Paronychia of the finger (according to ICD 10 code L03.0) occurs in adults and children. This is an inflammation of the lateral and proximal nail folds or skin folds that surround the nail. The main reason for the start of the inflammatory process is the destruction of the protective barrier, which prevents foreign particles and pathogenic microorganisms from penetrating deep into the skin. According to statistics, paronychia occurs 5 times more often in girls and women than in men. Out of the desire to be beautiful, women subject their nails to various, not always safe, procedures. The greatest risk of infection is in middle-aged women. The disease paronychia is otherwise called periungual panaritium. There are acute and chronic forms of inflammation. Their causes and treatments differ.
How does paronychia manifest?
The process itself takes place on the palms, but due to the thickness of the skin, the liquid penetrates through the lymphatic openings to the areas surrounding the nail plate. Often paronychia provokes the occurrence of periungual panacirium - acute purulent inflammation of the tissues of the finger.
The nature of the course of this disease can be:
- Acute , in which it lasts less than one and a half months. The disease is bacterial in nature and is accompanied by severe pain and suppuration, mainly on the back of the fingers. Tissues located closer to the palm may also be affected - in this case, the inflammation spreads deeply, involving the hand.
- Chronic , with a duration of more than one and a half months. As a rule, this type of paronychia is caused by chemicals, dermatitis, psoriasis, eczema, and onychomycosis. In the chronic course of the disease (without the development of an abscess), the nail plate is affected: it becomes deformed, splits, becomes dull and yellow, crumbles, thickens (with fungal infection).
Diagnostics
If you suspect acute paronychia, contact a podiatrist or surgeon if there is no podiatrist nearby. The diagnosis is made based on clinical symptoms, interviewing the person, and examining the affected area. It is important to talk about the specifics of your work and previous injuries in the nail area. The doctor will check whether there is an accumulation of purulent masses (abscess), assess the severity of the condition and decide on the method of treatment.
When diagnosing paronychia, it is important not to confuse the disease with other possible disorders in the nail plate area with similar symptoms.
These include:
- Superficial infection, which manifests as erythema and swelling in the affected part without throbbing pain;
- Panaritium or purulent inflammation of the deep layers of the skin of the finger. Characterized by a severe course. Paronychia is considered the initial stage of felon. With felon, redness, pain and the formation of a bubble with purulent contents do not necessarily occur near the nail. The affected area becomes warm, red, tense and very painful;
- Herpetic infection of the distal (upper) phalanx of the fingers. In this case, before the onset of the inflammatory process, the person will experience burning and itching. Herpetic infection of the fingers is characterized by the formation of vesicles, pain, and redness;
- Onychomycosis. This is a fungal infection of the nail that causes a cloudy, yellowish coloration of the nail plate.
- Squamous cell carcinoma. It mainly affects the skin, but sometimes also affects the nail bed. This is a rare malignant subungual tumor that may be mistaken for chronic paronychia;
In addition, it is important to carry out a differential diagnosis with eczema, posriasis and Reiter's syndrome (joint damage that can cause accumulation of pus in the area of the nail fold).
Instrumental diagnostic methods, such as radiography, ultrasound, and laboratory tests are prescribed only if the observed clinical picture of paronychia is atypical and raises doubts about the diagnosis.
Causes of the disease
Hands and nails are an area of increased risk of injury. The skin surrounding the nail plate is quite thin, so it is easy to damage. The inflammatory process that develops in tissues is the result of injury. Women suffer from paronychia much more often than men, and the main reason for this is manicure done with instruments that have not been sterilized. Infectious agents such as staphylococci, streptococci, and fungi penetrate into soft tissues.
Factors that can lead to inflammation:
- constant mechanical impact on the hands or feet, work at elevated temperatures;
- frequent contact with aggressive chemicals or cold water;
- hangnails (in children, the habit of biting their nails and the skin around them);
- injury during manicure or pedicure;
- nail extensions;
- poor hand skin care, which results in cracks;
- weak immunity;
- insufficient hygiene;
- inappropriate or low-quality shoes, as well as using someone else’s shoes;
- thrombosis, thrombophlebitis and other diseases in which blood circulation in the feet is disrupted;
- lack of vitamins, unhealthy diet;
- stress;
- diseases of the endocrine system, especially diabetes.
List of sources
- Petrov CB Purulent diseases of the fingers and hand / CB Petrov, HA Bubnova // General surgery / CB Petrov. M, 2007. - P. 592-708.
- Lyubsky A.S., Alekseev M.S., Lyubsky A.A., Brovkin A.E. and others. Errors and complications when providing medical care to patients with purulent-inflammatory diseases of the fingers and hands at the outpatient and inpatient stages // Attending physician. - 2000. - No. 3.
- Chadaev A.P. Purulent diseases of the fingers and hand / A.P. Chadayev, A.Ts. Butkevich, G.G. Savzyan. - M.: Helikon, 1996. - 148 p.
- Meleshevich A.V. Felon and phlegmon of the hand: a tutorial in 3 parts. – Grodno: Grodno State University. – 2002. – 185 p.
- Complex treatment of felons in a surgical hospital: Methodological recommendations / A.V. Shcherbatykh, S.M. Kuznetsov, P.E. Krainyukov, V.I. Kalashnikov and others / Irkutsk, state. honey. univ. - Irkutsk: "ASPrint", 2004. - 28 p.
Classification of paronychia and main symptoms
Characteristic forms
- Simple types of paronychia manifest themselves as an independent form of the disease, which is not a consequence of complications of other diseases. The skin around the nail turns red, swells, and minor pain appears. As a rule, with good immunity, the body copes with a simple form of paronychia in a few days; a visit to a doctor is not required.
- The purulent (pyococcal) form develops when microorganisms (staphylococci, streptococci) enter the tissues. The disease begins with the appearance of swelling and throbbing pain. After a couple of days, suppuration of the soft tissue occurs. Recovery begins after opening the abscess. Sometimes an abscess can spread to the hand; extremely rarely, it can spread throughout the body, affecting internal organs.
- Candidiasis is a form caused by fungi of the genus Candida. The nail fold loses the inner layer that protects the nail from damage. This form is chronic and is accompanied by minor inflammation. The purulent process is usually absent or not very pronounced. When fungi affect not only the skin, but also the nail plate, it begins to peel, crumble, thicken, and change shade. Most often, workers in the confectionery industry suffer from inflammation in the chronic stage.
- Ulcerative form - usually caused by pathogenic microorganisms or household chemicals, temperature exposure, injury, eczema or psoriasis. Ulcerative paronychia sometimes manifests itself as a complication of a simple form. Sores form on the skin around the nail, which can cause secondary infection.
- Horny form - occurs infrequently, mainly in patients with syphilis, characterized by the appearance of hyperkeratotic papules.
- The dry form is characterized by mild inflammation and the absence of suppuration. At the same time, the nail fold noticeably becomes coarser and flakes off.
- Tourniol is a form in which beta-hemolytic streptococci, staphylococci, and fungal microflora enter the tissue through wounds and burrs. Loose bubbles appear on the skin, the contents of which begin to fester. After opening the blisters, horseshoe-shaped wounds remain around the nail. Symptoms such as weakness and increased body temperature may appear. Tourniol is dangerous due to complete detachment of the nail and the development of lymphadenitis.
- Eczematous and psoriatic forms - the nail fold swells, becomes slightly inflamed, blisters appear, peeling, and the skin becomes thick. When the vesicles break open, crusts form. The nails acquire a lattice surface, longitudinal grooves, turn yellow, crumble and peel.
With the development of a purulent process, only the smallest ulcers open on their own. Therefore, to avoid an abscess, it is necessary to seek medical help as soon as possible.
Possible complications
With timely treatment of paronychia, fingers or toes are quickly cured. If you delay it and wait for everything to go away on its own, then the infection will even reach the muscles, tendons, bones of the finger, and enter the systemic bloodstream. Accumulations of pus can undermine the nail and lead to its detachment from the nail bed. In advanced stages, partial or complete removal of the nail plate with long-term rehabilitation is often required.
The main complication of chronic paronychia is nail dystrophy, caused by inflammation in the nail matrix. It manifests itself in the form of fragility, delamination of the nail plate, distortion of the shape, and the formation of grooves and grooves. The color of the nail plate may change.
Symptoms
Typically, the signs of paronychia are quite pronounced, which allows you to make a diagnosis quickly and accurately. They are expressed as follows:
- the patient complains of pain in the area of the nail plate; the nature of the pain can be different: throbbing, constant, pulling;
- swelling of the nail fold occurs and can spread to the entire upper part of the finger;
- due to swelling and pain, it is difficult to bend your fingers and work with your hands; if parochinia has developed on the foot, it hurts to put on shoes;
- damaged skin becomes red, burgundy, dark purple, and if there is suppuration, then yellow-green;
- if the process affects several fingers, body temperature often rises and pain appears.
The doctor determines the presence of the disease and determines the cause of the pathology: it may be associated with professional activity or with exposure to pathogenic microorganisms. In the second case, a microbiological test is prescribed to determine which pathogen caused the disease.
To confirm the inflammation process, the patient undergoes a general blood and urine test.
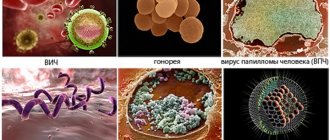
Based on the type of pathogen, paronychia is divided into:
- bacterial: in acute cases the culprit is Staphylococcus aureus, and in chronic cases – streptococci and pseudomonads;
- viral, the causative agent of which is the herpes simplex virus;
- fungal, in which infection occurs with fungi of the genus Candida;
- non-infectious, developing from exposure to adverse and irritating environmental factors, as well as as a side effect from taking certain medications; may be associated with skin diseases.
The “leaders” are bacterial and fungal forms of paronychia.
Clinical picture of different forms of panaritium
Symptoms of any form of panaritium include local and general infectious manifestations. Their severity depends on the depth and localization of the inflammatory process, as well as on the virulence of the pathogen and the activity of the immune response.
General manifestations of the disease include signs of intoxication (weakness, malaise, headaches, tachycardia), hyperthermia, even the development of fever. They can also occur in the most superficial form, when local changes are still limited to the thickness of the skin. This depends on the activity of the pathogen, the nature of the toxins it produces and the reactivity of the patient’s body. It is also possible to develop regional lymphangitis and lymphadenitis.
Local manifestations include skin changes in the affected area: pain, redness, swelling (swelling), locally increased temperature. With superficial forms of panaritium, at the stage of transition of inflammation to the purulent stage, an accumulation of pus is often visible. And with a percutaneous breakthrough, it is released out. Severe pain and tissue infiltration lead to limited mobility of the affected finger and forced removal from use.
But different types of panaritium also have their own characteristics.
Cutaneous and subcutaneous form
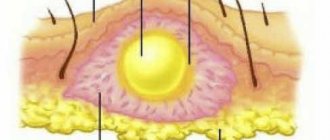
The cutaneous form is referred to when the purulent focus is localized under the epidermis. The accumulating exudate exfoliates the skin, forming a flat or convex bubble. Its contents can be serous, purulent and with hemorrhagic admixture. Patients with the cutaneous form rarely see a doctor. Their panaritium opens spontaneously; many also evacuate the accumulation of pus by puncturing it with a needle or using nail scissors.
The subcutaneous form is the most common. It is with this felon that people most often turn to the doctor, most often already at the purulent stage of the disease. The inflammatory focus is located in the subcutaneous tissue and is limited on the sides by connective tissue cords. Severe swelling of the inflamed tissues and accumulating pus lead to tension of the last natural formations. This becomes the cause of pronounced increasing pain, which acquires a twitching character as inflammation transitions from catarrhal to purulent. In this case, chills are often noted.
The subcutaneous panaritium rarely opens spontaneously. This is explained by the rapid closure of the wound channel (through which the infection entered) even before the accumulation of pus and the tendency for the infiltrate to sink along the fibrous septa. The source of inflammation can be determined by the clearing zone on a hyperemic and edematous background.
There is a combined form, when the panaritium has an hourglass shape with 2 communicating foci: cutaneous and subcutaneous. Most often, it develops with purulent melting of the basal layers of the skin as a result of the progression of inflammation. Such an abscess is also called cufflink-shaped.
Periungual and subungual form
The lesion is often localized in the periungual ridges. This is explained by the prevalence of microtraumas of the skin in this area due to overly diligent manicure trimming or the tendency to break off hangnails. In most cases, felon in a newborn is periungual. After all, young parents who do not have the proper experience often use traumatic conventional manicure tools or try to cut the corners of the child’s nail plates as short as possible.
The periungual panaritium is accompanied by thickening and hyperemia of the ridges, from under which drying serous-purulent fluid soon begins to ooze. In this case, a purulent cavity may not form; inflammation remains at the infiltration stage. If pus leads to the melting of deep-lying tissues, the process spreads in the horizontal and vertical directions. In this case, a branched cavity is formed, each pocket of which can open independently.
In case of damage to the upper periungual fold, panaritium is called paronychia. Here, the inflammatory focus is located in close proximity to the base of the nail plate, which can contribute to its detachment. The inflammatory process becomes subungual, and the plate lags behind its bed. Over time, pus can break out from its sides or, as the nail grows, come out from under the edge.
Subungual panaritium can also form primarily when the nail plate is broken or penetrated. But the most common cause of the development of this form of the disease is a splinter.
Acute paronychia
1. Panaritium against the background of nail fungus 2. Subungual panaritium
Herpetic whitlow
Tendon panaritium
The tendon form of the disease rarely occurs primarily. This is only possible with deep penetrating wounds of the fingers. Usually the subcutaneous tissue is also involved in the process. Most often, the tendons (or rather, the sheaths surrounding them) are affected as the superficial panaritium progresses. Moreover, at first the inflammation is reactive in nature, subsequently the penetration of the pathogen and suppuration of the already formed transudate occurs.
This form of the disease is also called tenosynovitis. The affected finger is sharply swollen, reddened, and constantly bent. Intoxication almost always occurs. The patient feels constant pain, which sharply intensifies when trying to actively or passively straighten the inflamed finger. A gentle position of the limb quickly leads to temporary disability of the patient.
The tendon form is the most severe type of disease, which most often leads to complications even with timely initiation of treatment.
Bone type of disease
Bone felon most often develops on the terminal phalanx. The bone located here is loose, spongy, has no internal canal and is abundantly vascularized from the subperiosteal vessels. This makes it easier for infection to penetrate from the inflamed tissue. In addition, on the terminal phalanx the bone is located very close to the nail bed, which also facilitates the transformation of paronychia into bony panaritium. Less commonly, this form of the disease develops with open fractures of the finger, usually accompanied by crushing and infection of soft tissues.
In fact, bone damage with such panaritium is osteomyelitis. A situation often occurs when bone destruction develops after the opening of a subcutaneous or periungual lesion and a period of improvement. This is explained by insufficiently complete emptying of the purulent cavity and early closure of the surgical wound.
Signs of bone panaritium are constant deep pain in the affected phalanx and the appearance of bone sequestra (pieces of bone) in the scanty discharge from a purulent wound. Body temperature rises, swelling increases sharply. The phalanx takes on a club-shaped appearance, and axial load on it becomes painful.
But many patients quickly get used to the existing pain and do not consult a doctor, preferring independent treatment with folk remedies. This is fraught with aggravation of the situation and further spread of infection, up to the development of sepsis.
Articular felon
An uncommon but disabling form of the disease. This is destructive purulent arthritis. Damage to the joints of the fingers most often occurs after injury to the skin on their dorsal or lateral surface, where there is little subcutaneous tissue.
Symptoms of the disease are severe swelling and severe pain in the affected joint, leading to a significant limitation of its mobility. The skin over it is reddened, hot, stretched tightly until the natural folds disappear. If treatment is untimely or insufficiently intensive, the adjacent tendon bursa, cartilage and bones are involved in inflammation, and the joint is irreversibly destroyed.
Pandactylitis
Pandactylitis is by no means an acutely developing form of the disease. It may be the result of the progression of various types of panaritium, with the spread of the purulent process to all adjacent tissues. But sometimes pandactylitis forms without clearly defined signs of local inflammation. This is possible when a finger is infected with highly virulent pathogens that tend to spread quickly and produce powerful toxins.
Pandactylitis is accompanied by severe intoxication, purulent axillary lymphadenitis and a potentially life-threatening septic condition. The finger is severely swollen, bluish-purple in color and sometimes with areas of ulceration. The patient experiences constant intense pain that intensifies with touching and attempting to move.
Treatment options
The initial stage of the disease can be treated conservatively. If slight redness and mild swelling occur, you can use home methods. If a purulent process is noticeable, emergency assistance from a specialist - a podologist, surgeon, or dermatologist - will be required. For any inflammation accompanied by the accumulation of pus, surgical intervention is necessary.
During the treatment process, you need to remember the following rules:
- When doing housework and any other work, hands must remain dry, all actions are carried out wearing protective gloves;
- if the cause of the disease is chemicals, you need to temporarily stop or at least limit contact with them;
- if parochinia is localized on the feet, you should wear only comfortable, spacious shoes of good quality.
Treatment of purulent form
If an abscess is present, the abscess is opened surgically. If this is not done, the patient's condition will inevitably worsen. This operation is performed with or without local anesthesia. In the first case, small incisions are made on the skin, in the second, punctures are made with a needle. Immediately after opening the abscess, a bandage with ointment is applied, the pain stops, and the patient feels relief. Ointments must be effective against Staphylococcus aureus. Drainage is almost always installed to speed up the separation of pus. In more serious cases, where the abscess has spread to the nail bed or there is an ingrown nail, partial removal of the nail may be necessary. Oral antibiotics are also prescribed, especially if the immune system is weak.
If the cause of parochinia is a fungus, antifungal drugs are used, for example, clotrimazole. Sometimes the doctor prescribes antifungal medications for internal use, such as fluconazole.
Parochinia, which has developed against the background of eczema, psoriasis or syphilis, requires specific treatment methods. Conventional therapeutic measures are supplemented by physiotherapeutic procedures (corticosteroids, ultraviolet irradiation).
After the operation and installation of drainage, the patient should come back for a follow-up appointment some time later to assess the condition. Usually, with adequate care and compliance with all medical recommendations, paronychia is completely cured and has no relapses. The patient is recommended to take multivitamin complexes to strengthen the body's protective reserves.
Treatment of paronychia with home methods
You can engage in independent treatment only if there is no purulent inflammation. Under no circumstances should children be treated at home!
If there is definitely no abscess, then baths with antiseptics (chlorhexidine, povidone-iodine), which are done several times a day for 15 minutes, will help.
Herbs such as calendula and chamomile also have antiseptic properties. Decoctions of them can also be used in the form of baths.
A good effect is obtained by using a solution of sea salt, as well as soda and potassium permanganate for baths.
The listed solutions can also be used for compresses.
Doctors surgeons
Dzhadzhiev Andrey Borisovich Surgeon
Cost of admission 1500
₽
Make an appointment
Marynich Alexander Alexandrovich Vascular surgeon, phlebologist, angiologist
Cost of admission 1500
₽
Make an appointment
Myshlyaev Anton Vsevolodovich Surgeon coloproctologist
Cost of admission 2000
₽
Make an appointment
Prevention of paronychia
Prevention:
- keep your hands and feet clean and dry at all times;
- get rid of the bad habit of biting your nails and surrounding skin;
- After washing your hands, apply cream to the skin;
- When contacting aggressive chemicals, be sure to use gloves;
- do not cut the cuticle, especially on the toes;
- do not bite off hangnails;
- disinfect manicure and pedicure tools;
- trim toenails correctly to prevent ingrown nails;
- fight sweaty feet;
- monitor blood glucose levels;
- wear comfortable, high-quality and dry shoes.
If infection does occur, paronychia begins to develop, without wasting time, seek medical help. This will allow you to cure the disease painlessly, in a short time and without the risk of complications.
Features of the rehabilitation period
Complete healing takes about a week on average. During this period, it is necessary to adhere to the surgeon’s recommendations regarding dressings, drug therapy and regimen. Until the wound heals, you should not put any weight on the operated finger or the limb as a whole.
Dressings should be done daily using antiseptics and wound healing agents prescribed by the doctor. To prevent recurrence of the disease and eliminate the risk of further spread of the inflammatory process, antibiotics may be prescribed by your doctor according to indications.