Pelvic varicose veins (PVVD) is one of the forms of varicose veins and affects the venous plexuses and vessels of the small pelvis. In 35% of cases, the pathology occurs due to hereditary connective tissue dysplasia, which leads to thinning of blood vessels and disruption of the functioning of venous valves.
The main symptom of the disease is long-term (more than 6 months) and intense pain in the pelvic area. Women are more susceptible to pelvic varicose veins, due to the peculiarities of the structure and functioning of the venous system of the female body.
Prices for phlebologist services
0
0 services selected for the amount of 0 rub.
| Total: | from 0 rub. | Sign up |
| Appointment (examination, consultation) with surgeon Globin A.V. (PhD) primary with ultrasound examination of the veins of the lower extremities | from 4000 rub. | Sign up |
| Microsclerotherapy (1 limb) (1 session) surgeon Globin A.V. | from 5400 rub. | Sign up |
| Microsclerotherapy (2 limbs) (1 session) surgeon Globin A.V. | from 7300 rub. | Sign up |
| Microsclerotherapy under ultrasound control or Venolight navigation (1 limb) (1 session) surgeon Globin A.V. | from 6400 rub. | Sign up |
| Microsclerotherapy under ultrasound control or Venolight navigation (2 limbs) (1 session) surgeon Globin A.V. | from 9200 rub. | Sign up |
| Endovenous laser surgery for varicose veins (1 limb) surgeon Globin A.V. | from 48400 rub. | Sign up |
| Endovenous laser surgery for varicose veins. CVI stage 1-2 (2 limbs) surgeon Globin A.V. | from 74600 rub. | Sign up |
| Endovenous laser surgery for varicose veins. CVI stage 3-4 (2 limbs) surgeon Globin A.V. | from 89300 rub. | Sign up |
Reasons for the development of VVDVT
The occurrence of pelvic varicose veins is caused by pathological changes in blood vessels, in which they cannot fully perform their functions - carry out the outflow of blood. This situation leads to stagnation or reverse blood flow (reflux), which provokes dilation of veins and the development of varicose veins.
The development of varicose veins can be caused by mechanical compression of the pelvic veins caused by pregnancy, inguinal hernia, the growth of voluminous tumors in the pelvis, and increased intra-abdominal pressure due to chronic constipation.
The main reasons for the development of pelvic varicose veins also include:
- genetic predisposition to vascular diseases (congenital weakness of the vascular wall);
- severe complicated childbirth;
- hormonal dysfunction;
- chronic, often recurrent diseases of the genitourinary system;
- constant uncontrolled use of hormonal contraceptives.
Risk factors for pelvic varicose veins are:
- lack of physical activity or excessive physical activity;
- excess weight, bad habits (alcohol abuse and smoking);
- long work in one position (standing, sitting);
- congestion in the pelvis associated with sexual disorders (anorgasmia, dyspareunia, erectile dysfunction).
Women of childbearing age from 25 to 45 years are more susceptible to violations. Every third expectant mother has VPVT of varying severity, and frequent pregnancies are the main provoking factor in the development of pelvic varicose veins.
Ultrasound diagnosis of varicose veins and thrombosis of the pelvic veins in women
Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Introduction
The prevalence of pelvic varicose veins varies widely, which indicates the ambiguity of diagnostic and tactical approaches to this problem. According to ultrasound studies, varicose veins of the small pelvis occur in 5.4% of apparently healthy women and in 15.7% of women with identified gynecological pathology. The combination of pelvic venous insufficiency and varicose veins of the lower extremities is noted in 62% of cases [1].
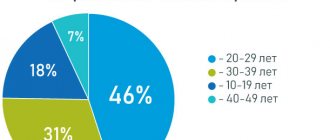
The disease affects women aged 20-25 years, and the largest number occurs in the period 25-45 years.
Dilatation of the pelvic veins in women is facilitated by the anatomical and physiological characteristics of the blood supply: the uterovaginal, vesical, rectal plexuses, anastomosing among themselves, carry blood into the internal iliac vein, and also, merging with the branches of the uterine veins of the upper third of the body of the uterus, the veins of the round and broad ligaments of the uterus - to the hilum of the ovary. Anastomosing with its veins, they form the pampiniform plexus of the ovary. Further outflow occurs into the ovarian vein, which on the right, anastomosing with the superior mesenteric vein, flows into the inferior vena cava, and on the left, anastomosing with the inferior mesenteric vein, into the left renal vein [2].
A feature of the structure of the veins of the listed plexuses, with the exception of the cystic and iliac veins, is the absence or poor development of the valve apparatus, and therefore the leading role in maintaining the tone of the venous wall is given to the sympathetic nervous system, hormones (in particular estradiol, progesterone), vasoactive substances, acid-base balance. There is a point of view that varicose veins are genetically determined collagenosis or a manifestation of angiodysplasia.
Chronic venous insufficiency develops under the influence of two main mechanisms: caval and regional left-sided venous renal hypertension. Every time a person strains, caval reflux occurs. In the absence of a predisposition to the varicose process, the spread of reflux into the parietal veins is prevented by their full-fledged valve apparatus, and into the valveless visceral plexuses by sufficient tone and active contractions of the venous walls. In women, isolated caval reflux causes varicose changes in the pampiniform plexus of the right ovary [3].
The anatomical prerequisite for the development of regional venous renal hypertension is compression of the left renal vein in the aortomesenteric “tweezers”. Against the background of a decrease in venous tone, this obstruction increases the pressure in the renal vein, which leads to the development of blood reflux through the left ovarian vein. Renoovarian reflux causes dilation of the veins of the pampiniform plexus of the left ovary, uterovaginal, presacral, vesical and rectal plexuses. The most pronounced phlebostasis in the pelvic organs in women develops with a combination of left-sided reno-ovarian and right-sided cava-ovarian blood reflux [4].
Factors that provoke the development of varicose veins of the small pelvis are considered working conditions (forced long-term orthostatic and physical activity), pregnancy and childbirth, sexual dysfunction, gynecological diseases, hyperestrogenism; In recent years, the adverse effects of hormone replacement therapy and oral contraception have been increasingly discussed [5].
Since the walls of venous vessels are an extensive reflexogenic zone, the expansion of their lumen is accompanied by pain. It is assumed that the retrograde nature of blood flow with the formation of turbulent flows has an irritating effect on the receptors of the vascular wall.
Varicose veins of the small pelvis still remain an insufficiently studied problem, since it is a pathology invisible to the clinician, but it leads to chronic pain, menstrual irregularities, infertility due to developing ovarian hypofunction, and can be complicated by vein thrombosis.
Thrombosis is based on the interaction of congenital and acquired factors. Congenital factors include lack of antithrombin III, inherited dysfibrinogenemia, decreased thrombomodulin levels in atherosclerosis, hyperhomocysteinemia, the presence of antibodies to phospholipids, excessive inhibition of plasminogen activators, plasminogen deficiency, G20210A mutation in the prothrombin gene (factor II), Leiden mutation, deficiency of proteins C and S , dysplasminogenemia, factor XII deficiency.
Acquired provoking factors include pregnancy and childbirth, surgery, infections, trauma, fractures, prolonged forced sitting or standing, long travel, immobilization, taking oral contraceptives, obesity, smoking, malignant tumors and chemotherapy, old age, heart failure, chronic venous insufficiency, stroke.
Until now, the detection of thrombosis of the pelvic venous plexus during transvaginal ultrasound (TVUS) is considered casuistry [6].
The purpose of this study was to assess the possibility of routine TVUS in diagnosing varicose veins and pelvic vein thrombosis and to develop an algorithm for further management of such patients.
Material and methods
We retrospectively analyzed the results of TVUS of 2,530 women aged 19 to 83 years (average age 51.3 years), performed on modern ultrasound machines with transvaginal sensors with a variable frequency of 7.5-10.0 MHz in a planned manner (2,210 patients) or for urgent indications (320) in the direction of a gynecologist with various diseases of the female reproductive system. A vein diameter not exceeding 4 mm was considered normal. When assessing the degree of ectasia of the pelvic veins, we used the classification of A.E. Volkov [2], according to which grade I included the diameter of the veins of any venous plexus of the small pelvis up to 5 mm and the corkscrew-like course of the vessels; to the II degree - the diameter of the veins is 6-10 mm with the total type of varicose veins, scattered ectasia of the ovarian plexus, parametric veins, veins of the arcuate plexus; to the III degree - the diameter of the veins is more than 10 mm with the total type of varicose veins or the main type of parametric localization.
results
Varicose veins of the small pelvis were diagnosed in 258 women, which accounted for 10.2% of the number of TVUS reports analyzed. Vein diameter up to 5 mm (I degree of ectasia) was found in 98 (38%) patients, from 6 to 10 mm (II degree of ectasia) - in 111 (43%) cases and more than 10 mm (III degree of ectasia) - in 49 ( 19%). In case of I degree of expansion, their left-sided localization was predominant; in case of II-III degree, the diameter of the veins on both sides was comparable, which is consistent with the literature data.
The main complaints of patients with varicose veins of the small pelvis were chronic pain in the lower abdomen and lower back, intensifying after prolonged static and dynamic loads, especially at the end of the working day and in the second phase of the menstrual cycle, after cooling, overwork, against the background of stress or exacerbation of diseases of the internal organs (73 %), dysmenorrhea - increased duration of menstruation, prolonged spotting, prolongation of the menstrual cycle, heavy menstruation (59%), dyspareunia - discomfort and pain during and after sexual intercourse (31% of patients). 3% of women had no pain or any other clinical manifestations. The absence or low severity of pain in some patients with significant varicose veins is explained by a high threshold of pain sensitivity [7].
In 53% of patients, a combination of varicose veins of the small pelvis with varicose veins of the lower extremities, perineum or chronic hemorrhoids was found.
When analyzing the frequency of combination of varicose veins of the small pelvis with non-vascular pathology, a predominance of uterine fibroids (28.4%), ovarian cysts and paraovarian cysts (24.3%) was noted. Less commonly, varicose veins of the small pelvis were combined with hyperplastic processes of the endometrium and cervical canal (13.5%), signs of adhesions in the pelvis (9.5%), internal endometriosis (4.0%), hydrosalpinx (1.4%) .
In 1 patient, varicose veins of the paraurethral plexus were accompanied by bilateral nephroptosis. In 40.5% of cases, varicose veins of the small pelvis were combined with one disease, in 56.8% - two or more, in 2.7% of women it was the only identified pathology.
Against the background of II and III degrees of ectasia, 34 cases of pelvic vein thrombosis were diagnosed.
On TVUS, the thrombus was visualized as an avascular formation, partially or completely blocking the lumen of the venous vessel. The echogenicity of the thrombus, depending on how long ago it occurred, ranged from low or medium (Fig. 1, 2) to high, up to the presence of calcified inclusions (Fig. 3, 4).
Rice. 1.
Patient K., 49 years old. The right uterine vein is dilated over more than 3.0 cm to 1.1-1.3 cm.
A)
In gray scale mode, an anechoic thrombus measuring 2.2×1.1 cm is practically not visualized.
b)
In the color flow mode, no staining of the vein lumen is observed.
Rice. 2.
Patient N., 42 years old.
In the lumen of the vein of the right parametric plexus, dilated to 0.7 cm, a weakly echogenic thrombus measuring 0.6×0.4 cm is visualized.
Rice. 3.
Patient X., 46 years old.
In the lumen of a vein dilated to 0.7 cm to the left of the uterus, a thrombus of medium echogenicity measuring 0.8×0.5 cm is visualized.
Rice. 4.
Patient R., 75 years old.
In the lumen of the vein of the right parametric plexus, dilated to 1.2 cm, a thrombus measuring 1.6×1.1 cm with an area of calcification with an acoustic shadow is visualized.
With color Doppler mapping (CDC), partial thrombosis was characterized by a parietal defect in filling the color cartogram; with complete thrombosis, the absence of staining of the vessel lumen was noted (Fig. 5).
Rice. 5.
Patient M., 28 years old.
A)
In the lumen of the vein of the left parametric plexus, dilated to 0.9 cm, a thrombus measuring 2.3×0.9 cm is visualized in gray scale mode.
b)
In the color flow mode, staining of the vessel lumen does not occur.
V)
In the energy mapping mode, coloring of the vessel lumen does not occur.
The age of women with pelvic vein thrombosis ranged from 25 to 82 years (average 49.6 years).
13 women were of reproductive age, 8 were perimenopausal, 12 were postmenopausal. In all cases, there was a burdened obstetric and gynecological history: inflammatory diseases of the pelvic organs or a history of urogenital infections were noted in 19 (55.9%) patients, fibroids uterus - in 15 (44%), internal endometriosis in 5 (14.7%), surgical birth, trauma, extirpation or supravaginal amputation of the uterus in 14 (41%). During hormonal therapy, pelvic vein thrombosis was diagnosed in 7 (20.6%) women, and against the background of the Mirena IUD - in 3 (8.8%). Chronic hemorrhoids bothered 12 (35.3%) patients, while in one patient taking oral contraceptives, thrombosis of the pelvic veins was accompanied by acute thrombosis of the hemorrhoid. Oncological diseases were noted in 4 (11.8%) cases: in 2 women (thyroid cancer and stomach cancer), surgical treatment was performed more than 5 years ago, in 2 malignant neoplasms were detected within 2 months after detection of pelvic vein thrombosis (cancer). breast and pancreatic head cancer).
Among the patients of the reproductive and perimenopausal periods, only one woman, 32 years old, had no history of pregnancy or childbirth, but she had uterine fibroids, paraovarian cysts, ureaplasmosis, was treated for trichomonas colpitis 2 months before treatment, and had previously taken hormonal drugs. contraceptives. The remaining patients in these groups had a history of childbirth, more than half of them twice or three times.
In the study group of patients, multiple (57.6%), fixed (87.9%), echogenic (75.8%) thrombi prevailed. The maximum size of blood clots was observed in younger patients; as a rule, it corresponded to the maximum expansion of the venous vessels.
Thrombosis was detected in 24.2% of patients against the background of grade I, in 69.7% against the background of grade II, and in 6.1% against the background of stage III varicose veins of the small pelvis.
Linear blood flow velocity was reduced in all cases. During menopause, there was a more significant decrease in speed indicators, even against the background of a smaller diameter of the venous vessels. The frequency of stasis increased in proportion to the age of the patients; the presence of retrograde blood flow was more common among perimenopausal women.
Phleboliths, or “venous stones,” are completely calcified blood clots and are considered as consequences of thrombophlebitis [8]. With TVUS they are visualized as hyperechoic formations with pronounced acoustic shadows (Fig. 6). In the analyzed group of patients, in combination with pelvic vein thrombosis, phleboliths were detected in 15 (44.1%) cases, which indicates a tendency for pelvic vein thrombosis to recur.
Rice. 6.
Patient P., 60 years old. Phleboliths are visualized in the lumen of a vein with a diameter of 0.5 cm.
A)
To the right of the uterus, two phleboliths measuring 0.3 and 0.4 cm with acoustic shadows are visualized.
b)
To the left of the uterus, in the lumen of a vein with a diameter of 0.5 cm, a phlebolith 0.4 cm in diameter is visualized; in the lumen of a vein dilated to 1.1 cm, a thrombus of medium echogenicity measuring 0.9 × 0.7 cm is visualized.
There were no cases of thromboembolic complications in the analyzed group of women. In 3 patients, during dynamic observation, under the influence of provoking factors, negative dynamics were noted in the form of an increase in the extent of thrombosis. During treatment, in almost all cases, there was either a decrease in the size of blood clots, their organization and calcification, or complete disappearance with the restoration of vascular patency according to CDC data.
As an illustration, we present two clinical observations.
Clinical observation 1
Patient Zh., 46 years old. Upon presentation, the patient was bothered by periodically occurring intense pain in the lower abdomen. History of yersiniosis, hormonal therapy prescribed by a gynecologist, which ended 2 months ago. Menstrual function is preserved. With routine TVUS: multiple uterine fibroids, endometrium without signs of pathology, ovarian follicular apparatus preserved; the pelvic veins are dilated to 0.7 cm, non-staining areas are visualized, the maximum blood flow velocity does not exceed 7 cm/s, in some cycles retrograde blood flow is recorded at rest, floating thrombi of medium echogenicity measuring 0.7 × 0.3 are visualized in the right parametric plexus ×0.5 and 0.8×0.3×0.5 cm, blood flow in these vessels is preserved, the spectrum is deformed; Single phleboliths were also identified (Fig. 7). There were no changes in the coagulogram at the time of the examination. According to a genotypic study of coagulation, a polymorphism was identified that predisposes to disruption of the folate cycle in a heterozygous form, which should explain the occurrence of pelvic vein thrombosis against the background of exposure to provoking factors (infection, hormonal therapy).
Rice. 7.
Patient Zh., 46 years old. Floating thrombi are visualized in the lumen of the convoluted dilated veins of the right parametric plexus.
A)
The size of the thrombus is 0.8×0.3×0.5 cm.
b)
The size of the thrombus is 0.7×0.3×0.5 cm (b).
Clinical observation 2
Patient Yu., 25 years old. The obstetric and gynecological history is burdened: in childhood she underwent surgery for pelvioperitonitis, in adolescence she received combined oral contraceptives due to dysfunctional juvenile uterine bleeding, 6 years ago there was laparoscopic resection of a paraovarian cyst and coagulation of foci of external endometriosis, 4 years ago - childbirth, Ureaplasmosis has now been identified. Due to an irregular menstrual cycle, on the recommendation of a gynecologist, she took hormonal contraceptives: Jess for 2 months, and then Diana-35. After 1 month of taking the last drug, the patient consulted a proctologist due to acute thrombosis of the external hemorrhoid. During the same period, a routine examination revealed small uterine fibroids, varicose veins of the small pelvis with symptoms of stasis and the presence of blood clots of varying echogenicity: in the left parametric and paraovarian spaces the veins are significantly tortuous, dilated to 0.8 cm, unstained areas are visualized, maximum speed blood flow is 4.4 cm/s, in some cycles retrograde blood flow is recorded. In the lumen of the dilated convoluted veins of the parametric (Fig. 8, a, b) and paraovarian plexuses (Fig. 8, c, d), multiple weakly echogenic fixed thrombi measuring from 0.4 to 2.5 cm are visualized.
Rice. 8.
Patient Yu., 25 years old.
a-d)
In the lumen of the dilated convoluted veins of the parametric (a, b) and paraovarian (c, d) plexuses, multiple weakly echogenic fixed thrombi measuring from 0.4 to 2.5 cm are visualized.
Despite the fact that thrombosis of the venous plexuses of the pelvis does not pose an immediate threat to pulmonary embolism, the very fact of detection of thrombus formation should be considered as a possible manifestation of systemic pathology, dictating the need for special diagnostics aimed at finding the causes of this phenomenon, i.e., primary predisposing factors.
When pelvic vein thrombosis is detected in the case of fixed blood clots, the patient must undergo a routine examination to identify the primary causes of thrombosis, namely a lack of antithrombin III, inherited dysfibrinogenemia, decreased thrombomodulin levels, hyperhomocysteinemia, the presence of antibodies to phospholipids, excessive inhibition of plasminogen activators, deficiency plasminogen, G20210A mutation in the prothrombin gene (factor II), Leiden mutation, protein C and S deficiency, dysplasminogenemia, factor XII deficiency with subsequent correction of treatment and recommendations for the prevention of secondary causes of thrombosis.
If floating blood clots are detected, the woman should be hospitalized in a specialized hospital.
Patients with varicose veins of the small pelvis, especially in combination with phleboliths and stasis phenomena, should be considered as a risk group for the development of diseases of the blood coagulation system, actively monitored and receive recommendations from a gynecologist for the prevention of secondary causes of thrombosis: quitting smoking, oral contraceptives, normalizing body weight , compliance with preventive measures during long trips, etc.
conclusions
Routine TVUS can detect not only varicose veins of the small pelvis, but also their thrombosis with a frequency of 10.2 and 1.3%, respectively. The fact of detection of thrombus formation in the venous plexuses of the pelvis should be considered as a possible manifestation of congenital defects of the blood coagulation system, and a special examination with subsequent recommendations will improve the quality of life of such patients.
Literature
- Ozerskaya I.A. Ultrasound diagnosis of dilated pelvic veins in women of reproductive age // Proceedings of the annual conference DiaMA (issue XII). Irkutsk, 2011.
- Volkov A.E. Echosemiotics of the pelvic veins // Echography. 2000. N 1. P. 55-59.
- Khomenko N.E., Voskanyan Yu.E., Gasparyan S.A. Varicose veins of the pelvis (etiopathogenesis, diagnosis, treatment) // Journal of the Russian Society of Obstetricians and Gynecologists. 2006. N 6. P. 44-46.
- Fedorova E.V., Ishchenko A.I., Lipman A.D. Study of the characteristics of venous blood flow in the pelvic area during laparoscopic gynecological operations // Ultrasound and functional diagnostics. 2002. N 2. P. 36-43.
- Ozerskaya I.A. Echographic findings in pelvic pain syndrome // Ultrasound and functional diagnostics. 2002. N 2. P. 151.
- Minaeva T.A. Varicose veins of the pelvis in women of early reproductive age with connective tissue dysplasia: Abstract of thesis. diss. ...cand. honey. Sci. Tomsk, 2005.
- Proskuryakova O.V. Particular issues of venous circulation of the internal genital organs of a woman // Dopplerography in gynecology / Ed. Zykina B.I., Medvedeva M.V. M., 2000. pp. 133-134.
- Bulanov M.N. Ultrasound diagnostics in gynecological practice. CD. M., 2002.
Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Classification
Pelvic varicose veins can be primary or secondary. The first occurs with congenital insufficiency of the venous valves, and the second, which occurs much more often, as a complication of inflammatory or tumor diseases in the pelvis.
The stage of the disease depends on the diameter of the affected vessels and at the initial stage of varicose veins it does not exceed 5 mm. The second stage of the disease is characterized by an increase in the size of the vessels to 10 mm, and the third stage of the disease and total damage is indicated by a vessel diameter of more than 10 mm.
Varicose veins of the pelvis can be accompanied by varicose veins of the perineum, vulva, pampiniform plexus of the spermatic cord, penis, buttocks, inner thigh and varicose veins of the lower extremities.
Symptoms, diagnosis
Patients complain of vague pain in the pelvic area, a feeling of heaviness. In some cases, there is pain during sexual intercourse. Pain can be provoked by prolonged static loads. If the venous plexus of the bladder is congested, there may be urinary disturbances (frequent urge, etc.).
Clinical manifestations of the disease are extremely scarce and uncharacteristic. Upon visual examination, the superficial veins of the perineum and buttocks may be dilated.
Of the instrumental methods, the simplest and most informative is ultrasound, which allows you to identify both the dilated veins themselves and examine the pelvic organs, which in some cases can clarify the cause of varicose veins.
Other methods include computed tomography, laparoscopy, and selective ovariography.
When is it necessary to contact a specialist?
The treatment of diseases of the pelvic veins is carried out by a phlebologist, and the reason for contacting a specialist is constant chronic pain in the lower abdomen. Pain may intensify after physical activity and sexual intercourse. Women experience severe premenstrual syndrome, dysmenorrhea, and copious vaginal discharge without signs of pathology. The disease may be accompanied by heaviness in the epigastric region, pulsation in the lower abdomen, and dysuric disorders.
Clinical symptoms of the disease are often similar to signs of endometriosis, organ prolapse, post-traumatic neuropathy, inflammatory diseases of the genitourinary system, radiculitis, neuralgia, chronic prostatitis and other pathologies.
Diagnosis of the disease
An examination by a phlebologist begins with clarifying the patient’s complaints, collecting anamnesis and visual examination of superficial vessels. Additionally, instrumental studies of blood vessels are performed.
- Ultrasound duplex scanning of the vessels of the pelvic veins solves a complex of diagnostic problems. It allows you to determine the presence of varicose veins, measure the diameter and patency of blood vessels, blood flow speed, choose the optimal method of therapy, etc. The study is carried out in two ways - transvaginally and transabdominally. In the first case, the veins of the parametrium, acrylic plexuses and uterine veins are visualized. Transabdominal examination allows you to evaluate the condition and functionality of the inferior vena cava, ovarian veins and left renal vein.
- Pelvic venography with selective bilateral radiopaque ovariography. Before the examination, a contrast agent is injected into one of the main veins using a catheter and the vessels are examined under the control of an X-ray machine.
- Diagnostic laparoscopy is a minimally invasive surgical procedure. Used when other diagnostic methods are insufficiently informative.
To assess the degree of development of venous pathology and the possibility of relapse, an additional scan of the vessels of the lower extremities, perineum, vulva of the inner thigh and buttocks is performed.
Treatment methods for pelvic varicose veins
At the Profimedica clinic, treatment of pelvic varicose veins is carried out in two ways: conservative and surgical.
In order to identify pathology, differential diagnosis is carried out using laparoscopy. The presence of varicose veins is indicated by bluish formations with a thin, tense wall in the area of the ovaries and the broad uterine ligament detected by this method.
Conservative treatment
The first method is used if the patient consults a doctor in the early stages of the disease. Conservative treatment methods include:
- Elimination of factors that provoke the development of pathology (change of sedentary or standing work, increased activity, etc.).
- Avoiding excessive physical activity.
- A balanced diet, including more fresh vegetables and fruits and excluding alcohol, cigarettes, fatty and spicy foods.
- Using a contrast shower to improve blood circulation in the body.
- Carrying out a daily set of exercises (“scissors”, “birch tree”, “bicycle”, etc.).
- The use of special breathing exercises, which are based on breathing using the muscles of the anterior abdominal wall.
- Constantly wearing compression tights.
- Taking medications that accelerate blood flow (phleboprotectors).
Surgery
If the disease was detected already in severe stages, or it was not possible to cure pelvic varicose veins in women using conservative methods, doctors may recommend surgical intervention.
During the operation, the surgeon eliminates the abnormal reflux of blood by passing through the dilated gonadal arteries. When eliminating the disease, as a rule, the method of embolization of ovarian vessels is used. For maximum precision of surgical intervention, all manipulations are carried out under the control of parallel angiography.
In rare cases, open resection or vein clipping techniques during laparotomy may also be used. In this case, the progress of the operation is monitored using an endoscope.
Treatment of pelvic varicose veins
Treatment of pelvic varicose veins is a set of measures aimed at normalizing vascular tone, improving tissue trophism and preventing congestion in the pelvis. Therapy includes changing the patient’s work and rest schedule, diet, eliminating heavy physical activity, and giving up bad habits.
Patients need daily physical activity and wearing compression garments. Drug therapy consists of taking venoprotectors, antiplatelet agents, membrane protectors, phlebotonics, and non-steroidal anti-inflammatory drugs.
Medicines reduce stretching of veins, venous stagnation, improve lymphatic drainage and blood microcirculation, and have an anti-inflammatory effect.
Treatment of dilated pelvic veins
Primarily, there are several medications that have been shown to be effective in approximately 75% of women in reducing the pain and size of varicose veins.
The usual treatment is percutaneous transcatheter pelvic vein embolization. This is a minimally invasive treatment that is safe and can be performed in 1 day. You arrive for your procedure in the morning and can leave a few hours later the same day. Indeed, in most cases, the cause of varicose veins is the ovarian vein. However, other pelvic veins, such as veins called the internal iliac vein, internal pudendal vein, obturator vein, and sciatic veins, may also be responsible and also need treatment.
Other treatment options for pelvic varicose veins in women include open or laparoscopic surgery to ligate the culprit veins. Both of these procedures are more invasive than ovarian vein embolization and require general anesthesia and a longer recovery period.
In addition to drug treatment, you can combat the problem with the help of physical therapy, as well as wearing special compression garments. In this case, compression tights will come in handy as they will improve blood flow in the legs and, as a result, partially in the pelvic organs.
Considering the benefits of physical activity, it is important for women with varicose veins of the pelvic organs to perform daily exercises such as “scissors”, “bicycle”, “birch tree”. Breathing exercises and contrast showers on the upper legs and pelvic area are also useful. Full-fledged gymnastics is the right path to a normal and healthy life.