Many patients, having received information about the presence of osteophytes, begin to associate the presence of back pain with osteophytes in the spine. However, bone growths (osteophytes) themselves are only a sign of degeneration in the spine and the presence of osteophytes does not necessarily mean that they are the actual cause of back pain.
In principle, osteophytes are a radiological marker of degenerative changes in the spine, and their appearance only means involutional changes in the spine. Over the age of 60, osteophytes (bone spurs) in the spine are quite common.
What are osteophytes
“Osteo” means bone in Greek, and “phyto” means plant. Growths form along the edges of bones, in areas that are subject to maximum stress. In the hip joint, this is, for example, the inner surface of the acetabulum. Thinning cartilage does not absorb the load, so the bones rub intensely.
Since the joint is not able to independently restore damaged cartilage, a compensatory mechanism is activated in the body. To prevent bones from being destroyed, osteophytes are formed, which slow down movement and stop the destruction of the joint capsule. This is how pathological ossification of the musculoskeletal system occurs. Thus, osteophytes are the body’s response to increasing load.
Osteophytes and deposits of calcium salts are formations of different structures
Arthroscopic findings
On arthroscopy, osteophytes appear much larger than on radiographs. Typical sites of osteophyte formation:
- Anterior edge of the tibia (most often).
The sizes of osteophytes on the anterior edge of the distal segment of the tibia vary from small (several mm) to large, extensive exostoses that complicate the study of the talotibial joint .
Such osteophytes often cause reactive synovitis of the anterior capsule. Usually, a partial synovectomy is necessary to determine the size of the osteophyte. Unstable osteophytes can behave like fixed intra-articular bodies, periodically causing ankle blocks.
If an osteophyte of the tibia of any location is detected, it is necessary to examine the anterior area of the ankle joint with its maximum dorsiflexion. Even small osteophytes In the later stages of the disease, secondary osteophytes of the talus are detected.
- Osteophytes of the talus.
Osteophytes of the talus most often occur on its medial and lateral surfaces and usually accompany osteophytes of the anterior edge of the tibia. Their size varies from a few millimeters to extensive exostoses that create a mechanical obstacle to dorsiflexion. Partial synovectomy is usually necessary to adequately evaluate these osteophytes.
- Medial malleolus.
Osteophytes of the medial malleolus, while less common than osteophytes of the anterior ankle, may nevertheless interfere with arthroscopic visualization of the anteromedial compartments. A partial synovectomy is usually necessary to evaluate them.
- Lateral malleolus.
Osteophytes of the lateral malleolus are relatively rare. Scar processes are much more common in this area.
- Posterior edge of the tibia.
Osteophytes in this area often accompany osteophytes of the anterior edge of the tibia. Osteophytes of this location are usually not diagnosed due to the fact that the posterior parts of the tibia are rarely examined during arthroscopy .
With a pronounced degenerative process of the ankle joint, in addition to osteophytes, deep damage and generalized reactive synovitis .
Reasons for the formation of osteophytes
Bone growths in joints are formed:
- due to injuries or bruises;
- as a result of inflammation of bones or nearby tissues;
- due to congenital or acquired dystrophic changes in the joints, for example due to endocrine disorders.
Most often, osteophytes cause age-related changes in joints or result from wear and tear of cartilage. In the second case, this occurs due to the same type of physical activity or sports overload. When hyaline cartilage fails, ossified areas appear in its place, limiting mobility.
Osteophytes are formed in those who load the joint with the same type of work.
Osteochondrosis
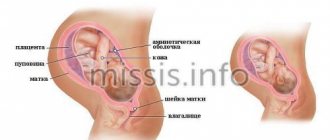
Behind the term “osteochondrosis” is a large group of pathologies that lead to degenerative processes affecting the intervertebral discs. As a result, they become smaller, delaminate, lose elasticity and ultimately rupture, leading to the formation of a protrusion or intervertebral hernia.
Osteochondrosis is considered to be the starting point for the development of other DDDDs, but in itself it is not their cause. A predisposition to osteochondrosis can be hereditary, but more common causes include metabolic disorders, posture and physical inactivity (weak back muscles, poor circulation and, accordingly, nutrition of the intervertebral discs).
Provoking factors
Arthrosis takes a long time to progress. In order for it to move from the chronic first stage to the pathological, painful second stage, a push is needed. Such provoking factors are:
- injuries, for example, a fracture of the middle part of a tubular bone (osteophytes form in the form of callus along the edges of the fracture);
- rupture of the periosteum (with the help of osteophytes, the body tries to connect the periosteum to the bone);
- inflammatory processes (with arthritis, osteomyelitis, brucellosis);
- malignant joint diseases, such as sarcoma.
4
If you have arthritis, your risk of osteophytes forming in your joints increases.
Symptoms of osteoporosis of the spine
Osteoporosis can occur for a very long time without any symptoms. In the early stages, you can determine it by measuring your height and comparing it with what it was at 20-25 years old. Also, changes in posture will indicate osteoporosis of the thoracic spine or cervical spine.
As osteoporosis of the spine develops, the following signs appear:
- Pain. It occurs mainly under compression loads. This could be a fall or lifting something heavy. Osteoporosis of the lumbar spine is manifested by pain with sudden turns of the torso. The pain syndrome may subside 4-6 weeks after onset. If the spine is affected by multiple microfractures, this leads to modification of the vertebrae and their gradual bending. Patients in this case experience periodic pain, which worsens when laughing, sneezing, coughing, or changing body position after sitting for a long time.
- Decreased growth. The difference between previous and current indicators can be 10-15 cm.
- Osteoporosis of the thoracic spine is manifested by a decrease in the size of the chest. Because of this, the arms look unnaturally long.
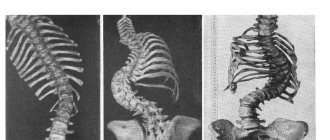
- Spinal deformity. Occurs when more than one vertebra is affected by the disease. Typically, such symptoms are caused by osteoporosis of the lumbar spine when 1-2 vertebrae are affected. Deformation also occurs when the thoracic region - 10-12 vertebrae - is involved in the process. As a result, the person becomes stooped, and as the disease progresses, a hump or humps may form.
- Reducing the distance between the pelvic bones and the rib area. In this case, a person with osteoporosis of the spine feels pain in the side.
- Pain in the vertebrae on palpation. This symptom occurs with a recent compression fracture.
- The pathological process may involve nerve roots and the spinal cord. In this case, a variety of dysfunctions arise: from loss of sensitivity in some parts of the body to paralysis of the limbs.
- Osteoporosis of the cervical spine causes pain after long periods of sitting or standing, weakness and soreness in the arms, discomfort in the shoulder girdle, headaches, surges in blood pressure, numbness, tingling and cramps in the arms.
- Brittle hair, deterioration of teeth and nails.
How to fight osteophytes today
The fight against osteophytes is part of the general treatment regimen for coxarthrosis, gonarthrosis or arthrosis of another joint. It is almost impossible to get rid of bone growths. The goal is to reduce pain and expand the range of motion. For this purpose, depending on the stage of arthrosis, the patient is prescribed:
- ointments to reduce unpleasant symptoms, such as hydrocortisone;
- non-steroidal anti-inflammatory drugs in the form of tablets or injections into the joint;
- physiotherapy - laser, magnets, electrophoresis, shock wave treatment.
One of the physiotherapeutic methods of combating pain due to arthrosis is magnetic therapy. What is it based on and why it helps, says the specialist:
Advantages of treatment at Top Ikhilov
- Qualified doctors with extensive experience.
- Advanced medical equipment for the diagnosis and surgical treatment of spinal diseases.
- Minimally invasive and robotic spine surgeries, after which patients recover in a matter of days.
- Loyal pricing policy, the possibility of stage-by-stage payment for each service performed.
- Extensive experience working with foreign patients. Availability of an international department and a staff of professional translators (if necessary).
- Accompanying a foreign patient at all stages of diagnosis and treatment of the disease.
- The opportunity to combine treatment with a holiday in Israel.
- 5
- 4
- 3
- 2
- 1
(8 votes, average: 4 out of 5)
Is surgery necessary?
If conservative treatment does not help and the patient continues to experience pain, there are two options. Bone formations can be removed surgically. True, this will have to be done regularly, since the problem will not disappear, and osteophytes will continue to form with enviable frequency. Therefore, it makes sense to act radically.
With the help of intra-articular injections of a synovial fluid prosthesis, for example, Noltrexin, it is possible to move the rubbing surfaces apart. Thinning cartilage no longer rubs, and the body does not receive a signal about the need for compensation. Under such conditions, when there is enough synovial fluid, despite damaged cartilage, osteophytes do not form.
Before deciding to have surgery, weigh the pros and cons. Osteophytes in the joints severely limit mobility. But to get it back and get rid of the pain, it is not at all necessary to undergo surgery.
Diagnostics
Diagnosis of the cervical spine in Israel takes 3 days. During this time, doctors manage to establish a diagnosis and prescribe a set of treatment measures.
First day – consultation with a doctor
Diagnosis of any disease in Top Ikhilov begins with a consultation with the attending physician. It is noteworthy that you can get a second opinion from an Israeli specialist without visiting Israel. To do this, you will need to send diagnostic data to our clinic, after which you will be scheduled for a video consultation with our doctor. If after the video consultation you decide to be treated in our clinic, then the initial in-person consultation will be free for you.
During the initial examination, the doctor examines medical documents in detail, asks the patient about the symptoms of the disease and examines the patient. Then the doctor refers the patient to undergo instrumental examinations of the cervical spine.
Second day – instrumental diagnostics
- X-ray studies of the cervical spine.
- CT and MRI.
- Myelography.
- Electromyography.
- Electroneurography.
- Other research methods.
Third day – doctors’ conclusions
On the third day of diagnostic activities, an expert group of doctors Top Ichilov studies the diagnostic data in detail, establishes an accurate diagnosis and determines the treatment tactics for cervical osteophytes.
Calcaneal spines
Osteophytes on the heel (according to IBC 10, the disease is numbered M25) develop due to calcium metabolism disorders or due to inflammatory processes in the foot. Heel growths are diagnosed in 50% of people with severe diseases of the spine or joints.
Symptoms and treatment of osteophytes on the heel are determined by the degree of neglect of the pathology and its root cause. Therapy for such patients is only comprehensive.
If osteophytes do not interfere with a person’s walking and do not cause severe pain, they can be treated with folk remedies to alleviate the condition.
For large osteophytes affecting the heel bone and soft tissues, surgical treatment is indicated (can be practiced in Israel and other countries). However, surgical treatment is very painful and cannot always completely eliminate the pathology.