The placenta is an organ located in the uterus and functions only during pregnancy. It is thanks to him that the normal development of pregnancy until birth becomes possible, so it is important that the placenta “works” normally. In this case, not only the correct structure of the placenta matters, but also its correct location. Placenta previa is a serious complication of pregnancy, which, fortunately, does not occur very often.
The placenta is laid at the very beginning of pregnancy and is fully formed by 16 weeks. It provides nutrition to the fetus, removes metabolic products, and also performs the function of the lungs for it, because It is through the placenta that the fetus receives the oxygen necessary for its life. In addition, the placenta is a real “hormonal factory”: hormones are formed here that ensure the preservation and normal development of pregnancy, the growth and development of the fetus.
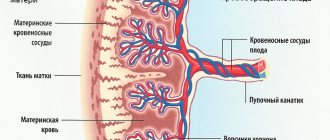
The placenta consists of villi - structures within which blood vessels pass. As pregnancy progresses, the number of villi, and therefore the number of vessels, constantly increases.
General information
What does placenta previa mean during pregnancy? During the normal course of pregnancy, the placenta is located predominantly in areas of better vascularization of the myometrium, that is, in the area of best blood supply to the uterine wall, which includes the body/fundus or posterior/lateral wall of the uterus. In addition, this location of the placenta minimizes the risk of damage to it. Somewhat less often, the placenta is located on the anterior wall of the uterus, since the anterior wall is subject to significantly greater changes. One of the anomalies (pathologies) of pregnancy is placenta previa, which is characterized by attachment of the placenta along any wall of the uterus to its lower segment (inferior recumbency), that is, the placenta is located in front of the presenting part of the fetus and completely/partially covers the internal uterine os (Fig. below ).
The placenta is an essential component of the mother-placenta-fetus system, which is formed from the beginning of pregnancy and functions until the birth of the child.
Embryoblast / trophoblast and decidual tissue participate in its formation , and its function is to provide the necessary conditions for the normal development of the fetus/physiological course of pregnancy (respiratory, nutritional, protective, excretory, endocrine functions).
The formation of the placenta is completed completely at 20 weeks of pregnancy and at the same period, placenta previa is determined by ultrasound. Normally, the placenta should not reach 7 cm or more with its lower edge to the internal os. Low adherence of the placenta is characterized by its location between the os of the uterus and the lower edge at a distance of less than 6 cm, and at the same time, the placenta does not overlap the internal os. As a rule, placenta previa in the early stages of pregnancy is detected at the first ultrasound examination (usually at 11-13 weeks) and is defined as an abnormal location of the chorion - subsequently the placenta (marginal chorion previa). Often, central chorion presentation, determined in the 1st trimester of pregnancy towards its end, turns into a low location of the placenta. It should be noted that marginal presentation of the chorion at the 12th week does not mean that the pregnant woman will necessarily have marginal presentation of the placenta by the time of delivery. This is due to the so-called “migration phenomenon” of the placenta, which manifests itself in its displacement upward from the internal os of the cervix as the duration of pregnancy increases.
According to literature data, in almost 10% of cases at 12-13 weeks of pregnancy, chorion previa is detected, but only in 0.5% of cases complete placenta previa remains at the time of delivery. According to research data, migration of the placenta when it is low occurs in almost 95% of cases. In this case, there is a displacement of the underlying myometrium, and not movement of the placenta itself. The process of placenta migration proceeds slowly and ends approximately at 32-35 weeks. This is evidenced by numerous reviews from many women visiting a specialized forum for pregnant women. Migration occurs more often when it is located along the anterior wall, and less often when located along the posterior wall.
However, marginal presentation of the chorion is the basis for classifying such women as a “potential risk” group with careful dynamic monitoring of them, since such localization of the chorion increases the risk of uterine bleeding with the threat of interruption of the gestation (spontaneous termination of pregnancy in the early stages). And if placenta previa persists until 26-28 weeks of gestation (under ultrasound control), mandatory hospitalization with constant medical supervision until the moment of birth is indicated.
According to statistics, the frequency of placenta previa varies between 0.3%-1.04%, and the frequency of low placentation reaches 9.1%. At the same time, with placenta previa, maternal mortality rates range from 2.1% to 10.5%, and perinatal mortality reaches 22.5–41.8%. Placenta previa is more common in women who are pregnant again than in women who are pregnant for the first time.
What are the risks of low placenta previa during pregnancy?
Low placenta adherence during pregnancy is accompanied by an increased risk of its damage/detachment under pressure from the fetus or during its active behavior in late pregnancy, as well as under any external influence. What are the dangers of placenta previa for the fetus and the pregnant woman?
Placenta previa is accompanied by a high risk of developing chronic placental insufficiency in the 2-3 trimesters of pregnancy, which has a negative impact on the development/growth of the fetus, contributing to the development of hypoxia , abnormal position/prematurity of the fetus, and premature birth. The main complication of placenta previa is bleeding from the genital tract. At the same time, the likelihood of developing uterine bleeding increases as pregnancy progresses, which is the leading cause of perinatal morbidity/reproductive losses.
What are the dangers of marginal placenta previa and what are the dangers of complete placenta previa?
As is known, the type of placenta previa also affects the nature of bleeding. For incomplete placenta previa, bleeding in the 3rd trimester of pregnancy/birth up to hemorrhagic shock , and for complete placenta previa, early bleeding is more typical (in the 2nd trimester of pregnancy). The frequency of bleeding also varies depending on the type of presentation. According to the literature, with incomplete placenta previa, bleeding is observed in 66.6% of cases, and with complete presentation in 33.4%.
If there is no bleeding/abruption of the placenta previa, with partial presentation, birth through the birth canal is possible, and with complete presentation, a cesarean section .
Observation and treatment of placenta previa
An expectant mother diagnosed with placenta previa needs careful medical supervision. The timely conduct of clinical trials is of particular importance. If even a slightly reduced level of hemoglobin or disorders in the blood coagulation system are detected, the woman is prescribed iron supplements, because in this case, there is always a risk of rapid development of anemia and bleeding. If any, even minor, deviations in health are detected, consultation with relevant specialists is necessary.
Placenta previa is a serious pathology, one of the main causes of serious obstetric hemorrhage. Therefore, if bleeding develops, all the health problems a woman has, even minor ones, can aggravate her condition and lead to adverse consequences.
Regimen plus diet If there is no bleeding, especially with partial placenta previa, the woman can be observed on an outpatient basis. In this case, it is recommended to follow a gentle regimen: physical and emotional stress should be avoided, and sexual contact should be excluded. You need to sleep at least 8 hours a day and spend more time in the fresh air. The diet must contain foods rich in iron: buckwheat, beef, apples, etc. There must be sufficient protein content, because without it, even with a large intake of iron into the body, hemoglobin will remain low: in the absence of protein, iron is poorly absorbed. It is useful to regularly eat fiber-rich vegetables and fruits, because... Retention of stool can provoke the appearance of bloody discharge. Laxatives are contraindicated for placenta previa. Like all pregnant women, patients with placenta previa are prescribed special multivitamin preparations. If all these conditions are met, the manifestations of all the symptoms described above, which accompany placenta previa in most cases, are reduced, which means that conditions are provided for the normal growth and development of the child. In addition, in the event of bleeding, the adaptive capabilities of the woman’s body increase, and blood loss is more easily tolerated.
In the presence of bloody discharge, observation and treatment of pregnant women with placenta previa during pregnancy over 24 weeks is carried out only in obstetric hospitals that have the conditions for providing emergency care in an intensive care unit. Even if the bleeding has stopped, the pregnant woman remains under the supervision of hospital doctors until the due date.
In this case, treatment is carried out depending on the strength and duration of bleeding, the duration of pregnancy, and the general condition of the woman and fetus. If the bleeding is minor, the pregnancy is premature and the woman feels well, conservative treatment is carried out. Strict bed rest and medications to reduce uterine tone and improve blood circulation are prescribed. If anemia is present, a woman takes medications that increase hemoglobin levels and general health-improving medications. Sedatives are used to reduce emotional stress.
Pathogenesis
The fertilized egg is normally attached to the fundus of the uterus (the upper third of the uterine cavity). But if it is inferior, the fertilized egg cannot attach in this area in a timely manner, which facilitates its implantation into the endometrium when it has already moved to the lower parts of the uterus. This occurs with the late appearance of enzymatic processes in the trophoblast, the presence of atrophic/dystrophic processes in the uterine mucosa, which disrupt the implantation process.
As pregnancy progresses, the walls of the lower uterus begin to stretch. At the same time, the muscle fibers of the lower parts of the uterus begin to contract, and since the placenta is unable to contract/stretch following the walls of the uterus, this leads to a displacement of the placenta and the lower segment of the uterus.
Accordingly, the villi covering the placenta are torn off from the walls of the uterus, which causes bleeding from the vascular bed of the placental tissue. When muscle contraction stops, placental abruption also stops, vascular thrombosis and bleeding stops. With repeated contractions of the uterus, repeated bleeding occurs.
When labor (labor) begins, the appearance of bleeding is caused by the tension of the membranes holding the edge of the placenta, which does not allow it to contract with the lower parts of the uterus. This tension disrupts the connection between the placenta and the uterus, causing bleeding. When the membranes rupture, the placenta contracts along with the muscles of the lower segment of the uterus and the detachment process stops. In addition, in case of incomplete presentation, the fetal head during childbirth, descending into the pelvis after rupture of the membranes, presses the edges of the placenta, which helps stop bleeding, and in cases of complete presentation, bleeding continues, since the placenta continues to exfoliate in the process of smoothing the cervix.
Why is it worth saving cord blood in Cryobank?
Today, more than 100 diseases can be cured using stem cells. The procedure for collecting umbilical cord blood is possible only at the birth of a child - at the moment of cutting the umbilical cord.
It is absolutely safe and painless for both the child and the mother in labor. When the days are counting, and there is no way to urgently find a suitable donor, then the only way out is treatment with stem cells. While searching for a donor takes months, preparing stem cells takes several hours.
A feeling of maximum peace of mind for the most valuable thing in life - for your children - is only possible if you are 100% sure that the right medicine is at hand. It is stored in the Cryobank of the Institute of Cell Therapy and is available to you and your family upon request.
placenta
Classification
The classification sign of placenta adherence is its location relative to the area of the internal os, and therefore it is customary to distinguish:
- Complete placenta previa - in this case, the placenta completely covers the internal os of the cervix. In the structure of cases of improper location of the placenta, complete presentation occurs in 20-44% of cases.
- Partial placenta previa - in this case, the placenta does not completely cover the internal os of the cervix (incomplete presentation). In turn, partial presentation is divided into lateral presentation (the placenta covers the internal os by 2/3 of its area) and marginal placenta (its edge approaches the internal os at a distance of less than 3 cm). Partial presentation occurs in 31% of cases.
The division into anterior placenta previa, posterior and central placenta previa is not used in the classification. In this case, the anterior, central or posterior location of the placenta itself may be distinguished, but it is not associated with presentation.
Stem cells can be used to treat both the child and his relatives
Today, stem cell treatment methods are successfully used all over the world. In Ukraine, the leading position in the development and application of such techniques belongs to the Institute of Cell Therapy. Cord blood stem cells are stored in the Cryobank of the Institute of Cell Therapy in special containers under guaranteed maintenance of the necessary conditions.
Causes
Placenta previa can be caused by many factors, including:
- Pathological changes in the inner layer of the uterine wall (endometrium), caused by an infectious-inflammatory process, contributing to the development of atrophic/dystrophic changes in the endometrium.
- Anomalies of the uterine cavity /genital organs (underdevelopment of the uterus, bicornuate/unicornuate uterus, sexual infantilism).
- Uterine fibroids with deformation of its cavity.
- Pregnancy after surgical interventions ( abortion , cesarean section , removal of uterine fibroids ).
- Repeated pregnancy after complications in the postpartum period.
- Extragenital diseases of pregnant women occurring against the background of the development of congestion in the pelvis and uterus, including.
- Use of assisted reproductive technologies (IVF).
- The pregnant woman’s age is over 30 years.
Gynecological manipulations, excessive physical activity/strain during defecation, sexual intercourse, and thermal procedures (hot bath, visiting a sauna) can cause bleeding during placenta adherence.
Symptoms
The main clinical symptom of placenta previa is uterine bleeding at different stages of pregnancy (from the 1st trimester to childbirth), of varying severity. Bleeding with placenta previa is often provoked by coughing, straining during bowel movements, physical activity, vaginal examination, sexual intercourse, and thermal procedures. On the eve of childbirth, bleeding usually intensifies, due to periodic contractions of the uterus.
Symptoms of placenta previa (nature/intensity of bleeding) are determined by the type of placenta previa. Moreover, the greater the degree of placenta previa, the more intense and earlier the bleeding occurs. Thus, complete presentation is characterized by profuse blood loss, sudden development of bleeding against the background of the absence of pain. With incomplete presentation, bleeding develops mainly closer to the due date and is observed especially often during the period of smoothing/opening of the pharynx (at the beginning of labor).
Bleeding is characterized by a number of features:
- Sudden onset, often for no apparent reason (during night sleep, rest).
- External and repetitive in nature.
- No pain.
- Bright red color of the flowing blood.
Often recurrent blood loss contributes to the rapid development of anemia in the pregnant woman . At the same time, a decrease in the number of red blood cells and bcc can cause the development of disseminated intravascular coagulation syndrome and hypovolemic shock .
Pregnancy with placenta previa often occurs with arterial hypotension , gestosis , and the threat of spontaneous abortion . Preterm birth is more common with complete placenta previa. The most important symptom of placenta previa is also fetal hypoxia , which is due to the non-participation of the detached part of the placenta in the uteroplacental circulation, and the degree of hypoxia is determined by the area of placental abruption.
Tests and diagnostics
When making a diagnosis of placenta percreta, the following are taken into account:
- Data from obstetric and gynecological history and the presence of risk factors (previous operations (caesarean section)/abortions, inflammatory processes in the appendages/uterus, the presence of ovarian dysfunction, abnormalities of the uterus.
- Complaints of recurrent painless bleeding from the genital tract.
- Data from external obstetric examination.
- Results of vaginal examination of a pregnant woman. A diagnostic sign is the presence of placental tissue in the area of the internal os.
- Data from instrumental research methods - transabdominal/transvaginal ultrasound. Allows you to establish the fact of placenta previa and obtain objective data about the variant of placenta previa, assess the area, structure, size and degree of maturity of the placenta, the degree of abruption, the presence of retroplacental hematomas, identify “placental migration” and its dynamics.
The diagnosis is made starting from 20 weeks, since low lying placenta/placenta previa may disappear in early pregnancy.
Diagnosis of placenta previa
Diagnosis of this pathology is most often not difficult. It is usually installed in the second trimester of pregnancy based on complaints of periodic bleeding without pain.
During an examination or ultrasound, a doctor may reveal an abnormal position of the fetus in the uterus. In addition, due to the low location of the placenta, the underlying part of the child cannot descend into the lower part of the uterus, therefore a characteristic feature is also the high standing of the presenting part of the child above the entrance to the pelvis. Of course, modern doctors are in a much better position compared to their colleagues 20-30 years ago. At that time, obstetricians-gynecologists had to navigate only by these signs. After the introduction of ultrasound diagnostics into widespread practice, the task became significantly simplified. This method is objective and safe; Ultrasound allows you to get a high degree of accuracy about the location and movement of the placenta. For these purposes, three-time ultrasound monitoring at 16, 24-26 and 34-36 weeks is advisable. If an ultrasound examination does not reveal a pathology in the location of the placenta, the doctor may, upon examination, identify other causes of bleeding. They can be various pathological processes in the vagina and cervix.
Advertising
Consequences and complications
Low placenta previa can cause a number of negative consequences and complications such as:
- Recurrent bleeding from the genitals.
- Spontaneous termination of pregnancy .
- Premature birth.
- Placental insufficiency (with fetal hypoxia ).
- Anemia.
- Hypotension.
- Incorrect (transverse, pelvic) position of the fetus.
- Anomalies of labor.
Forecast
Prognosis for placenta previa is determined by timely diagnosis, type of placenta previa, adequacy of therapy and a number of other reasons that influence the outcome of childbirth (blood loss, condition of the pregnant woman and fetus, indicators of the hematopoietic organs/cardiovascular system). The prognosis for marginal placenta previa in the absence of bleeding is more favorable and in most cases it is possible to carry the fetus to 38 weeks and give birth naturally to a healthy child. The prognosis for complete presentation with large blood loss is less favorable, and infant/maternal mortality varies between 3-5%. A more favorable outcome for the fetus/mother is cesarean section .
Precautionary measures
It should also be noted that with placenta previa, you should always keep in mind the possibility of severe bleeding. Therefore, it is necessary to discuss with your doctor in advance what to do in this case, which hospital to go to. Staying home, even if the bleeding is light, is dangerous. If there is no prior agreement, you need to go to the nearest maternity hospital. In addition, with placenta previa, it is often necessary to resort to a blood transfusion, so if you have been diagnosed with this, find out in advance which relative has the same blood type as you, and get his consent to donate blood for you if necessary (the relative must get tested for HIV, syphilis, hepatitis in advance).
You can arrange at the hospital where you will be observed so that your relatives donate blood for you in advance. At the same time, it is necessary to obtain a guarantee that the blood will be used specifically for you - and only if you do not need it will it be transferred to a general blood bank. It would be ideal for you to donate blood for yourself, but this is only possible if your condition is not alarming, all indicators are normal and there is no bleeding. It is possible to donate blood for storage several times during your pregnancy, but you also need to ensure that your blood is not used without your knowledge.
Although placenta previa is a serious diagnosis, modern medicine allows you to carry and give birth to a healthy child, but only if this complication is diagnosed in a timely manner and with strict adherence to all doctor’s prescriptions.
When everything is over and you and your baby find yourself at home, try to properly organize your life. Try to get more rest, eat right, and be sure to take your baby for walks. Don't forget about multivitamins and medications to treat anemia. If possible, do not give up breastfeeding. This will not only lay the foundation for the baby’s health, but will also speed up the recovery of your body, because... Stimulation of the nipple through sucking causes the uterus to contract, reducing the risk of postpartum bleeding and inflammation of the uterus. It is advisable that at first you have someone to help you with child care and household chores, because your body has gone through a difficult pregnancy and needs to recover.
List of sources
- Kolchina V.V. Factors influencing the unfavorable course of pregnancy in patients with low pregnancy rates / V.V. Kolchin // Modern problems of science and education. - 2014. - No. 3.
- Kolchina V.V. Development of a standard for the management of pregnant women with low placentation in the early stages of gestation / V.V. Kolchin // Proceedings of the conference “Innovative developments of young scientists of the Voronezh region for the service of the region.” - 2013. - pp. 66-68.
- Obstetrics. National leadership / Ed. Ailamazyan E.K., Kulakov V.I., Radzinsky V.E., Savelyeva G.M. - M.: GEOTAR-Media, 2014. - 1200 p.
- Davydov A.I., Agrba I.B., Voloshchuk I.N. Pathogenesis of placental attachment pathology: the role of growth factors and other immunohistochemical markers // Issues of gynecology, obstetrics and perinatology. - 2012. - T. 11, No. 1. - P. 48-54.
- Baev O.R. Anomalies of placenta attachment // Issues of gynecology, obstetrics and gynecology. - 2009.- No. 5.- P.3-6.