasmodics, anticholinergics, antihistamines, broad-spectrum antibiotics, antioxidants, etc. are used. Novocaine blockades (subxiphoidal, round ligament of the liver, perinephric, etc.), gastric lavage and local hypothermia are performed. Treatment of concomitant diseases is prescribed according to indications. Abnormalities of acid-base balance and electrolyte metabolism are corrected (polarizing mixtures, panangin, 4% sodium bicarbonate solution); dysproteinemia (albumin, protein, amino acid mixtures, plasma); detoxification therapy (forced diuresis) is carried out. For infusion-transfusion therapy, it is advisable to catheterize the central vein, which allows for correction of hemostasis in a short time.
Patients with a significant degree of surgical risk. It is advisable to carry out two-stage treatment. The risk group consists of patients over 60 years of age, sub- and decompensated forms of acute and chronic vascular, pulmonary, renal or liver failure; acute or previous myocardial infarction; acute or residual effects of a previous cerebrovascular accident; bronchial asthma; pronounced changes in the lungs (emphysema, acute and chronic pneumonia, acute and chronic bronchitis, etc.); phlebothrombosis of the deep veins of the lower extremities; moderate to severe diabetes mellitus; heart disease with circulatory failure stage 2-3; atrial fibrillation; acute cholecystitis, complicated by obstructive jaundice, cholangitis; acute cholecystitis lasting more than 5 days. At the first stage, decompression of the gallbladder is performed using one of the well-known methods: percutaneously transhepatic (through the edge of the liver) under ultrasound or laparoscopy control; using laparoscopic microcholecystostomy or cholecystostomy from minilaparotomy access. Decompression of the gallbladder in combination with general treatment makes it possible to prevent the progression of the destructive process in its wall, as well as in the bile ducts, and remove patients from a state of severe intoxication within 3-5 days. In addition, transdrainage cholecystocholangiography allows one to establish the surgical anatomy of the gallbladder and bile ducts, knowledge of which is necessary to determine the scope of subsequent surgery.
During the second stage, after relief of acute inflammation in the gallbladder wall, a complete examination and comprehensive preoperative preparation, patients undergo a planned cholecystectomy. If patients refuse surgery, the stones remaining in the lumen of the gallbladder create a real danger of developing another attack of acute cholecystitis. However, patients with an extremely high degree of surgical and anesthetic risk are prescribed symptomatic conservative treatment. The operation of choice for acute calculous cholecystitis is cholecystectomy: laparoscopic or open in combination with corrective interventions on the extrahepatic bile ducts (if necessary). The surgical approach for open cholecystectomy is an upper midline laparotomy or an oblique incision in the right hypochondrium. The choice of method for removing the gallbladder depends on the experience of the surgeon, the technical equipment of the operating room, and the nature of inflammatory changes in the gallbladder and surrounding tissues.
According to generalized literature data, laparoscopic cholecystectomy in patients with acute cholecystitis can be performed in 73.8-97.2%. The following are considered contraindications to its implementation: 1) inflammatory infiltrate or abscess in the gallbladder area; 2) expansion of the common bile duct (more than 8 mm); 3) the thickness of the gallbladder wall is more than 1 cm; 4) “shrinked” gallbladder; 5) increased levels of bilirubin and amylase in the patient’s blood; 6) pulmonary heart diseases in the stage of sub- and decompensation; 7) uncorrectable disorders of the hemocoagulation system; widespread peritonitis; 9) third trimester of pregnancy; 10) biliodigestive and biliobiliary fistulas; 11) portal hypertension syndrome; 12) unclear anatomical situation in the area of the gallbladder neck and hepatoduodenal ligament. However, due to the constant progress of endoscopic surgery, contraindications to laparoscopic cholecystectomy for acute calculous cholecystitis are constantly narrowing. But keep in mind that the consistent rule of modern gallbladder surgery is immediate conversion to open cholecystectomy in case of difficulties in manipulation in the subhepatic space, rough adhesions and extensive dense infiltration in the area of the gallbladder that is not amenable to blunt preparation, and unclear anatomical situation.
The following are considered contraindications to its implementation: 1) inflammatory infiltrate or abscess in the gallbladder area; 2) expansion of the common bile duct (more than 8 mm); 3) the thickness of the gallbladder wall is more than 1 cm; 4) “shrinked” gallbladder; 5) increased levels of bilirubin and amylase in the patient’s blood; 6) pulmonary heart diseases in the stage of sub- and decompensation; 7) uncorrectable disorders of the hemocoagulation system; widespread peritonitis; 9) third trimester of pregnancy; 10) biliodigestive and biliobiliary fistulas; 11) portal hypertension syndrome; 12) unclear anatomical situation in the area of the gallbladder neck and hepatoduodenal ligament. However, due to the constant progress of endoscopic surgery, contraindications to laparoscopic cholecystectomy for acute calculous cholecystitis are constantly narrowing. But keep in mind that the consistent rule of modern gallbladder surgery is immediate conversion to open cholecystectomy in case of difficulties in manipulation in the subhepatic space, rough adhesions and extensive dense infiltration in the area of the gallbladder that is not amenable to blunt preparation, and unclear anatomical situation.
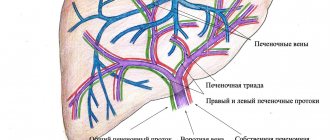
The results of cholecystectomy for acute calculous cholecystitis largely depend on the condition of the bile ducts. Therefore, all patients with this disease must undergo a comprehensive examination of the biliary tract before surgery: ultrasound, ERCG, intravenous cholecystocholangiography. In the event that it is not possible to carry out a comprehensive examination of patients in the preoperative period (emergency surgery), the condition of the biliary tract should be assessed during the operation. The most informative method for intraoperative assessment of the patency of the bile ducts during laparoscopic cholecystectomy is intraoperative cholangiography. Indications for its implementation in patients with acute calculous cholecystitis are: 1) a history of jaundice with a common bile duct diameter of up to 7-8 mm according to ultrasound; 2) dilation of the extrahepatic bile ducts more than 7-8 mm, discovered during surgery; 3) the diameter of the cystic duct is more than 2 mm; 4) small (up to 1-2 mm) stones in the gallbladder; 5) changes in the anatomy of the extrahepatic bile ducts and difficulties in preparation in the area of Calot’s triangle; 6) lack of visualization of the bile ducts due to swelling of the hepatoduodenal ligament; 7) the impossibility of using ERCG in the preoperative period if there are appropriate indications. If a pathology of the biliary tract or major duodenal papilla is established, an appropriate corrective operation is performed. Thus, in patients with stenosis of the papilla of Vater and choledocholithiasis, endoscopic pagkillosphincterotomy is performed in the postoperative period. In the case of cicatricial stricture of the common bile duct, a transition to open surgery is performed with the formation of one of the options for biliodigestive anastomosis.
Complications of chronic cholecystitis
In chronic acalculous cholecystitis, during the period of exacerbation of the disease, several syndromes can be observed, which are part of the clinical picture of the disease.
- Solar syndrome when the solar plexus is involved in the process. It usually manifests itself as pain in the abdomen: the navel area with irradiation to the back (“solar nail”) and dyspeptic manifestations.
- Premenstrual tension syndrome is a complex of physical and psychopathological symptoms that quickly disappear at the beginning of menstruation.
- Cholecystocardiac syndrome, which manifests itself as pain in the heart, palpitations, rhythm disturbances, is sometimes combined with changes in the electrocardiogram (ECG).
- Allergic syndrome - urticaria, Quincke's edema, drug and food intolerance, increased eosinophils in the blood.
Complications of chronic cholecystitis can occur during its exacerbation in the form of the development of pericholecystitis, the development of suppuration (abscess), inflammation of the bile ducts (cholangitis), biliary pancreatitis, chronic duodenitis, papallitis, liver damage, jaundice, etc.
What is the danger of pathology?
A low-grade inflammatory process affects the gallbladder. Pathology during periods of remission does not particularly annoy the patient; the person often does not realize that the digestive organs are in serious danger.
Despite rare attacks, damage to the gallbladder is quite serious:
- the outflow of bile is disrupted, the biochemical composition of the fluid changes;
- cells cope poorly with the load, food digestion occurs more slowly than expected;
- a sluggish inflammatory process causes degeneration of the walls of the gallbladder and inhibits immune mechanisms;
- improper operation of an element of the digestive system worsens the general condition of the patient.
In the absence of competent therapy or untimely seeking medical help, damage to the inflamed walls of the gallbladder is so severe that the problem organ has to be removed.
Chronic cholecystitis. Diagnostics
Diagnosis of chronic cholecystitis consists of
- clinical picture,
- laboratory data,
- instrumental data.
Clinical blood test during exacerbation of the disease - increased leukocytes (leukocytosis), accelerated ESR, increased C-reactive protein, increased blood bilirubin, cholesterol, alkaline phosphatase, gamma glutamate transpeptidase, liver tests and pancreatic tests to exclude concomitant lesions of the liver and pancreas.
Of the instrumental examination methods, the X-ray method - cholecystography - is rarely used. Duodenal intubation is currently rarely performed.
The main method is ultrasound. Chronic cholecystitis is accompanied by gallbladder dyskinesia (impaired motility) of the hypokinetic or hyperkinetic type, or without dyskinesia; sometimes a “disabled” gallbladder is observed. Ultrasound examination reveals signs of chronic acalculous cholecystitis:
- changes in the shape of the gallbladder (congenital or acquired),
- compaction or thickening of its wall (more than 4 mm),
- increase in the size of the gallbladder,
- signs of inflammation - the presence of a shadow from the walls of the gallbladder, doubling of the contour,
- contractile dysfunction,
- inhomogeneity of bile,
- infiltration of peri-vesical tissue along its contour or inside the contour,
- presence of sludge or stones.
Endoscopic examination - gastrodeudenoscopy with examination of the sphincter of Oddi.
Hepatobiliscintigraphy (radionuclide method), laparoscopy, endoscopic retrograde cholangiopancreatography are special methods for diagnosing the gallbladder, which are usually performed in a hospital setting.
general description
Cholecystitis is an inflammatory disease of the gallbladder, a consequence of complications of gallstone disease.
Inflammation occurs due to a violation of the outflow of bile from the gallbladder and the presence of pathogenic microflora in the wall of the bladder. Cholecystitis often affects people over 50 years of age, but it also occurs at an earlier age. In the scientific literature, cases of an attack of biliary colic in children 11-15 years old have been recorded. Elderly people aged 60-75 years and senile people account for 35-55% of the total number of cases of cholecystitis.
Cholecystitis can be: acute (according to the morphological picture it is divided into: catarrhal, phlegmonous and gangrenous) and chronic.
Treatment of chronic acalculous cholecystitis
Treatment is often carried out on an outpatient basis and is comprehensive and individual.
Medical nutrition
The basic principles of therapeutic nutrition are: frequent split meals (5-6 times a day) at regular intervals, which trains the gallbladder, causing it to contract after each meal, and complete meals with sufficient content and the correct ratio of proteins, fats and carbohydrates, vitamins and mineral salts food.
Dietary fiber (wheat bran) is important, increasing the synthesis of bile acids in the liver, eliminating constipation, consuming vegetables and fruits rich in plant fiber.
Among animal fats, preference is given to butter, combining it with vegetable oils, which are added to ready-made dishes (porridge, salads, mashed potatoes) and to a lesser extent the use of fats when frying.
In case of exacerbation of chronic acalculous cholecystitis, it is recommended to limit salt, reduce the total calorie content of the diet, and carry out “fasting days” - rice-kefir, watermelon, etc.
The diet of patients with chronic acalculous cholecystitis should be significantly limited:
- strong meat broths and rich fish soup containing a large amount of extractive substances,
- animal fats (except butter),
- egg yolk,
- fried foods,
- beer and alcoholic drinks,
- spicy seasonings for dishes,
- carbonated and cold drinks.
Causes and risk factors
Factors that predispose to the appearance of a chronic form of cholecystitis include the following:
- bile stagnation;
- prolapse of internal organs;
- pregnancy;
- disruption of the blood supply to the organ;
- entry into the bile ducts of pancreatic juice;
- being overweight;
- excessive fatigue;
- the presence of intestinal infections in the body;
- chronic form of pancreatitis;
- insufficiently active lifestyle;
- excessive consumption of alcoholic beverages;
- eating disorders;
- foci of infection in the body;
- eating a lot of spicy and fatty foods;
- hypoacid gastritis;
- hypothermia;
- Stressful situations, endocrine disorders, autonomic disorders can lead to problems with the tone of the gallbladder.
The causative agents of cholecystitis, as a rule, are pathogenic microorganisms - staphylococci, streptococci, helminths, fungi. They can enter the gallbladder from the intestines, as well as through the blood or lymph.
Prevention of exacerbations
To prevent the occurrence of the disease or avoid its exacerbation, general hygiene rules should be followed. Nutrition plays an important role. You need to eat food 3-4 times a day at approximately the same time. Dinner should be light and you should not overeat. Excessive consumption of fatty foods in combination with alcohol should be especially avoided. It is important that the body receives a sufficient amount of fluid (at least 1.5-2 liters per day).
In order to prevent chronic cholecystitis, it is necessary to allocate time for physical activity. This could be exercise, walking, swimming, cycling. In the presence of chronic foci of infection (inflammation of the appendages in women, chronic enteritis, colitis, tonsillitis), they should be treated in a timely manner, the same applies to helminthiasis.
If you follow the above measures, you can prevent not only inflammation of the gallbladder, but also many other diseases.
Classification
The disease is characterized by a chronic course and a tendency to alternate exacerbations and remissions. Taking into account their number throughout the year, experts determine the nature of the disease: mild, moderate or severe.
There are 2 main types of chronic cholecystitis:
- non-calculous (stone-free) – (inflammation of the walls of the gallbladder without the formation of stones);
- calculous (with the formation of hard concretions - stones).
Depending on the course of the disease, there are 3 forms of the disease - sluggish, recurrent and purulent.