Reactive arthritis poses a threat to the younger generation and can even affect infants. It is one of the acute spondyloarthropathies, i.e., it is an acute inflammatory process that spreads to the spine, ligaments, various organs and skin. Reactive arthritis mainly affects peripheral joints: knees, hips, necks, interphalangeal joints of the hands and feet, wrists and others. In rare cases, it can lead to inflammation of the aorta, kidneys, pleurisy, damage to the nervous system, even meningoencephalitis.
What is reactive arthritis (ReA)
The term “reactive arthritis” was first used more than 50 years ago to name arthritis that develops after yersiniosis in the absence of infectious agents in the joints. But after a few years, this name began to be associated with certain infections of the gastrointestinal tract, genitourinary organs and nasopharynx.
Currently, reactive arthritis is considered to be non-purulent inflammation of the joints, developing no later than 6 to 8 weeks after a urogenital, intestinal or nasopharyngeal infection. ICD-10 code M02.
Young men aged 17–40 years are more likely to get sick after suffering from sexually transmitted infections (women get sick much less often). In children, adolescents, as well as people of any age and gender, reactive arthritis can develop after intestinal infections, as well as infections of the nasopharynx.
The prevalence of ReA in our country among adults is about 43 per 100,000 population, among children - 99, among adolescents - 172. The incidence is growing, which is largely due to genetic predisposition, asymptomatic infections and untimely administration of adequate treatment.
There is also Reiter's syndrome, which develops after a urogenital infection and manifests itself in the form of three main symptoms: arthritis, conjunctivitis and urethritis.
The first signs and symptoms of sepsis
Identifying the first signs of sepsis can be difficult, even for specialists. This is due to the fact that, firstly, this syndrome develops against the background of an existing pathology, which can have a wide variety of symptoms, and secondly, in the presence of immunodeficiency, the clinical picture can be erased. However, there are some symptoms that suggest the onset of sepsis:
- Increase or decrease in body temperature - above 38 and below 36 degrees.
- Pressure drop below operating value.
- Increased heart rate.
- Increased frequency of breathing movements (shortness of breath).
- Decreased amount of urine excreted.
- General weakness, exhaustion.
- Impaired consciousness or behavior.
Particular attention is paid to the occurrence of these signs in chronic patients, in the presence of leukopenia, cancer, and in patients who have undergone trauma or surgery. If at least 2-3 of these symptoms occur, you should immediately contact your doctor.
Causes of the disease
The main causes of reactive arthritis are past infection and genetic predisposition. Infections that can cause ReA include:
- urogenital form of ReA
– chlymydia, ureaplasmosis, mycoplasmosis; - intestinal form of ReA
– shigenellosis (dysentery), salmonellosis, yersiniosis, intestinal infection caused by Escherichia coli; - nasopharyngeal form
– previous nasopharyngeal infections caused by staphylococcal, streptococcal and other infections.
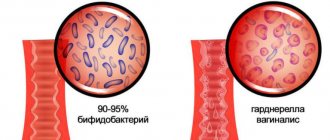
A previous infection is a trigger (triggering factor) that starts a chain of immuno-allergic and inflammatory reactions. This occurs predominantly in genetically predisposed individuals who have the HLA-B27 antigen in their body, which causes an imbalance in the immune system, which leads to increased formation of prostaglandins and cytokines - biologically active substances that cause inflammation.
A long-term inflammatory process is also supported by incompletely removed infectious pathogens and the appearance of antibodies to them. Reactive arthritis caused by urogenital infection (chlamydia, mycoplasma, ureaplasma), which penetrates cells and remains viable for a long time, takes a particularly long time. Failures in the immune system cause allergic and autoimmune (allergy to the body's own tissues) processes, which also support long-term inflammation.
Symptoms of reactive arthritis
Regardless of the cause of the disease, reactive arthritis develops in the same way. By the time the first symptoms of reactive arthritis appear, all manifestations of the trigger infection end or go unnoticed.
Pain, swelling and redness over the affected joint are some of the first symptoms of reactive arthritis.
The first signs of ReA
The disease begins 3 to 30 days (sometimes more) after the infection, acutely with an increase in body temperature, headache, malaise, and the appearance of an inflammatory process in the joints. More often one or more asymmetrically located joints of the lower extremities are affected. Most often these are the knee, ankle and toe joints.
The skin and subcutaneous tissue over the affected joint are red, swollen, and painful. Sometimes pain immediately appears in the lower back - a sign of damage to the sacroiliac joints and joints of the spine. When the first signs of joint inflammation appear, you should consult a doctor. The Paramita clinic will definitely help you.
Obvious symptoms
Reactive arthritis can occur in the form of:
- acute inflammatory process
– up to 3 months; - subacute
– for 3 – 6 months; - protracted
– 6 – 12 months; - chronic
– more than 12 months; - recurrent
– with relapses and remissions.
In addition to the symptoms of reactive arthritis with pain and dysfunction of the affected joints, damage to periarticular tissues - ligaments, tendons, periarticular capsules (enthesitis) is also characteristic. Particularly characteristic is damage to the heel (subcalcaneal bursitis), accompanied by severe pain and inflammation of the periarticular tissues, as well as the 1st toe with redness and swelling of the tissues - “sausage toe”. Such symptoms can completely disrupt the function of the lower extremities - it becomes impossible to move due to pain.
ReA of urogenital origin is often combined with long-term urethritis in men or cervicitis in women, as well as eye damage (Reiter's syndrome). Eye damage can occur in the form of mild conjunctivitis, but in some cases the deeper membranes of the eye are also affected.
Sometimes with reactive arthritis, psoriasis-like rashes appear on the skin, palms and soles, as well as psoriatic-like lesions on the nails. Painless erosions appear on the oral mucosa. There may also be enlargement of the lymph nodes in the groin area.
Dangerous symptoms
The most dangerous is reactive arthritis associated with urogenital infection. This form of the disease is prone to a long-term relapsing course followed by the formation of a rheumatoid-like course. Therefore, it is very important to promptly and adequately treat arthritis.
YOU can call us: 8 (8452) 98-84-68 and +7-967-500-8468 or
Reactive arthritis is an inflammatory disease affecting the joints that develops after suffering certain infections (genitourinary, intestinal, nasopharyngeal).
The disease belongs to the group of seronegative spondyloarthritis. In most cases it is associated with acute or persistent intestinal (caused by Enterobacteriaceae) or urogenital chlamydial infection, but can also be associated with respiratory tract infections caused by mycoplasmas and chlamydia. There is evidence of a possible connection with some parasitic diseases.
A complex of symptoms including arthritis, conjunctivitis, urethritis or cervicitis, colitis and characteristic skin lesions is called Reiter's syndrome.
History The term “reactive arthritis” was first introduced by Finnish scientists K. Aho, K. Sievers and R. Ahvonen, who in 1969 described the occurrence of arthritis in enterocolitis caused by Yersinia. At the same time, the “reactive”, sterile nature of arthritis was emphasized and it was believed that there were no infectious agents and their antigens in the synovial fluid and synovial membrane.
Later, with the development of imaging and laboratory diagnostic methods, intracellular inclusions of Chlamydia trachomatis, microbial DNA and RNA fragments, as well as circulating immune complexes were discovered in the joint environment of patients. Later it was found that normally the joint is not sterile, and various microorganisms are often present in it.
As we studied, a close relationship between reactive arthritis and the HLA-B27 antigen was revealed. It has been found that antibodies to a number of microorganisms cross-react with HLA-B27 and can damage the body's own tissues during the immune response.
Etiology Today, the ability to cause reactive arthritis has been identified in many microorganisms:
Pathogens of intestinal infections: Yersinia enterocolitica Yersinia pseudotuberculosis Salmonella enteritidis Salmonella typhimurium Shigella flexneri Shigella sonnei Shigella Newcastle Campylobacter jejuni Clostridium difficile Pathogens of urogenital infections: Chlamydia trachomatis Pathogens of respiratory tract infections: Mycoplasma pneumoniae Chlamydophila pneumoniae
Epidemiology After a chlamydial urogenital infection, reactive arthritis develops in 1 - 3% of cases. After intestinal - in 1.5 - 4% of cases. People aged 20 to 40 years old, most often men, become ill. Urogenital reactive arthritis occurs in men 20 times more often than in women, enterocolitic arthritis occurs 10 times more often.
There is evidence that carriers of the HLA-B27 antigen develop arthritis 50 times more often after an intestinal or chlamydial infection than those who do not have this antigen.
Pathogenesis In the development of reactive arthritis, the phenomenon of cross-reaction of antibodies to the pathogen with the HLA-B27 antigen of the host's major histocompatibility complex has been revealed. A possible explanation for this is the theory of “molecular mimicry” - the structural similarity of proteins in the cell wall of bacteria with proteins in the cells of a sick person.
There are several immunological hypotheses for the pathogenesis of reactive arthritis.
Antigen-presentation hypothesis: according to it, the HLA-B27 complex is capable of presenting microbial peptides that cause arthritis. By interacting with cytotoxic CD8 T lymphocytes, they cause lysis of cartilage cells and an inflammatory process. Disorders of heavy chain assembly of the HLA-B27 antigen: proposed in 2000 by RA Colbert et al. According to it, under the influence of polysaccharides of microbial cells, the synthesis of heavy chains of the HLA-B27 antigen is disrupted. This leads to disruption of macrophage activity, reduces the effectiveness of their immune response and destruction of bacterial cells, and can lead to the development of inflammation in the joint. Cytokine hypothesis. Proposed by J. Sieper in 2001. Based on studies showing cytokine imbalance in patients with reactive arthritis. A decrease in the Th1 immune response (production of IF-γ, TNF-α, IL-2 and IL-12) in favor of a Th2 immune response (synthesis of IL-4 and IL-10) was revealed. At the same time, in the macrophages of the synovial fluid, the production of IF-γ and TNF-α decreases and the production of IL-4 increases, which contributes to the persistence of bacteria in the joint. This hypothesis is under development and has not yet been fully formulated. Currently, the concept of reactive arthritis as sterile has lost its relevance. One of the important advances in the study of reactive arthritis at present is that arthritis-initiating microorganisms, in particular chlamydia, disseminate into the joint. Proof of this is the detection of viable chlamydia in the joint membrane and joint fluid by nucleic acid amplification. Despite this, during routine diagnostics it is almost impossible to isolate chlamydia from a joint. It is believed that chlamydia is “recruited” into the joint by the synovial membrane as part of macrophages and dendritic cells. The latter probably stimulate a specific T-cell immune response directly in the joint. This is confirmed by the fact that the synovial membrane consists of 50% macrophages, so that in the joint, as a rule, the capture of certain particles from the bloodstream is inevitable. More often this occurs in large and medium-sized joints (knees, ankles), which are subject to microtrauma as a result of the fact that they bear a supporting load. According to various authors, chlamydia is determined in the joint with subsequent cultivation in developing chicken embryos and in living cells in more than half of the cases (53%). During cultivation, both typical and L-forms are determined. Both of them, therefore, can persist in the synovium.
Clinical picture Joint damage: Develops within a month after the infection. Mostly large joints of the lower extremities (knees, ankles, big toes) are affected on one side. Other joints may also be involved, rarely more than six, and arthritis of the sacroiliac joints (sacroiliitis) and the overlying parts of the spine often occurs. Damage to the tendons: Along with the joints, the tendons, at the place of their attachment to the bone, and the tendon bursae of the toes and hands are often affected with the development of dactylitis. Damage to the mucous membranes: Conjunctivitis - often oligosymptomatic or asymptomatic, short-term. Non-infectious urethritis, annular balanitis, cervicitis, oral erosions, and uveitis may develop. Skin lesions: Keratoderma (keratoderma blennorrhagica) is a painless keratinization of the skin with rashes in the form of papules and plaques, most often on the plantar part of the feet and palms. Nail damage: More often detected on the toes: yellow discoloration, peeling and destruction of the nail. Systemic manifestations: Enlarged lymph nodes, especially inguinal ones. Pericarditis, myocarditis, leading to cardiac conduction disturbances; aortic valve insufficiency, pleurisy, kidney inflammation (glomerulonephritis). Possible development of polyneuritis. Reiter's syndrome Main article: Reiter's syndrome A classic manifestation of reactive arthritis, it combines the “Reiter's triad”: damage to the joints (arthritis, synovitis), eyes (conjunctivitis, uveitis), and mucous membranes of the genitourinary organs (urethritis). In the case of the addition of skin manifestations (keratoderma), it is called “Reiter's tetralogy”. It was first described by Benjamin Brody, and then in 1916 by the German military doctor Hans Conrad Reuther in a soldier who had suffered from dysentery.
Currently considered as a special form of reactive arthritis. The disease begins 2 - 4 weeks after a chlamydial or intestinal infection, most often with damage to the urogenital tract. The most common triggering agents are Chlamydia trachomatis and Shigella flexneri 2a, as well as their combination.
Diagnostics Diagnostic criteria Criteria of the III International Meeting on Reactive Arthritis (Berlin, 1996):
Peripheral arthritis : Asymmetric Oligoarthritis (affects up to 4 joints) Predominantly affecting the joints of the legs Infectious manifestations: Diarrhea Urethritis Occurrence 2-4 weeks before the development of arthritis Laboratory confirmation of infection: In the presence of clinical manifestations of infection - desirable In the absence of obvious clinical manifestations of infection - mandatory Exclusion criteria - an established cause of the development of mono- or oligoarthritis: Spondyloarthritis Septic arthritis Crystalline arthritis Lyme disease Streptococcal arthritis Differential diagnosis Septic arthritis: occurs in the form of monoarthritis. It is characterized by high leukocytosis of synovial fluid (20,000-100,000/μl), positive results of bacterial culture. Viral arthritis can be caused by rubella viruses, parvovirus, adenovirus, hepatitis B virus, herpes viruses of various types, mumps virus, enteroviruses, Coxsackie viruses, etc. History often shows a connection with a viral infection or vaccine. In the clinic, the syndrome is more pronounced: arthralgic syndrome (joint pain) than arthritic syndrome (swelling, hyperemia). Within 1-2 weeks, symptoms disappear without residual effects. Poststreptococcal arthritis : appears against the background or 1-2 weeks after a streptococcal infection, characterized by simultaneous involvement of the middle joints, an increase in the titer of anti-streptococcal antibodies. Patients often have chronic foci of infection in the nasopharynx (tonsillitis, pharyngitis, sinusitis). The effect of NSAIDs may be delayed, and the improvement in laboratory parameters is insignificant. Rheumatoid arthritis : the clinic differs. There are no special markers. With reactive arthritis, inflammation of the tendons occurs and a common symptom is heel pain. It is difficult to differentiate in the case of the onset of oligoarthritis in young people, asymmetry of lesions and seronegativity. A thorough search for trigger infections and dynamic monitoring are required. Ankylosing spondylitis : The only difference is the x-ray of the SIJ (sacroiliac joint) and hip joints: if sacroiliitis is unilateral or absent, then reactive arthritis (RA), and if bilateral, at least stage 2, or unilateral, at least stage three, then Ankylosing spondylitis. But this is not suitable for early diagnosis, since these changes appear only after several years of illness. There is every reason to believe that prolonged reactive arthritis will develop into Ankylosing spondarthritis, and may be considered a certain stage in the development of the disease. Psoriatic arthritis : Difficulties arise when arthritis develops before skin symptoms appear. To exclude reactivity, a search for trigger infections and monitoring over time is carried out. Lyme disease : has a characteristic epidemiological history: stay in endemic areas, tick bite. Antibodies to the genus Borrelia are detected in the blood. Tuberculous arthritis : there are general symptoms of tuberculosis: intoxication syndrome, low-grade fever, autonomic disorders. Joint pain, mainly at night, symptoms of arthritis. The diagnosis is confirmed by x-ray data, analysis of synovial fluid, and biopsy of the synovial membrane. Laboratory diagnostics Mandatory tests include: a general blood test, urine test, detection of chlamydia and antibodies to them, testing for the presence of HIV infection, gonococci, stool testing for Salmonella, Shigella, confirmation of the absence of antinuclear antibodies and rheumatoid factor.
Study for the result: Complete blood count: leukocytosis, increased ESR, normochromic anemia. General urine analysis: possible proteinuria, microhematuria, leukocyturia AT, PCR: often positive for chlamydia AT: positive for gonococci only in case of mixed infection Stool analysis: Possible detection of Salmonella, Shigella Antinuclear AT: Absent Rheumatoid factor: Absent Additional studies include analysis of synovial tissue liquids. Signs of a reliable diagnosis of reactive arthritis are: low viscosity of the synovial fluid, poor formation of a mucin clot, leukocytosis (5000-10,000/μl) with a predominance of segmented neutrophils. Unlike septic arthritis, a decrease in glucose concentration is uncharacteristic.
Instrumental studies Mandatory: X-ray examination of the affected joints. Characteristically: changes can be noticed only with a long course of the disease; it is possible to detect unilateral sacroiliitis, more often in carriers of the HLA-B27 antigen. Gross changes in bone and cartilage, ossifications are uncharacteristic.
Additional : echocardiography (detection of damage to the aortic valves).
Treatment The outcome of the disease is closely related to the destruction (eradication) of the pathogen, which is why long-term use of antibacterial drugs is necessary. The goals of symptomatic treatment are to eliminate pain and inflammation in the joints.
Treatment is usually carried out on an outpatient basis; cases of severe arthritis with systemic manifestations and unclear cases requiring clarification of the diagnosis require hospitalization.
Non-drug treatment A motor regimen is indicated: rest of the affected limb during the first two weeks of the disease, but joint fixation and immobilization are not indicated. Cold on the affected joint. In the future, exercise therapy is prescribed according to an individual plan. There is no need to adhere to a special diet.
Drug therapy 1. Antibacterial therapy is of paramount importance in case of detection of chlamydial infection and is carried out for a long time. There are mainly three groups of drugs used that act on intracellular microorganisms: macrolides, fluoroquinolones and tetracyclines.
Drugs of choice:
Doxycycline 0.3 g per day, orally in 2 doses for 30 days; Azithromycin 1 g per day on the first day, then 0.5 g/day orally for 30 days; Clarithromycin 0.5 g per day, orally in 2 doses for 30 days; Spiramycin 9 IU per day, in 3 doses for 30 days. Second-line drugs (in case of intolerance or ineffectiveness of the above drugs):
Ofloxacin 600 mg per day orally in 2 doses for 30 days; Ciprofloxacin 1500 mg per day, orally in 2 divided doses for 30 days; Lomefloxacin 400-800 mg per day, orally in 1-2 doses for 30 days. In the case of enterocolitis, the effectiveness of antibiotics has not been proven.
2. NSAIDs - have a symptomatic effect: relieve pain and inflammation of the joints.
Diclofenac orally 2-3 mg/kg/day in 2-3 divided doses; Naproxen orally 15-20 mg/kg/day in 2 divided doses; Ibuprofen orally 35-40 mg/kg in 2-4 doses; Nimesulide orally 5 mg/kg in 2-3 doses; Meloxicam orally 0.3-0.5 mg/kg in 1 dose. Without exception, all NSAIDs have a negative effect on the stomach and kidneys! Therefore it is necessary to use the smallest possible dose.
When taking NSAIDs, you should monitor your blood tests to monitor your kidneys and liver. It is also necessary to use drugs to protect the stomach (Omeprozole...)
3. Glucocorticoids - for severe arthritis, they are used for intra-articular administration. A necessary condition is the exclusion of septic arthritis.
4. Immunosuppressors - used for severe and protracted course, signs of spondyloarthritis, high activity of arthritis.
Sulfasalazine 2 -3 / g/day. Methotrexate 7.5-15 mg/week. (Not used in modern treatment of reactive arthritis. Not a drug of choice since it has not shown effectiveness in studies in the group of seronegative spondiarthritis) Azathioprine 150 mg/day (Not used in modern treatment of reactive arthritis. Not a drug of choice since it has not shown effectiveness in studies in the group of seronegative spondiarthritis)
Course and prognosis The duration of the primary case is on average 3-6 months. Symptoms often persist for up to 12 months or more. There is a greater tendency to develop relapses in patients with Reiter's syndrome, both due to the possibility of reinfection and persistence of chlamydial infection.
The outcome of acute to chronic arthritis is observed in 20-50% of patients. In 15% of cases, severe joint dysfunction develops. The most severe course of reactive arthritis occurs in HIV-infected patients.
The period of temporary disability in acute cases is 30-60 days, in subacute cases 35-65 days, in case of exacerbation of chronic cases - 30-35 days.
With a protracted course of reactive arthritis, there is a high probability of its transition to one of the chronic diseases of the group of seronegative spondiarthritis (Ankylosing spondylitis)
Prevention Prevention of reactive arthritis comes down to preventing the infections that cause it: maintaining a hygienic regime regarding intestinal infections, boiling water, washing hands, following the rules of storing and preparing food. People who have a positive HLA-B27 antigen are recommended to take prophylactic antibiotics while traveling (norfloxacin 0.4 g 2 times a day). To prevent chlamydia, protective equipment is used during casual sexual contact.
How dangerous is the disease?
The danger of reactive arthritis is that it can develop into a long-term chronic recurrent disease that is difficult to treat.
Stages of ReA
Any form of arthritis has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
The inflammatory process in the joints occurs in several stages:
- initial
- with an acute onset, general symptoms appear: fever, headache, malaise, as well as inflammation, swelling and tenderness of the joints; At first, the ankle joints and joints of the 1st toe are most often affected; - expanded
- asymmetrical damage to the joints of the legs (from bottom to top), starting from the ankle joints to the knees; pain appears in the lower back associated with damage to the joints of the spine, skin rashes, erosions on the mucous membranes, enlarged lymph nodes; with Reiter's syndrome - conjunctivitis and urethritis; - final
- with intestinal and nasopharyngeal forms of reactive arthritis, the inflammatory process ends after 3 months with recovery; in a subacute course, the process can last up to 6 months and also end in recovery; The urogenital form of ReA often occurs chronically.
Possible complications
Chronic reactive arthritis can cause lameness
Reactive arthritis should be treated as early as possible.
Prolonged inflammation can lead to chronic pain, especially in the heel, foot and toes, leading to lameness.
With a long chronic course of Reiter's syndrome, damage to the optic nerve and blindness is possible, as well as damage to the reproductive system and infertility.
What to do during an exacerbation
If the inflammatory process has taken a chronic, relapsing course, then it is necessary to carry out long-term treatment under the supervision of a physician. When the first signs of relapse of reactive arthritis appear, you should:
- limit physical activity;
- take a medicine from the group of NSAIDs (non-steroidal anti-inflammatory drugs) - Diclofenac, Ibuprofen, Meloxicam; a tablet of any product can be taken orally, and a cream, gel or ointment with the same composition can be applied externally to the area of the affected joint;
- Urgently contact your doctor to prescribe adequate treatment.
Possible localization of inflammation
In intestinal and urogenital forms of reactive arthritis, the joints of the lower extremities are most often affected. In the nasopharyngeal form - the joints of the upper extremities and the temporomandibular joint.
Arthritis of the lower extremities
Affection of the lower extremities predominantly begins with the big toes and moves upward (staircase sign), affecting the overlying joints asymmetrically. In reactive arthritis, one to five joints become inflamed:
- interphalangeal toes; Most often the first toe is affected, it swells and turns red - the “sausage toe” symptom;
- ankles with damage to surrounding tissues; Particularly characteristic is damage to the tendons and ligaments in the heel area with the formation of loose heel spurs, which causes constant pain that intensifies when walking and stepping on the heel;
- knee – this location is characterized by the formation of a large amount of exudate (inflammatory fluid in the joint), which leads to the formation of popliteal cysts; rupture of cysts leads to the development of thrombophlebitis and impaired venous circulation;
- hip – rarely affected, occurs in the form of moderate joint pain.
Chondroprotectors: what are they, how to choose, how effective are they?
Joint pain at rest
Arthritis of the upper extremities
Localization of reactive arthritis in the joints of the upper extremities is much less common. This mainly occurs in diseases of the nasopharynx and dental infectious and inflammatory processes.
The most common joints affected by ReA are:
- elbow - the elbow swells, turns red, becomes painful, the arm has difficulty bending and unbending;
- wrist with damage to the ligaments and tendons of the hand - pain in the joint is transmitted to the hand; severe pain does not allow you to squeeze and unclench your hand or hold objects in it;
- shoulder – rarely affected, characterized by swelling and pain.
Temporomandibular arthritis
Reactive arthritis affects the joints of the lower and upper extremities, temporomandibular joints
Triggers include infections of the nasopharynx, ear and mouth. Characterized by slight swelling, redness and swelling in the area of development of reactive arthritis. When opening the mouth, there is a slight asymmetry; the chewing process may be disrupted and become painful. The disease occurs acutely or subacutely, is well treated, and the prognosis is favorable.
Symptoms
Acute peritonitis occurs in three stages, each of which has its own manifestations.
On the first day from the onset of peritonitis, in the reactive stage, a local reaction to irritation of the peritoneum is noted. Initially, pain is localized where the source of inflammation is located, and can radiate to the shoulder, under the collarbone. Subsequently, the pain spreads throughout the abdomen. To alleviate the condition, a person assumes the “embryo” position, lying with his legs pressed to his stomach. The patient is concerned about dry mouth, nausea and vomiting, and loss of appetite. The toxic stage develops between four and seventy-eight hours. Characterized by increasing intoxication up to endotoxic shock, increased general manifestations - blood pressure decreases, heart rate increases, body temperature rises and breathing problems appear. The pain is diffuse in nature, its intensity decreases, as paralysis of the nerve endings of the peritoneum begins, bloating and constipation are noted.
In the terminal stage, after seventy-two hours from the onset of inflammation of the peritoneum, a gross disruption of vital processes inside the body occurs. The symptoms of peritonitis are dominated by manifestations of paralytic intestinal obstruction - intense abdominal pain, severe vomiting that does not bring relief, and severe bloating. The patient's condition is extremely serious, facial features are sharpened, blood pressure is sharply reduced, urine does not pass, consciousness is confused, limbs acquire a bluish or yellow tint, increased sweating and other signs of multiple organ failure are characteristic.
Chronic peritonitis is characterized by “blurred” symptoms that arise as a result of prolonged intoxication and the formation of adhesions in the abdominal cavity, disrupting the functioning of internal organs.
Pathology manifests itself:
- lack of appetite and weight loss;
- increased sweating;
- persistent low-grade fever up to 37.5 °C;
- bowel dysfunction;
- periodic abdominal pain and bloating.
Adhesions and dense scar cords make it difficult to empty the hollow organs, which is accompanied by dyspeptic symptoms - nausea, vomiting, flatulence, urination and menstrual disorders.
Diagnostics
Diagnosis of reactive arthritis includes identifying characteristic manifestations of the disease and confirming the diagnosis with the following studies:
- Laboratory diagnostics:
- general clinical blood and urine tests - these studies reveal the presence of an inflammatory process, anemia;
- biochemical blood tests - total protein and protein fractions, the presence of C-reactive protein (a sign of an inflammatory reaction);
- immunological studies - rheumatoid factor, antibodies to cyclic citrullinated peptides to exclude rheumatoid arthritis; markers of systemic lupus erythematosus;
- detection of the HLA-B27 antigen by testing blood using the PCR (polymerase chain reaction) method, which allows identifying the smallest DNA particles of this protein;
- identification of urogenital, intestinal infections and foci of nasopharyngeal infections using microscopic, microbiological (culture on nutrient media), immunological studies;
- To exclude purulent arthritis, synovial fluid is sometimes examined.
- X-ray of the joints, during which the degree of their damage is revealed.
- Ultrasound - allows you to identify changes in the periarticular tissues.
- Arthroscopy is the examination of the inner articular surface using optical equipment. Rarely used in ReA.
Treatment of reactive arthritis
Only a doctor can cure reactive arthritis after an examination and taking into account its results. Basic principles of treatment of reactive arthritis:
- elimination of inflammation and joint pain;
- suppression of infectious-allergic and autoimmune processes;
- eliminating the trigger infection.
The following types of treatment for reactive arthritis are carried out:
- medicinal;
- non-medicinal;
- using folk remedies.
Drug therapy
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Treatment for reactive arthritis begins with eliminating inflammation, swelling and pain. For this purpose, patients are prescribed NSAID drugs. The most effective medications include Diclofenac, Aceclofenac, Ibuprofen and others in the form of injections, tablets or externally (gels, ointments).
In case of severe swelling and inflammation that cannot be eliminated by NSAIDs, glucocorticoid hormones are prescribed. They are prescribed in courses in the form of tablets orally (Prednisolone), in the form of pulse therapy - short intensive courses intravenously (Methylprednisolone), and also by injection into the joint or periarticular tissue (Hydrocortisone, Diprospan).
If there is a risk of transition to a chronic course, basic therapy is prescribed - drugs that suppress immune reactions: Sulfasalazine, Methotrexate, Azathioprine, etc. Biological agents are also prescribed - biologically active substances (antibodies, cytokines, etc.) that take part in immune reactions ( Mabthera).
For trigger urogenital infections, a long course of antibacterial therapy must be prescribed: antibiotics from the group of macrolides (Clarithromycin), tetracyclines (Doxycycline) or fluoroquinolones (Ciprofloxacin) for a month or more.
For intestinal infections, antibacterial therapy is considered inappropriate. For nasopharyngeal and dental infections, the decision to prescribe antibiotics is made by the doctor individually.
Medicines for the treatment of reactive arthritis
Non-drug treatment
Non-drug treatments include:
- Diet. There is no special diet, but given the allergic component of the disease, foods that cause allergies (eggs, nuts, citrus fruits, red and orange vegetables and fruits, etc.), spicy seasonings, fried, canned, smoked foods, sweets and baked goods are excluded from the diet.
- Physiotherapeutic procedures. In the acute period, to eliminate swelling and pain, electrophoresis with Hydrocortisone is prescribed, and then laser and magnetic therapy. At the recovery stage, sanatorium-resort treatment with balneo and mud therapy is recommended.
- Reflexology courses.
- PRP therapy is the stimulation of the body’s regenerative abilities by introducing the patient’s own plasma enriched with platelets.
- Therapeutic exercises and massage are carried out after eliminating the acute inflammatory process.
Folk remedies
Treatment of reactive arthritis with folk remedies is often included in complex treatment to enhance the effectiveness of drugs and reduce the drug load on the patient’s body. Folk remedies are selected for each patient individually, depending on the nature of the disease.
Self-treatment of reactive arthritis with folk remedies is ineffective.
Lecture on the topic “Inflammation”
Inflammation is a pathological process that occurs when tissue is damaged and is manifested by impaired circulation, changes in blood and connective tissue in the form of alteration, exudation and proliferation. This predominantly local process involves, to one degree or another, the entire body and, above all, such systems as the immune, endocrine and nervous. External signs of inflammation have been known for a very long time. They are formulated in the famous pentad of Celsus - Galen. These are swelling (tumor), redness (rubor), heat (calor), pain (dolor) and dysfunction (functio laesa). Although these symptoms have been known for over 2000 years, they have not lost their significance today; Over time, only their explanation changed.
Inflammation is a protective-adaptive reaction of the body to the action of a pathogenic stimulus, manifested at the site of damaged tissue by a change in blood circulation and an increase in vascular permeability.
This is a typical pathological process aimed at eliminating the pathological irritant and restoring damaged tissue.
Causes of inflammation:
· Physical
· Chemical
· Biological
The occurrence, course and outcome of inflammation depend on the reactivity of the body, which is determined by age, gender, the state of physiological systems, and the presence of concomitant diseases.
Its location is important in the occurrence, development and outcome of inflammation (a brain abscess or inflammation of the larynx due to diphtheria is extremely life-threatening).
Types of inflammation:
• Normergic
: the body's response to irritation corresponds to the strength and nature of the stimulus.
• Hyperergic:
The body's response to stimulation is more intense than the action of the stimulus.
• Hypergic
: inflammatory changes are mild or absent.
Stages of inflammation development:
1. Cell alteration
2. Cell exudation
3. Cell proliferation
All these stages are present in the area of any inflammation.
I. Alteration – tissue damage – a trigger for the development of the inflammatory process.
It leads to the release of biologically active substances - inflammatory mediators. All changes that occur at the site of inflammation under the influence of these substances are aimed at the development of the second stage of inflammation. Inflammatory mediators change the metabolism, properties and functions of tissue. These include histamine, serotonin, kinins (blood plasma polypeptides). They cause pain, dilation of microvessels, increase their permeability, and activate phagocytosis. The restructuring of metabolism in the alteration zone leads to a change in the physicochemical properties of the tissue and the development of acidosis in them, which increases vascular permeability, protein breakdown, oncotic and osmotic pressure. This increases the release of water from the vessels, causing the development of exudation and inflammatory edema.
II. Exudation
–
exit from the vessels into the tissue of the liquid part of the blood, as well as blood cells.
As a result of alteration, arteriolar spasm develops and arterial blood flow decreases (tissue ischemia in the area of inflammation). This leads to metabolic disorders in the tissue and acidosis. The spasm of the arterioles is replaced by their expansion, the speed of blood flow and the volume of inflowing blood increase. At the site of inflammation, metabolism increases, the influx of leukocytes and antibodies to it increases. The temperature increases and redness of the area of inflammation occurs (arterial hyperemia). As inflammation develops, it changes to venous hyperemia. The volume of blood in the venules and capillaries increases, the speed of blood flow decreases, the volume of blood decreases, the venules become tortuous, and jerky blood movements appear in them. The tone of the walls of the venules is lost, they become thrombosed, and are compressed by edematous fluid. A decrease in blood flow speed promotes the movement of leukocytes from the center of the blood flow to its periphery. They adhere to the walls of blood vessels - the marginal position of leukocytes. It precedes their release from the vessels into the tissue.
Venous hyperemia ends with blood stoppage. Lymphatic vessels become overfilled with lymph, and lymph flow slows down. The source of inflammation is isolated from undamaged tissue. At the same time, blood flows to it, and its outflow slows down, which prevents the spread of toxins throughout the body.
Venous hyperemia is the highest point of the exudation stage. The leading importance at this stage is the increase in microvascular permeability, the development of acidosis and hypoxia. The fluid that accumulates at the site of inflammation is exudate. It contains protein, globulins and fibrinogen, and also always contains blood cells that form an inflammatory infiltrate.
Exudation is the flow of fluid from the vessels into the tissue towards the center of the inflammation, preventing the spread of a pathogenic irritant, facilitating the entry of leukocytes, antibodies and biologically active substances into the inflammation. The exudate contains active enzymes, the action of which is aimed at destroying microbes and melting dead cells and tissues. But at the same time, the exudate can compress the nerve trunks and cause pain, disrupt the function of organs and tissues. Exudation is accompanied by the immigration of leukocytes from the vascular bed into the tissue.
Mechanism of passage of leukocytes
: the endothelial cells of the vessel contract, and into the resulting gap the leukocyte throws out part of the cytoplasm - pseudopodium, as a result the leukocyte ends up under the endothelial cell. Having overcome the basement membrane, it leaves the vessel and goes to the center of the inflammation. The movement of leukocytes is facilitated by their negative charge, while in inflamed tissue the charge is always positive.
I.I. Mechnikov developed the idea of chemotaxis of leukocytes, i.e. The leukocyte reacts to chemical irritation emanating from the site of inflammation.
In 1882, Mechnikov’s work “On the healing powers of the body” was published in Russia, which substantiated the idea of phagocytosis - the process of active capture, absorption and intracellular digestion of living and non-living particles by special cells (phagocytes):
• Microphages (neutrophils)
• Macrophages (motile – blood cells – monocytes; fixed – stellate endothelial cells in the liver)
Macrophages destroy pathogens of chronic infections, single-celled creatures, animal parasites, altered and dead cells of the body.
Stages of phagocytosis:
1. approaching the object
2. adhesion of the object to the phagocyte membrane
3. immersion of an object in a phagocyte
4. intracellular digestion of the object
A vacuole, a phagosome, is formed in the cytoplasm of the phagocyte around the object of phagocytosis. Lysosomes approach it, and the digestion process begins.
Types of phagocytosis:
• completed (the object is completely destroyed)
• incomplete (the object is not destroyed, but quickly multiplies in the phagocyte, which then dies, and microorganisms are carried by blood and lymph).
This is phagocyte failure
:
hereditary (impaired phagocyte maturation)
acquired (result of radiation sickness, protein starvation; in old age)
III. Proliferation
– the process of cell reproduction, the final stage of inflammation. Cells of mesenchyme, blood vessels, and blood multiply. As a result, at the site of inflammation, tissue is restored either identical to the destroyed one, or a scar that can disrupt the function of the organ (in the pyloric part of the stomach, at the site of the ulcer, a keloid sometimes forms, which prevents the evacuation of food into the duodenum).
1. redness
2. fever
3. swelling
4. pain
5. dysfunction
Manifestation of inflammation:
Local
Redness is associated with the development of arterial hyperemia (the influx of arterial blood containing oxyhemoglobin is bright red). It also creates heat (local increase in temperature). The swelling occurs due to the accumulation of exudate, which puts pressure on the nerve trunks, causing pain. It is the result of the work of inflammatory mediators. Dysfunction of an inflamed organ is the result of a disturbance in its metabolism, blood circulation and nervous regulation.
Are common
They are protective and adaptive in nature: the number of leukocytes increases and the leukocyte formula changes. Fever often occurs, developing under the influence of pyrogens (secreted by neutrophils). The protein composition of the blood changes (the amount of a and b - globulins increases - acute inflammation; y - globulins - chronic inflammation). Leukocytes phagocytose and destroy microorganisms; increased body temperature activates leukocytes and the production of antibodies. SOE (ROE) increases, because the charge of red blood cells and their number decreases, but the amount of albumin and globulins increases.
Forms of inflammation.
Depending on the causes of the inflammatory process, a distinction is made between banal and specific inflammation.
Banal
can be caused by various microorganisms, physical and chemical factors.
Specific
are caused by pathogens of certain infections (tuberculosis, syphilis, leprosy).
According to the course, inflammation can be acute, subacute and chronic. Depending on the causes of the inflammatory process and the conditions, one of the stages of inflammation may predominate.
Therefore, they distinguish:
1. alternative
2. exudative
3. proliferative
1. With alternative
In inflammation, the process of cell alteration predominates, and exudation and proliferation are weakly expressed (heart, liver, kidneys, brain), therefore such inflammation is called parenchymal. If dystrophic changes lead to the death of cells and tissues, such inflammation is necrotic. It develops when tissue is exposed to highly active toxic substances (acid, alkali).
2. With exudative
In inflammation, the process of exudation predominates. Depending on the composition of the exudate, the following are distinguished: • Serous
• Fibrinous
• Purulent
• Hemorrhagic
• Mixed
If mucus is present in the serous or purulent exudate, it is called catarrhal inflammation. If inflammation is accompanied by tissue decay, it is called putrefactive.
Serous
inflammation is characterized by the presence of serous exudate, which contains 3% protein and does not contain desquamated cells. It is transparent, but if dead leukocytes are mixed with it, it becomes cloudy. Serous inflammation develops in parenchymal organs; on the serous membranes of cavities and mucous membranes of organs, with serous pleurisy, exudate accumulates in the pleural cavity. The leaves of the pleura become cloudy and congested; with serous myocarditis, exudate accumulates between the muscle fibers of the heart, which lose their cross-striations and disintegrate; in the kidneys, exudate accumulates in the cavities of the glomerular capsules.
Typically, serous inflammation is acute and ends well. After it, the original tissue is restored. Connective tissue rarely grows, and sclerosis of the organ develops, and adhesions form in the cavities.
Fibrinous
inflammation is characterized by the content of exudate, which contains the protein fibrinogen.
Once in the tissue, fibrinogen turns into fibrin and coagulates into thin white threads. In this case, a whitish film forms on the organs. Fibrinous inflammation can be lobar and diphtheritic. If the film is loosely connected to the underlying tissues and is easily separated from them, it is croupous.
If the film is tightly fused with the underlying tissues, and when it separates, ulcers form -
diphtheritic
. Croupous fibrinous inflammation often develops in children with diphtheria, while the film is easily separated and can clog the lumen of the trachea, leading to asphyxia.
For lobar inflammation
pericardium, a “hairy heart” effect occurs. At the end of lobar inflammation, the original tissue is usually restored.
For diphtheritic inflammation
necrosis of the mucous and submucosal membranes always occurs. At the end of such inflammation, granulation tissue forms at the edges of the ulcers, which matures into a scar.
Purulent inflammation
characterized by the presence of a large amount of protein and leukocytes, including dead ones (purulent bodies). Pus is a creamy mass of yellow-green color with an unpleasant odor. Necrosis of inflamed tissue always occurs under the action of enzymes in the lysosomes of neutrophil leukocytes during their breakdown.
As a result of the melting of the tissue, a cavity is formed in it, filled with pus and containing microorganisms. A cell wall of leukocytes and macrophages forms around the cavity - an abscess - limited purulent inflammation.
In the muscles, purulent exudate can diffusely spread - phlegmon - unlimited purulent inflammation. When pus accumulates, a channel is formed through which the pus is periodically removed to the outside.
Hemorrhagic inflammation
characterized by the presence of erythrocytes in the exudate. Develops in microbial and viral diseases (viral flu, anthrax, plague). It is acute and severe, the outcome depends on the type of pathogen.
Putrid inflammation
characterized by the presence of putrefactive bacteria. With this inflammation, tissues acquire a dark color and an unpleasant odor. It is very difficult and ends in the death of the patient.
3. Proliferative (productive)
) is characterized by the process of cell reproduction.
Interstitial (interstitial)
) inflammation develops in the interstitial tissue of parenchymal organs. The inflammatory infiltrate contains lymphocytes, monocytes and plasma cells. Some of them pass into fibroblasts, which form the protein protocollagen. It serves as the basis for the construction of collagen fibers of connective tissue. As a result of inflammation, diffuse sclerosis of the organ develops.
Granulomatous
inflammation is characterized by the accumulation of cells capable of phagocytosis in the inflamed tissue. They form groups in the form of nodules (granulomas). They are visible only under a microscope. Occurs with typhoid fever, typhus, rheumatism, tuberculosis, syphilis, leprosy. Granulomas grow in the lungs of people who work in hazardous industries for a long time. Often, a focus of necrosis forms in the center of the granuloma. The maturation of the granuloma ends with its sclerosis. Lime is often deposited in them, i.e. petrification occurs.
Specific
inflammation develops with tuberculosis and syphilis (chronic course). The inflammation is specific with the formation of granulomas. As inflammation progresses, granulomas undergo specific cheesy necrosis.
The course of these diseases is accompanied by significant immune restructuring of the body. In tuberculosis, acute inflammation begins with an alterative reaction, resulting in the formation of a focus of cheesy necrosis. Then tuberculous granulomas are formed - small, pinhead-sized, whitish tubercles. Cheesy necrosis contains Mycobacterium tuberculosis. With the progression of specific inflammation, the cellular tubercles merge, forming large cheesy nodes - solitary tubercles. When the process subsides, fibroblasts form a connective tissue capsule around the granuloma. The granuloma becomes sclerotic, lime is deposited in the necrosis focus, and the granuloma turns into petrification.
With syphilis caused by Treponema pallidum, granulomas also form in the internal organs. Syphilitic granulomas - gummas.
They can be single or multiple, 3–5 cm in diameter. They are most often localized in the bones and liver. As the process subsides, the gumma scleroses into a rough, star-shaped scar.
Approach to treating the disease in our clinic
When a patient is admitted to the clinic with symptoms of reactive arthritis, a mandatory comprehensive examination is carried out before prescribing complex treatment. At the same time, the patient undergoes emergency procedures to eliminate inflammation and pain. This includes drug treatment, acupuncture, physiotherapy, etc. After the examination, a comprehensive treatment is prescribed, which includes:
- modern Western methods of treatment using the latest drugs, treatment regimens and non-drug methods aimed at eliminating the symptoms of reactive arthritis;
- traditional oriental treatment methods aimed at restoring the health of the entire body, including joint function.
This approach allows you to quickly and effectively completely cure reactive arthritis.
Treatment of sepsis
Treatment of sepsis is based on three principles:
- Sanitation of the primary lesion. This can be achieved with surgery and/or adequate antibiotic therapy. If a primary lesion is discovered that can be treated surgically, it is necessary to do this as soon as possible. This may include opening and drainage of abscesses, removal of infected invasive devices (catheters, implants, etc.), drainage and lavage of the abdominal cavity, etc.
Antimicrobial therapy is another cornerstone of sepsis treatment, and its timeliness and adequacy are important. For example, if septic shock develops, drugs should be administered within an hour of the onset of symptoms. In this case, the drug must cover the entire spectrum of suspected pathogens and, importantly, penetrate the primary infectious focus. If it is necessary to prescribe combination therapy of several drugs, they are used for no more than 5 days, after which data from biological research methods must be obtained and the treatment regimen must be adjusted.
- Ensuring oxygen transport - all clinical manifestations of sepsis are aggravated in conditions of lack of oxygen, so it is very important to control this process. To do this:
- Hemodynamic support - infusion of solutions that ensure replenishment of water and electrolyte balance, medications are prescribed to maintain blood pressure, etc.
Respiratory support - artificial ventilation, oxygen masks, etc.
- Correction of metabolic disorders
- Ensuring the supply of necessary nutrients (proteins, fats, carbohydrates). If the patient is unable to take food or nutritional formulas on his own, replacement therapy is considered.
Monitoring glucose levels.
- Detoxification activities.
One of the effective ways to treat sepsis is selective sorption on TORAYMYXIN columns. This technique is successfully used in many countries around the world. Currently, more than 200 thousand patients with septic shock and severe forms of sepsis have undergone such treatment. The effectiveness and safety of the technology has been confirmed in clinical studies.
General clinical recommendations
In the acute and subacute course of ReA, after a course of treatment, the patient should be under the supervision of a rheumatologist for six months with clinical and laboratory monitoring every 3 months.
In the chronic course of the disease, dispensary observation is longer with the prescription of courses of anti-relapse therapy until a state of stable remission appears.
After an illness, it is recommended to avoid heavy physical activity and strength sports. Swimming is a good way to restore joint function.
Persons with a genetic predisposition (presence of the HLA-B27 antigen) to reactive arthritis are recommended to have one proven sexual partner.
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthritis
FAQ
Is reactive arthritis contagious?
No. But the urogenital infection that caused it can persist for a long time and be contagious.
Are there any peculiarities of the course, diagnosis, treatment in children?
In children, ReA is more acute and rarely becomes chronic.
What prognosis do doctors usually give?
The prognosis for reactive arthritis is favorable; in most cases, complete recovery occurs. But if left untreated, it becomes chronic with a long course and constant pain in the joints.
Reactive arthritis is a complex, incompletely studied infectious-allergic disease that mainly affects genetically predisposed people and requires timely and adequate treatment. It's not worth running.
But if you were unable to seek medical help in time, do not despair, modern technologies make it possible to provide assistance and relieve pain at any stage of the disease. The Paramita clinic (Moscow) will always help you.
Literature:
- Agababova ER, Bunchuk NV, Shubin SV, etc. Criteria for the diagnosis of reactive arthritis (draft). Scientific and Practical Rheumatology 2003;(3):82–3.
- Kovalev YN, Ilyin NI. Reiter's disease. Chelyabinsk: Option-book; 1993. 240 p.
- Zeidler H, Hudson AP. New insights into Chlamydia and arthritis. Promise of a cure? Ann Rheum Dis. 2014;73:637–44. doi:1136/annrheumdis-2013-204110.
- Ford D.K. Natural history of arthritis following venereal urethritis. Ann Rheum Dis. 1953;12(3):177–97. doi: 10.1136/ard.12.3.177.
Themes
Arthritis, Joints, Pain, Treatment without surgery Date of publication: 10/13/2020 Date of update: 12/14/2020
Reader rating
Rating: 5 / 5 (2)