Dysbiosis, or dysbacteriosis, is characterized by a violation of the vaginal microflora, its properties, qualitative and quantitative composition. As a result of this disease, pathogenic microorganisms begin to multiply, which lead to the development of more dangerous infections.
The first symptoms of the development of vaginal dysbiosis are easy to miss. That is why you need to undergo regular gynecological examinations in order to detect the disease in time and prevent complications. Visits to the doctor are especially important during pregnancy, menopause and puberty.
Causes of vaginal dysbiosis
The vaginal microflora of a healthy woman consists of approximately 95% lactobacilli. About 5% are all other microorganisms, including bifidobacteria and opportunistic bacteria, including mycoplasmas, gardnerella, and Candida fungi. However, at different periods of life, the vaginal microflora changes. Thus, during pregnancy, the number of bifidobacteria increases, and in girls before menarche, micro- and anaerobic bacteria predominate. The pH value under normal conditions does not exceed 4.5.
In case of a sharp change in the balance (a decrease in the number of lactobacilli and an increase in opportunistic microorganisms), dysbacteriosis develops. In this case, anaerobic bacterial flora predominates in the microflora, and the pH level increases to 5–6. This happens under conditions favorable to pathogenic organisms, which include:
- hormonal changes;
- sexually transmitted diseases;
- promiscuous or unprotected sexual intercourse;
- infectious or inflammatory diseases of the genital organs;
- abuse of douching;
- wearing synthetic underwear;
- hypothermia;
- bad habits (smoking, drinking alcohol or drugs);
- severe stressful shocks;
- intestinal dysbiosis, dysfunction of the digestive system;
- helminthic infestations;
- failure to comply with personal hygiene rules;
- constant use of panty liners;
- improper use of sanitary pads (delayed replacement);
- sudden climate change;
- incorrectly selected contraceptives;
- frequent use of antibacterial soap;
- decreased immunity.
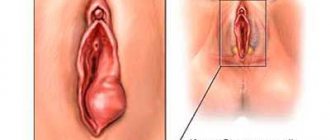
Vaginal dysbiosis in a girl before the onset of sexual activity can be caused by hormonal fluctuations and the development of menstrual function. Also, vaginal dysbiosis is a consequence of the anatomical features of the structure of the hymen.
Why does dysbiosis occur?
Typical reasons may be:
- Hypothermia (one-time severe or regular).
- Hormonal changes
Puberty, pregnancy, abortion, irregular sex life, menopause, cycle disorders.
- Frequent change of sexual partners (subject to unprotected sexual intercourse)
- Pelvic organ infections
- Sexual infections (trichomoniasis, gonorrhea, chlamydia)
- Taking antibiotics, antifungal drugs, cytostatics
Symptoms of vaginal dysbiosis
At the initial stage, the pathological process is asymptomatic. Sometimes the nature of the discharge changes slightly, but women do not attach any importance to this.
The most common signs of vaginal dysbiosis, which progresses, are:
- burning and itching in the perineum;
- swelling and redness of the mucous membrane;
- yellowish-white discharge with a fetid, putrid odor.
Often women with vaginal dysbiosis complain of discomfort and pain during intercourse.
In the case of an inflammatory process, the discharge becomes purulent in nature, and pain appears when emptying the bladder. Possible increase in body temperature. Inflammation most often occurs in virgins, since the hymen does not normally remove the resulting discharge.
Signs of vaginal dysbiosis
As mentioned above, dysbiosis manifests itself unnoticed. First of all, there is a slight change in the discharge. Then more characteristic signs appear:
- itching and burning in the vaginal area;
- dryness during PA;
- pain in the vaginal area;
- pain in the lower abdomen;
- purulent yellowish discharge with an unpleasant “fishy” odor.
If dysbiosis is not treated, it can lead to the development of cystitis, colpitis, infections of the reproductive and urinary systems. Eventually, a woman may develop chronic dysbiosis.
Diagnosis of vaginal dysbiosis
When asymptomatic, the disease is often diagnosed accidentally during a routine gynecological examination. Women with characteristic symptoms are prescribed a bacteriological culture of a smear for vaginal microflora.
The presence of two of the following criteria almost always means vaginal dysbiosis:
- Absence of lactoflora in Gram-stained smears, presence of key cells.
- Positive amino test result (smears mixed with a special reagent have a putrid odor).
- Increased pH level as determined by pH testing.
In some cases, to confirm the diagnosis, the following tests are prescribed for vaginal dysbiosis: bacterial culture on a nutrient medium (plant culture), PCR for infections, laser correlation spectroscopy, sensitivity of the pathogen to antibacterial agents, etc.
Differential diagnostics are also carried out with allergies, candidiasis, inflammatory diseases of the reproductive system, sexually transmitted infections, and bacterial vaginosis.
Vaginal microflora disorders: video
Gynecologists of the Medhelp research clinic and vaginal dysbiosis.. Source - HealthCare
Sources:
- BACTERIAL VAGINOSIS: DIAGNOSIS AND TREATMENT AT THE CURRENT STAGE. Ordiyants I.M., Chetvertakova E.S., Chymba A.A., Klychmamedova G.B. // Zemstvo doctor. – 2011. – No. 2. – P. 28-30.
- MODERN VIEW OF BACTERIAL VAGINOSIS. Reshetnikova N.S., Plekhanov A.N. // Bulletin of the Buryat State University. Medicine and pharmacy. – 2014. – No. 12. – P. 75-78.
- Biofilms in bacterial vaginosis. Berezovskaya E.S., Makarov I.O., Gomberg M.A., Borovkova E.I., Chulkova E.A., Arakelyan L.A. // Obstetrics, gynecology and reproduction. - 2013. - 2: pp. 34-36.
- Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Amsel R., Totten PA, Spiegel CA et al. //Am. J. Med. - 1983. - R. 74:14
- Comparative effectiveness of local therapy for bacterial vaginosis in obese pregnant women. Makarov I.O., Borovkova E.I. // Obstetrics, gynecology and reproduction. - 2012. - 3: pp. 14-17.
- https://www.researchgate.net/publication/303538419_Vaginal_Dysbiosis_from_an_Evolutionary_Perspectiv…
- https://www.frontiersin.org/articles/10.3389/fphys.2015.00253/full
- https://www.ncbi.nlm.nih.gov/pubmed/28257809
- https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-017-0999-x
Treatment of vaginal dysbiosis
For therapy to be effective, it is necessary to eliminate the risk factors that provoke the pathological process.
Treatment is carried out in two stages: first, drugs are prescribed that kill pathogenic microorganisms, then - drugs that restore the natural microflora of the vagina.
The treatment regimen for vaginal dysbiosis is based on an integrated approach and includes the following medications:
- Local antiseptics. They inhibit bacterial growth and reduce elevated vaginal pH. For example, Vaginorm-S, Betadine, Hexicon, Yovidox, Fluomizin.
- Eubiotics. They restore the normal microflora of the vagina and act on opportunistic bacteria. For example, Acylact, Ecofemin, Bifidumbacterin, Bifiliz, Lactobacterin.
In most cases, suppositories for vaginal dysbiosis (local treatment) give good results. However, in some cases, concomitant oral medications are required.
As a rule, the doctor individually selects immunomodulators for the patient - drugs for vaginal dysbiosis that increase local immunity. Microflora disturbance is almost always associated with a decrease in local or general immunity, so its correction is an important part of a complete treatment. Otherwise, dysbiosis can quickly return.
To enhance drug therapy, herbal medicine is additionally prescribed: medicinal tampons, baths and douching.
In the absence of sexually transmitted diseases, treatment of the woman’s sexual partner is not required, but barrier contraceptives (condoms) must be used throughout the entire period of therapy. In the presence of such diseases, it is imperative to prescribe oral antibiotics.
Complete therapy for vaginal dysbiosis during pregnancy is impossible due to the potential negative impact on the health of the fetus. Therefore, symptomatic treatment is carried out to eliminate the unpleasant manifestations of the disease, and a full course is prescribed after childbirth.
It is advisable to treat chronic vaginal dysbiosis in women in parallel with intestinal dysbiosis. With frequent relapses of the disease, the gastrointestinal tract usually becomes the repository of pathogenic microorganisms, especially Candida. Then the signs of vaginal dysbiosis are similar to the symptoms of intestinal dysbiosis - white discharge with a cheesy consistency. It is noted that almost all patients with the chronic form of the disease have identical strains of vaginal and gastrointestinal bacteria.
Types and forms of bacterial vaginitis
The inflammatory process during vaginitis can be acute or chronic. In the first case, the patient notes pronounced symptoms - severe itching, burning, pain and profuse discharge. The chronic form can be very insidious, occurring almost asymptomatically.
The types of bacterial vaginitis, depending on the pathogen, deserve special consideration:
- Trichomonas colpitis . The causative agent in this case is the bacterium Trichomona vaginali, which is sexually transmitted. The manifestations of this disease generally coincide with the characteristic signs of bacterial vaginitis of other types. In this case, the distinctive symptom of Trichomonas colpitis in women is the appearance of foamy yellowish-green discharge. Due to the fact that the bacterium Trichomona vaginali is capable of producing carbon dioxide, vaginal discharge may foam and emit an unpleasant putrid odor. The danger of trichomanas colpitis in women is that the bacterium can penetrate deeply into the vaginal epithelium. It is in this regard that the treatment of trichomanas colpitis in women is particularly difficult.
- Candidiasis colpitis . In this case, vaginitis is caused by opportunistic yeast fungi of the genus Candida. This disease especially often develops against the background of long-term use of antibiotics, hormonal medications and oral contraceptives. Candidal vaginitis is characterized by the release of a large amount of white, cheesy discharge, which women often mistake for thrush. Treatment of candidal colpitis is carried out with antifungal drugs.
Only a gynecologist can make an accurate diagnosis and determine the causative agent of bacterial vaginitis, based on bacterioscopic and bacteriological studies. To assess the condition of the mucous membranes of the vaginal walls, colposcopy is additionally performed.
FAQ
What sensations does vaginal dysbiosis cause?
Among the unpleasant manifestations, it is worth noting the itching of the genitals and the putrid smell of the discharge.
What causes vaginal dysbiosis?
Basically, the disease occurs due to poor personal hygiene. Some women use gynecological tampons and pads incorrectly. Also, the reason may lie in a decrease in local or general immunity.
How long does the treatment last?
The full course takes about 3 weeks.
Treatment of bacterial vaginitis
The gynecologist should determine how to treat bacterial vaginitis based on a study of the sensitivity of the pathogen to the action of antibiotics. At the same time, doctors assure that only an integrated approach to therapy is effective. This complex should include the following areas:
- antibiotic therapy - antibacterial drugs can be prescribed either orally or in the form of local pharmacological forms (vaginal tablets, suppositories, tampons);
- physiotherapy – UHF and UV irradiation of the genital organs (vulva) is effective. As well as local darsonvalization;
- general strengthening therapy - consists of strengthening the immune response by fortifying the body, taking hepatoprotectors and immunomodulators;
- lifestyle - proper nutrition, regular moderate physical activity and giving up bad habits significantly reduce the likelihood of developing bacterial vaginitis and speed up its treatment.
You can learn more about the prevention and treatment of vaginitis in women by making an appointment with a highly qualified gynecologist at the NEOMED clinic.
Make an appointment with a gynecologist
Bacterial vaginosis of the vagina in pregnant women
Bacterial vaginosis often worsens during pregnancy. During this period, a significant restructuring of the female body occurs. Hormonal levels change, immunity decreases, lifestyle and nutrition change, which disrupts the protective mechanisms of the reproductive system. Pregnant women may experience copious discharge with an unusual smell and color, itching, burning, pain and discomfort during sexual intercourse.
Many medications are contraindicated during pregnancy, which is why dysbiosis during this period of a woman’s life is very difficult to treat. For example, it is impossible to correct immunity, which is a mandatory part of the treatment of the disease. Most doctors in such cases limit themselves to local symptomatic therapy.
If women are given antibiotics after childbirth or a caesarean section, they can also cause an imbalance in the vaginal flora. Patients experience an increase in the amount of discharge, a feeling of dryness in the vagina, itching, and a burning sensation. It is also difficult to carry out full therapy while breastfeeding. Therefore, topical drugs are prescribed that relieve the main symptoms. First of all, suppositories with antiseptic components are prescribed that sanitize the vagina. If symptoms persist after completion of breastfeeding, a full course of treatment for dysbiosis is carried out.
Why is the composition of the vaginal microflora disrupted?
The causes of vaginal dysbiosis are very different. Most often, the disease occurs under the influence of the following factors:
- Intensive proliferation of fungi from the genus Candida (thrush or candidiasis) in the vagina.
- Hypothermia (one-time or constant), which causes changes in immune reactivity, which affects the state of the vaginal microflora and provokes vaginal dysbiosis.
- Physiological hormonal changes in a woman’s body, endocrine disorders: puberty, pregnancy and childbirth, abortion, premenopause, menopause and postmenopause, disruption of the hormonal function of the ovaries and the menstrual cycle.
- Change of place of residence and climate.
- Stressful situations.
- Casual sex, unprotected sex.
- Inflammatory pathologies of the pelvic organs (cystitis, urethritis, vulvitis, etc.).
- Infections of the reproductive organs (ureaplasmosis, trichomoniasis, chlamydia).
- Long-term antibiotic therapy or frequent use of these drugs for various infectious diseases.
- Intestinal dysbiosis, chronic constipation, diarrhea and other gastrointestinal problems.
- Excessive and incorrect use of tampons during menstruation. After all, the hygiene product must be changed every 2 hours, even at night. If this is not done, the balance of the vaginal microflora is disrupted, creating conditions for the development of pathogenic microorganisms. Therefore, it is better to use pads while sleeping.
- Gardnerellosis. The disease is caused by opportunistic bacteria Gardnerella, it occurs when the immune system is weakened, and provokes vaginal dysbiosis. It remains asymptomatic for a long time. The main symptoms are copious discharge with a specific fishy odor and severe itching.
- Entry of pathogenic microorganisms into the vagina.
Not every woman experiences vaginal dysbiosis under the influence of the factors listed above. A healthy body regulates the composition of microflora. But in certain circumstances (with the simultaneous action of several unfavorable factors, weakened immunity), the protective mechanisms fail and vaginosis develops.