The cause of inflammation can be sexually transmitted pathogens. Most often these are chlamydia and gonococci. If these bacteria enter the female genital tract as a result of infection, then the acidic environment of the vagina is not suitable for them, and they strive with all their might to get into the pipes, where the environment is more suitable. In addition, there is a cylindrical epithelium in which chlamydia can live. These pathogenic bacteria are “armed” with a sufficient arsenal of means to resist the immune system. However, inflammation in the appendages can be caused not only by the listed microorganisms.
Inflammation of the ovarian appendages is accompanied by nagging pain in the iliac region, which can even be confused with appendicitis. Fever and weakness are often noted. Pain occurs or intensifies during menstruation.
Complications
- Infertility.
It occurs due to the fact that during the inflammation the epithelial cells of the fallopian tubes are also affected. As a result, their normal function is disrupted, and the outcome may be scarring of the tube, which completely stops its functioning. During prolonged inflammation of the ovarian capsule, connective tissue grows. The ovarian capsule thickens and becomes denser. And it may happen that it becomes too strong and does not rupture at the moment of ovulation of the follicle. A mature egg will not be able to leave the follicle and will remain “imprisoned.” In this case, pregnancy will also be impossible. In addition to the tube and ovary, the adjacent peritoneum, the inner lining of the abdominal cavity, is affected. To limit the spread of infection in the peritoneum, connective tissue grows and adhesions are formed that glue the layers of the peritoneum together, limiting inflammation, but at the same time leading to immobility of the internal organs. This includes a decrease in the mobility of the fallopian tubes, which is necessary for the complete transfer of the egg to the uterus. The functioning of the fallopian tubes and ovaries is especially severely disrupted if the process has a long, chronic course. And acute inflammation almost always leads to it if left untreated. Therefore, when signs of inflammation of the appendages appear, you cannot expect that everything will go away by itself. In addition to infertility, inflammation of the appendages is fraught with serious complications, for example, a purulent abscess, which threatens peritonitis.
- Pyovar
is an extensive suppuration of the ovaries, up to their transformation into ulcers, due to the development of the inflammatory process in the pelvic organs. Pyovar occurs when the inflammatory process tends to suppurate. The course of the disease is characterized by duration and is accompanied by frequent exacerbations. For acute cases, the following symptoms are typical: sharp pain, high fever and leucorrhoea. In chronic cases, leucorrhoea becomes purulent, the patient notes painful sensations in the groin, which noticeably intensify during menstruation. These pains radiate to the thigh and sacrum. They become sharp during physical activity, sexual intercourse, and bowel movements.
- Sactosalpinx
is an accumulation of fluid in the lumen of the fallopian tube with the formation of a saccular formation. It is formed as a result of “soldering” of the pipe, most often during a subacute ongoing inflammatory process. The contents may be serous, serous-hemorrhagic. When suppuration occurs from the sactosalpinx, pyosalpinx develops. Salpingitis is an inflammation of the fallopian tubes, salpingoophoritis is a general inflammation of the tubes and ovaries, and pyosalpinx is the accumulation of pus in the tubes and their adhesion to the ovary when the infection and purulent inflammatory process spreads towards the peritoneum. Most often, both the fallopian tubes and the ovaries are simultaneously involved in the process (due to the proximity of the anatomical location) with the development of salpingoophoritis - a general inflammation of the fallopian tubes and ovaries (uterine appendages).
- With further development of the purulent process, salpingo-oophoritis can lead to the development of tubovarial formation and abscess, the rupture of which causes peritonitis.
Complications of PID
Diseases of the pelvic organs are very insidious, as they can cause serious complications, such as:
- ectopic pregnancy (can occur in every sixth woman with PID);
- chronic pelvic pain (one in five women with pelvic inflammatory disease suffers from it);
- tubal infertility (diagnosed in every fourth patient);
- ovarian dysfunction.
Also, with PID, inflammation of the pelvic peritoneum (pelvioperitonitis) is possible, which often develops into sepsis, tubo-ovarian abscess, which can be fatal.
Treatment
Depends on the stage of the disease and the severity of the process. In the subacute and chronic stages - physiotherapy. In case of an acute process - treatment in a hospital.
Conservative treatment includes rest, regimen, and antibacterial drugs (selected individually, taking into account the sensitivity of the patient’s flora).
Laparoscopy has proven itself well for therapeutic purposes: it allows you to eliminate the purulent focus in a gentle way, wash and drain the abdominal cavity, and remove the effects of chronic inflammation. In addition, in case of salpingo-oophoritis, the gynecological department of our center performs local injection of antibiotics into the ligaments next to the tube (during laparoscopy), which shortens the duration of the disease, quickly improves the patient’s condition, and reduces rehabilitation time.
Thus, diagnosis and appropriate treatment tactics, including the extent of the upcoming operation, in patients with purulent inflammatory diseases of the internal genital organs are determined individually, based on the results of clinical diagnostic studies, and are directly dependent on the nature of the identified changes.
It should be emphasized that for patients with severe purulent inflammatory diseases of the internal genital organs, surgical treatment is vital. The scope of operations varies from conservative-saving methods of laparoscopy and laparotomy to radical ones in the most severe cases.
Diagnostics
The ultrasound method is not sufficiently informative in diagnosing salpingoophoritis. It allows you to identify only space-occupying formations in the pelvis. Those. With ultrasound, it is possible to see the fallopian tubes, which are filled with fluid (with hydro- or pyosalpinx), as well as with the formation of abscesses (with purulent melting of the fallopian tubes and ovaries). Therefore, the diagnosis of acute inflammatory diseases of the uterine appendages is mainly based on clinical data and gynecological examination data.
Inflammatory diseases of the pelvic organs
Endometritis.
Women encounter the incomprehensible term “endometritis” after a difficult birth or after a complicated miscarriage. Quite often, patients hear about this during miscarriage, infertility, etc.
Endometritis is an inflammation of the inner functional layer of the uterus (endometrium). It should immediately be noted that this inner lining of the uterus is very important in the functioning of the female body. It contains a huge number of receptors for sex hormones and, under their influence, changes its structure during the menstrual cycle. In the first phase of the menstrual cycle, it is restored (grows again), then, under the influence of the hormones of the second phase, it “ripens” and a large amount of nutrients accumulates in it. Throughout the menstrual cycle, the uterus prepares to receive a fertilized egg. If pregnancy does not occur, the functional layer of the uterus is rejected (menstruation occurs). Figuratively speaking, the uterus “mourns” a failed pregnancy with tears of blood.
Any inflammatory process initially occurs under the influence of infection (microbes, viruses), which most often enter the uterus from the vagina. The uterine cavity, covered with endometrium, plays a very important role in the woman’s reproductive system and is very well protected from external infection by various mechanisms. Thus, the external and internal sphincter of the cervix narrow the entrance to the uterus, the cervical canal contains special mucus, rich in protective antibodies, which destroy microbial cells before they enter the uterus, and the endometrium itself can “protect itself” from infection with various biologically active substances ( local immunity). However, there are special microbes and viruses that are tropic to the inner membranes of the cervix and uterus, that is, they very easily “gnaw” their way up, blocking local protective mechanisms. Such infections include chlamydia, gonorrhea, and trichomoniasis.
Factors that contribute to the occurrence of endometritis are a decrease in general immunity (chronic stress, concomitant chronic diseases, vitamin deficiency, chronic intoxication, etc.). The factor of trauma to the uterus and cervix during childbirth and during miscarriages is very important. In women with deep postpartum cervical ruptures, chronic endometritis is much more common.
Symptoms of pelvic inflammation in women
In most cases, pelvic inflammatory disease does not cause any symptoms. Asymptomatic pelvic inflammation is normal when the infection was caused by chlamydia.
In other cases, the most common symptoms are:
- pain in the lower abdomen and pelvic area;
- copious vaginal discharge with an unpleasant odor;
- irregular menstrual bleeding;
- pain felt during sexual intercourse;
- lower back pain;
- fever, fatigue, diarrhea, vomiting;
- pain felt when urinating;
- problems with urination.
According to the clinical picture, acute and chronic endometritis are distinguished
- Acute endometritis
Postpartum endometritis is the most common manifestation of acute postpartum infection.
Its frequency after natural birth is 4 - 20%, after cesarean section - 45%. Hormonal and immune changes aimed at ensuring the development and growth of the fetal egg simultaneously reduce the general immunity of the pregnant woman and reduce resistance to infections. The main symptoms of the disease in the acute course (after childbirth, miscarriages, against the background of an IUD) are pain in the lower abdomen, increased body temperature, chills, copious purulent discharge from the genital tract, and possible uterine bleeding.
- Chronic endometritis
In the presence of sexually transmitted infections, a primary chronic inflammatory process of the endometrium often develops.
The main symptoms of chronic endometritis are menstrual irregularities: spotting before and after menstruation, scanty or, conversely, heavy menstruation, miscarriage, infertility. The complexity of the problem of endometritis is that after a single episode of inflammation in the uterine cavity, “traces” often remain for life in the form of intrauterine adhesions (the so-called synechia), compaction (sclerosation) of the walls of the uterine cavity.
Due to persistent damage to endometrial receptors, its improper functioning occurs, which is expressed in menstrual irregularities, as well as the absence of its normal maturation (thickening) in the second phase of the menstrual cycle, which leads to the development of spontaneous short-term miscarriages, and often to infertility.
Against the background of chronic endometritis, endometrial polyps can form as a consequence of a violation of local reception.
Endometritis
Acute endometritis Most often occurs after abortion, childbirth or diagnostic curettage of the uterus. Clinical signs of acute endometritis usually appear 3-4 days after infection. The temperature rises, the pulse quickens, there is chilling, there are all signs of an inflammatory process in the body and according to a clinical examination. The discharge is serous-purulent, often sanguineous for a long time, which is associated with a delay in the regeneration of the mucous membrane. The acute stage lasts 8-10 days. With proper antibacterial treatment, the process ends and less often becomes subacute or chronic.
Chronic endometritis The frequency of chronic endometritis averages 14%. In recent years, there has been a tendency towards its increase, which is associated with the widespread use of intrauterine devices and the increase in the number of abortions.
As a rule, chronic endometritis occurs as a result of untreated acute postpartum or post-abortion endometritis; its development is often facilitated by repeated intrauterine interventions due to uterine bleeding.
The diagnosis can be indirectly made by ultrasound signs, but it can be 100% confirmed only by hysteroscopy and histological examination of the endometrium!!
Quite often, chronic endometritis is a uterine factor of infertility, and requires long-term and serious treatment after confirmation of the diagnosis.
When the infection spreads upward from the uterine cavity into the fallopian tubes, salpingoophoritis develops, i.e. inflammation of the uterine appendages.
How is endometritis treated?
Since the main cause of acute endometritis is microbial infections, the treatment complex necessarily includes antibiotics. After relief of acute symptoms, the course of treatment includes physical therapy, restoratives, and vitamin supplements.
To prevent the occurrence of chronic endometritis during menstruation, additional courses of antibacterial therapy are carried out. It is very good after a course of anti-inflammatory therapy to take oral contraceptives, which have antioxidant (anti-inflammatory) properties, for 2-3 menstrual cycles.
In case of chronic endometritis, if sexually transmitted infections are detected, antibacterial therapy is carried out, and treatment begins from the first day of the cycle. However, often the infection is no longer in the body, and the disorders are functional in nature, and treatment is aimed at normalizing the functioning of the endometrium: cyclic hormone therapy, physiotherapy, immunomodulators.
In the presence of intrauterine adhesions and endometrial polyps, separate diagnostic curettage under hysteroscopy control is required to destroy synechiae and remove polyps. The very procedure of “cleaning” the uterine cavity from heterogeneous scar-altered endometrium, removal of polyps followed by anti-inflammatory treatment very often leads to pregnancy in case of infertility, promotes normal pregnancy in the future, and normalization of the menstrual cycle.
So, the uterus with its inner layer - the endometrium - is a very important organ of the woman’s reproductive system with complex functions. After inflammatory diseases of the endometrium, the frequency of complications such as threatened miscarriage, placental insufficiency, and postpartum hemorrhage increases significantly. To minimize the risk of endometritis, it is necessary to avoid induced miscarriages and use barrier methods of contraception (condom) to prevent sexually transmitted infections. It is important to strengthen the immune system: get fewer colds, exercise, exercise, take multivitamins.
Important
And in conclusion: we live in a world populated by a huge number of microbes, viruses, fungi, however, nature has endowed humans with powerful protective mechanisms that allow him to live in balance with the environment. If this balance is temporarily disrupted, it is important to quickly help the body restore it. Therefore, preventive examinations by a gynecologist should be mandatory once every 6-12 months, even if it seems that there are no special health problems. This will allow timely detection of asymptomatic infections and avoid long-term inflammatory diseases. The diagnosis of “endometritis” is not a death sentence; in most cases, timely treatment leads to good results, which allows one to avoid complications of pregnancy and childbirth.
What is included in the concept of PID?
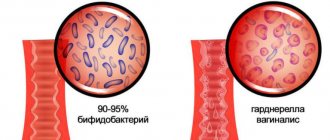
Pelvic inflammatory disease (PID ) is a group of diseases caused by pathogenic microorganisms (such as herpes virus, gonococci, chlamydia, human papillomavirus, trichomonas, cytomegalovirus) and opportunistic microorganisms (staphylococci, streptococci, gardnerella, mycoplasma and ureaplasma ). Often the cause of PID is mixed communities of pathogens.
Of course, the body has protection against pathogenic microbes. This is the acidic environment of the vagina, supported by lactobacilli, cervical mucus containing lysozyme, IgA. However, natural defense factors cannot always cope with the infection, and in such cases an inflammatory reaction develops.
1 Diagnosis of diseases of the pelvic organs
2 Diagnosis of diseases of the pelvic organs
3 Laboratory diagnostics
Medical statistics indicate the prevalence of inflammatory diseases of the pelvic organs in our country: more than 65% of women turn to a gynecologist with this particular problem.
PID can cause infertility, ectopic pregnancy, miscarriage, premature birth, and pathology of fetal development. Regular gynecological examination will help avoid such complications.