Fetal development
The physiological indicators of the child’s height and weight are already quite impressive, especially compared to the first months of pregnancy. At this time, his height is about 44 cm, and his weight reaches 2 kg. The baby feels a little cramped in his stomach, so he can no longer turn from head to foot. The child, of course, continues to move, and the woman should feel these movements. From this time on, the fetus begins to actively accumulate subcutaneous fat, and muscle strength increases.
Lanugo gradually disappears, all organ systems improve. The brain is finally formed, but the neural connections will continue to be sharpened for a long time, including after the birth of the child. At the same time, the baby is already able to express his emotions and feel the mother’s mood. He hears loud sounds perfectly, can distinguish smell and taste, he needs care, affection and love. The baby may express his dissatisfaction, for example, if he does not like a sharp noise. Therefore, you need to be very picky when choosing the environment.
The child can play at this time, which is what he actively does when he is not sleeping. For now, he uses the umbilical cord and his body as toys. The baby’s life is measured and calm, and he has nowhere to rush, because the process of preparing for childbirth is not yet completed.
The pulmonary system also continues to actively improve so that after birth the baby can breathe independently. For this purpose, surfactant accumulates in the alveoli.
- The cardiovascular system continues to develop and strengthen. A small heart performs 100-150 beats per minute.
- The child's kidneys are already able to carry out the filtration function.
- The pattern on the skin becomes more expressive every week. It takes on a color that is closer to pink rather than red. The hair on your scalp continues to grow, becoming longer and thicker.
- Calcium accumulates in the bones, making them stronger. The cartilage tissue gradually thickens, but the seams of the skull remain wide. This is necessary for the baby to easily pass through the birth canal.
- The immune system is developing, but it is still very far from perfect.
At 33 weeks of pregnancy, the baby is in the correct position in the uterus. Normally, he should lie head down. However, sometimes the fetus is positioned exactly the opposite way - head up, or even laid on its side. If, with a breech presentation, independent childbirth is still possible, then with a transverse presentation, a cesarean section will definitely be required.
Fetal fetometry: table of body measurements of the unborn baby
Fetal ultrasound The table of fetal fetometry indicators is the norms of various sizes of an intrauterine developing child, determined by ultrasound . It was compiled on the basis of measurements taken in a large sample and subsequent statistical analysis of the results obtained. It is this table that is the basis for determining the duration of pregnancy.
In addition, by comparing the sizes obtained for a particular child with the norms, the symmetry of its development and compliance with the calculated gestational age are assessed. The content of the article
- How to prepare for research
- How is the procedure for measuring baby parameters carried out?
- Which table will help you find out what age your baby is at?
- What parameters are assessed from week 13
- What is "norm"
How to prepare for research
The measurement of the developing baby in utero is carried out during an ultrasound. This study can be performed either with a transvaginal sensor or through the anterior abdominal wall.
If the procedure will be performed through the vagina, there is no need to prepare for fetal fetometry. If you are planning a transabdominal ultrasound, then in the early stages of pregnancy you will need to drink about half a liter of water an hour before the examination and not go to the toilet after that.
This is necessary so that through a full bladder, like through a window, you can look into the uterine cavity. After 12 weeks, this is no longer required, since the necessary “window” is created by amniotic fluid.
How is the procedure for measuring baby parameters carried out?
A woman comes to the ultrasound room, where she undergoes a regular ultrasound examination - through the wall of the abdomen (then the abdomen is lubricated with a special gel) or through the vagina (a condom is put on the sensor).
Next, the doctor performing the ultrasound also performs fetometry: measures the main indicators of circumferences, diameters and lengths. Then these indicators are compared with standard fetal fetometry tables by week.
Which table will help you find out what age your baby is at?
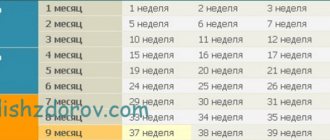
The fetal fetometry data table consists of quite a few indicators. From 5 to 13 weeks, only three fetal sizes are assessed by ultrasound:
- coccygeal-parietal size (CRL, KTP) is the maximum distance that can be measured from the head to the coccyx
- biparietal distance (BPD) can be measured from one parietal bone to the other, that is, we can say that this is the diameter of the head
- the fertilized egg (FE) is the volume of the cavity in which the baby develops; later the placenta and water around it will appear there.
| Term | PY, mm | BPD, mm | CRL, mm |
| 5 | 5 | 1-3 | |
| 6 | 13 | 4-6 | |
| 7 | 21 | 3 | 8-10 |
| 8 | 29 | 7 | 14-16 |
| 9 | 36 | 10 | 22-23 |
| 10 | 44 | 14 | 31-32 |
| 11 | 51 | 17 | 41-43 |
| 12 | 57 | 20-22 | 42-73 |
| 13 | 63 | 24-26 | 51-87 |
This is what the table of fetal sizes looks like according to ultrasound, with which comparison is made to determine whether it corresponds to the norm.
What parameters are assessed from week 13
The size of the child according to ultrasound is estimated based on:
- OG – head circumference (girth)
- BDP – biparietal size (BPD), that is, the distance between the most distant points of the parietal bones
- DB – femur lengthwise
- LZR – fronto-occipital size, that is, the distance between the most distant points of the forehead and the back of the head
- OB – circumference (girth) of the abdomen
- SDA - abdominal diameter in the anteroposterior direction, that is, sagittal size
- PJ is the diameter of the abdomen in diameter
- OG (or DrGK) – circumference (girth) of the chest
- DP – humerus length
- There are also lengths of the tibia, fibula, radius, ulna, and foot. Each of them has its own norm.
You can evaluate pregnancy using fetometry by comparing the indicators indicated in the transcript of your personal ultrasound with the standard parameters in the available tables.
Fetal ultrasound
It is especially important to compare the BDP or coccygeal-parietal distance - these 2 criteria are fundamental for determining the gestational age using ultrasound.
| Duration in weeks | LZD | BPD | OG | coolant | SJ | PJ | DB | DP | Dl.M.Bertz | L.B.berts | DgrK |
| 13 | 32 | 96 | 67 | 21 | 22 | 11 | 10 | 8 | 9 | 24 | |
| 14 | 35 | 26 | 106 | 78 | 24 | 25 | 15 | 13 | 11 | 12 | 26 |
| 15 | 39 | 32 | 118 | 89 | 28 | 29 | 18 | 17 | 14 | 15 | 28 |
| 16 | 43 | 35 | 130 | 100 | 31 | 32 | 21 | 20 | 17 | 18 | 34 |
| 17 | 47 | 39 | 143 | 111 | 35 | 36 | 24 | 23 | 20 | 21 | 38 |
| 18 | 52 | 42 | 155 | 122 | 38 | 39 | 27 | 26 | 2 | 24 | 41 |
| 19 | 56 | 44 | 168 | 132 | 42 | 43 | 30 | 28 | 25 | 26 | 44 |
Fetal fetometry at 20 weeks presents the following indicators (data in mm)
In the photo: embryo on ultrasound at 6-7 weeks of pregnancy
- BPR: 47-49
- OG:181
- DGrK: 48
- LZR: 60
- Coolant: 143
- PJ: 46
- SJ: 45
- thigh length: 33
- normal length of tibia: 29
- fibula length: 28
- shoulder length: 31
- length of forearm bones (radius/ulna) = 25/28
- foot of a 20-week fetus – 33.
Fetal fetometry at 22 weeks is represented by the following indicators in millimeters
- BPR: 54-56
- OG: 206
- DGrK: 53
- Coolant: 165
- PJ: 53
- SJ: 52
- hip: 39
- fibula/tibia (tibia): 33/34
- shoulder: 36
- Radius/ulna = 30/33
Fetometric parameters at 23 weeks (indicators in millimeters)
In the photo: embryo on ultrasound at 6-7 weeks of pregnancy
- BPR: 57-59
- OG: 218
- DGrK: 56
- Coolant: 175
- PJ: 55
- SJ: 56
- hip: 41
- shin = 35/36
- shoulder: 38
- forearm: 32/35
- height: 31 cm
- 580-600 g.
Fetal fetometry upon reaching 31 weeks (figures are in mm)
- BPR: 80-82
- OG: 301
- DGrK: 81
- Coolant: 258
- PJ: 82
- SJ: 81
- hip: 60
- shin = 51/52 mm
- shoulder: 54
- forearm bones = 44/50
- height: 42 cm
- body weight: 1590-1690.
Fetometry norms at 32 weeks on average look like this (mm)
- BPR: 83-85
- OG: 309
- DGrK: 83
- Coolant: 266
- PJ: 85
- SJ: 84
- hip: 62
- shin = 52/54
- shoulder: 55
- forearm bones = 46/52 mm
- height: 43
- weight: 1790-1890.
Fetal fetometry at 33 weeks can be presented in the form of the following table
| BPR | OG | coolant | SJ | PJ | Hip | M. Berts/B. Berts | Shoulder | Beam/Elbow | Weight – 2030-2130 gHeight – 44-45 cm |
| 87 | 316 | 276 | 87 | 88 | 64 | 54/56 | 57 | 47/53 |
Fetometric data at 34 weeks in millimeters
- maximum distance between parietal bones (BPD): 89
- head circumference (OG): 323
- chest diameter (DGrK): 88
- abdominal circumference (AC): 285
- PJ: 91
- SJ: 90
- hip: 66
- shin = 56/57 mm
- shoulder: 59
- forearm bones = 48/55
- height: 46-47 cm
- body weight: 2270-2390.
Fetometry at 36 weeks (mm)
- BPR: 92
- OG: 335
- DGrK: 94
- Coolant: 303
- PJ: 97
- SJ: 96
- hip: 70
- shin bones: 58/60
- shoulder: 61
- forearm bones = 50/57
- height: 49 cm
- body weight: 2750-2860.
Fetometry at 37 weeks
- BPR: 94
- OG: 339
- DGrK: 97
- Coolant: 311
- PJ: 100
- SJ: 98
- hip: 71
- shin: 60/62
- shoulder: 63
- forearm bones = 51/58
- height: 50 cm
- weight: 2970-3090.
The main parameters that are important for the correct assessment of the baby in the first two trimesters are abdominal circumference, biparietal size and thigh length.
After this period, just before childbirth, the chest circumference, abdominal circumference and length of the femur become more important.
What is "norm"
In the photo: 3D ultrasound of a child
In the photo: 3D ultrasound of a child
It is considered normal if your child’s data corresponds to the size of the fetus according to ultrasound weeks, and if it lags behind or exceeds the period calculated by your gynecologist, then by less than 14 days.
That is, this will not yet be considered either a delay or an advance in development. Evaluate yourself, find out what weight you and your husband were born with: maybe just one of you is short, and the child inherited this trait.
It is also normal if the indicators are not on the same line, but have a slight scatter, which occurs because the child grows spasmodically.
If, for example, everything “fits” into the norm, except for the length of the femur and tibia, this does not indicate pathology. Perhaps the child's parents or older relatives do not have long legs.
A situation is considered dangerous when, not for the first time, it is noticeable from fetometry that one of the circles is more or less than 2 lines in comparison with other indicators. This should be considered a health hazard.
For example, if the head circumference increases, this may indicate intrauterine hydrocephalus; if it corresponds less and less to the deadline, this may indicate another brain pathology. In this case, measurement of the baby’s size by ultrasound is supplemented by Doppler measurements, CTG and mandatory dynamic monitoring.
However, making a diagnosis of “Intrauterine growth retardation” or “Hypotrophy” is the responsibility of a joint assessment of ultrasound fetometry parameters by two doctors: an obstetrician-gynecologist and a medical geneticist.
Only these specialists can assess your genetic predisposition, and also, in case of a disappointing diagnosis, will be able to find the causes of this pathology. So, these can include chromosomal abnormalities, bad habits, the age of one or two parents, and an infection acquired in utero by a developing child.
Considering all of the above, it is necessary for an obstetrician-gynecologist to decipher the indicators of this study: the ultrasound doctor only provides him with data in which he indicates what and how different it is from the norm.
Thus, what the table of fetal fetometry indicators represents is averaged data. They are used to determine whether the gestational age calculated by the obstetrician corresponds to that obtained from these data. Using the same parameters, they look at whether the baby’s growth is symmetrical (when everything is 1-2 lines lower or higher), or, conversely, asymmetrically. This allows you to identify some developmental defects in time.
ATTENTION! The information on the site is for reference or popular information only. Correct treatment and prescription of medications can only be carried out by a qualified specialist, taking into account the diagnosis and medical history.
You can always make an ultrasound appointment with an ultrasound doctor in Sochi at the medical ]VegaMed[/anchor], ultrasound prices start from 400 rubles, you can visit an ultrasound doctor on the same day as the clinic has free rooms for receiving patients.
You can make an appointment by calling +7 (862) 295-00-95 We also invite you to follow us on Instagram You can use WhatsAPP Make an appointment without a phone call to the medical center Click here to sign up
Ultrasound and other tests
At 33 weeks of pregnancy, an ultrasound examination is necessary to assess the development of the fetus. The doctor will record the exact dimensions and weight, and note all the existing anatomical features of development. Ultrasound helps to exclude the presence of pathology and developmental anomalies, fetal presentation and entanglement of the umbilical cord
As a rule, the gender of the unborn child has already been determined. If this did not happen before, then certain difficulties may arise now. After all, there is less and less space in the stomach, which means that the child can squeeze his legs and close his genitals.
During an ultrasound, the doctor also evaluates the condition of the placenta, the quantity and quality of amniotic fluid, uteroplacental blood flow, and the degree of maturity of the cervix.
Sometimes the doctor adjusts the already set date of expected birth. If a woman receives any therapy, then after the study it may be changed, because more and more information about the condition of the fetus is becoming available.
Thus, an ultrasound at 33 weeks of pregnancy is an important and extremely informative study that must be done without fail. This diagnostic method often helps doctors make very important decisions, for example, about the need for early delivery. In the vast majority of cases, an ultrasound simply allows you to once again make sure that the pregnancy is proceeding normally and everything is fine with the baby.
Other tests and examinations
At this time, the woman should also visit her gynecologist, donate blood and urine for a general analysis. At the appointment, the doctor will measure the height of the uterine fundus, abdominal volume, blood pressure level, and listen to the fetal heartbeat. The normal height of the uterine fundus is 33 cm (deviations of 1-2 cm are allowed).
In addition, this week the woman gains about 300-550 g in weight. The volume of circulating blood in the body increases. There is already a liter more of it than before the moment of conception.
If there are any deviations during pregnancy, then it is possible to determine the level of hCG (the norm is 2700-78100 mIU/ml), dopplerography, CTG and other studies.
How to prevent stretch marks from appearing
It is difficult to predict their appearance: neither heredity nor the absence of stretch marks in previous pregnancies guarantees that this time too you will manage without them. It is extremely difficult to get rid of stretch marks that have already appeared. Therefore, the best option is prevention. It includes:
- daily systematic body skin care using moisturizers or special creams against stretch marks;
- proper nutrition high in vitamins and minerals, polyunsaturated acids, fiber;
- weight control - do not allow sudden gain;
- wearing a bandage and support underwear;
- light massage of problem areas.
A contrast shower promotes blood circulation and makes tissue more elastic. Exercising during pregnancy will not only help keep your body in good shape, but will also improve the condition of your skin.
Sex
If the doctor does not find any abnormalities, then there should be no reason to refuse intimate relationships. At this time, sex, as before, will bring pleasure to both partners.
Many couples refuse intimacy because they are afraid of harming the baby. Expectant parents may be frightened by an overly large belly or the active movements of the child inside it. You shouldn't be so suspicious.
It is possible that the following tips will help the couple gain courage:
- Penetrations during sexual intercourse should not be too deep and movements should not be too sudden.
- During intimacy, do not put pressure on the stomach. Therefore, it is necessary to choose appropriate poses.
- If discomfort or pain occurs, sexual intercourse should be stopped immediately.
- It is best to have sex with a condom at 33 weeks of pregnancy. The fact is that male sperm contains substances that soften the cervix and prepare it for childbirth. But now it’s too early to go to the maternity hospital, which is why it is best to prevent seminal fluid from entering the vagina.
It is necessary to refuse sex if a woman’s mucus plug has come off, as the risk of infection spreading to the fetus increases.
Good to know
What to do for hemorrhoids in a pregnant woman?
Pregnancy and edema: causes and treatment. What and how much to drink?
How the baby develops inside the belly by week of pregnancy
Pregnancy, swollen legs: what to do? Outdated recommendations and a modern view
Third trimester of pregnancy: how to relieve swelling and prepare for childbirth
Diuretics during pregnancy
All texts for pages about mother and baby were kindly provided by RAMA Publishing - these are chapters from the book by Svetlana Klaas “Your Favorite Little Man from Conception to Birth”, reviewer Irina Nikolaevna Kononova, Candidate of Medical Sciences, Associate Professor of the Department of Obstetrics and Gynecology of the Ural State Medical Academy (Ekaterinburg).
What kind of discharge can there be at 33 weeks of pregnancy?
A deviation from the norm is the appearance of discharge with blood when it turns brown, red or scarlet. Blood in the discharge may indicate placental abruption, vaginal injury, or the onset of premature labor. All these situations are extremely dangerous for the woman and the fetus.
You should also go to an appointment immediately if flakes, foam, or an unpleasant odor appear in the discharge. Green or yellow discharge is considered abnormal.
Watery and clear discharge may indicate a water leak. This is dangerous and requires hospitalization. When your waters completely break, you should also immediately go to the maternity hospital, as labor will begin soon.
If a woman has not previously taken a smear test to determine infectious diseases, then she must do so now. After all, the risk of infection is almost always present. Moreover, thrush often develops during pregnancy, which also requires specific treatment. There is no need to be afraid of therapy. Thrush is treated with antifungal suppositories, which are not contraindicated for women at this time. But you can’t prescribe medications for yourself.
Sometimes at this stage of pregnancy the mucus plug comes off. It is presented in a lump, the volume of which can fit in 2 tablespoons. Sometimes the cork comes off in parts, and sometimes all at once. Its color may be cream or streaked with blood. The removal of the plug is considered a harbinger of impending labor, so you must inform your doctor about this.
A woman should carefully examine her discharge; those that have a uniform consistency, transparent, light or whitish tint are considered normal. The discharge should not have an unpleasant odor. In addition, the genitals at this time are supplied with blood better than usual. Therefore, the volume of discharge may also increase, but not much. There is no need to worry about this. =
What to do if the membranes rupture?
RUPTURE of the amniotic sac always occurs unexpectedly and WITHOUT PAIN.
If amniotic fluid leaks or is suspected of leaking, you should NOTE THE TIME of the incident (“note the time”), PLACE a clean SHEET between your legs, take a horizontal position (LIE) and CALL your doctor.
If it is impossible to discuss the situation with your doctor, you should immediately CALL an ambulance.
This algorithm of actions in case of rupture of membranes is the only correct one, since after 12 hours the probability (risk) of infection of the fetus and the pregnant woman increases significantly, and the need arises to resolve the issue of the method of delivery (birth).
Considering that RUPTURE of the amniotic sac always occurs UNEXPECTEDLY, a pregnant woman must constantly CARRY with her an outpatient (exchange) card, a copy of her passport, and an insurance policy. YOU CAN have electronic COPIES of your exchange card, passport, insurance policy in your PHONE.
CHECK that your doctor's telephone number, obstetric hospital telephone number and emergency medical service telephone number are available in your phone book (in your phone).
If a critical situation arises, DO NOT rely only on yourself - LOUDLY, thinking about the child and WITHOUT HESITATION, seek help from others, warning about your pregnancy.
Starting from 24 weeks of pregnancy, it is very wise to form an “ALARM SUITCASE”. A complete list of things for the maternity hospital in detail...
The threat of miscarriage, the threat of premature birth, rupture of amniotic fluid are contraindications to driving: call an ambulance, DO NOT RISK the health of the baby, your life and the well-being of your family!
Causes of pain
Pain can occur at any stage of pregnancy, but it is important to correctly determine its source:
- Pain during urination may indicate a genitourinary infection. Body temperature may also increase, and sometimes unusual discharge from the genital tract may appear.
- Hemorrhoids are indicated by pain in the rectal area and the appearance of blood stains on underwear.
- Headaches indicate a lack of rest, excessive fatigue, overheating of the body or oxygen starvation. Often, to get rid of it, you just need to lie down to rest or take a walk in the fresh air.
- Due to increased weight, pain may appear in the back, legs, and lumbar region. To reduce them, you need to carefully monitor your posture, wear a prenatal bandage, and choose comfortable shoes. It is necessary to avoid prolonged physical activity, do not lie on your back, do not sit on chairs without a back.
- Lumbar pain bothers almost all pregnant women. They are associated with pressure from the enlarged uterus on the sciatic nerve. The pain intensifies if the woman lies on her back.
- Pain in the knee joints occurs due to increased load on them. Cool baths help reduce pain in the lower extremities. After this procedure, it is good to raise your legs to some height.
- Pain in the pelvic area and pubic area appears due to the fact that the woman’s body is gradually preparing for the process of childbirth. The pelvic bones slowly move apart, which causes discomfort. Swimming, wearing a bandage, and taking a bath help reduce their severity.
- Pain in the hypochondrium occurs due to the fact that the child has grown up and began to kick the mother from the inside with greater force. Noticeable fetal movements are often associated with an uncomfortable position that the woman takes, or with external pressure on the uterus. As the belly lowers before giving birth, the pain in this area will become less intense.
In any case, you should report any pain to your doctor. Sometimes at 33 weeks of pregnancy, training contractions occur, so a woman may feel a slight painful tension in the lower abdomen. This is normal, provided that the intensity of contractions does not intensify. Otherwise, you need to call an ambulance.
What happens to the belly at 33 weeks of pregnancy?
In addition to the fact that a woman will experience pain, she may experience heartburn. By this time it intensifies significantly. There are two reasons: the pressure of the uterus on the stomach and physiological changes in the body that provoke an increase in the acidity of gastric juice.
Another unpleasant sensation that occurs at 33 weeks of pregnancy is shortness of breath. It should decrease as the baby descends a little. Until this happens, you need to reduce your physical activity and look for comfortable positions.
Itching of the skin of the abdomen is another common complaint of expectant mothers. It can be reduced by applying moisturizer to your stomach. It’s good to rub olive or almond oil into your skin immediately after a shower.
By this time, the stomach rises very high, which will cause some discomfort. But there is no need to worry about this, because in the coming weeks it will go down and it will become easier to breathe.
Sometimes a woman is surprised to notice rhythmic twitching of the abdomen. This happens when the baby starts to hiccup. And this happens quite often.
You also need to be especially careful, because the stomach has become heavier and pulls the woman forward. Falls at this time are very dangerous.
What happens in the tummy? Pain in the hands, baby movements and the benefits of omega-3:
Weight
You need to monitor your weight carefully. This is important, since a sharp gain in body weight, especially in the third trimester, may indicate gestosis.
It is important to follow a diet, not to overeat, and limit the consumption of sweets. You need to reduce calories through baked goods and confectionery products, fried and fatty foods.
Sometimes a woman gains weight due to edema. To avoid retaining excess fluid in the body, it is necessary to limit salt intake. Sometimes the doctor advises to give it up altogether.
From the moment of pregnancy, a woman’s weight increases by 9-13.5 kg. These are averages that may vary slightly in one direction or another, but should remain within normal limits.
Nutrition
Nutrition for a pregnant woman at 33 weeks
Proper nutrition is one of the important elements of pregnancy well-being. A woman should follow simple rules to avoid discomfort from the gastrointestinal tract, obtain the necessary amount of nutrients necessary for the development of the fetus and maintain the health of the mother. The daily diet should ideally include:
- meat, offal or fish (preferably sea);
- dairy products (cottage cheese, cheese, yogurt, kefir);
- porridge (buckwheat, rice, oatmeal, etc.);
- chicken eggs (1-2 per day);
- vegetables and fruits, raw and boiled (carrots, pumpkin, broccoli, asparagus, bananas, apples);
- dried fruits and nuts (dried apricots, prunes, almonds, walnuts);
- berries (seasonal).
In order for the digestion process to proceed normally, it is advisable to consume these foods in compliance with some recommendations:
- eat 5-6 times a day in small portions;
- stop eating before you feel full;
- be guided by the principle that one dish per meal;
- do not eat 2-3 hours before bedtime. If there is an urgent need to stop hunger with yogurt or fruit;
- observe the drinking regime. Drink at least 1.5 liters of fluid per day, unless otherwise prescribed by the gynecologist;
- exclude all unhealthy foods from the diet, including processed foods, smoked meats, pickles, and dried meats;
- do not eat fast food, sushi;
- refuse strong tea and coffee, unless otherwise prescribed by the gynecologist;
- Reduce the amount of salt used for cooking to a minimum.
Vitamins
Taking multivitamins and dietary supplements during pregnancy should be prescribed exclusively by a doctor. Despite all the apparent benefits of dietary supplements, it should be borne in mind that an excessive amount of a certain beneficial substance not only does not bring benefit, but can also cause harm. The prescription of additional vitamins should be based on the woman’s tests, the characteristics of the region and other indicators.
Feelings of the expectant mother
By this time, the woman begins to feel clumsy and clumsy. Sometimes there is a feeling of fatigue and helplessness. After all, it is often impossible to even get a good night’s sleep - the enlarged belly does not allow you to find a comfortable position and makes breathing difficult. Urination also becomes more frequent, because the uterus puts pressure on the bladder, so there is a desire to empty it even if it is partially full. To reduce the number of nighttime trips to the toilet, you need to drink less fluid in the evening.
If a woman's blood pressure rises, this may be a sign of gestosis. Therefore, you should definitely report such surges to your doctor. In general, high blood pressure is dangerous for a pregnant woman.
Here are some more common complaints of all pregnant women at 33 weeks:
- Ear congestion;
- Bleeding gums;
- Nosebleeds;
- Numbness of the limbs;
- Leg cramps;
- Protruding navel.
Of course, it is not easy to withstand such a load on the body, but you need to remember that it is temporary. Very soon a new person will be born, who already needs care and love. Therefore, despite all these minor troubles, you need to try to relax as much as possible and get as much rest as possible. Firstly, the upcoming birth is far from an easy process. Secondly, the baby will take a lot of strength from the mother, not only physical, but emotional. Now the woman has very little time left that she can devote only to herself.
Interesting Facts
| Options | Indications |
| Time from conception | 31 weeks |
| Period by month | 33 weeks |
| What month | 8 |
| Dimensions and weight of the fetus | 440 mm, 1900 g |
| Uterus dimensions | VDM - 31-33 cm |
| Pregnant weight | Gain from the beginning of pregnancy is 10-12 kg; over the last week 400-500 g |
Your baby is the size of
Mexican turnip
440 mm Size
1900 g Weight
You are probably finding it increasingly difficult to feel comfortable right now. You may get tired quickly, suffer from insomnia, and experience frequent pain in your legs and lower back. Be patient! There is very little time left to wait. Very soon you will have a beautiful baby, and unpleasant symptoms will be a thing of the past. Now you can help yourself by tuning into positive emotions and listening to the sensations in your body. Let's find out what happens to the mother and fetus during this period, but let's start with the “arithmetic”.
What to do if labor begins?
If labor occurs at 33 weeks of pregnancy, it is premature and the baby will be premature. However, at this stage the baby can breathe independently, which is very important. This greatly facilitates the process of nursing and allows the child to grow up healthy.
Most often, premature birth can be avoided, but a woman must be extremely attentive to her health and herself. It happens that labor begins, and nothing can be done about it. If this happens, then you need to remain calm and completely trust the doctors. In some cases, labor at this stage is induced artificially, for medical reasons.
When there are no prerequisites for premature birth, you need to prepare for the upcoming trip to the maternity hospital. The bag must be packed, as well as the package of documents.
Signs of ruptured membranes
The amniotic sac may rupture (rupture) in the CENTER just above the cervix. In the event of a central rupture of the amniotic sac, the amniotic fluid will come out in a hot stream (“gushing out like a bucket”), the waters will break.
In some cases, rupture of the membranes occurs above the internal os (opening) of the cervical canal. In the case of a high lateral rupture of the membranes, a SIGN OF RUPTURE of the membranes is the leakage of amniotic fluid in small portions (water leakage).
Often a pregnant woman feels that the pad or underwear has become wet, but cannot understand the reason - it is heavy discharge or rupture of water, leakage of amniotic fluid.
Increased vaginal discharge when coughing (“COUGH TEST”) is a sign of high rupture of the membranes and leakage of amniotic fluid.
What can affect the fetus?
The baby is reliably protected in the womb by the placenta and membranes. However, there are many factors that can affect its growth and development.
The nature of a woman’s diet is of no small importance. When she eats little and low-quality food, the child will not gain weight well. There may even be developmental delays.
Another negative factor that can affect a child’s health is radiation exposure. The larger the dose received, the more severe the consequences. Even fetal death or severe developmental defects cannot be ruled out. Small doses of radiation damage the placenta and impair its protective properties.
It is imperative to avoid any pressure on the abdomen, including falls. This can lead to rupture of the membranes, premature labor, or placental abruption.
It is important to completely exclude alcohol, nicotine, and drugs from entering the body. A woman should not come into contact with paint and varnish products, aggressive chemicals, and insecticides.
Separately, it is necessary to note the intake of medications. They should only be prescribed by a doctor. At such a late date, many drugs are already permitted, for example, NSAIDs, drugs for topical use, but self-medication is in any case unacceptable.
Complications at 33 weeks of pregnancy
At this stage, it is necessary to take care of the prevention of rickets in the child. To do this, a woman must receive a sufficient amount of vitamin D.
If not enough calcium enters the mother’s body, it begins to be washed out of the bones, and for this reason the woman develops hemorrhoids, varicose veins and calf cramps.
A significant increase in weight will lead to the fact that after childbirth a woman will become obese with all the ensuing consequences: metabolic disorders and diabetes.
A very serious complication of pregnancy is eclampsia. Doctors do not know how to prevent its development and how to cure it. Eclampsia begins with gestosis or preeclampsia. Early signs of this condition: increased blood pressure, increased edema, a jump in protein levels in the urine. Eclampsia itself is characterized by cerebral edema, convulsions and subsequent death of the woman and/or child.
The only way to save the life of the woman and child is an emergency caesarean section.
Why sing lullabies to your baby in your belly?
What other actions of mom and dad help communicate with the Baby and have an unconditional developmental effect?
Lullabies. There are two well-known and beloved ones - “Sleep, my joy, go to sleep” and “Tired toys are sleeping.” These melodic, drawn-out songs have a good calming and relaxing effect. Warm, kind, sweet words of lullabies familiar to us from childhood, performed by mom or dad, are filled with tenderness, love and care. And this strong connection - pleasant emotions and daily lullabies - will lead to the fact that the Baby will begin to recognize songs even before birth.
Let us remind you that the presence of hearing (or lack thereof in you or your husband) does not play a role: there are cases when two-year-old children asked their mothers with perfect pitch not to sing, because “you don’t know how.” Of course, the point here is not in performing skills, but in the feeling and attitude with which the songs are sung towards the Kid.
There is another version of lullabies, which is often liked by dads, since it does not require memorizing words. Mothers resort to it after the birth of the Baby, when the above-mentioned lullabies “with words” have already been sung, and the child does not want to calm down. These are lullabies with the beginning “Bay-bye, bye-bye, my son/my daughter go to sleep.” Apart from the line about a top that will bite the side, few people remember anything from this lullaby. But you can insert any words into it according to the principle “what I see is what I sing about.” It was this method that Shurik used when rocking Helen in the famous “Operation Y”. The song turns out to be almost endless, does not require intellectual effort - only calmness and love for the Baby.
Singing any other (non-lullaby) songs to suit your mood, especially when accompanied by any musical instrument: guitar, piano, harmonica, accordion, etc. By singing your favorite songs from the heart, you instill in your child a special relationship with them. And most likely, these songs will eventually end up in the repertoire of your son or daughter.
Reading children's books out loud - in any volume, that is, as far as the parent's passion is enough. Unlike developmental activities, such a pastime can be unsystematic, that is, depending on the mood, and is aimed at dialogue with the Baby, the desire to be together, on the same emotional wavelength.
A visit to the zoo and circus - traditional places that children like so much. Different sounds and voices combined with the emotions of mom and dad and their comments “for the Baby” are a great way to spend time together.