Vaginal dysbiosis (dysbacteriosis) is a disruption of the normal microflora of the vagina. Most women suffer from this disease to one degree or another.
When the microflora is disturbed, the balance between the bacteria that are normal inhabitants of the vagina changes. At the same time, the number of lacto- and bifidobacteria decreases and the number of some other pathogen increases. This other pathogen may be one of the key cells (then gardnerellosis, candidiasis, etc. develop), it may be one of the sexually transmitted infections (trichomoniasis, chlamydia), or it may be any saprophytic pathogen (Escherichia coli, Proteus, streptococci, staphylococci etc.).
Vaginal dysbiosis and genital infections
Sexual infections are always associated with a violation of the vaginal microflora. On the one hand, normal microflora will not allow the development of a sexually transmitted infection in a woman, and if a sexually transmitted infection is detected, the microflora cannot but be disturbed. On the other hand, the appearance of a pathogen of any sexually transmitted disease (STD) in the vagina shifts the pH, causes an inflammatory reaction and further contributes to the progression of microflora disorders.
A situation in which only one STD pathogen lives in a woman’s vagina almost never arises. Sexually transmitted infections, one or more, are always in association with opportunistic microflora. And this should always be taken into account when treating STDs. Otherwise, a situation may arise in which antibiotics completely kill the STD pathogen, and the number of opportunistic infections only increases.
STD treatment
in women, it must necessarily end with the restoration of the vaginal microflora. If we are talking about serious infections (chlamydia, trichomonas) or several STDs, then it first makes sense to carry out antibacterial therapy against them, and then begin to restore the vaginal microflora in the next course. In less complex situations, it makes sense to first carry out a comprehensive diagnosis of the entire urogenital microflora, and then restore it while simultaneously eliminating sexually transmitted infections.
Smear standards for flora
Normally, among the microorganisms that make up the vaginal biocenosis there are lactobacilli, gram-positive bacilli, bifidobacteria, opportunistic microorganisms and fungi.
In a healthy woman, about 90% of the microflora is made up of beneficial bacteria. These microorganisms prevent the proliferation of conditional pathogens and fungi, releasing special substances that have an antibacterial effect. When the number of beneficial bacteria decreases, conditional pathogens begin to grow. This condition is called flora dysbiosis and requires therapy. Treatment consists of strengthening the immune system with probiotics. In some cases, your doctor may prescribe antibiotics. Among other microorganisms, the smear may contain staphylococci, streptococci and other bacteroids. Their number should not exceed 5% of the total bacterial mass.
The norm of leukocytes in a vaginal smear is from 0 to 15 units. In the urethra and cervix - up to 10 units. Leukocytosis is considered a condition in which their number in the analysis exceeds 15 or more units. As a rule, during pregnancy and during the recovery period after childbirth, this figure increases slightly. Such leukocytosis does not have any accompanying symptoms and does not cause discomfort in the woman.
The smear results contain small numbers of squamous epithelial cells. Their level in women correlates depending on the day of the menstrual cycle. If there are many such cells in the analysis, and they are visualized in layers, this may be the result of an inflammatory process in the vagina.
Another indicator of the study is the mucus secreted by the glands of the cervical canal. If such mucus is found in excess, this may be a sign of acute or chronic cervicitis.
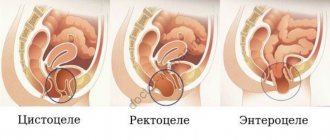
Vaginal dysbiosis and intestinal diseases
Many diseases of the gastrointestinal tract lead to disruption of the normal intestinal microflora and the development of dysbacteriosis. With intestinal dysbiosis, approximately the same thing happens as with vaginal dysbiosis - a large number of some bacteria live in the intestines.
The wall of the rectum is in close contact with the wall of the vagina, bacteria easily pass through it. In cases of severe intestinal dysbiosis, disruption of the vaginal microflora is always caused by this, and as a rule, one of the intestinal infections is sown from the vagina - Escherichia coli, enterococci, etc.
Treatment of vaginal dysbiosis
in such a situation it is extremely difficult, the probability of relapse of the disease is very high. Restoring normal vaginal microflora in such a situation is possible only with simultaneous treatment of intestinal diseases.
Are there factors contributing to the development of vaginal dysbiosis?
An unfavorable environment, decreased immunity and the stress in which we live leads to a weakening of the body’s natural strengths and can contribute to a decrease in its protective functions. In addition, there are a number of factors that increase the risk of vaginal pH imbalance.
- Improper intimate hygiene: vaginal douche, use of inappropriate detergents, too active and frequent vaginal hygiene
- Using antibiotics, especially on a regular basis and without consulting a doctor
- Intestinal dysbiosis
- Some methods of contraception: intrauterine device, condoms with antibacterial lubricant, external contraceptives containing antiseptics
- Endocrine changes in the body: menstruation, pregnancy, menopause
Measuring the acidity of the vagina - at an appointment with a gynecologist, will help to immediately determine whether you have signs of infection and will allow you to begin treatment immediately.
Vaginal dysbiosis and sexual partner
Most often, a violation of the vaginal microflora in a woman does not cause any problems for her sexual partner, even with regular sexual activity without the use of contraception. In some cases, when there is severe vaginal dysbiosis, a man may develop the phenomena of balanoposthitis and nonspecific urethritis. But this usually only happens if the man already had a predisposition to these diseases; they will not develop in a completely healthy body.
No disease of the sexual partner, with the exception of sexually transmitted diseases, has an effect on the vaginal microflora in a woman. Treatment of vaginal dysbiosis in women does not require mandatory treatment of the sexual partner, unless at least one of them is diagnosed with a sexually transmitted infection.
Vaginal pH, video
Vaginal ph. Source – Yulia Oliynyk
The doctor decides how to reduce acidity in the vagina for faster and more successful conception. At the same time, he prescribes a series of tests aimed at examining both partners. Home methods of reducing vaginal acidity (for example, using soda douching) can harm women's health.
To protect yourself from possible pH imbalances, it is important to select suitable intimate hygiene products that do not negatively affect acidity levels. To do this, we recommend that you familiarize yourself with the washing gels for intimate hygiene “Ginocomfort”. Thanks to their balanced composition, these products maintain the physiological level of acidity and at the same time have a delicate cleansing effect.
If you already have an imbalance in your pH level, you can reduce its manifestations with the help of the intimate moisturizing gel "Gynocomfort".
It was developed by specialists from the pharmaceutical company VERTEX, has undergone clinical trials and has a package of necessary documents and quality certificates. Testing of the gel, carried out at the Department of Dermatovenereology with the clinic of St. Petersburg State Medical University, showed its good tolerability by women, the absence of side effects and allergic reactions. The product helps to cope with vaginal dryness, itching and burning - common symptoms of both increased and decreased acidity of the vagina. Sources:
- STATE AND REGULATION OF NORMAL MICROBIOCENOSIS OF THE VAGINA. Orlova V.S., Naberezhnev Yu.I. // Scientific bulletins of Belgorod State University. Series: Medicine. Pharmacy. – 2011. – No. 22 (117). – pp. 15-21.
- HORMONAL STATUS AND VAGINAL MICROBIOCENOSIS. Dobrokhotova Yu.E., Zatikyan N.G. // Obstetrics, gynecology and reproduction. – 2008. – No. 2. – P. 7-9.
- Anaerobic microflora of the female reproductive tract. Valyshev A.V., Elagina N.N., Bukharin O.V. // Microbiol. - 2001. - No. 4, pp. 78-84.
- Bacterial vaginosis - modern concepts, complex treatment. Tikhomirov A.L., Oleinik Ch.G., Sarsania S.I. // Guidelines. – M. – 2005. – P. 5–7, 11–18.
- Microecology of the vagina. Microbiocenosis in normal conditions, in pathological conditions and methods for its correction. Kafarskaya L.I., Efimov B.A., Pokrovskaya M.S. // Lecture. – M. – 2005. – P. 1-5.
- https://www.researchgate.net/publication/11817901_Origins_of_vaginal_acidity_high_DL_lactate_ratio_i…
- https://www.medicalnewstoday.com/articles/322537.php
- https://www.frontiersin.org/articles/10.3389/fmicb.2016.01936/full
- https://www.pubfacts.com/detail/16859053/Association-of-bacterial-vaginosis-trichomonas-vaginalis-an…
Vaginal dysbiosis and pregnancy
Pregnancy is one of the factors that can provoke an exacerbation of vaginal dysbiosis. During pregnancy, discharge, itching or burning in the genitals, pain during intercourse, etc. may appear or intensify. This is due to the fact that during pregnancy a woman’s body undergoes serious hormonal changes, which cannot but affect both the immune system and the vaginal microflora.
Complete treatment of vaginal dysbiosis during pregnancy is not possible. Even if this treatment is not associated with taking antibiotics, which is extremely undesirable during pregnancy, it is always associated with immunocorrection, and this is completely unacceptable during pregnancy. Therefore, the doctor’s task during an exacerbation of vaginal dysbiosis in a pregnant woman is only to eliminate the symptoms and prepare the woman for childbirth.
In our clinic, for this purpose, a course of procedures is carried out that, if not normalize the situation, then make it more tolerable. Local treatment carried out in this case is completely harmless to the fetus. If necessary, this treatment can be carried out repeatedly throughout pregnancy.
Vaginal acidity test
Test strips for determining vaginal pH
There are special test strips for determining vaginal pH, which help identify the level of acidity at home, without contacting a gynecologist. They are freely available, sold in most pharmacies and available without a prescription.
Test strips for determining vaginal acidity are small pieces of special gray-green paper. To check the pH yourself, you need to open the test package immediately before taking the measurement, since prolonged exposure to air can affect the accuracy of the test strip. Next, you need to apply the strip to the vaginal wall for a few seconds (the exact time is usually indicated by the manufacturer on the packaging), then remove it and compare it with the color scale included in the test kit. When exposed to an acidic environment, the color of the strip changes, and this helps determine changes in the acidity of the vagina. If the result does not correspond to any of the given shades of the verification scale, you need to select the closest color.
Vaginal dysbiosis in girls
Disorders of the vaginal microflora occur in girls who have not begun sexual activity with approximately the same frequency as in women who are sexually active. This is due to several other factors - hormonal instability, the formation of a cycle, as well as the anatomical features of the structure of the hymen.
Vaginal dysbiosis in girls rarely manifests itself as heavy discharge, since the openings of the hymen, as a rule, do not allow them to be removed from the vagina in the quantity in which they are formed. Therefore, stagnation of vaginal discharge develops, and the likelihood of developing inflammatory diseases in virgins is higher. On the other hand, when sexual activity begins with the first sexual intercourse, a large number of bacteria are thrown from the vagina into the bladder, and this can lead to the so-called “honeymoon cystitis”.
Treatment of vaginal dysbiosis in virgin girls is somewhat difficult due to the fact that the structure of the hymen does not always allow for proper treatment of the vagina with medications. In some cases, it is even necessary to resort to artificial disruption of the integrity of the hymen - hymenectomy.
At SM-Clinic, gynecologists, after conducting examinations and tests, will identify the exact causes of vaginal dysbiosis and prescribe effective comprehensive treatment that will lead to the restoration of normal vaginal microflora.
Why do you need a flora smear?
A gynecological smear is what the doctor should first recommend at the initial appointment, regardless of the symptoms. This study, along with colposcopy, is included in the gold standard for annual preventive examinations in women. Smear microscopy allows you to assess the condition of the vagina and the presence/absence of an inflammatory process in the organs of the reproductive system. The laboratory technician will see the number of leukocytes, epithelial cells and the ratio of bacteria on the slide. If cocci predominate over beneficial bacilli in the results or fungi are visualized, this means dysbiosis, inflammation or candidiasis. If the number of leukocytes in the smear is increased, the gynecologist may prescribe additional tests for STIs.
Popular questions
I need a product with a neutral ph, and another very important point is that I am allergic to many intimate hygiene products from well-known brands.
Are your products hypoallergenic and what can you recommend to me? In your case, Ginocomfort gel with mallow extract is suitable if you are not allergic to its components indicated in the instructions.
Hello, what is the pH of the creams?
Gynocomfort gels containing lactic acid (washing gel for intimate hygiene and restoring gel with tea tree oil from the Gynocomfort line) have a pH of 4.2, which corresponds to the slightly acidic environment of the genital tract. Gynocomfort moisturizing gel has a neutral pH environment.
I can’t find a gel with a neutral pH (lichen sclerosus).
Hello! In your case, Ginocomfort gel with mallow extract is suitable. This will provide anti-inflammatory and moisturizing effects. The gel is applied once a day, the duration of use is not limited.
Hello, is it possible to use GINOCOMFORT intimate restorative gel for everyone to prevent problems, or are there any contraindications?
Hello!
Gels from the Gynocomfort line can be used as prophylactic agents. Contraindication is individual intolerance to the components of the product. For an accurate diagnosis, contact a specialist