Among ophthalmological diseases, cataracts are considered one of the most dangerous for vision. It occurs in every sixth person on the planet over 40 years of age and is the most common cause of blindness. According to the World Health Organization, more than 47% of blind people have lost their sight due to the development of cataracts.
In this article
- What is a cataract?
- Congenital cataract
- Acquired cataract
- Causes of cataracts
- Symptoms of cataracts
- How quickly does cataract develop?
- Diagnosis of cataracts
- Complications of cataracts with late diagnosis
- Cataract treatment
- Contraindications to cataract removal
- Ways to restore vision after surgery
- Intraocular lens installation
- Complications after cataract surgery
- Postoperative period
- Prevention of cataracts
What is a cataract?
Although most people have heard the concept of cataract, not everyone knows what it is. This pathology is a clouding of the lens, which gradually reduces the quality of vision and, in the absence of proper treatment, ends in a complete loss of visual function. The eye lens is the organ responsible for focusing light rays onto the retina of the eye. Essentially, it is a lens placed between the iris of the eye and the vitreous body, which transmits and refracts light rays. In a young body, the lens, as a rule, has an elastic and transparent structure; it easily changes its shape under the control of the eye muscles, freely “adjusting” the desired sharpness, thanks to which the eyes see well at any distance. With age, the lens becomes denser, less elastic and loses transparency. This state of cloudiness is called a cataract. It can be partial or complete, depending on how much of the eye lens is opaque. A clouded organ transmits light rays into the eye worse and interferes with their correct refraction and focusing. As a result, the patient's visual sharpness decreases, the contours of the objects in question seem blurry, indistinct, and there is a feeling of a “veil” before the eyes. Cataracts gradually develop and can lead to complete loss of vision.
The name of the pathology itself comes from the Greek word, which translated means “waterfall” or “spray of a waterfall.” This name well explains the main symptom of the disease - blurred vision, when a person sees surrounding objects unclearly, as if through a stream of water.
Signs of cataracts
The main and most common clinical sign of cataract is a visual defect, which is characterized as a veil before the eyes. This symptom directly indicates clouding of the lens and is accompanied by a decrease in visual acuity. Most patients describe this symptom as if they are looking at the world through foggy glass, a foggy veil. Often the patient does not notice for a long time that his vision has become worse, since the eye that sees better compensates for the difference in vision. For self-diagnosis, doctors recommend closing your eyes one at a time and checking your vision separately with each eye.
Ophthalmologists include other symptoms of cataracts:
- blurred or blurred vision;
- colors appear dull and faded;
- circles appear around light sources;
- sensitivity to sunlight or bright lights;
- blurred vision at night;
- high need for brighter lighting when reading;
- glasses don't help anymore.
Congenital cataract
Cataracts of the eye can be congenital or acquired. Congenital lens opacity, according to doctors, accounts for over 50% of all congenital eye defects and is considered one of the main causes of poor vision and blindness in young children. Depending on how many eyes are affected by this pathology, it can be bilateral or unilateral. Based on the location of the turbidity, it is divided into several types:
- layered - is the most common, affects several layers of the lens from the core to the periphery, and always has a significant impact on the quality of vision;
- nuclear - affects both eyes and is almost always hereditary, in most cases greatly reduces vision (up to 0.1);
- capsular - it is characterized by clouding of the posterior or anterior capsule of the lens; a decrease in visual acuity directly depends on the degree of clouding of the capsule. May occur in a child due to illness of the pregnant mother or intrauterine inflammation;
- polar - with this type of congenital cataract, opacification affects both eyes, spreading not only to the capsules, but also to the substance of the lens at the posterior or anterior pole. The effect on vision depends on the shape and size of the clouding;
- Complete cataracts, in which the clouding extends to the entire lens, are almost always bilateral. In this case, the child does not see anything, but may experience light sensations. Complete cataracts can develop in the womb or in the first weeks after birth. Often combined with strabismus, nystagmus, microphthalmos and other defects in the development of visual organs;
- Complicated cataracts occur due to severe diseases or infections (viral rubella, diabetes). Usually accompanied by other congenital malformations: deafness, heart disease, etc.
For children born with congenital lens opacity, doctors recommend surgical treatment as early as possible. If this is not done in a timely manner, the child may become blind for life.
Since in the first year of life the baby’s visual function is just developing, the eye with a cloudy lens becomes insensitive to the image, and light rays stop stimulating the retina. This is why, with an advanced form of congenital cataract, vision may not be restored even after surgery. To preserve visual function, ophthalmologists recommend removing the clouded lens within two months after birth. The main difference between congenital and acquired cataracts is the non-progressive form.
Gender factor
A number of epidemiological studies using cross-sectional data have shown that women are at higher risk of developing cataracts compared to men. Some results indicate a general increase in the incidence of this disease. Most investigators report a higher prevalence of cortical cataracts, with only one study showing a higher prevalence of nuclear cataracts among other types (Am J Ophthalmol 1999; 128:446–65). The mechanism of the influence of the gender factor on the occurrence of cataracts is not clear, but may be associated with hormonal differences between women and men.
One reason may be postmenopausal estrogen deficiency. Recent epidemiological data provide some evidence that estrogen and hormone replacement therapy may play a protective role in the development of age-related cataracts (Am J Epidemiol 2002; 155:997–1006). Data from the Beaver Dam Eye Study suggest that early age at menarche, long-term use of estrogen-containing medications, and use of birth control pills prevent the development of nuclear cataracts. The latest Beaver Dam Eye Study assessed the possible association between reproductive age and the incidence of cataracts. The only significant result was the identification of a trend towards a decrease in the incidence of posterior subcapsular cataracts due to an increase in the number of successful deliveries.
Acquired cataract
If clouding of the lens occurs during a person’s life, this form of the disease is called acquired. Its distinctive feature is constant progression. The types of cataracts in this case are determined by the causes of its occurrence. There are senile, traumatic, toxic and other forms of pathology. Based on the location of the clouding, acquired cataracts are divided into the following types:
- nuclear - it is characterized by a brown or yellow coloration of the central part of the eye lens. With this type of pathology, distant vision is more blurred than near vision;
- posterior subcapsular - with it, the clouding is localized on the posterior surface of the lens, often forming a plaque. A person with this type of cataract may complain of difficulty reading, a glowing effect;
- cortical - lens opacification has a radial shape and is localized in the peripheral zone of the lens. Such a lesion often occurs asymptomatically until it affects the central part of the organ.
The main factor in the successful treatment of acquired cataracts is timely detection of symptoms and early diagnosis.
Lens clouding in older people
According to statistics provided by WHO, about 70% of all cases of age-related cataracts occur over the age of 70 years. This means that the older a person gets, the higher the likelihood of lens clouding.
Despite these data, cataracts are not only a disease of the elderly. The disease does not develop due to the fact of aging, but due to changes that occur in the body with age. Some of these changes may well occur at the age of 40-50, it all depends on the individual characteristics of each person’s body, as well as genetic factors.
In old age, the main reason for the development of pathology is considered to be changes that occur in the lens at the biochemical level. This process is regarded by doctors as natural, that is, every person is susceptible to the development of cataracts to a certain extent.
Causes of cataracts
Congenital lens opacity can have several causes:
- heredity;
- chromosomal or gene abnormality - cataracts often occur in children with Down, Marfan, Lowe, and Ehlers-Danlos syndromes;
- genetic changes in the structure of proteins that are responsible for the transparency of the lens;
- taking medications by a pregnant woman - in particular, the use of certain tetracycline antibiotics;
- infectious diseases of the mother during pregnancy - rubella, herpes, chickenpox, cytomegalovirus, measles, toxoplasmosis, polio, Epstein-Barr virus, etc.;
- systemic and chronic diseases of the mother - chronic infections, endocrine system disorders, diabetes mellitus;
- exposure to toxic substances on the fetus - alcohol, nicotine.
Acquired cataracts of the eye have causes not related to the woman’s pregnancy and intrauterine development of the fetus. All these reasons are conventionally divided into external and internal. Internal ones include those caused by age-related changes, the presence of diseases or metabolic disorders. External ones include those associated with traumatic, radiation and other external influences.
The main cause of cataracts is considered to be natural aging of the body. This process is inevitable and cannot be influenced. With age, the eye lens loses its elasticity and transparency, which contributes to the development of the disease. Other causes of cataracts include the following:
- eye injury - a cut, blow, chemical or thermal burn, puncture can lead to clouding of the lens at any age;
- diabetes mellitus - with this disease, cataracts develop very quickly in both eyes;
- prolonged exposure to ultraviolet radiation on the eyeball;
- taking corticosteroids;
- high myopia;
- glaucoma, retinal detachment and other ophthalmic pathologies that lead to metabolic disorders in the eye tissues.
Regardless of the cause of cataracts, the symptoms of the disease are often identical.
What is the nature of cataracts?
To fully understand the mechanism of disease development, it is important to understand that protein compounds are present in the biochemical composition of the lens. They have certain physical, chemical and biological properties, the balance of which ensures the crystal transparency of the lens.
With age, changes occur in the body, accompanied by the process of denaturation of protein compounds. In this case, proteins lose their original properties due to molecular rearrangements. The protein compound in the lens, undergoing these changes, darkens in the manner of egg white during cooking; this biological process is irreversible.
Symptoms of cataracts
The main symptom of cataracts is cloudy, blurry vision. But the difficulty is that the clouding of the lens can have different sizes and different zones of localization, so you may not immediately detect signs of the disease. If cataracts affect the central part of the eye, then the symptoms of the disease appear most clearly: surrounding objects have blurred contours and look fuzzy and cloudy. In addition, in the dark, when the pupil is dilated, the patient sees better than in bright light and a constricted pupil. When cataracts are localized in the peripheral zone of the lens, a person may not notice a deterioration in the quality of vision for a long time, which complicates early diagnosis and does not allow timely treatment.
In addition to a blurred image, the following symptoms may indicate the development of cataracts:
- the pupil becomes white, yellow or gray;
- double vision occurs in the eyes (special attention should be paid to this symptom, because it is characteristic only of the early stage of the disease and allows for a timely diagnosis);
- blurry images cannot be corrected with contact lenses or glasses. A person sees poorly both closely located objects and those distant from him at a considerable distance;
- glare and flashes that often occur at night;
- progressive deterioration of vision;
- increased light sensitivity of the eyes at night and general deterioration of night vision. Any light source irritates the visual organs and seems excessively bright;
- the perception of colors is impaired, which seem paler than before. Violet and blue shades are the most difficult for the eyes to perceive;
- when looking at light sources, halos appear before the eyes;
- temporary improvement in visual acuity, which after a short period of time worsens again;
- Difficulties appear while reading and working with small details.
The following signs will help to suspect congenital cataracts in a newborn:
- the child does not fix his gaze on faces and objects;
- he has squint;
- the pupils are different in color and have spots on them;
- the baby behaves restlessly in bright light;
- the child constantly turns to the mother with the same side;
- the child's eye “twitches” vertically, horizontally or in a circular direction.
Any suspicion of cataracts in a child or adult should be a reason to consult a doctor for an accurate diagnosis.
Types of cataracts
Congenital cataract
Cataracts are one of the most common vision defects in children. Almost half of all ophthalmological diseases that develop in the fetus during a woman’s pregnancy or in a child in the first year of life due to a history of other pathologies are hers. The main distinguishing characteristic of the pathology, besides the fact that it accompanies a person from the moment of birth, is that it almost never progresses.
In children, partial and complete cataracts are equally common; in the second case, clouding affects the entire lens: the child is born blind, usually in both eyes.
Cataracts develop due to disruption of the intrauterine formation of the body. The exact causes of congenital anomalies can be determined by a doctor; the most common are:
- genetic predisposition;
- the impact of radiation or toxins on the body of a pregnant woman, poor ecology;
- smoking;
- drinking alcohol both before and during pregnancy;
- taking certain medications;
- past viral and infectious diseases, mainly during pregnancy, but in some situations before it;
- diabetes;
- poor nutrition;
- lack of vitamins;
- injuries.
Symptoms of the disease in babies differ from those in adults because the newborn cannot assess or report his or her health status. Parents should consult a doctor if:
- the child crosses his eyes;
- the child does not fix his gaze on anything;
- the child begins to be capricious in bright light;
- there are spots on the child's eyes;
- the baby's eyes often twitch;
- The pupil of one eye is a different color from the pupil of the other.
In a number of situations, the diagnosis remains with the patient until the end of his life, but modern advances in medicine make it possible to improve the patient’s condition. Many parents are interested in how cataracts are treated in childhood. There are two methods:
- drug therapy;
- surgical intervention.
Typically, surgery helps children avoid lifelong blindness, protects the retina and preserves the accommodation of the eye. If a child has congenital cataracts, it is better not to postpone an appointment with an ophthalmologist and surgery: if the child does not see objects, then the retina does not develop, which means it will not function even if the lens is replaced, and full vision will not return.
Acquired cataract
According to statistics, every sixth person over 40 years of age has acquired or age-related cataracts, approximately 50% of people over 65 years of age, 70% of people over 75 years of age and almost 100% of people over 80 years of age.
Cataracts develop due to the natural processes of aging of the body: with age, the proteins that make up the lens of the eye begin to disintegrate, and the more of them are destroyed, the lower the visual acuity.
Unfortunately, even if the patient protects the retina, regularly visits a specialist and follows his recommendations, the disease cannot be avoided. But it is possible to delay the onset of the disease and slow its progression so that the clouded lens of the eye has as little impact on the quality of life as possible.
Age-related cataracts begin to develop asymptomatically; only regular consultation with an ophthalmologist can help in making a diagnosis. Protect your health: make an appointment with us at your nearest optical salon.
Traumatic cataract
Blows, contusions, penetrating injuries, exposure to chemicals and other factors can also cause cataracts. Trauma to the organs of vision or head can negatively affect the lens of the eye, which is why various diseases of the affected eye develop. Children and production workers are at risk.
Typically, cataracts appear within a month after the injury. It all starts with decreased vision, which is what becomes the reason to see a doctor. Over time, the disease progresses. Therefore, it is especially important to make an appointment with a doctor and get diagnosed. A number of measures can stop the spread of the disease, maintain eye accommodation, and timely treatment of eye cataracts helps preserve vision and avoid disability, if possible.
Secondary complicated cataract
Primary cataracts are usually corrected with surgical treatment. But, unfortunately, it cannot be guaranteed that the disease will never return. Fibrous changes in the posterior capsule of the eye lens can develop both several months and many years after surgery. The disease that develops again is called secondary complicated cataract.
Secondary cataracts develop for a number of reasons, including:
- taking hormonal or other medications;
- metabolic disease;
- diabetes;
- influence of radiation;
- injuries;
- poor nutrition;
- vitamin deficiency;
- weakened immunity;
- age over 60 years.
How quickly does cataract develop?
Most often, cataracts develop gradually, and their symptoms do not appear simultaneously. Experts distinguish several stages of development of this disease.
- The initial stage is characterized by clouding of the lens in the peripheral zone. Often at this stage the disease has virtually no effect on the quality of vision and goes unnoticed by the patient.
- Immature cataracts are characterized by the fact that the opacities shift from the periphery to the central optical zone, and at this stage a person notices a noticeable deterioration in vision. He can see streaks and spots in front of his eyes, and objects and objects seem blurry.
- When cataracts enter the mature stage, the entire lens is already affected by opacities, and visual acuity may decrease down to light perception.
- With overripe cataracts, the lens fibers are destroyed, the substance liquefies, and the organ acquires a milky color.
Because cataracts do not immediately affect the eyes, many patients miss the onset of the disease and see a doctor at an advanced stage.
Statistics can give an exact answer to the question of how quickly cataracts develop. In about 12% of people, the disease progresses at a rapid rate, with complete loss of vision occurring after about six years; In 15% of people, the disease progresses slowly, and complete clouding of the lens occurs on average after 15 years. Most patients (over 70%) completely lose their vision 7-10 years after the first signs of cataract appear. The exception is the so-called “swelling” cataract. It is characterized by almost instantaneous development, which is accompanied by a rapid enlargement of the lens, which clogs the outflow pathways of intraocular fluid, contributes to increased eye pressure and the appearance of headaches. This type of disease requires urgent hospitalization and surgical treatment.
Stages of cataract development
- Initial.
Clouding of the lens begins, but it goes away almost asymptomatically: the eyes may itch, black flies may fly in front of them, objects may look slightly yellowish, and bright light may be irritating. If patients have farsightedness, it may go away for a while. - Immature cataract .
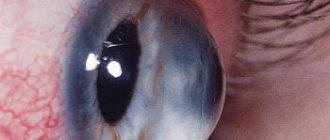
The opacities formed at the edges of the lens begin to unite, and new opacities appear in the center. Immature cataracts are already felt by patients, so they consult a doctor. This stage is optimal for the operation. - Mature cataract (usually a complete cataract).
The disease develops over 1-3 years. The entire lens becomes cloudy and dense, so the patient loses vision and reacts only to light. Mature cataracts are diagnosed with the naked eye, as at this stage the color of the pupil changes. But for an accurate diagnosis, the doctor uses biomicroscopy - the method allows you to study the anterior chamber of the eye, since the posterior layers are no longer visible. Mature cataracts can only be treated surgically, and there is no point in postponing the procedure. Immediate surgical intervention protects the retina, restores accommodation of the eye, visual acuity and overall eye health. - Overripe cataract.
The eye at this stage looks unaesthetic and even frightening: the pupil becomes very light, large, and white spots appear on it. The lens may be dehydrated, its nucleus may sink down, and the protein structures may completely decompose and dissolve. Overmature cataracts look as if there is no pupil at all, so many patients are afraid that treatment will not work. Their fears are justified, but even at this stage it is possible to get good results.
Even mature cataracts are not a death sentence. At the appointment, the doctor will examine the anterior chamber of the eye, assess the condition of the retina and other tissues, select the most appropriate surgical method and help restore vision and accommodation of the eye to the extent possible.
Diagnosis of cataracts
The earlier lens opacification is diagnosed, the higher the patient’s chances of maintaining vision. At the first signs of cataracts, you should immediately consult an experienced ophthalmologist. The main diagnostic method for cataracts is biomicroscopy - the doctor examines the anterior segment of the eye using a light lamp. This device operates on the principle of a microscope and helps to obtain an optical section of the lens, examine its structure in detail at an enlarged size, and determine the extent and localization of opacities. Diagnostic studies also include a number of other standard procedures:
- tonometry - a specialist determines the level of intraocular pressure;
- visometry - evaluates the acuity of visual perception;
- ophthalmoscopy - the doctor examines and evaluates the condition of the fundus of the eye;
- refractometry - using computer technology, an ophthalmologist measures the refraction of the eye.
Also, if necessary, specialized diagnostic methods can be prescribed. Ophthalmometry is the measurement of the radius of curvature and refractive power of the lens or cornea. This technique is used when irreversible changes in the eye lens have begun. Assessing the degree of curvature and refractive power allows us to clarify the stage of the ophthalmological disease. Ophthalmometry is also prescribed before surgical treatment in order to create an eye implant that is anatomically precisely suitable for a particular person. To calculate the power of an intraocular lens, or artificial lens, in addition to ophthalmometry, the anteroposterior axis of the eye (APA) and electrophysiological studies are determined (the lability of the optic nerve and the threshold of electrical sensitivity are determined).
According to indications, before surgical treatment, the doctor may prescribe other diagnostic methods. For example, ultrasound examination in B-mode is prescribed for severe opacities of the vitreous body and lens in order to determine the location, extent and nature of structural changes in the eye. This allows the doctor to choose the appropriate surgical technique. In preparation for surgical treatment, the patient undergoes laboratory tests, which include blood tests, urine tests, x-rays and opinions of a number of specialists (ENT specialist, endocrinologist). Careful preoperative diagnostics allows us to identify possible contraindications to surgical treatment, timely detect and sanitize foci of chronic infection, and decompensate diseases that can cause complications in the postoperative period.
Reviews
Review from Zadolnaya Margarita Ivanovna
5 ★
29.04.2021
Hello. In December 2021, at the Moscow City Hospital on Semenovskaya, I underwent surgical treatment of cataracts in both eyes, complicated by high myopia. Many thanks to the ophthalmologist Yudina Nadezhda Aleksandrovna for my insight! The world is beautiful and amazingly colorful - I now see this thanks to the professionalism, sensitivity, and attentiveness of this wonderful doctor! I would also like to note the well-coordinated and friendly work of the staff of the operating room, reception, examination room, security - the logistics at MGK are excellent, visiting the clinic is always positive. I recommend!
Valery Alexandrovich Firsov
5 ★
16.03.2020
The world has returned in color! Many thanks to all the clinic staff for their friendly and sensitive attitude towards patients. Special thanks to surgeon A.Kh. Dagaev. for two professionally performed lens replacement operations. The world is in color again!
Dear Russians! All those who, unfortunately, were struck by cataracts and blurred vision. Don't cloud your mind - turn to professionals who will bring your colorful world back to you!
Complications of cataracts with late diagnosis or lack of treatment
Once you have been diagnosed with lens opacities, it is important to begin treatment immediately. Treatment of eye cataracts must be carried out even if the symptoms are mild and vision is not yet impaired. The disease will progress, and the deterioration of visual function is only a matter of time. If you ignore treatment for eye cataracts, sooner or later this can lead to the death of the optic nerve, which stops transmitting nerve impulses to the brain, resulting in blindness. There are other complications of cataracts if the diagnosis is delayed.
- Lens luxation.
With this complication, the lens is displaced and separated from the ligament that held it. In this case, vision with cataracts deteriorates sharply, and the patient requires mandatory surgery to remove the lens.
- Phacogenic glaucoma.
Long-term lack of therapy contributes to the growth of opacities, increased intraocular pressure and the development of glaucoma - another dangerous ophthalmological disease. With this complication, surgery and therapy to help reduce eye pressure are indicated.
- Phacolytic iridocyclitis.
The main signs of this complication are inflammation of the iris and ciliary body. A person feels headache and eye pain, the vascular network in the eyes acquires a red or blue tint, and pupil mobility worsens.
- Obscurational amblyopia.
This complication is often observed with congenital cataracts. The main signs are atrophy of the previously healthy retina, cessation of its functioning, and lack of response to visual stimuli. Amblyopia can only be treated surgically. To avoid such serious complications, it is necessary to diagnose cataracts in time and seek professional help at the first symptoms.
Nuclear cataract
Cloudiness in nuclear cataracts affects the sutures and the embryonic nucleus, due to which vision is impaired early. First, the core is affected, then the remaining layers lose their transparency. Vision deteriorates early, as the central part undergoes changes: complaints of false myopia appear, and clear recognition of objects in the distance is also difficult. Upon examination, it is clear that the cloudy central part is separated from the transparent periphery by a sharp boundary, there is no disintegration of the lens tissues. This cataract is dense, the nucleus sometimes changes color to black or brown. For quite a long time, nuclear cataracts in the elderly remain immature, but if the clouding spreads, we can talk about the nuclear-cortical form of the disease. Differential diagnosis is carried out with lens sclerosis.
Cataract treatment
Conservative treatment of cataracts using special eye drops and other medications can slow down the progression of the disease. However, no medicine or eye gymnastics can restore transparency to the lens. As soon as the disease begins to negatively affect the quality of life and seriously impairs vision, doctors recommend surgical removal of the clouded organ and replacing it with an intraocular lens (artificial implant). Today, microsurgical treatment is the only way to get rid of cataracts. According to statistics, normal vision returns to 90% of patients after surgery. Just a few years ago, surgery to remove the lens was performed only for so-called “ripe” cataracts. Modern technologies, the use of the latest operating techniques, and advanced equipment have made it possible to expand the list of indications for cataract surgical treatment.
Today, you don’t have to wait for vision to deteriorate critically, but perform surgery when the acuity is 0.1-0.2. These figures may be even higher if acute vision is a condition for maintaining professional activity. In eye microsurgery, there are several types of operations to remove the lens.
- Extracapsular cataract extraction.
With this method of surgical treatment, the doctor removes the nucleus and masses of the lens, leaving the posterior capsule of the organ in the eyeball. This method is good because it maintains a barrier between the anterior segment of the eye and the vitreous body. Its disadvantage is that it is excessively traumatic, since the doctor has to make an incision in the cornea and apply sutures.
- Intracapsular cataract extraction.
With this method, the lens is removed from the capsule through a large incision. To carry out the manipulation, a cryoextractor is used - a device that freezes the lens to its tip and allows it to be removed. Today the technique is rarely used because it is very traumatic.
- Ultrasonic phacoemulsification.
This method was first used in the 70s of the 20th century, and still remains one of the most popular and effective methods of treating cataracts. During the operation, the ophthalmic surgeon, through a small incision, inserts the tip of a phacoemulsifier into the anterior chamber of the eye - a device that emits ultrasonic vibrations and thus crushes the damaged organ into an emulsion state. After this, the lens masses are removed from the eye using a tube system. Ultrasonic phacoemulsification is less traumatic than extraction techniques, but it also has disadvantages. Ultrasound negatively affects the posterior epithelium of the cornea and intraocular structures. The greater the power and the longer the period of exposure, the stronger the damaging effect. Every year, the surgical technique is improved, new phacoemulsification techniques appear, which help reduce the time of exposure to ultrasound and thereby reduce complications in the postoperative period.
- Laser phacoemulsification.
Today there are several technologies for laser cataract removal, which are based on the use of different types of lasers. The laser method has several advantages. It is effective in removing cataracts at various stages, including when the lens has hardened. The laser effectively destroys the dense core, which is then removed through a microscopic incision. Laser phacoemulsification is used if the lens is resistant to ultrasound. The procedure has minimal contraindications, is low-traumatic and often occurs without complications.
The laser acts on the eye tissue with maximum precision, allowing you to remove even the smallest particles of the lens, which eliminates the possibility of secondary cataracts. The disadvantage of the method can be considered its complexity, which requires high skill from the ophthalmic surgeon. Also, laser treatment is complicated by high degrees of lens opacity, since the opaque medium interferes with the necessary manipulations. Experts say that this method is suitable for only 70% of patients.
The optimal method for cataract removal is determined by an ophthalmologist, taking into account the medical history, indications and contraindications of the individual patient. If lens opacity is diagnosed in both eyes, the specialist first operates on the eye with less visual acuity.
Cataract surgery at MGK
The Moscow Eye Clinic provides diagnostics, conservative and surgical treatment of lens opacities.
Only surgical treatment can radically eliminate the problem of cataracts. To remove a cloudy lens, a phacoemulsification operation is used, aimed at removing the lens while preserving the lens capsule and further installing an intraocular lens into it. This “artificial lens”, which performs the refractive functions of a natural lens, provides the patient with normal vision.
Phakaemulsification of cataracts has virtually no complications. This technique is physiological and will minimize injury to eye tissue. Its result is the patient’s rapid recovery and the opportunity to return to their usual active life.
Contraindications to cataract removal
Despite the fact that surgical removal of the lens is the only way to treat cataracts, not all patients can undergo this operation. There are a number of contraindications to lens removal.
- Infectious ophthalmological diseases.
With conjunctivitis, scleritis, uveitis and other infectious diseases of the eye, the risk of complications in the postoperative period increases, so first the ophthalmologist prescribes drugs to treat the infection and only after the end of therapy begins cataract removal.
- Decompensated glaucoma.
Glaucoma is characterized by increased intraocular pressure. If this condition is not corrected before surgery, it can lead to a dangerous complication - expulsive bleeding, which can result in the death of the eye.
- Pregnancy.
In most cases, doctors recommend postponing lens removal surgery until after pregnancy and breastfeeding.
- Somatic diseases in the acute stage.
- Diabetes mellitus, tumors, and severe multiple sclerosis are contraindications for cataract removal because they increase the risk of complications and worsen the patient’s general condition.
An ophthalmologist will tell you in more detail about contraindications for surgery after a thorough examination of the patient.
Main eye drops prescribed for cataracts
| Vita-Iodurol | Emoxipin | Quinax | Taufon |
In addition to eye drops, ophthalmologists recommend taking tablet forms of vision vitamins to prevent the development of cataracts. As a rule, they contain substances such as lutein and zeaxanthin, vitamins A, B, C, E, and trace elements (selenium, zinc). Some manufacturers produce forms that are strengthened in composition and have the prefix “forte”: “Lutein Forte”, “Okuwait Lutein Forte”, “Blueberry Forte”, etc. As a rule, they are prescribed to people who suffer not only from eye cataracts, but also other related diseases - glaucoma, macular degeneration, diabetic retinopathy, etc.
Ways to restore vision after surgery
Removing the lens does not mean that your eye will completely stop seeing. But the quality of vision will resemble the feeling when you open your eyes underwater. Orientation in space and the ability to perform simple actions are preserved, but the quality of life noticeably deteriorates.
After surgery, glasses, contact lenses, or intraocular lenses (IOLs) can replace the removed lens. For most patients, it is preferable to implant an artificial lens, which is installed instead of one removed immediately during surgical treatment. Glasses and contact lenses are used when the patient has contraindications to implant installation.
Choosing vision correction technology
Only an ophthalmologist can choose the right artificial lens (intraocular lens - IOL) and decide on the possibility of surgery. There are several types of IOLs:
- Monofocal lenses. Provide the best quality of vision at a certain distance (near or far). After implantation of such lenses, patients must use glasses for reading or distance vision.
- Multifocal lenses. Allow patients to see clearly at different distances (near, intermediate and distance) and reduce or eliminate the need to wear glasses after surgery.
- Toric lenses. Allows patients with cataracts to obtain high visual acuity who also require correction of the original corneal astigmatism.
Get a complete vision examination at the Lege Artis Eye Clinic
It's time to correct your vision!
Make an appointment by phone:
8(804) 333-02-14 Free call
Intraocular lens installation
An artificial lens is a clear lens with a specific refractive power that is placed in the eye, centered, and secured during cataract surgery. Modern safe materials are used to make the prosthesis, most often silicone or acrylate. Intraocular lenses can be hard or soft. In modern microsurgery, the latter are used more often, since implantation of an elastic lens requires a minimal incision in the eye tissue. Special elastic arms are usually located along the edge of the implant. With their help, the lens is fixed in the capsular bag of the eye lens. The selection of an artificial lens is carried out by an ophthalmologist, taking into account the vision characteristics and wishes of a particular patient. Monofocal IOLs provide good vision at one distance - near or far; toric ones additionally correct astigmatism. There are also multifocal IOLs, which are specially designed with multiple foci. They provide good vision at far, medium and near distances, helping to reduce dependence or completely abandon glasses. Accommodating lenses that copy the work of the natural lens have a similar effect. Aspherical intraocular lenses provide high-quality images at dusk, in low light conditions. They correct spherical distortions well and help get rid of highlights and halos.
To determine the appropriate type of intraocular lens, the doctor assesses the state of the visual system, and also clarifies with the patient his wishes regarding the range of vision, its quality, and the correction of associated disorders. Artificial lenses made from modern materials are tolerated by most patients. These implants do not require replacement and can serve as a natural lens throughout a person’s life. More recently, American and Chinese biologists have discovered a new way to create an artificial lens using stem cells. Essentially, a new lens is grown directly in the patient's eye after the damaged organ is removed. The authors of the study are confident that in the future this technology will become the main one in the treatment of cataracts. However, today it is completely new, little studied and has not yet found mass application.
Prices for treatment of age-related cataracts
The price of cataract removal using phacoemulsification with implantation of a modern IOL made in the USA, Germany or Great Britain in our clinic starts from 39,500 rubles.
The final price is set after consultation with a specialist and depends on the model of the lens being installed and the condition of the patient’s eyes.
At the same time, you can return 13% of the amount spent using a tax deduction. You can read more about this here.
The operation is performed by surgeons of the highest category: Shpilko Stanislav Andreevich, Dagaev Adam Huseinovich, Ilyukhin Oleg Evgenievich.
You can find out the price of procedures and make an appointment at the Moscow Eye Clinic by phone (daily from 9:00 to 21:00) or through the online registration form.
Complications after cataract surgery
Even modern cataract removal techniques, although they reduce, do not eliminate the risks of complications.
- Swelling and inflammation.
Because this complication is common after surgery, doctors often give the patient antibiotics or anti-inflammatory drugs as a preventative measure.
- Implant displacement.
This complication most often occurs when the prosthesis is not properly fixed. Careful selection of a professional surgeon with extensive experience in performing such operations will help minimize this risk.
- Secondary cataract.
It manifests itself as clouding of the posterior capsule of the lens and decreased vision in the long-term postoperative period. This complication arises due to the fact that after surgery to remove the lens, its epithelial cells remain in the posterior capsule. When they grow or fibrosis of the capsular bag, symptoms that are characteristic of cataracts occur: blurred images, decreased brightness, deterioration of visual acuity. A special laser capsulotomy method is used for treatment.
- Increased intraocular pressure.
Pressure increases when fluid accumulates in the eyes and puts pressure on the optic nerve. To treat this complication, medications are prescribed that promote the outflow of fluid from the eye chamber.
- Bleeding in the eyes.
This complication is rare and requires immediate surgical intervention.
Subcapsular cataract
Opacities in subcapsular age-related cataracts begin from the periphery of the lens in the anterior part of the capsular apparatus. Under it, spaces of different sizes are formed, resembling bowls in appearance. These opacities grow, moving towards the equator, but do not affect the cortical zone. As the pathological process progresses, vision deteriorates more and more. Subcapsular cataracts are distinguished from complicated forms of cataracts. A diagnosis can only be made in a clinical setting using special high-precision equipment.
Postoperative period
Surgical treatment of cataracts, depending on the chosen method of operation, can be performed on an outpatient or inpatient basis. In the second case, the patient is discharged from the hospital after a few days.
To reduce the risk of developing postoperative complications and speed up healing, you must strictly follow the recommendations of doctors:
- for 1.5-2 months it is necessary to instill eye drops with special medications prescribed by a specialist;
- during this period, regularly visit an ophthalmologist to monitor the dynamics of recovery;
- Wear a protective bandage over your eyes that prevents the entry of dust, dirt, smoke, and water.
- If the operation was performed with the replacement of the lens with an intraocular lens, then in order to avoid its displacement, the following rules must be followed:
- do not rub the operated eye or put pressure on it;
- do not sleep on the side where the operated organ is located;
- Do not take a steam bath for a month. You can shower and wash your hair with shampoo a few days after surgery. In this case, it is necessary to close your eyes, and after hygiene procedures, instill them with special drops;
- Limit physical activity for 30 days, avoid lifting heavy objects;
- do not drink alcoholic beverages;
- limit reading until vision is completely stabilized;
- wear safety glasses;
- don't wear makeup.
Your ophthalmologist will give you precise instructions on how to behave in the postoperative period. Rehabilitation usually takes from two months to six months.
Smoking
Observations confirm the connection between smoking and the risk of developing cataracts. The risk of disease in heavy smokers who smoke 15 cigarettes a day or more is three times higher than in non-smokers.
A number of studies have shown that taking antioxidants reduces the risk of developing the disease. A recent study examined the effect of smoking on the development of cataracts in men and women in the United States (Am J Epidemiol 2002;155:72-9). The results suggest that any recovery from damage caused by smoking occurs at a very slow pace. This highlights how important it is not to start smoking at all, or to quit smoking as early as possible. People who quit this bad habit 25 or more years ago have a 20% lower risk of developing the disease than those who continue to smoke. However, the risk for former smokers will not be reduced to the level observed among never smokers.
Prevention of cataracts
Knowing how cataracts develop, you can take preventive measures that will help avoid its occurrence or diagnose it at an early stage, which is very important for effective treatment. Prevention of cataracts includes:
- regular examinations by an ophthalmologist every six months;
- use of sunglasses and contact lenses with a UV filter to protect the eyes from the negative effects of ultraviolet radiation;
- rational nutrition, eating foods rich in antioxidants, avoiding or limiting junk food;
- regular monitoring of blood sugar levels and timely treatment of diabetes mellitus;
- compliance with safety rules when working in chemical plants, laboratories, hot shops and other facilities where there is an increased risk of eye injury;
- thorough hand hygiene protects against eye infections that can cause the development of cataracts;
- quitting smoking, drinking alcohol and other bad habits.
Cataract prevention is especially important for those people who have crossed the age limit of 60 years. At this age, the risk of developing the disease increases, so you need to visit an ophthalmologist at least four times a year and, when the first signs of the disease are detected, begin its treatment immediately. The ability to listen to your body and notice even the slightest changes in the functioning of the visual system will help maintain vision and a high quality of life even with such a serious disease as lens opacity.
Prevention
It is impossible to completely avoid eye disease, but there are ways to protect yourself, delay the disease, or alleviate and slow down its progression.
- Wear sunglasses.
The impact of ultraviolet radiation on the eyes is enormous, which is why it is so important to reduce it. But don’t skimp on your health, don’t buy cheap, low-quality sunglasses, as they don’t protect your eyes, but only darken the surrounding objects so you don’t have to squint. As for UV rays, they continue to enter through glasses and cause damage to vision. The products presented on our website protect the retina well. It is important to us that you look stylish and stay healthy in any situation. Remember: wearing sunglasses isn't just for the sun. Glare from water and snow also negatively affects the eyes. - Stop smoking, including passive smoking.
Substances contained in cigarettes and smoke accelerate the aging process of the body in general and the lens in particular. And since age is one of the main reasons for the development of pathology, smoking provokes its appearance. A healthy lifestyle has a positive effect on health and protects the retina. - Watch your health.
Endocrine diseases, injuries, work in unfavorable conditions, etc. are the reasons why age-related cataracts develop. Therefore, you should not neglect your health. If you have chronic pathologies, you should be regularly checked by a doctor. - Take vitamins.
Cataracts often develop in people with weakened immune systems and vitamin deficiency. Try to avoid these conditions. Discuss with your doctor which vitamins are best to take. Perhaps he will be able to choose a complex for you that not only strengthens the entire body, but also protects the retina. - Do not self-medicate.
Even if it is written on the drug or in the advertisement that the product protects the retina, you cannot buy it without a doctor’s advice. - Visit your doctor if you take various medications for a long time.
Don't forget to get tested regularly and track important indicators of life and health. - Eat right.
An excellent measure to prevent cataracts is proper nutrition. It is advisable to keep fatty, spicy, fried foods to a minimum. And there should be as much fruit, fresh and stewed vegetables in the diet as possible. It is worth adding red fish to it, it has a positive effect on vision and, together with other foods and a healthy lifestyle, also protects the retina.
Forecast
If left untreated, cataracts lead to blindness. Usually this process takes decades, but in some cases (in the presence of aggravating factors) vision loss can develop rapidly, in just 1-2 years. A favorable prognosis is possible only with surgery. The outcome of surgical treatment is influenced by internal and external factors. Internal ones include:
- Patient's age – very elderly people may experience lower treatment results.
- The presence of ophthalmological diseases (glaucoma, retinal detachment, corneal dystrophy, severe myopia).
- Diseases of the endocrine system, metabolic disorders in the body.
- Tumors.
- Hypertonic disease.
- Autoimmune disorders.
External factors include:
- Poor nutrition, lack of vitamins and minerals.
- Eye injuries.
- Operations.
In general, the prognosis for cataract surgery is favorable. Complications occur only in 1-2% of cases.
Is surgery necessary?
This question worries many patients, but there is no clear answer to it. In most cases, everything is individual. If you have been diagnosed with cataracts, then surgery is inevitable. Moreover, the sooner it is performed, the safer it will be for the eye and it is better not to delay it. For one person, minimal clouding of the lens may not be an indication for surgical manipulation, but for another it may greatly complicate his life and cause discomfort.
After 50 years, the lens stops performing its functions properly - clouding and presbyopia develop. Ophthalmologists at CVH, relying on the opinion of authoritative experts around the world, recommend removing it and replacing it with a high-quality implant - an intraocular lens. Our center also uses the latest PanOptix multifocal lenses.
There is no need to be afraid of surgery. Our clinic is equipped with modern equipment from leading global manufacturers, and our specialists are qualified doctors with extensive experience. The surgical procedure takes only 5 minutes and is completely safe. It is carried out with initial cataracts or even in its absence, to correct poor vision for refractive purposes.
Modern artificial lenses have the same functions as natural ones. The American company Alcon produces the AcrySof IQ IOL. This is a high-quality imitation of a healthy lens, which has the following advantages:
- reduction of optical aberrations;
- vision becomes comfortable and functional in any lighting;
- natural and rapid adaptation to the implant is provided;
- hydrophobic lenses.
There are currently no reported cases of complications or implant failure with PanOptix multifocal IOLs.
Treatment of the initial stage of cataracts
Non-surgical methods of combating initial cataracts include drug treatment, taking vitamin complexes and various diets. But you need to understand that if a cataract is diagnosed, it will develop and this process cannot be stopped.
The conservative method involves the use of various biologically active substances that act as blockers of eye lens abnormalities. One part of them is available in the form of drops. The other is in the form of injections, administered intramuscularly.
Complexes of vitamins and minerals are aimed at normalizing metabolic processes in the eyeball. They necessarily contain taurine and adenosine, as well as other elements that have a beneficial effect on the lens. What the doctor may prescribe:
- "Facovit." The medicine is sold in pharmacies in the form of drops and is intended to improve metabolism and block an increase in the area of lens clouding.
- Quinax.” In the case of cataracts, this drug is most often prescribed by an ophthalmologist. It eliminates symptoms well, prevents oxidation of the lens, and improves metabolism.
- "Taufon". Stabilizes metabolic processes and stimulates regenerative processes in the body. Protects the eye from pathogenic microflora, which can cause infection and other complications.
- "Catarax". The medication prevents the spread of clouding and destruction of the lens by slowing down protein reactions (protein is the main component of the eyeball). Drops trigger active metabolism, accelerating the regenerative function of the visual organ. Allowed for use during pregnancy and lactation.
It is not recommended to use medications on your own initiative. The type and dosage should be prescribed exclusively by the attending physician, taking into account the individuality of each case and contraindications.
Treatment of initial cataracts also includes diet. It consists of limiting foods and dishes high in fat - they increase cholesterol in the blood. You need to eat red fish, black currants, and spinach. These products contain a lot of vitamins C, E, and omega-3 fatty acids that are beneficial for vision. They delay the development of eye diseases and have a beneficial effect on the entire body.