General information
Due to the high pace of life, working with equipment, driving vehicles, constant migration and active travel of people, the risk of injuries, including severe ones, increases.
In case of severe injuries and polytrauma, victims develop a traumatic disease - this is a set of changes and reactions that occur in the body from the moment of injury until its outcome. Traumatic illness occurs in several periods. The first of these is traumatic shock (ICD-10 code T79.4). This is a severe, critical condition, characterized by severe disturbances in vital functions, especially blood circulation - a critical decrease in blood flow in the tissues develops. Pulmonary and tissue gas exchange and metabolism in tissues are also disrupted, and endotoxicosis (poisoning of the body with tissue decay products) increases.
Hemodynamic disturbances arise due to hypovolemia (decreased circulating blood volume) that develops against the background of blood loss. In patients with severe shock, the volume of the liquid part of the blood also decreases due to its transfer into tissues (interstitial edema). As a result, the blood thickens sharply, the pressure decreases, and under these conditions the function of the heart as a pump decreases almost twice (small output syndrome). Thus, in shock, hypocirculation syndrome with impaired tissue perfusion in response to mechanical damage comes first. A type of traumatic shock is burn shock . They have much in common in pathogenesis and basic approaches to treatment.
The period of acute shock is followed by a period of multiple organ failure lasting 3-7 days. This is followed by a period of infectious complications (up to 1 month) and a period of delayed convalescence. Thus, disturbances in important body functions caused by injury are long-lasting. If in case of shock all measures are aimed at saving life (eliminating the causes of shock, correcting blood circulation and breathing), then in the future the traumatic disease requires long-term treatment until the outcome.
The processes occurring in later periods are associated with the initial hours of the disease. The relevance of the problem is that the state of shock not only poses a threat to life if assistance is provided incorrectly and untimely, but also has adverse consequences regarding the physical and mental health of a person.
Publications in the media
Traumatic shock is shock that occurs in response to severe injury.
Pathogenesis . The main pathogenetic factors in traumatic shock: pain, toxemia, bleeding and subsequent cooling • With prolonged compartment syndrome and extensive soft tissue damage, one of the causes of shock is early toxicosis. Failure of kidney function occurs as a result of toxic damage to the renal epithelium and blockage of convoluted tubules by hyaline and pigment casts containing myoglobin. In some cases, oliguria and anuria, even with a satisfactory level of blood pressure, make it possible to judge the severity of shock • In burn shock, in addition to pain and toxemia, an important pathogenetic factor is plasma loss from the burn surface, which determines protein and potassium deficiency.
Clinical picture . Traumatic shock has a phase course (it was first described by N.I. Pirogov) • The erectile phase lasts several minutes (with burn shock - up to 2 hours) and is characterized by agitation of the patient, tachycardia. In the absence of blood loss, hemodynamics remain satisfactory (normotension or even hypertension). The skin is pale, there is no cyanosis • The torpid phase is characterized by lethargy, physical inactivity, bradycardia, oliguria, and shortness of breath. The skin is pale, with an earthy tint (cyanosis is added). Cold sticky sweat appears.
Treatment . In the treatment of traumatic shock, the same methods are used as for hemorrhagic shock (see Hemorrhagic shock). The following steps are performed in the prehospital phase: at the scene or in the ambulance.
• Restoration of airway patency: elimination of tongue retraction, toilet of the oropharynx, mouth-to-mouth artificial respiration, if necessary, tracheal intubation.
• Restoration of hemodynamics: closed cardiac massage, emergency hemostasis (finger pressure of the vessel, tight bandage, tourniquet), jet intravenous infusion of polyglucin, 0.9% sodium chloride solution, sodium bicarbonate, strophanthin K 0.5–1 ml 0.05% solution in 20 ml of 0.9% sodium chloride solution IV slowly.
• Administration of painkillers (analgesics in combination with antihistamines, inhalation of nitrous oxide with oxygen).
• Aseptic dressing for open injuries.
• Immobilization of fractures.
• Rational positioning on a stretcher •• If the chest is damaged - semi-sitting position •• If there is a head injury - Fowler's position •• If the abdomen is injured - horizontal •• If the pelvis is damaged - the frog position.
ICD-10 • T79 . 4 Traumatic shock
Pathogenesis
The pathogenesis of traumatic shock can be represented as follows: a deficiency of circulating blood and plasma due to blood loss and the release of the liquid part of the blood into the tissue, which leads to a decrease in venous return and a decrease in the stroke volume of the heart with the development of changes in vital organs and disruption of their function.
The trigger for any shock is the discrepancy between the volume of circulating blood and the volume of the vascular bed. As a result, the pressure decreases, to which the baroreceptors of the vascular wall react. Impulses from them enter the brain and the sympathoadrenal system is activated: adrenaline and norepinephrine and accumulate in them. Catecholamines , affecting the heart and blood vessels, cause increased frequency and intensification of heart contractions, vascular spasm (skin, kidneys, gastrointestinal tract). Centralization of blood circulation occurs. Catecholamines do not affect the blood vessels of the brain. This mechanism maintains pressure at a sufficient level until the supply of catecholamines is exhausted. These phenomena correspond to the erectile phase of shock.
When catecholamine reserves are depleted, the second phase of shock (torpid) develops. All spasmodic vessels lose their tone (dilate) and the cardiac output decreases. By this time, non-oxidized products have accumulated in the damaged tissues, which enter the bloodstream, which worsens the situation. , multiple organ failure quickly develops .
Causes and mechanisms of development
What is important for the development of traumatic shock is not so much the absolute amount of blood loss as the rate of blood loss. With rapid blood loss, the body has less time to adjust and adjust, and shock is more likely to develop. Therefore, shock is more likely when large arteries, such as the femoral artery, are injured.
Severe pain, as well as neuropsychic stress associated with injury, undoubtedly play a role in the development of the shock state (although they are not its main cause) and aggravate the severity of shock.
Factors leading to the development of traumatic shock or aggravating it are also injuries with damage to particularly sensitive areas (perineum, neck) and vital organs (for example, a wound to the chest, rib fractures with impaired external respiration function, traumatic brain injury). In such cases, the severity of shock is determined by the amount of blood loss, the intensity of the pain syndrome, the nature of the injury and the degree of preservation of the function of vital organs.
On this topic ▼
Shock
Types, phases, degrees and treatment
Rapid and massive blood or plasma loss leads to a sharp decrease in the volume of circulating blood in the victim’s body. As a result, the victim’s blood pressure quickly and severely drops, the supply of tissue with oxygen and nutrients deteriorates, and tissue hypoxia develops. Due to the lack of oxygen in the tissues, toxic under-oxidized metabolic products accumulate in them, metabolic acidosis develops, and intoxication increases. Lack of glucose and other nutrients in tissues leads to their transition to “self-sufficiency” - lipolysis (fat breakdown) and protein catabolism increase.
The body, trying to cope with blood loss and stabilize blood pressure, reacts by releasing various vasoconstrictor substances into the blood (in particular, adrenaline, norepinephrine, dopamine, cortisol) and spasm of peripheral vessels. This may temporarily stabilize blood pressure at a relatively “acceptable” level, but at the same time further worsens the situation with the supply of oxygen and nutrients to peripheral tissues. Accordingly, metabolic acidosis, intoxication with under-oxidized metabolic products, and catabolic processes in tissues intensify even more. Centralization of blood circulation occurs - the brain, heart, and lungs are primarily supplied with blood, while the skin, muscles, and abdominal organs do not receive enough blood. Lack of blood supply to the kidneys leads to a decrease in glomerular filtration of urine and a deterioration in the excretory function of the kidneys, up to complete anuria (lack of urine).
Spasm of peripheral vessels and increased blood clotting as a reaction to bleeding contribute to the blockage of small spasmodic vessels (primarily capillaries) with tiny blood clots - blood clots. The so-called “DIC syndrome” develops – disseminated intravascular coagulation syndrome. Blockage of small vessels further increases problems with blood supply to peripheral tissues and, in particular, the kidneys. This leads to a further increase in metabolic acidosis and intoxication. The so-called “consumption coagulopathy” may develop - a blood clotting disorder due to the massive consumption of clotting agents in the process of widespread intravascular coagulation. In this case, pathological bleeding may develop or bleeding from the injury site may resume, and further worsening of shock may occur.
On this topic ▼
Providing first aid depending on the situation
A decrease in blood supply to the adrenal glands and their function against the background of an increased need for glucocorticoids in “shock” tissues leads to a paradoxical situation. Despite the high level of cortisol in the blood (spike!), there is relative adrenal insufficiency. This is explained by the fact that less is “thrown away” than the tissues need, and the poorly supplied adrenal glands are physically unable to produce more cortisol.
The body's attempts to cope with pain by increasing the secretion of endorphins (endogenous analogues of opiates) lead to a further drop in blood pressure, the development of lethargy, lethargy, and anergy. The reaction to a decrease in blood pressure and a high level of catecholamines in the blood is tachycardia (rapid heartbeat). At the same time, due to insufficient circulating blood volume, cardiac output (stroke volume of the heart) is simultaneously reduced and there is weak filling of the pulse (up to a thread-like or undetectable pulse in the peripheral arteries).
Severe shock without treatment usually results in agony and death. In the case of a relatively mild or moderate shock, self-healing is in principle possible (at some stage, further development of the shock may stop, and then the condition will stabilize, the body will adapt and recovery will begin). But this cannot be relied upon, since the development of a shock state of any degree in itself indicates a failure of adaptation, that the severity of the injury has exceeded the compensatory capabilities of this particular organism.
Classification
According to the etiology (reason), traumatic shock occurs:
- As a result of mechanical injuries (fractures, severe injuries, tissue compression).
- As a result of burns.
- From exposure to low temperatures.
- As a result of exposure to electricity.
By time of occurrence:
- Primary - develops immediately after injury (1-2 hours) and is the result of injury.
- Secondary - appears after 5-24 hours as a result of additional trauma.
If we consider the clinical stages of traumatic shock, then two phases are distinguished:
- Erectile phase. In case of injury, impulses entering the central nervous system cause short-term excitation.
- Torpid phase. Short-term excitation is replaced by inhibition and true shock develops with inhibition of all functions. Hemodynamic disturbances prevail - a drop in arterial and venous pressure, a decrease in cardiac output, impaired gas exchange in tissues and metabolic disorders. As a result of circulatory and respiratory hypoxia , all organs suffer.
True shock is classified according to the severity of its manifestations. The following degrees of traumatic shock are distinguished:
- First degree (this is compensated shock). The victim is a little lethargic, the skin is pale, the extremities may be cold, breathing and cardiac activity are increased. Tachycardia up to 100 beats. Systolic pressure 100-90 mmHg. Art.
- Second degree (or subcompensated shock). The victim is slow and does not move. There is pallor and coldness of the skin, as well as a marbled pattern of the skin. Heart rate increases to 110-120, and pressure decreases to 80-75 mm Hg. Art. There is also a decrease in diuresis. The first two degrees have a favorable outcome, since protective-adaptive reactions and assistance prevent the development of hypoxia and deepening of shock.
- Third degree (decompensation). As a result of prolonged spasm of small vessels, hypoxia and cell damage occurs when assistance is delayed. The patient is lethargic, does not respond to external stimuli, and has an earthy-colored skin. Heart rate increases even more (130-140 beats), pressure progressively decreases (60 mm Hg and below), and diastolic pressure is often not determined. The patient develops anuria . This condition is typical for prolonged (hours) traumatic shock. However, properly performed resuscitation measures are often effective and the patient is brought out of shock. However, after removing patients from this state, 70% develop severe complications, the treatment of which is more complex than recovery from shock.
- Fourth degree (terminal, irreversible). Changes in the body reach the point where all measures taken are unsuccessful. Destructive processes in the body continue, deep decompensation of homeostasis and the victim dies.
Burn shock is one of the types of traumatic shock that develops with deep burns occupying more than 15% of the body. It is the first stage of burn disease. Its severity is influenced by the total area of the burn and its depth. The pathogenesis of burn shock is associated with pain from the burn area, which causes overexcitation of the central nervous system, and then hemodynamic and microcirculatory disorders occur. Generalized spasm of the arteries in the periphery in the next 1-2 hours maintains the pressure and functions of the life support organs, but after this the volume of circulating blood decreases due to loss of plasma, which increases over the course of two days. Victims experience increased blood coagulation and thrombosis . Oliguria appears associated with arterial spasm.
Large loss of plasma, blood thickening and the formation of toxic substances in the necrosis zone after a burn leads to disturbances in the acid-base state and electrolyte balance. A peculiar clinical picture is noted: at first the patient is agitated, talkative, fidgety, and inadequately assesses the condition. After this, excitement gives way to inhibition, as the patient develops hypovolemia - its degree depends on the severity of the burn. There are also 4 degrees of severity, which depend on the area of the burns.
- A mild degree develops with superficial or deep burns, the area of which is up to 10% of the surface. Consciousness is preserved, pale skin, muscle tremors, nausea, and sometimes vomiting. Moderate tachycardia , blood pressure within normal limits. The victims can be brought out of shock by the end of the day.
- Moderate severity of shock occurs with superficial burns, occupying 20-40% of the surface. This stage is characterized by excitement turning into inhibition. The patient's consciousness remains intact, the skin is pale and cold. The victim is worried about thirst and nausea, breathing is rapid, blood pressure is reduced, oliguria and kidney function is impaired (residual nitrogen increases, blood and protein appear in the urine). The victims can be brought out of this state within two days.
- Severe degree accompanies superficial burns of 40-60% of the surface. The patient's condition is extremely serious, confusion and lethargy are noted. Patients are pale gray in color and have severe thirst, vomiting, seizures , tachycardia and shortness of breath . Oliguria is noted , and in older patients anuria . The level of residual nitrogen increases to 51-56 mmol/l. Treatment is not always effective.
- An extremely severe degree is observed with burns affecting 60% of the surface. The condition is very serious, there is no consciousness. The victim's temperature is reduced, there is severe shortness of breath, and the pulse is thready. The vomiting of “coffee grounds” is disturbing, intestinal paresis progresses, and metabolic acidosis intensifies. Patients have anuria, blood and protein are detected in the urine, residual blood nitrogen is above 60 mmol/l. Victims in this condition die within the first or second day.
In clinical practice, we encounter not only post-traumatic shock associated with various injuries, but also shock that develops against the background of various diseases, for example, the cardiovascular system. Thus, arrhythmic shock (another name is “cardiogenic”) occurs in 4-5% of patients with large-focal transmural myocardial infarction . Its development is associated with a decrease in cardiac output due to disturbances in heart rate. It occurs in the form of tachysystole (rapid contractions of the heart) or bradysystole (excessive slowdown of contractions).
Tachysystolic shock develops in patients with atrial fibrillation. In this condition, diastole is shortened, therefore the filling of the heart decreases and its minute volume decreases. However, the leading role in the development of shock is given to ventricular tachysystole, in which it develops in the first hours of the disease. The condition of the patients is serious, since the pressure decreases significantly and diuresis decreases. Patients are given adequate pain relief (narcotic analgesics) and antiarrhythmic drugs are administered.
With intractable tachysystole, pulmonary congestion and right ventricular failure develop. The prognosis for tachysystolic shock is unfavorable. Mortality is 40% and its main cause is progressive heart failure. Bradysystolic shock develops with atrioventricular block , junctional rhythm and Frederick's syndrome . The course is severe, and the mortality rate reaches 60%.
Among the complications of acute pancreatitis is pancreatogenic shock , which occurs in 20% of patients. It most often develops with necrotizing pancreatitis and is characterized by unstable hemodynamics. The cause of the development of this type of shock is endotoxemia due to necrotic damage to large volumes of pancreatic tissue. The volume of pancreatic necrosis determines the likelihood of endotoxic shock. The timing of its appearance is different, and therefore there are early (appears in the first week of the disease) and late (develops in the third week) shock.
The main cause of shock of this nature is a decrease in the volume of circulating blood. This can occur due to swelling of the gland tissue, saturation of the retroperitoneal space with fluid, accumulation of hemorrhagic fluid in the abdominal cavity and intestinal loops, as well as due to stagnation of blood in the portal system of the liver. This loss of extracellular fluid leads to hypovolemia and shock.
In early shock, the patient experiences tachycardia (or bradycardia), signs of peritonitis , decreased blood pressure, cold extremities and facial cyanosis . Late shock occurs against the background of generalized sepsis (fever, leukocytosis ), which is accompanied by hemodynamic instability, which, in fact, is shock.
Kinds
Shock can be primary (early) , which occurs immediately after injury and is an immediate reaction to injury. Secondary (late) shock occurs 4-24 hours after the injury and even later, often as a result of additional traumatization of the victim (during transportation, cooling, renewed bleeding, tightening a limb with a tourniquet, from rough manipulations during the provision of medical care, etc.). A common type of secondary shock is postoperative shock in the wounded. Under the influence of additional trauma, relapses of shock in victims are also possible, usually within 24-36 hours. Shock often develops after the tourniquet is removed from the limb.
Symptoms
Symptoms of pain shock differ in the erectile and torpid phases. The first is very short, it occurs immediately after the injury, does not happen to all victims and is characterized by excitation of the sympathoadrenal system . The patient retains consciousness, there is arousal (motor and speech), rapid breathing, satisfactory pulse filling, not accelerated, blood pressure is normal or increased. The victim's behavior resembles a state of alcohol intoxication.
In the torpid phase, signs of traumatic shock include lethargy, mental depression, an indifferent attitude towards everything, and lack of response to pain come to the fore. The temperature is low, the skin is cold, clammy sweat, breathing is rapid, pulse is increased, blood pressure is reduced, urination is impaired, the severity of which depends on the stages of shock.
- In the first degree (considered as a mild degree), the general condition is satisfactory, the patient is conscious, there may be slight lethargy, pulse up to 100 beats, pressure 95-100 mm Hg. Art. The prognosis is favorable. If help is not provided or additional trauma occurs, shock of this degree may progress to the second degree.
- In the second degree, severe lethargy is noted, pressure (90-75 mm Hg) and temperature decrease, pulse 110-120 beats, breathing becomes rapid. Pale skin with a bluish tint. The prognosis for this degree is serious. Recovery from shock is possible, but requires long-term (possibly several days) anti-shock therapy.
- Stage 3 pain shock is severe. In the general serious condition of the victim, a sharp lethargy appears, a decrease in pressure of 70 mm Hg. Art. (below a critical level), increased heart rate, which has very weak filling and tension. Decreased diuresis and anuria. If the causes are not eliminated in a timely manner and assistance is not provided, it enters a terminal state.
- Shock of the 4th degree is a preagonal state. The patient's pressure and pulse are not determined in the radial arteries, but a weak pulsation is still detected in the large arteries, heart sounds are barely audible, and rare shallow breathing is noted. Reflexes are not evoked, anuria. In the agonal state, respiratory disturbances ( Chine-Stokes breathing ) are more pronounced. Clinical death is considered from the moment of cardiac arrest and the last breath. The functions of the central nervous system are completely absent, but metabolic processes in the brain continue for another 5-6 minutes.
Trauma of any location is accompanied by blood loss. There is a relationship between it and the severity of the shock. In the first degree, blood loss is 500 ml, in the second 1,000 ml, and in the third - 1,500 ml or more.
Patients who have suffered severe trauma and stress develop post-traumatic syndrome, which is characterized by changes in the psycho-emotional sphere. The patient develops unmotivated vigilance, he monitors what is happening around him and does not leave him with a feeling of threatening danger. Patients have an explosive reaction when they throw themselves to the ground at unexpected loud noises. It becomes difficult for such patients to establish contacts with others and they experience dullness of emotions. From time to time, aggressiveness and the desire to solve all problems with the help of force arise, getting one’s way.
The most important symptom is uninvited memories. They are the ones who give the right to say that the patient has post-traumatic syndrome . Scenes associated with a trauma, disaster, fire or other event emerge in his memory. Memories arise during sleep, and when awake they appear in cases where the situation is somewhat reminiscent of what happened (this could be a smell, sound or sight). The patient is worried about anxiety, constant worry, a feeling of fear, fear of persecution, constant preoccupation. An important factor in this condition is depression , when a person feels that everything is useless, there is a negative attitude towards life and apathy. It is also possible to develop a tendency to abuse alcohol and drugs. In some patients, post-traumatic syndrome is very pronounced and requires psychiatric correction.
Coma state
6
THE CONCEPT OF THE FINAL (TORPID) STAGE OF SHOCK
REMEMBER! If the victim does not receive medical assistance within 30-40 minutes, then prolonged CENTRALIZATION OF BLOOD CIRCULATION will lead to gross disturbances of microcirculation in the kidneys, skin, intestines and other organs excluded from the blood circulation.
Thus, what played a protective role at the initial stage and gave a chance for salvation will become the cause of death in an hour.
REMEMBER! The time factor in the development and outcome of shock is of decisive importance.
A sharp decrease in the speed of blood flow in the capillaries, up to a complete stop, will cause disruption of oxygen transport and accumulation of under-oxidized metabolic products in the tissues - ACIDOSIS and lack of oxygen - HYPOXIA.
It is from this moment that the precapillaries completely relax and the PS sharply decreases. The rational system of blood distribution at the initial stage of shock development instantly collapses.
An acute and practically irreparable deficit of bcc occurs: filling the entire capillary network of the body, capable of holding up to 100 liters of blood, will not allow, first of all, the anatomy of organs and tissues.
This stage will very quickly give way to agony, when the victim loses consciousness, stridor breathing appears, the pulse in the radial arteries and blood pressure are determined with great difficulty. Then there is only death.
REMEMBER! If the victim is not taken to the intensive care unit within one hour, there will be practically no chance of salvation.
7
SIGNS OF TORPIDS STAGE OF SHOCK
Motor and emotional excitement of the first phase of shock is replaced by apathy and indifference within 30-40 minutes. The blood pressure level drops to 30-60 mmHg. Art.
The skin takes on an earthy tint with characteristic crimson and grayish-greenish stains. Their bizarre pattern is so reminiscent of marble that even the term SKIN MARBLEMENT arose. This pattern is most pronounced on the skin of the abdomen and the front of the thighs.
Since the time of the great medical scientist Pirogov, military surgeons began to distinguish this stage as TORPIDS (Latin torpidum - inhibition), which ends in death and is considered irreversible.
Loss of fluid through profuse sweat and redistribution of plasma from the bloodstream into the intercellular spaces of tissues causes significant thickening of the blood.
Red blood cells begin to line up in the capillaries in the form of coin columns, completely filling their lumen, and stick together with countless thin, mud-like filaments of FIBRIN.
The process of THROMBUS FORMATION begins. The staff of the ambulance and intensive care units know very well how, already in the first minutes of shock, the needle instantly thromboses when attempting an intravenous injection, which indicates a sharp increase in blood clotting.
Massive thrombosis in the capillaries leads to the formation of zones of NECROSIS (Greek nekros - necrosis) in organs such as the kidneys, liver and intestines.
REMEMBER! The torpid stage is that stage of shock when the chances of salvation disappear with every minute. It is easier to prevent its development by promptly starting to provide first aid than to save it from complications incompatible with life.
SIGNS OF THE FINAL STAGE OF SHOCK:
|
8
WHAT ARE SHOCK ORGANS
REMEMBER! The organs that suffer most during shock are called SHOCK ORGANS.
REMEMBER! The main reason for their death is that they were excluded from a full blood supply for too long during the centralization of blood circulation.
REMEMBER! The death of shock organs is complications of shock incompatible with life.
SHOCK LUNG The discharge of venous blood into the arterial bed, bypassing the alveolar network, without proper oxygen saturation, leads to the withdrawal of a huge number of alveoli - “pulmonary vesicles” - from gas exchange. A state of acute respiratory failure develops: shortness of breath, blue lips and fingertips appear.
SHOCK KIDNEY Long-term exclusion of the capillary network of the kidneys from the blood circulation leads to acute renal failure and the accumulation of toxic substances in the blood, to a decrease in urine output, up to the development of ANURIA (complete cessation of urine output).
SHOCK LIVER Damage to bloodless liver tissue results in a gross violation of its protective functions, which will certainly cause acute liver failure and rapid accumulation of extremely toxic metabolic products in the blood.
REMEMBER! The death of shock organs inevitably leads to death.
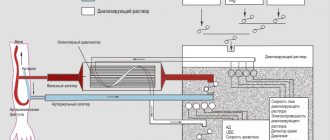
| Rescue of victims is possible only in the intensive care unit, where there are “artificial kidney” and lung ventilation devices, monitors for continuous monitoring of body functions and highly qualified medical personnel. |
| to transport victims with SEVERE INJURIES TO THE BEST intensive care units, you can always seek help from the Federal Medical and Biological Agency of Russia +7 (499) 190-33-25 |
| The main task in providing first aid by eyewitnesses is to reduce the suffering of the victim and prevent the development of the torpid stage of shock. |
9
RULES FOR PAIN RELIEF OF A VICTIM BY MEDICAL PROFESSIONALS
REMEMBER! Thorough pain relief is the most effective component in preventing the development of the final torpid stage of shock.
REMEMBER! The most effective painkillers are narcotic analgesics: PROMEDOL, MORPHINE, OMNOPON, FENTANYL.
REMEMBER! In all cases where medical personnel did not use narcotic analgesics to relieve the suffering of victims with open bone fractures or traumatic amputation of limbs, their actions should be subject to an official investigation.
REMEMBER! All potent painkillers (narcotic analgesics) cause depression of the respiratory center.
For this reason, they are practically not prescribed to children under 5 years of age and are used with great caution for pain relief in adults.
REMEMBER! Another side effect of narcotic analgesics is nausea and repeated vomiting.
Undoubtedly, only a medical professional has the right to use drugs. However, it is still useful for our reader to know in what situations they cannot be used in order not to cause harm, and most importantly, to eliminate undeserved reproaches against ambulance crews for callousness or indifference to the suffering of victims.
UNACCEPTABLE! Treat pain with narcotic analgesics:
- Children under 5 years old,
- Victims in a coma
- Victims whose burn area exceeds 60-70% of the body surface,
- In case of complaints of abdominal pain.
Remember! Injecting a narcotic into a victim in a coma will cause him to stop breathing and gag reflex at the same time.
REMEMBER! Victims with a large area of burnt skin surface quickly lose consciousness and fall into a coma due to dehydration and severe intoxication emanating from damaged tissues (“toxic shock”).
IT IS FORBIDDEN! Accuse medical personnel of callousness or indifference to suffering when they do not provide pain relief to young children screaming from unbearable pain, victims with extensive burns or complaints of abdominal pain.
10
How to help the ambulance crew in cases of using narcotic analgesics in a situation with a large number of victims.
Remember! All narcotic analgesics cause a very unusual phenomenon - controlled cessation of breathing.
The victim, being conscious, literally forgets to breathe. First his lips turn blue, then his nose. And then he loses consciousness and dies from respiratory arrest.
The only thing that can save him is your dialogue with him. But not in the version when, after your 10-minute inspired story about a trip to a neighboring village, he fell silent forever.
You must ask him any questions, even the most stupid ones, so that he is forced to answer them with at least one word, at least in a whisper.
Remember! Every phrase or even one word said by the victim (in response to your question) is his exhalation. And inhalation happens by itself.
15-20 minutes of such communication is enough for the depression of the respiratory center to cease to threaten his life.
REMEMBER! In cases with a large number of victims, one ambulance team has the ability to numb up to 10 victims with strong painkillers.
Very often, a team consisting of only one medical worker (doctor or paramedic) arrives at the scene of an incident, who, before the arrival of other teams, has to provide assistance to several victims for an hour or even more.
Remember! If a medical professional asks you to monitor the victim's breathing after administering drugs, then it is quite enough to just ask him questions out loud.
What to do? If a victim who has been given a strong anesthetic suddenly becomes silent? Immediately check the carotid pulse. If there is a pulse, it makes sense to try to wake it up.
What to do? What if a victim who has been given a strong painkiller suddenly loses consciousness and has no pulse in the carotid artery? Immediately deliver a blow to the sternum, and if it is ineffective, begin resuscitation.
What to do? If the victim, after the administration of an anesthetic, lost consciousness, does he have a pulse in the carotid artery, but it was impossible to wake him up? Immediately call a doctor who is treating another victim nearby.
| In any case of loss of consciousness after the administration of an anesthetic, you should immediately call a medical worker PROVIDING ASSISTANCE NEAR ANOTHER VICTIM. |
Tests and diagnostics
In the diagnosis of shock, examination, physical examination and instrumental examination methods are of primary importance. The patient is continuously monitored for vital signs to monitor the severity of shock and the effectiveness of treatment.
- Physical examination gives a general idea of the severity of the condition.
- The general condition ranges from moderate to very severe. Impaired consciousness from confusion to coma.
- Characteristic appearance: pale face, cold sticky sweat, cyanosis of the extremities, decreased temperature.
- Frequent weak pulse, low blood pressure, rapid and shallow breathing.
- Damage to internal organs.
- Fractures, crushed tissue.
At the hospital level, examinations, depending on conditions and indications, include:
- General radiography (extremities, skull, pelvis, chest, abdominal cavity).
- Ultrasound of the abdominal and pleural cavity.
- Carrying out laparoscopy .
- Measurement of central venous pressure.
- Conducting thoracoscopy and bronchoscopy .
- Computed tomography.
- MRI.
Phases
Regardless of the causes of shock, it goes through two phases - erectile (excitement) and torpid (inhibition).
Erectile
This phase occurs at the moment of traumatic impact on a person with a sudden sharp excitation of the nervous system, manifested in excitement, anxiety, and fear. The victim remains conscious, but underestimates the complexity of his situation. He can answer questions adequately, but has impaired orientation in space and time.
The phase is characterized by pale human skin, rapid breathing, and severe tachycardia. Mobilization stress in this phase varies in duration; shock can last from several minutes to hours. Moreover, with severe trauma, it sometimes does not manifest itself in any way. And too short an erectile phase often precedes a more severe course of shock in the future.
Torpidnaya
Accompanied by a certain inhibition due to inhibition of the activity of the main organs (nervous system, heart, kidneys, lungs, liver). Circulatory failure increases. The victim becomes pale. His skin has a gray tint, sometimes a marble pattern, indicating poor blood supply, stagnation in the blood vessels, and he breaks out in cold sweat. The limbs in the torpid phase become cold, and breathing becomes rapid and shallow.
The torpid phase is characterized by 4 degrees, which indicate the severity of the condition.
- First degree.
Considered easy. In this condition, the victim has a clear consciousness, pale skin, shortness of breath, slight lethargy, the pulse reaches 100 beats/min, the pressure in the arteries is 90-100 mm Hg. Art.
- Second degree.
This is a moderate shock. It is characterized by a decrease in pressure to 80 mm Hg. Art., pulse reaches 140 beats/min. The person has severe lethargy, lethargy, and shallow breathing.
- Third degree.
An extremely serious condition of a person in shock, who is in a confused state of consciousness or has completely lost it. The skin becomes earthy gray in color, and the fingertips, nose and lips become bluish. The pulse becomes thread-like and increases to 160 beats/min. The man is covered in sticky sweat.
- Fourth degree.
The victim is in agony. Shock of this degree is characterized by a complete absence of pulse and consciousness. The pulse is barely palpable or completely imperceptible. The skin is gray in color, and the lips become bluish and do not respond to pain. The prognosis is most often unfavorable. The pressure becomes less than 50 mm Hg. Art.
Diet
The patient’s nutrition depends on his condition and the presence or absence of injuries to the abdominal organs for which surgery was performed. If the victims are in serious condition after burns or in a comatose state due to polytrauma, they are provided with parenteral nutrition, which is included in the complex of treatment measures. Before it is carried out, the victim’s condition must be stabilized and hypoxia eliminated. Therefore, in terminal conditions and shock, only glucose solutions with insulin . After the glucose infusion, an amino acid preparation or protein hydrolysate . Amino acid mixtures: Polyamine , Panamin , Levamin-80 , Levamin-normo , Alvezin , Aminoplasmal , Aminofusin , Moriamin , Trofisan , Okhamin , Friamin . Protein hydrolysates: Casein hydrolysate , Aminofusin , Aminonorm , Aminoplasmal , Aminomel , Aminovenoz , Aminon , Amigen , Izovac .
Then amino acid mixtures or protein hydrolyzate are administered with vitamins, electrolytes and glucose. Fat emulsions are poured together with amino acid mixtures and hydrolysates. They should not be administered with electrolytes, since electrolytes enlarge fat particles, which significantly increases the risk of fat embolism. Fat emulsions include Lipofundin 10% , Intralipid , Lipomul 15% , Lipofundin 15% , Lipifizan 15% . Preparations based on soybean oil are also produced: Lipofundin-S 20% , Emulsan , Venolipid , Infusolipol . The main components of parenteral nutrition are distributed as follows: proteins make up 10-15% of the total daily caloric intake, carbohydrates - 50%, and fats - 35-40%. Vitamins are also an integral component of parenteral nutrition, they are administered separately, and there are also multivitamin complexes for parenteral administration - these are Vitafuzin , Protavit , Soluvit , which contain the daily requirement of essential vitamins.
As the patient's condition improves, the patient is transferred to enteral nutrition with formulas. This is especially indicated if there were abdominal injuries with damage to the gastrointestinal tract or if operations were performed on these organs. Semi-element mixtures are fully balanced with nutrients; proteins are represented by peptides and protein hydrolysates. The most commonly used are Peptamen and Nutrien Elemental - these are specialized medical nutrition products that can be used as the only source of nutrition. Available in powder form, which is diluted with warm boiled water and taken orally.
When switching to a normal diet, the patient must gradually expand the food load, starting with Dietary Table No. 1 with the transition to the standard Diet No. 15 with the physiological content of proteins, fats and carbohydrates, vitamins and minerals.
Particular attention is paid to nutrition in case of burn disease, in which there is an increased breakdown of muscle and visceral proteins. For such patients, the following scheme is used: parenteral nutrition - transition to enteral nutrition - siping (consumption of specialized mixtures in small sips) - transition to specialized diets with a high protein content.
Prevention
The following preventive measures can prevent the development of shock or reduce its severity:
- Timely stopping of bleeding.
- Reliable immobilization for fractures.
- Carrying out analgesia (pain relief).
- Knowledge of the rules for providing self- and mutual assistance and the ability to apply them in the right environment.
- Because serious injuries often occur in the workplace, increased worker vigilance and safety monitoring by management can significantly reduce injuries and related complications.
Consequences and complications
Complications of shock include:
- Increasing respiratory failure ( respiratory distress syndrome ).
- Coagulopathic disorders with possible transition to disseminated intravascular coagulation.
- Traumatic endotoxicosis . Endogenous intoxication develops due to the accumulation of tissue destruction products and is caused by bacterial toxins and vasoactive substances. The effect of these factors manifests itself 48-72 hours after injury.
- Development of fat embolism with bone injuries and extensive destruction of soft tissues.
- Hepatic-renal failure (development of “shock kidney” and “shock liver”).
- Heart failure and central hemodynamic disorders.
- Infectious and septic complications.
- Delay of reparative processes at the site of damage.
The consequence of trauma and shock is post-traumatic syndrome. It develops in people who have experienced life-threatening events (transport accidents, plane crashes, natural disasters) and received injuries as a result. These events deeply affect a person’s psyche, and he loses a sense of security, anxiety, fear appear, sleep disturbances occur, suicidal tendencies and alcohol or drug abuse occur. If the trauma and stress suffered were severe, the painful mental reaction can persist for many years.
Forecast
The prognosis depends on the degree of shock: in the first degree it is favorable, in the second it is doubtful, in the rest it is not favorable. Despite the improvement of anti-shock therapy methods, mortality in severe injuries has decreased slightly. As stated above, shock is a life-threatening condition, but death does not occur from painful shock. The main cause of death from injuries is blood loss in the absence of medical attention. Pain aggravates shock and is not its main cause, much less the cause of death.
Death can also occur after recovery from shock due to multiple organ failure. The immediate cause of death is heart, kidney and liver failure , increasing respiratory failure and coagulopathic disorders.
If death is prevented during the first week, then the threat of generalization of wound infection ( wound sepsis , pneumonia ) is of decisive importance in the patient’s condition. It is infectious complications that occur at a later date that affect the survival of patients. This threat persists for several weeks, as victims of the trauma experience severe metabolic disorders and impaired immunity .
List of sources
- Bagnenko S. F., Lapshin V. N., Shah B. N. Hemodynamic depression in victims with combined trauma in the acute period of traumatic illness is the basis for subsequent hypoxic changes and reperfusion injuries // Efferent Therapy, 2004. Vol. 1, No. 5 . pp. 23–34.
- Shestopalov A. E., Pasko V. G. Volume replacement therapy for acute blood loss in victims with severe combined trauma // Difficult Patient. 2005. No. 4. pp. 17–23.
- Gural K.A., Klyuchevsky V.V., Dambaev G.Ts. Human traumatic shock // International Journal of Experimental Education. – 2011. – No. 12. – P. 15-16.
- Singaevsky, A.B. Current problems of modern severe trauma // Abstracts of the All-Russian Scientific Conference. - St. Petersburg, 2001. - pp. 106-107.
- Sheiko V.D. Surgery of injuries during polytrauma in peacetime and wartime / Textbook. — Poltava ASMI LLC. — 2015. 558 p.