What is arrhythmia? Causes and treatment of arrhythmia at home
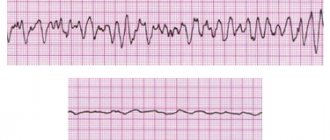
Arrhythmia is a violation of the frequency, rhythm and/or sequence of contractions of the heart. The term combines heartbeat disturbances that are different in their causes, clinical manifestations and consequences: increased heart rate (> 100 beats/min, tachycardia); slowing (<60 beats/min, bradycardia); irregularity (extrasystole).
To understand what cardiac arrhythmia is and why it occurs, you need to understand what natural mechanisms continuously maintain the heart rhythm throughout life.
Causes of cardiac arrhythmia
In practically healthy people, arrhythmia can occur due to overheating, being in a stuffy room, overeating, and also as a result of taking certain medications.
There is a high risk of this disease in patients suffering from diabetes, hypertension, and obesity. In women, arrhythmia is often detected during menopause and pregnancy, which is a temporary condition.
Much more serious causes are heart diseases: myocarditis, coronary disease, heart defects, myocardial infarction, malignant neoplasms. In these cases, arrhythmia is an indicator to which the doctor must pay close attention in order to prescribe the correct timely treatment.
Classification
In medicine, there are several types of arrhythmias - each of them has different symptoms and course, so it is necessary to diagnose not just the arrhythmia, but also its specific type - the choice of therapeutic therapy will depend on the results.
- Sinus arrhythmia. Most often diagnosed in childhood and adolescence, it is characterized by an abnormal alternation of heart beats. With this type of disorder in question, no specific treatment is required, the patient’s condition is not disturbed, and the normal rhythm of the heartbeat can be quickly restored by simply holding the breath for a few seconds.
- Sinus tachycardia is diagnosed if the heart rate exceeds 90 beats/min, of course, for no apparent reason (running, exercise, excitement). Typically, with such tachycardia, the heart rate does not exceed 160 beats per minute under calm conditions, and only during intense exercise can it reach up to 200 beats. It is caused by many factors associated with pathological processes in the body, therefore the treatment of such tachycardia is aimed at the underlying disease;
- Sinus bradycardia. This type of arrhythmia is manifested by a decrease in heart rate - in a patient this figure may be less than 55 beats per minute.
- Paroxysmal tachycardia, similar to extrasystole, developing suddenly and also suddenly stopping, is characterized by a regular, strict rhythm, although the contraction frequency can reach 240 beats/min (atrial) or pronounced changes in hemodynamics (ventricular);
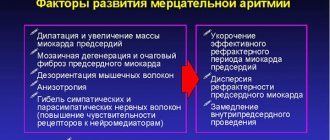
- Flickering arrhythmia. Doctors characterize this type of arrhythmia as fluttering in the chest - the heart begins to contract faster (up to 150 beats per minute), then even faster (up to 300 beats per minute), the atria do not contract completely, and the ventricles do so irregularly.
Ventricular flutter and fibrillation are considered the most life-threatening manifestations of arrhythmia. This usually occurs against the background of heart pathologies, electric shock, or taking certain medications.
High technologies in the treatment of cardiac arrhythmias
Republican Scientific and Practical Center "Cardiology"
D. Goncharik, leading researcher at the laboratory of cardiac arrhythmias, candidate of medical sciences, associate professor
Irregular or fast beating of the heart is called arrhythmia. There are many different types of arrhythmias - from the usually harmless atrial extrasystoles to the truly life-threatening paroxysms of rapid ventricular tachycardia. An episode of acute rapid heartbeat is called paroxysm. Many arrhythmias can respond well to treatment with medications or disappear with rest (vacation), reducing alcohol consumption, caffeine, and quitting smoking.
*****
However, in some patients, arrhythmias occur so frequently that they interfere with normal life or cannot be treated with medications. In such cases, modern cardiology has a wide arsenal of highly effective minimally invasive and surgical treatment methods. “Minimally invasive” means that elimination of arrhythmia is achieved using special catheters that are inserted into the heart through the vessels of the legs, without cutting the chest, and the patient is conscious only under local anesthesia, without experiencing pain.
This procedure is called ablation, a complex, high-tech heart surgery. On average it takes several hours. Such minimally invasive operations are the most effective method of treating heart rhythm disorders, as they allow patients to completely get rid of arrhythmia.
First, several catheters are inserted into the patient through the veins and/or artery of the thigh under local anesthesia - thin wires that make it possible to record an electrocardiogram of the heart directly from the inside. This is necessary to correctly establish the diagnosis and further treatment tactics. The doctor can control the movement of the catheter tip inside the patient's body using a special device. Such intracardiac cardiograms, recorded from several points, make it possible to most accurately diagnose arrhythmia and determine its source.
After the doctor determines the point in the heart that is responsible for the arrhythmia, it can be eliminated using a special ablation catheter. An ablation catheter differs from other catheters inserted into the heart in that its tip can heat up to 45 - 60 C and “cauterize” the source of the arrhythmia.
All ablations have some risks, although they are usually not particularly dangerous. Fortunately, complications occur in only about 1% of patients. The most common types of arrhythmias that can be successfully treated with catheter ablation in a single procedure are atrioventricular nodal and some other atrial tachycardias, atrial flutter and fibrillation, WPW, and some types of ventricular tachycardias. Unfortunately, not all types of arrhythmias can be successfully eliminated using modern treatment methods, but science and technology do not stand still and new technologies are being introduced every year.
*****
One of the most common types of tachycardia (fast heartbeat) in young people is atrioventricular nodal paroxysmal tachycardia. With such an arry inside the atrioventricular node (connection). To prevent repeated paroxysms of tachycardia, prophylactic administration of special medications may be required. However, most patients do not want to take medications for a long time: they stop taking them or take them irregularly, so attacks of arrhythmia recur. Lasting recovery of patients suffering from such tachycardia can be achieved by cauterization (ablation). To do this, it is necessary to cauterize a small area in the atria in the area of the AV junction and thus break the ring along which the arrhythmia “runs.” After this, it completely disappears and the patient feels like a completely healthy person.
Another arrhythmia that often requires calling an ambulance is arrhythmia in patients with Wolff-Parkinson-White syndrome (or WPW syndrome). WPW syndrome is a congenital defect—an additional abnormal conduction pathway (besides the normal atrioventricular junction) through which impulses can also travel from the atria to the ventricles and vice versa, causing severe cardiac arrhythmias. Some of these arrhythmias can be truly life-threatening.
Patients with WPW syndrome often require special medications to prevent heart rhythm disturbances. It should be noted that although medications can usually provide some control of arrhythmia attacks, complete resolution of symptoms cannot be achieved with medications alone. Therefore, many doctors recommend catheter ablation as the best treatment method.
It is often difficult to localize this additional pathway, but modern computer equipment can significantly increase the efficiency of operations.
One of the most common cardiac arrhythmias in middle-aged and elderly people is atrial fibrillation. In atrial fibrillation (AF), the upper chambers (atria) of the heart contract chaotically and uncoordinatedly (fibrillate) at a rate of approximately 400 times per minute. This chaotic heart rhythm has an adverse effect on the heart, which ultimately leads to the formation of heart failure.
In most cases, patients experience palpitations, dizziness, shortness of breath and fatigue. For some, atrial fibrillation is completely asymptomatic. The tricky thing about atrial fibrillation is that it can cause strokes.
A new episode of arrhythmia is called paroxysm. When AF paroxysm persists for a long time, blood clots (thrombi) can form in the atria, which travel through the bloodstream into the arteries and cause their blockage. The area of tissue that does not receive oxygenated blood dies. The most dangerous is the entry of blood clots into the arteries of the brain, which is accompanied by a stroke. To prevent strokes, patients must take blood thinners such as aspirin or warfarin.
Restoring the rhythm in a patient with atrial fibrillation can be achieved with pills or intravenous medications, or with an electrical shock (electrical shock therapy).
It is extremely important not to delay restoring the rhythm, because if paroxysm persists for a long time, this can be difficult. For example, if a patient's paroxysmal AF persists for more than 48 hours, clots may form in the heart. Before restoring the rhythm, the doctor must make sure that the patient does not have thrombi (blood clots) in the cavities of the heart. For this purpose, transesophageal echocardiography (ultrasound of the heart using a probe similar to a gastric tube) is performed or the drug warfarin is prescribed for 3 to 4 weeks immediately before the cardioversion procedure to thin the blood.
Although electrical cardioversion can restore normal heart rhythm in approximately 90% of patients, unfortunately, in a significant proportion of patients, the rhythm is re-disturbed within a year for various reasons. If AF recurs repeatedly, the doctor decides whether it is advisable to restore the rhythm again in a particular situation or whether it makes sense to transfer AF to a permanent (chronic) form.
Some patients cannot maintain rhythm with medication. There are modern surgical and minimally invasive treatment methods for them.
*****
The labyrinth type surgery is performed under general anesthesia while the heart is stopped. The right and left atria are cut with a scalpel and then stitched together. In this way, it is possible to form a normal “path” for the propagation of a normal rhythm from the atria to the ventricles. However, this operation is complex and requires cutting into the chest.
Physicians with experience in treating cardiac arrhythmias are constantly developing new methods to identify the sources of arrhythmia without cutting into the chest (mapping) or cauterizing the sources of atrial fibrillation so that AFib disappears once and for all.
The mapping and cauterization procedure has been in use since the late 1990s, with new variations being introduced every year. During the ablation procedure, doctors use special catheters to eliminate the sources of arrhythmia in the atria, and if there are too many such areas, they “isolate” them from healthy heart tissue by drawing circular ablation lines. This is a rather complex and lengthy procedure, lasting several hours. Sometimes it is carried out in several stages. The advantage of this invasive operation is that it is performed under local anesthesia; the patient is conscious, there is no need to cut the chest.
Currently, the best results are achieved using a special catheter navigation system inside the heart cavity (CARTO system), which allows you to control the catheter that cauterizes arrhythmia inside the heart cavities with an accuracy of 1 mm. This catheter allows you to build a map of arrhythmia.
The procedure is more effective for patients with frequent short paroxysms of AF; the effectiveness against long-standing AF is significantly lower.
The AF ablation procedure is not without risks. About 2 to 3% of patients experience serious complications such as blood leaking into the heart (tamponade), strokes, nerve damage, narrowing of the pulmonary veins, or a hole forming between the atria and esophagus (atrioesophageal fistula). Many of these complications are treatable but require the patient to remain in the clinic for an extended period of time.
Therefore, to decide on the advisability of a procedure, the doctor weighs the potential benefits and possible risks for a particular patient, choosing the optimal solution for the given case at the time.
*****
Atrial flutter is often an arrhythmia related to atrial fibrillation, in which the atria contract at a high rate of up to 200 to 300 beats per minute, and this rapid rhythm is conducted to the ventricles and causes them to contract at a rate of 100 to 150 beats per minute. This leads to rapid disruption of the normal pumping function of the heart. Treatment of atrial flutter with medications is usually ineffective.
The best treatment for atrial flutter is ablation (cauterization), which produces positive results in approximately 90% of patients.
Excessively fast heartbeats that originate from the heart's ventricles are called ventricular tachycardia (VT). This arrhythmia often poses a serious threat to the patient's life, often leads to loss of consciousness and requires the use of special medications, the use of invasive (catheter ablation) or even surgical treatments.
Typically, severe ventricular tachycardia is treated by sewing a special device under the skin - an implantable cardioverter-defibrillator (ICD), which allows you to interrupt severe attacks of arrhythmia using an electrical discharge from the inside.
Some forms of ventricular tachycardia are less life-threatening and occur in people with nearly normal heart function. Although these forms of the disease can be treated with medications, a permanent cure can be achieved with the help of an ablation procedure and save the patient from repeated breakdowns once and for all. Sophisticated computer systems make it possible to create a map of cardiac excitation during such tachycardia, which makes it possible to identify its source.
Often, a paroxysm of ventricular tachycardia develops into an even more severe arrhythmia - ventricular fibrillation (VF), in which the heart contracts uncoordinatedly at such a high speed that it is unable to pump blood, and this is tantamount to cardiac arrest. With ventricular fibrillation, a person always loses consciousness.
There are many causes of VT and VF, but most often it occurs due to disruption of the blood supply to the heart muscle due to narrowing of the coronary arteries or the presence of scars in the heart muscle. The most effective means of stopping repeated paroxysms of ventricular fibrillation (rhythm restoration) are implantable cardioverter defibrillators (ICDs).
An ICD is an implantable device (similar to a pacemaker) that monitors the heart's rhythm. Unlike a pacemaker (which prevents the heart from beating too slowly), an ICD can also detect and interrupt excessively fast heartbeats - ventricular tachycardia, as well as ventricular fibrillation. If a severe arrhythmia occurs, the cardioverter-defibrillator commands the restoration of the normal rhythm (using a series of rapid electrical impulses or an electrical discharge from the inside). Information about each episode can be downloaded using the programmer and can be read from the ICD memory without cutting the skin. The clinic of the Republican Scientific and Practical Center "Cardiology" has sufficient experience in treating such patients.
In general, the lives of patients with ICDs are almost no different from the lives of other people. Although ICDs successfully treat VT and VF but do not prevent them, patients should avoid situations where they might lose consciousness in a life-threatening situation, such as during unaccompanied swimming, etc. If the patient is touched by another person at the time of the shock, You may feel a slight, momentary tingling sensation, but it poses absolutely no danger. Modern ICDs last for four to six years before the generator needs to be replaced.
Electrical system of the heart
The heart has its own electrical (conducting) system, consisting of an electrical impulse generator - the main pacemaker (sinus node) - and conduction pathways (atrioventricular junction, His bundle and its branches) connecting the entire electrical circuit. The main pacemaker (sinus node), located in the right atrium, generates regular electrical impulses at a certain frequency, like a metronome. In response to each impulse, the heart contracts in a strict sequence - first the atria, then normally through a single connection (atrioventricular, in which its short-term delay occurs), the impulse passes to the ventricles, spreading through the system of fibers, causing the ventricles to contract synchronously.
Bradycardia and pacing
At rest, our heart beats at approximately 50 to 90 beats per minute, although athletes and patients taking certain medications, such as beta blockers, may contract slower. Heart rate increases during exercise, and the maximum varies greatly among individuals.
A slow heartbeat (bradycardia) may cause no symptoms or may cause dizziness, blurred vision, shortness of breath, or fatigue. Bradycardia can occur due to problems with the main pacemaker of the heart (sick sinus syndrome) or a delay in the impulse at the atrioventricular junction (heart block).
Patients with high-grade heart block and sick sinus syndrome usually have a pacemaker fitted.
Pacemakers
A pacemaker is an implanted device that monitors a person's heartbeat and prevents the heart from beating too slowly.
It consists of a “pulse generator” (the pacemaker itself) to which one or two wires (electrodes) are attached. Typically, the pacemaker is placed under the skin or in the muscle just below the collarbone. Almost all modern pacemakers work “on demand”, that is, they turn on only when necessary - when the heartbeat is too slow to set the correct rhythm. The rest of the time, the device only monitors the patient’s own heart rhythm without interfering with its work.
There are many different types of pacemakers available today. Belarusian clinics have all the necessary types. There are physiological pacemakers: they can recognize when the patient is sleeping or, conversely, doing hard work. In response to exercise (fast walking or running), the stimulator increases the heart rate, and at night, on the contrary, it works even slower than during the day at rest.
The service life of modern pacemakers under standard conditions is approximately 7 - 10 years, but can be much longer for a particular patient. The expiration date of the pacemaker battery can be easily predicted during the next scheduled check of the pacemaker.
The pacemaker imposes almost no restrictions on the patient's daily life. Household appliances and mobile phones do not interfere with the operation of the device, although you should not store a mobile phone in a pocket near a pacemaker.
Heart failure
With severe damage to the heart by various diseases, its pumping function gradually decreases. When the pumping function is significantly reduced, the heart is unable to pump the required amount of blood, which is called heart failure.
Most cases of heart failure are caused by the fact that the main pumping chamber of the heart (the left ventricle) cannot contract with sufficient force, but usually the right and left ventricles continue to contract synchronously (almost simultaneously).
Resynchronizing pacemaker
As heart failure increases, the right and left ventricles begin to contract at the same time - the contraction of the left ventricle or part of it is greatly delayed in relation to the right ventricle. Asynchronous contraction further reduces the efficiency of the heart's pumping function. To treat such patients, special stimulants are used. The goal of cardiac resynchronization therapy (CRT) is to stimulate the ventricles so that they contract simultaneously, thereby improving the pumping function of the heart.
In general, the implantation procedure is similar to the procedure for implanting a conventional pacemaker. The only difference is that an additional electrode is inserted to set the correct rhythm to the left ventricle and synchronize the work of the right and left ventricles.
Currently, implantation of pacemakers, including physiological ones, is performed in all regional centers of Belarus. Implantation of more complex devices - resynchronizing pacemakers and cardioverter-defibrillators - is carried out in the republic.
It is important!
Attacks of dizziness and loss of consciousness
Approximately 30 - 50% of people experience fainting or blackout at some point in their lives. Fainting occurs for a variety of reasons, but the immediate common cause is usually a sudden drop in blood pressure, which in turn leads to a short-term reduction in blood flow and oxygen delivery to the brain.
Usually, but not always, a person immediately before losing consciousness feels lightheaded or dizzy, and also complains of darkening of the eyes and ringing in the ears. In addition, nausea, vomiting, sweating, and rapid or slow heartbeat may occur.
Fainting among people of all ages is so common that many do not immediately perceive it as a serious threat to life and may seek professional help from a doctor only after a series of fainting spells, which is a mistake.
The most common type of fainting is due to improper reflex interaction between the cardiovascular and nervous systems, as a result of which the cardiovascular system selects a heart rate and degree of relaxation of the body’s blood vessels that is inadequate to the current situation. In addition to the so-called functional, or “reflex” forms of fainting, patients may also lose consciousness due to organic heart diseases: excessively fast or slow heartbeat, dysfunction of the heart muscle or heart valves, as well as diseases of the nervous system and overdose of drugs that lower blood pressure. Differential diagnosis usually requires an electrocardiogram, as well as an ultrasound scan of the heart or “echocardiogram”, etc.
Doctors may recommend that patients who complain of recurrent “reflex” fainting avoid certain situations that lead to fainting (for example, standing up on a crowded train in hot weather), wear medicated compression stockings, prescribe certain medications, and in some cases, get a pacemaker. if such fainting is accompanied by an excessive slowing of the heart rate.
To diagnose disease of the heart muscle and/or heart valves, certain non-invasive tests are available, such as 24-hour continuous recording of heart rate and rhythm using an ECG (Holter ECG monitoring). In some cases, invasive tests may be required, such as coronary angiography (cardiac catheterization) and/or specialized tests of the heart's electrical system, known as an electrophysiological study, or EPS.
In patients suffering from organic heart muscle disease, fainting often occurs due to an excessively fast heartbeat. In such a situation, the heart simply does not have time to emit the amount of blood necessary to ensure normal functioning of the brain, and the doctor may raise the question of a special heart operation to eliminate or cauterize the source of such arrhythmia. In some cases, it may be decided to implant a special device under the skin, similar to a pacemaker, which will restore excessively fast heartbeats using an electrical current discharge from the inside (ICD).
The main thing is that if fainting occurs, you should not wait for it to recur many times (since the second or third may already be the last), but quickly seek help from a specialist.
Symptoms of arrhythmia
Manifestations of rhythm changes can either be completely invisible to the patient, or have quite noticeable signs:
- sensations of heartbeats, interruptions;
- increased or slowed heart rate;
- feeling of a sinking heart;
- When blood flow is impaired, dizziness occurs and there may be episodes of loss of consciousness.
Rhythm disturbances can be permanent or occur in the form of paroxysms. In this case, an attack of arrhythmia occurs unexpectedly and also suddenly stops.
Clinical signs of atrial fibrillation
Atrial fibrillation, or atrial fibrillation, is the most common disorder, characterized by an increase in heart rate up to 600 beats per minute.
It can be constant, persistent and paroxysmal. The most common symptoms of atrial fibrillation include rapid heartbeat, shortness of breath, discomfort or stabbing pain in the heart area, increased sweating, increased urination and muscle weakness. Patients complain of a feeling of unreasonable fear, a state of panic, and dizziness and fainting are often observed.
Arrhythmia
Pyelonephritis
Thyrotoxicosis
Rheumatism
11436 09 April
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Arrhythmia: causes of occurrence, in what diseases it occurs, diagnosis and treatment methods.
Definition
The heart is a muscular organ, a pump that maintains a constant flow of blood in the vessels, generating impulses at a certain frequency that lead to excitation and contraction of the myocardium. Normally, the contraction of the heart’s parts occurs sequentially: first, the right and left atria contract, then the right and left ventricles.
The main source of heart rhythm is located in the right atrium - the sinus node, which in a healthy adult sets the correct heart rate rhythm (60-80 beats per minute).
In addition to the sinus node, other parts of the myocardium can generate impulses and set the rhythm, but in a healthy person they do not cause arrhythmias due to the adequate functioning of the sinus node.
The heart has the property of conductivity, i.e. the ability to quickly propagate an impulse throughout the myocardial tissue, which is necessary for the coordinated work of all cardiac muscle cells.
Cardiac arrhythmia is a condition characterized by a disturbance in the rhythm of the heart, the process of impulse formation and its conduction. Some arrhythmias at a certain age are considered normal, but most are still a sign of one or another pathology, and therefore require close monitoring and treatment.
Types of cardiac arrhythmias
Depending on the heart rate (HR), arrhythmias are divided into
tachyarrhythmias
(with an increase in heart rate of more than 80–90 beats per minute) and
bradyarrhythmias
(with a decrease in heart rate of less than 60 beats per minute).
Based on the location of the myocardial area, which is an abnormal source of rhythm, supraventricular (supraventricular) arrhythmias
, when the pacemaker is located in the atria or in the atrioventricular node, and
ventricular arrhythmias
, when the pacemaker is located in the ventricles of the heart.
One of the most important classifications of cardiac arrhythmias is based on the immediate cause of its development.
- Arrhythmias due to impaired impulse formation, which are based on impaired functioning of the sinus node, for example, sinus arrhythmia, sick sinus syndrome, etc. According to statistics, the prevalence of sinus arrhythmia (SA) in the general population is 33.9-34.5%, sinus bradycardia (SB) - 7.1-12.8%, sinus tachycardia (ST) - 4.9-9.8%.
- Arrhythmias due to changes in the automaticity of latent pacemakers, for example, replacement cardiac rhythms.
- Arrhythmias caused by abnormal circulation of the impulse in the myocardial tissue, for example, extrasystole, atrial fibrillation (atrial fibrillation), atrial flutter.
- Disturbances in the conduction of impulses through the myocardium:
- blockades, for example, atrioventricular block, right bundle branch block, etc.;
- premature excitation of the ventricles - the passage of an impulse along additional pathways, for example, Wolff-Parkinson-White syndrome.
Separately, there is a respiratory arrhythmia, which is normally observed in young children and consists of an increase in heart rate during inhalation and a slowdown during exhalation.
Possible causes of arrhythmia
Some of the causes of heart rhythm disturbances lie directly in the structure of the heart, while others are caused by external influences on the heart.
To the reasons of the heart
arrhythmias include congenital and acquired heart defects, consequences of myocardial infarction, inflammatory changes in heart tissue (carditis), heart tumors, cardiomyopathy (changes in normal myocardial tissue), etc. Long-term diseases of the endocrine system, arterial hypertension, alcoholism, etc. can lead to changes in the structure of the myocardium.
To extra-cardiac reasons
conditionally include those conditions that cause rhythm disturbances without leading to structural changes in the heart tissue: changes in the innervation of the heart, changes in the balance of electrolytes (potassium, magnesium, calcium) with damage to the kidneys, adrenal glands, parathyroid glands, with prolonged diarrhea or vomiting, with intoxication, other changes in metabolic processes.
What diseases cause arrhythmias?
- Coronary heart disease (a disease based on insufficient blood supply to the heart muscle, resulting in oxygen starvation of the heart) and the consequences of a myocardial infarction.
- Long-term arterial hypertension.
- Hypertrophic, restrictive, dilated (including alcoholic) cardiomyopathy, arrhythmogenic dysplasia of the right ventricle are pathological conditions based on restructuring of the myocardium with disruption of its basic functions.
- Heart defects, for example, mitral stenosis, aortic insufficiency.
- Congenital heart defects, manifested by numerous symptoms, incl. arrhythmia, already from childhood.
- Congenital anomalies of the cardiac conduction system, for example, an accessory bundle in Wolff–Parkinson–White syndrome.
- Inflammatory damage to the myocardium (carditis, myocarditis).
- Acute and chronic kidney diseases, leading to changes in electrolyte balance, restructuring of myocardial tissue: chronic kidney disease due to glomerulonephritis, pyelonephritis, etc., acute kidney injury.
- Diseases of the endocrine glands: hypothyroidism, hyperthyroidism, adrenal dysfunction, etc.
- Tumors of the heart and other organs.
Which doctors should you contact if you have an arrhythmia?
As a rule, arrhythmias are first diagnosed either during a medical examination or when a patient approaches with specific complaints. Deviations in heart rhythm require consultation to clarify the type of arrhythmia and conduct a comprehensive study of the state of the cardiovascular system.
If the cause of the rhythm change is of extracardiac origin, the patient may be referred to other specialists - a nephrologist. If systemic rheumatic diseases are suspected, observation by a rheumatologist is required.
Diagnostics and examinations for arrhythmia
The doctor may suspect arrhythmias when the patient complains of interruptions in the heart, a feeling of “fading” of the heart, fainting, and shortness of breath. The diagnosis algorithm consists of a thorough history taking, assessing the state of the cardiovascular system (listening to the heart with a stethoscope, feeling the pulse, measuring blood pressure, etc.). According to the clinical examination, the doctor assumes damage to one or another system and prescribes additional laboratory and instrumental examinations:
- electrocardiography (ECG) in 12 leads;
Symptoms of extrasystole
Extrasystole is a heart rhythm disorder characterized by the occurrence of one or more extraordinary contractions of the heart muscle. The most characteristic symptoms of the disease include strong heartbeats, a short stop and a subsequent noticeable shock.
Patients often complain of chest pain, lack of air, feelings of fear and causeless anxiety, and increased sweating. Depending on the location of the source of excitation, extrasystolic heart rhythm disturbances are atrial, ventricular and atrioventricular (atrioventricular).
Symptoms of sinus bradycardia
This type of arrhythmia is characterized by a heart rate not exceeding 60 beats per minute. Most often, bradycardia develops against the background of organic heart damage. Heart rhythm disturbances (heart rate below 40 beats per minute) are accompanied by weakness, sticky cold sweat, pain in the heart area, dizziness, instability of blood pressure, possible short-term loss or confusion, impaired memory and concentration, short-term visual disturbances.
The most dangerous condition with bradycardia is convulsions (Morgagni-Adams-Stokes attacks), lasting about a minute. In the absence of timely medical assistance, the attack can drag on and lead to respiratory arrest.
Modern methods of treatment
In some cases, arrhythmias occur due to bad habits, such as drinking too much alcohol. Giving up the habit will be a real help for arrhythmia. Reducing stress, avoiding caffeine, improving diet, and increasing the amount of exercise the patient does during the week can also reduce the incidence of arrhythmias. Before you begin making these changes, you should first talk to your doctor. For others, arrhythmias are a symptom of heart disease and will not go away unless the underlying problem is addressed. Fortunately, many people can benefit from invasive treatment of cardiac arrhythmias using modern medical interventions, especially surgery and special electrical devices.
Drug treatment for cardiac arrhythmia is also possible. There are several medications that can slow a fast heartbeat (known as "antiarrhythmic drugs"). Beta blockers are medications that are very useful in controlling heart rate in people with various heart conditions. Calcium channel blockers may also be used to control heart rate. Often these drugs can be used for more than one purpose (eg, to control heart rate, high blood pressure, protect the heart after a heart attack). The drug Digoxin is derived from a substance called Digitalis, which has been used for arrhythmias for over 200 years.
Other medications called antiarrhythmics can convert the abnormal rhythm to a normal one and prevent seizures from recurring (known as "rhythm control"). Patients with atrial fibrillation (AF) are usually prescribed the anticoagulant Warfarin, which thins the blood and prevents blood clots and strokes. Recent studies have shown that heart rate control and adequate anticoagulation are very important (perhaps even more important than rhythm control) for people with certain types of arrhythmias (eg, AF).
In some cases, AF returns to a normal rhythm with a treatment called cardioversion. The patient is given a small electrical shock that resets the heart's natural pacemakerSource: Innovations in the Treatment of Cardiac Arrhythmia. Zh.A. Arzykulov, A.A. Omarov, B.B. Kituev, F.A. Tursunova, A.A. Yeshtay, N.G. Pavlova. Bulletin of Surgery of Kazakhstan, 2012. p. 4-5.
Many arrhythmias can be completely treated with radiofrequency ablation. Thin catheters are passed into the heart to send radio waves directly to electrical pathways carrying inappropriate signals. These waves destroy abnormal tissue, preventing it from causing abnormal heart rhythms. Artificial pacemakers can take over the job of generating electrical signals. They are not limited to treating low heart rates, newer pacemakers can also control high heart rates. They can operate for up to 15 years on a single battery to prevent heart arrhythmia. Some save energy by turning off when the heartbeat is normal. Most units are placed under the skin, requiring only minor surgery.
Symptoms of paroxysmal tachycardia
Paroxysmal tachycardia is a pathological condition accompanied by paroxysms (attacks of palpitations) with a heart rate of 140-220 beats per minute. A suddenly developing and also suddenly subsiding disturbance of heart pulsation, characterized by a preserved regular rhythm, can have a different duration (from several seconds to several days).
Depending on the location of the source of excitation, paroxysmal tachycardia is divided into 3 forms: atrial, ventricular and atrioventricular. Attacks of arrhythmia are accompanied by dizziness, a feeling of numbness and compression in the chest, in the heart area, and tinnitus. Some patients may experience neurological symptoms (weakening of voluntary movements (hemiparesis), speech impairment). Also characteristic signs of paroxysmal tachycardia include a slight increase in body temperature, nausea, accumulation of gases in the intestines, and increased sweating.
After an attack, the patient develops polyuria (excretion of large amounts of low-density urine). With long-term supraventricular arrhythmia, a drop in blood pressure is observed, severe weakness develops, and fainting is possible.
Diagnostics
Symptoms of suspected arrhythmia need to be carefully checked. Alarming signs include not only rapid heartbeat, but also sudden cardiac arrest, pressure changes, weakness, alternating with drowsiness.
If you experience the above symptoms, it is time to see a doctor and undergo a full diagnosis. You should contact a cardiologist - first of all, he will begin to check the thyroid gland and identify possible heart diseases.
Many methods have been developed to diagnose arrhythmia. An electrocardiogram must be recorded - it can be short or long. Sometimes doctors provoke an arrhythmia to record readings and more accurately determine the source of the problem. Thus, diagnostics are divided into passive and active. Passive techniques include:
| Echocardiography | An ultrasonic sensor is used here. The doctor receives an image of the heart chambers, observes the movement of the valves and walls, and specifies their sizes. |
| Electrocardiography | Electrodes are attached to the patient's chest, arms and legs. The duration of the contraction phases of the heart muscle is studied and the intervals are recorded. |
| Daily ECG monitoring | This diagnosis is also called the Holter method. The patient carries a portable recorder with him at all times. This happens within 24 hours. Doctors receive information about heartbeats during sleep, rest and activity. |
In some cases, passive research is not enough. Then doctors induce arrhythmia by artificial means. Several standard tests have been developed for this purpose. Here they are:
- exercise stress;
- mapping;
- electrophysiological study;
- Tilt table test.
Arrhythmia. Why is it dangerous? How to restore heart rhythm?
Arrhythmia is not a specific disease, but only a medical term that indicates that the heart rhythm is disturbed. These disorders can be very diverse: increased or slowed heart rate, loss of some heartbeats or, on the contrary, extra heart beats out of sequence. There are also severe variants of arrhythmias that require emergency medical care, and without it quickly lead to death.
Examples of arrhythmia:
- tachycardia – the heart beats too fast;
- bradycardia – contraction frequency is low, less than 60 beats per minute;
- extrasystole - frequent extraordinary contractions of the heart;
- heart blockades - periodic cardiac arrest (one or more contractions may be missed due to impaired impulse conduction);
- atrial fibrillation - frequent contraction, desynchronization with the ventricles.
Some arrhythmias are not dangerous. They are only manifestations of certain diseases or physiological conditions not associated with heart damage. Other pathologies are very dangerous and have a poor prognosis if left untreated. Your doctor will help you understand what kind of arrhythmia you have, what causes it and how dangerous it is.
Causes of less dangerous arrhythmias:
- pregnancy;
- any surgical operations;
- disturbance of electrolyte metabolism (little magnesium, too much or little calcium in the body); taking medications;
- thyrotoxicosis or hypothyroidism (under or overfunction of the thyroid gland);
- professional sports.
At the same time, some arrhythmias are dangerous both in themselves and by the diseases of which they are symptoms. They occur against the background of myocardial infarction, heart failure, cardiomyopathy, and inflammatory heart diseases. Arrhythmias themselves can lead to the formation of intracardiac blood clots, strokes, cardiac arrest and sudden cardiac death.
Any arrhythmia requires diagnosis. An ECG will help evaluate the heart rhythm. The doctor will immediately determine which type of arrhythmia we are talking about. Further research will be aimed at finding out its cause.
Options to solve the problem:
- treatment of an underlying disease that disrupts the heart rhythm (for example, antihypertensive therapy for high blood pressure or thyroxine replacement therapy for hypothyroidism);
- eliminating the immediate cause of arrhythmia (prescribing magnesium and calcium supplements for a deficiency of these minerals, discontinuing medications that disrupt the heart rhythm);
- the use of antiarrhythmic drugs (symptomatic therapy, which is used as long as the arrhythmia persists);
- treatment of the underlying cardiovascular disease (for example, surgical correction of a heart defect or antibiotic therapy for myocarditis);
- surgical methods: implantation of a pacemaker, cardioverter-defibrillator.
If you experience interruptions in your heart function, contact a cardiologist at the Quantum Satis clinic. We have access to all modern laboratory and instrumental tests that will help determine the cause of the arrhythmia. If possible, the doctor will eliminate it or prescribe symptomatic therapy to normalize the heart rhythm.
Why is arrhythmia dangerous?
If we are talking about sinus tachycardia or bradycardia, the patient most often experiences severe discomfort during unexpected attacks: dizziness, rapid or slow heartbeat, nausea, fear. There is also general weakness and malaise.
These symptoms seriously affect your well-being, but are not life-threatening, and with the right regimen and treatment lead to complete recovery. Paroxysmal arrhythmia, which disrupts blood circulation and is an indicator of the presence of heart disease, requires a more serious attitude. Extrasystole can be deadly and indicate myocardial infarction or other serious pathologies.
Treatment of arrhythmia
Effective treatment of disorders of proper excitability and conduction in the heart requires not only an individual approach taking into account the existing pathology, but also a comprehensive examination for a targeted impact on the underlying cause of the disease.
The worst way to treat arrhythmias is considered to be advice from friends, because antiarrhythmic drugs require individual selection, which depends on the form of arrhythmia, the patient’s body’s response to treatment measures, the presence of concomitant diseases and simply one’s own sensitivity to the drug. One thing suits one, another suits another, so only a specialist in these matters can prescribe or advise.
However, some medications should still be considered, since patients follow new products and are very interested in their pharmacological effects.
- In case of overwhelming bradycardia, implantation of a pacemaker will be the most effective. It is recommended in cases where there are signs of AV block or heart rate drops below 40 times per minute. If the reduction in contractions is not so significant, then treatment is limited to medications.
- With atrial fibrillation, it is possible to prescribe medications during attacks, but if it is permanent, then drug therapy is required on an ongoing basis. Among the drugs, the most effective are novocainamide, quinidine, cordarone, propanorm, potassium preparations, and sedatives. In some cases, electrical cardioversion may be performed. It is most effective in the first 48 hours from the moment the flicker develops and can be medicinal or electrical. In both cases, it is aimed at coordinating the contractions of the ventricles and atria in the correct rhythm. At a later date, attempts to normalize heart function may be less effective due to the development of thrombus formation in the vessels and inevitable stroke.
As for respiratory arrhythmia, it does not require special treatment, and in the case of sinus tachycardia not associated with the act of breathing, treatment is aimed at eliminating the underlying disease that caused this pathology.
BY THE WAY
Experts give the following advice on preventing arrhythmia:
- To keep your heart working smoothly, include oranges, pears, raspberries, and currants in your diet. In winter, let it be frozen berries, it’s still good. The diet should also include red sweet peppers, tomatoes, beets, parsley, apples, and corn;
- a very healthy mixture of honey, walnuts, lemon, dried apricots and raisins. These products contain a lot of potassium, magnesium, calcium, which are needed for normal heart function;
— for arrhythmia and cardiovascular diseases, it is better to drink mint tea. Mint relieves irritability and calms. In this case, you should keep the liquid in your mouth longer and drink it in small sips. You could also take a mint candy before bed;
- An infusion of viburnum berries is also useful. It contains a large amount of vitamin K, which has a beneficial effect on the heart and blood vessels and normalizes cardiac activity. Viburnum is also rich in vitamin C, which strengthens the immune system, and vitamin P, which is necessary for the body to absorb ascorbic acid. This is why viburnum is indispensable for high blood pressure. The recipe is simple:
Pour 1 cup of fruit with 1 liter of hot water, put on low heat and let boil for 10 minutes. Then strain and cool. Drink half a glass three times a day;
— what about coffee? Scientists have come to the following conclusion: if a strong coffee overdose can lead to arrhythmia, then a couple of cups of good grain coffee a day, as it turns out, for some reason stabilize the heart rhythm. This mainly concerns atrial fibrillation.
#diseases #heart #health
The material was published in the newspaper “St. Petersburg Vedomosti” No. 094 (6692) dated 06/03/2020 under the title “If the heart beats out of sync.”
Share on VKontakte Facebook
Cool
How to treat cardiac arrhythmia at home?
You can try to treat arrhythmia at home, but remember that arrhythmia and arrhythmia are different. In some forms, even drug treatment does not respond, but in simple cases, the power of plants may help.
- It is highly advisable to start treating arrhythmia at home with nutrition and daily routine. As with any other cardiac pathology, the patient is prescribed diet No. 10, excluding fatty, fried, pickled, spicy, and salty foods. Meals should be fractional, since a significant portion of food taken at large intervals can itself provoke arrhythmia (food load). Indulging in strong coffee and teas, and even more so, drinks containing alcohol, will not lead to good either; they can become sources of rhythm disruption.
- Infuse 1 tbsp. dried calendula flowers in half a liter of boiling water for an hour. Take half a glass of infusion half an hour before meals three times a day. It is useful to consume up to 20 drops of alcohol tincture on a piece of sugar 2 hours after meals.
- Crush three glasses of viburnum berries and place in a three-liter jar. Pour boiling water to the top, close the lid and place the jar in a warm place. After a few hours, strain and add honey to taste. Store in a cellar or refrigerator. Drink 1/3 cup half an hour before meals for thirty days. It is most effective to treat cardiac arrhythmia in three courses, taking weekly breaks.
- Heart arrhythmia is treated with dill seeds. Pour 200 ml of boiling water over a third of a glass of seeds and leave for 15-20 minutes. Take 1/3 cup half an hour before meals.
- Hawthorn tincture, purchased at a pharmacy, is taken 30 drops before meals.
- Brew 20-30 hawthorn berries with a glass of boiling water, leave for 15 minutes. Drink throughout the day, dividing into equal portions.
- Brew 1 tsp. dried hawthorn flowers or leaves with a glass of boiling water, leave for two hours, strain. Take 50 ml half an hour before meals.
- Grind turnips, 2 tbsp. Brew a glass of boiling water, simmer in a water bath for 15 minutes. Leave for half an hour, strain. Take half a glass half an hour before breakfast and lunch. Then prepare a fresh decoction.
- Wash 5 lemons, cut, remove seeds, mince. Add 30 crushed apricot kernels, 300 g of honey. Mix thoroughly and wait at room temperature for 8-10 hours. Keep refrigerated. Take 1 tbsp. after breakfast and dinner.
- If sleep is disturbed and you cannot fall asleep, you can prepare the following composition. Mix lemon balm leaves and valerian roots, taken in equal parts, with three parts of yarrow herb. Pour the resulting mixture with 250 ml of cold water and leave for 3-4 hours, simmer for a quarter of an hour in a water bath, strain. Treat yourself with the resulting decoction, taking a few sips every day.
- Brew a glass of boiling water with 4 calendula flowers and 1 tsp. mint tea, insist. Take with honey four times a day.
It’s great if, with the help of folk remedies, arrhythmia is forgotten, but if it still continues to bother you, then with this problem you need to go straight to the doctor to find out its origin, the degree of danger and choose treatment.
First aid for an arrhythmia attack
Defibrillators are devices that restart blocked heart muscles by delivering electricity to the chest. Defibrillators are effective in stopping the heart from ventricular fibrillation, but because ventricular fibrillation can be fatal in less than 4 minutes, they should be used as soon as possible. Most defibrillators are external devices, but there are now automated implantable cardioverter/defibrillators (AICDs). These devices can be as large as pacemakers. They can detect dangerous fibrillation and return the heart to normal before any damage is done.
Article sources:
- "New Theory of Arrhythmia" clarifies the causes of arrhythmia. Ermoshkin V.I. Educational bulletin “Consciousness”, 2015. p. 22-30
- Innovations in the treatment of cardiac arrhythmia. Zh.A. Arzykulov, A.A. Omarov, B.B. Kituev, F.A. Tursunova, A.A. Yeshtay, N.G. Pavlova. Bulletin of Surgery of Kazakhstan, 2012. p. 4-5
- On the issue of classification of cardiac arrhythmias. Batyanov I.S., Batyanova E.I. Cardiovascular therapy and prevention, 2005
- A look from the inside focuses on a patient with arrhythmia. Boqueria O.L. Annals of Arrhythmology, 2014. p. 196-199
- Cardiac arrhythmias from the point of view of their dimension. Ubiennykh A.G. Measurement. Monitoring. Control. Control, 2021. p. 70-76
- Epidemiology of arrhythmias (review of literature data). Zatonskaya E.V., Matyushin G.V., Gogolashvili N.G., Novgorodtseva N.N. Siberian Medical Review, 2021. p. 5-16