How does panaritium occur?
To start the pathological process, a tiny wound on the finger is enough - for example, from an injection or splinter.
Small wounds heal quickly, but the infection remains inside and continues to multiply. In this case, the human body recognizes the danger and begins to produce phagocytes (leukocytes). The structure of the connective tissue of the hands is specific - it forms vertical fascial partitions. They go from the periosteum to the skin, dividing into vertical cells. This keeps the infection from spreading to other areas, but creates ideal conditions for an abscess to form.
When swelling occurs in such partitions and pressure in the tissues increases, debilitating pain appears. If panaritium is not treated, the infection breaks into neighboring cells, spreading to the joints and tendons.
Complications
Complications of panaritium include:
- Blood poisoning. In this case, purulent foci form in other internal organs, and DIC syndrome develops. Sepsis often ends in the death of the patient.
- Purulent tendovaginitis with damage to the synovial bursae of the hands and forearm. This complication most often results from panaritium concentrated on the 1st or 5th finger of the hand.
- Phlegmon of the hand.
- Osteomyelitis of the metacarpal and carpal bones.
- Vascular thrombosis with tissue necrosis, periphlebitis and thrombophlebitis of the extremities.
- Purulent lymphadenitis. Sometimes it is lymphadenitis and general intoxication of the body that become the first symptoms of panaritium.
- Contractures of the fingers. This complication develops against the background of the articular or tendon form of the disease.
Types of felon
Panaritium on the fingers is more common than on the feet. It can develop in a person of any age, both men and women. However, most often the disease affects patients 20-50 years old. In children, severe forms of panaritium are rarely diagnosed; in them, only the periungual fold (paronychia) is usually inflamed.
Classification of panaritiums:
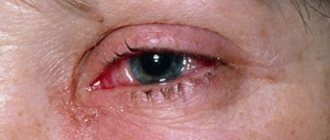
- Periungual form or paronychia. The painful process engulfs the edge of the nail plate and moves to the periungual fold. The reason for the occurrence of such panaritium is microtrauma of the tissues adjacent to the nail, almost imperceptible cuts - for example, as a result of an unprofessional manicure.
- Subcutaneous panaritium. Suppuration forms on the reverse side of the injury; exudate accumulates in the subcutaneous purulent bladder, often with bloody impurities. It is noteworthy that such an abscess does not hurt; a person may only be bothered by a slight burning sensation. The skin around the felon turns red. If the subcutaneous bladder increases in volume, this means that the disease is progressing. It is this form of the disease that is easier to treat than others. But due to the structure of soft tissues, inflammation quickly spreads to the joints and tendons.
- Subungual panaritium. The source of inflammation is located under the nail plate, in the soft tissues. The infection can be caused by a nail injury or splinter.
- Bone panaritium. In this case, the bone tissue of the finger becomes inflamed. Such inflammation can occur after deep injuries and fractures.
- Articular form or purulent arthritis. The joint between the phalanges is affected, the fingers acquire a spindle-shaped shape and any movement becomes painful.
- Combined articular-osseous form. Inflammation affects not only the joint, but also the bone.
- Tendon form. The most difficult and painful type of panaritium. In addition to the bone and joint, the inflammation spreads to the tendons, the affected area swells and, due to severe pain, it becomes almost impossible to move the fingers and limbs.
Attention! Identifying subcutaneous panaritium is especially difficult in people with thick, insensitive skin. The first signs of inflammation begin to appear 5-7 days after the injury, when a person hardly pays attention to the first unpleasant sensations. Without treatment, inflammation affects the tendons, joints and phalanges, leading to a complicated form of the disease.
Reviews
Irina: Elon ointment saves me - it’s so green, it smells like rosemary. It is better to start treatment as soon as symptoms of the sore appear. I lubricate the sore spot with ointment, apply a bandage and leave it overnight. Elon draws out pus well and relieves inflammation. The drug also helps relieve throbbing pain.
Maria: I once cut a hangnail, it became inflamed, but I didn’t dare go to the doctor. And then they told me that without treatment you could even lose a finger, it’s such a dangerous sore. The surgeon administered anesthesia before the autopsy, and it didn’t hurt me. After taking antibiotics. Now I try to be more careful when doing manicures.
Alla: I had a panaritium on my little finger. As soon as my finger started to swell and hurt, I started making salt lotions, wrapped it in a bandage and put a finger guard on top. I wore it without taking it off until the bandage dried out. Then she wet it again, tied it, and did this for 3 days in a row. It didn’t get to the point of suppuration, the finger began to heal.
It is necessary to treat panaritium in a timely manner. Folk remedies can only help at the initial stage of the disease, with superficial types of pathology. Deep tissue damage to the finger requires qualified treatment, most often surgical intervention. The pathological process cannot be started, otherwise the consequences will be the most severe.
Symptoms of felon
How the disease will progress depends on the pathogen, the type of inflammation and the nature of tissue damage. However, different types of panaritium still have common features. These include:
- swelling of the fingers on the back of the hand;
- redness and feeling of skin tension;
- limited movement, awkwardness, stiffness;
- discomfort or pain: from tingling to sharp pulsations (depending on the depth of the lesion).
In severe cases of panaritium, the patient will suffer from high fever, intoxication, and weakness.
If the causative agent of inflammation is staphylococcus, there may not be a clear clinical picture with pain and fever. This is the danger of such felon: in the presence of staphylococcus, decay processes develop very quickly and a necrotic focus develops. Therefore, be careful - severe swelling of the hand, accompanied by weakness, drowsiness and lack of appetite, may indicate the destructive activity of staphylococcus. See a doctor immediately!
If anaerobic flora is working inside the panaritium, the hand will not only be swollen, but also purple or even cyanotic. With this type of lesion, tissue necrosis also develops very quickly.
Classification
The classification of panaritium is based on the depth and localization of the purulent-inflammatory process. But the type of pathogen does not play a key role; the nature of the flora is indicated in the diagnosis as a clarification.
The disease can have several clinical forms:
- cutaneous panaritium;
- subcutaneous;
- periungual, also called paronychia;
- subungual;
- articular;
- bone;
- tendon panaritium;
- pandactylitis (damage to all tissues of the finger).
Articular, bone and tendon panaritium belong to the deep form of the disease, as does pandactylitis. And all other varieties are superficial; they are the ones diagnosed most often.
a - cutaneous; b - paronychia; c - subungual; g - subcutaneous; d - tendon; e - bone; g - articular; h - osteoarticular; and - pandactylitis
Some experts also call panaritium purulent-inflammatory diseases of the hand that affect the palm, dorsum, interdigital spaces and subgaleal formations. But it is more correct to classify them as phlegmons. Inflammation of the dorsal surfaces of the proximal and middle phalanges of the fingers is also usually not considered felon, except in cases of secondary damage to pandactylitis.
Stages of the disease
The initial stage of the disease is called serous-infiltrative. 2-3 days after the onset of the lesion, it passes into the purulent-necrotic stage.
The serous-infiltrative stage is characterized by:
- moderate pain;
- exacerbation of unpleasant sensations when the hand is lowered down;
- redness on the back of the hand;
- swelling of fingers and hands;
- the affected finger is difficult to bend;
- body temperature fluctuates between 37-37.5 degrees;
- satisfactory health.
When the disease enters the purulent-necrotic stage, the symptoms are pronounced:
- throbbing or jerking pain in the affected finger;
- the patient is forced to keep the hand raised upward;
- paler spots are visible in the center of the reddened areas of the skin;
- the veins of the hand are dilated;
- fever, general intoxication;
- The blood test shows a high ESR and an increased number of leukocytes.
If you use folk remedies, which ones?
- Salt bath: dissolve 100 g of salt in a liter of water, soak your finger for 30 minutes.
- Compresses: bake onions until soft, cut in half, apply to the affected finger, wrap and hold for 4 hours.
- Compress: peel the aloe leaves, apply the pulp to your finger and leave for up to 6 hours. You can do this procedure at night.
- At the pharmacy you can buy special ointments that help before the pus appears and after it opens.
Diet is not important in the treatment of this disease. You can only focus on absorbing plenty of vitamins through tablets and food to strengthen your immune system.
go to top
Risk factors
The inflammatory process occurs when pathogenic microorganisms enter the wound. They may be:
- Staphylococcus aureus;
- beta-hemolytic streptococcus;
- enterococcus;
- Escherichia coli or Pseudomonas aeruginosa;
- fungal infection.
Often the cause of inflammation is a combination of several types of aerobic and anaerobic microorganisms.
People can open the gates of infection due to carelessness or bad habits. For example, microtrauma can be caused by the habit of biting nails or picking off hangnails, or getting a manicure done by an insufficiently conscientious specialist.
Factors in which you need to be extremely careful and protect your fingers from microtraumas:
- fungal infection:
- dermatosis complicated by bacterial and fungal microflora;
- nail damage due to psoriasis or eczema;
- diabetes mellitus (especially its decompensated form);
- damage to arteries and veins - it leads to disruption of blood microcirculation and disruption of tissue trophism;
- taking immunosuppressants or glucocorticoids;
- old age, vitamin deficiencies, exhaustion. hypoproteinemia;
- frequent contact with caustic chemicals;
- frequent exposure to high humidity conditions;
- work involves exposure to vibration;
- Raynaud's syndrome.
Causes
What are the reasons for the development of felon? Only two components play an important role here:
- An open wound, better when it is punctured. If a person gets burned, gets a splinter, injures the hand, an open wound forms, cracks in the skin, then an infection can easily get inside - the second reason for the development of panaritium. This often happens during physical work, when preparing food, manicure, pedicure, etc.
- Infection. Staphylococci are common, less often - streptococci, Pseudomonas aeruginosa, Proteus and other microorganisms. They penetrate into an open wound located on the hands or feet. The deeper it is, the greater the risk of developing the disease.
The most interesting thing is that not only the reasons described above become factors in the development of panaritium. There are other situations:
- Skin contamination.
- Frequent hypothermia.
- Exposure of finger skin to various metals and chemicals.
- Ingrown nail.
- Vibration.
- Diabetes.
- Foot fungus.
Blood circulation, tissue nutrition and local immunity should be disrupted in the area. When there is no immunity, then it is easier for microorganisms to penetrate the wound and begin the inflammatory process.
On the feet, panaritium develops due to uncomfortable shoes, constant friction, punctures, etc.
go to top
Diagnosis of felon
A traumatologist, orthopedist and infectious disease specialist can make a diagnosis. After examination and history collection, the doctor will prescribe:
- clinical urine analysis;
- clinical blood test;
- bacteriological culture from the affected area:
- radiography.
To clarify the shape and location of the inflammation, the doctor will carefully palpate the sore spot with a button probe.
Since articular panaritium is more difficult to identify, it may be necessary to take comparative radiographs of the finger of the same name on the right and left hands. Based on the results of the examination, the doctor will decide how to treat panaritium.
Forecast
With adequate/timely treatment, primary articular felons result in complete recovery with preservation of the functions of the affected finger. With inadequate/untimely treatment, the prognosis is less favorable, especially with secondary felons (with the spread of suppuration from neighboring tissues) in the form of the formation of deformities of the phalanges / fingers , ankylosis with disruption of their functions, and in some cases, amputation of the phalanges and fingers.
Treatment of felon
If the patient seeks medical help in a timely manner, felon can be successfully treated using conservative treatment methods: local and systemic use of antibiotics, analgesics, UHF therapy, electrophoresis. The main thing is to ensure resorption of the infiltrate.
At this stage of treatment, additional procedures are effective: baths with saline solution or compresses on the site of inflammation, the use of ichthyol ointment or Vishnevsky ointment. Depending on the area of the lesion, you can use ointments and lotions with antibiotics, antiseptics, and applications with dimexide.
To relieve pain, you will be offered non-steroidal anti-inflammatory drugs.
If the inflammation has developed into purulent-necrotic, the painful cavity must be promptly opened, drained and washed with antiseptic solutions. During intensive treatment, a bandage and splint will be applied to the finger. Most likely, the doctor will prescribe a course of antibacterial drugs, depending on the results of a sensitivity test to one or another type of antibiotic.
Sources
- Felon, Naomi M. Nardi; Timothy J. Schaefer.Updated: December 19, 2021. —[https://www.ncbi.nlm.nih.gov/books/NBK430933/](https://www.ncbi.nlm.nih.gov/books/ NBK430933/)
- Hand Infections Clinical Presentation, updated: Jun 06, 2018, Author: Eden Kim, DO; Chief Editor: Jeter (Jay) Pritchard Taylor —[https://emedicine.medscape.com/article/783011-clinical](https://emedicine.medscape.com/article/783011-clinical)
- Common Acute Hand Infections, American Family Physician - [https://www.aafp.org/afp/2003/1201/p2167.html](https://www.aafp.org/afp/2003/1201/p2167.html )
- Paronychia: acute and chronic (nail disease, felon/whitlow), Avner Shemer, C. Ralph Daniel -[https://www.clinicaladvisor.com/dermatology/paronychia-acute-and-chronic-nail-disease-felonwhitlow/article /590255/] (https://www.clinicaladvisor.com/dermatology/paronychia-acute-and-chronic-nail-disease-felonwhitlow/article/590255/) 5.Paronychia Treatment & Management, Updated: Oct 22, 2021, Author: Elizabeth M Billingsley, MD - [https://emedicine.medscape.com/article/1106062-treatment#d12] (https://emedicine.medscape.com/article/1106062-treatment#d12)
- Valery A. Privalov, Ivan V. Krochek. Diode laser treatment for osteal and osteoarticular panaritium [Electronic resource] // Therapeutic Laser Applications and Laser-Tissue Interactions II, 2005.
- MAX SAEGESSER. DAS PANARITIUM [Electronic resource] // VEHL. G VON JULIUS SPRINGER, 1938.
- Ligonenko OV FOR INDEPENDENT WORK OF THE STUDENT IN TIME FOR PREPARATION TO THE PRACTICAL STUDY [Electronic resource] // Department general surgery with care of the patient, 2021.
- Marijke J. Molegraaf, Alexander G. J. van Marle, L. N. L. Tseng. H. influenza Panaritium tendineum. A Rare Pathogen [Electronic resource] // Article in Hand, December 2009.
Prevention panarization
It is not difficult to prevent the appearance of panaritium. To do this, it is important to follow the following rules:
- wear protective gloves when working;
- observe safety precautions at work and at home;
- immediately treat any skin damage with antiseptics, including splinter injections and hangnails;
- cover injured areas with a protective plaster.
- ensure that manicure tools are sterile;
- Avoid prolonged exposure to water - it weakens the protective qualities of the skin.