Prolapse of the uterus and vaginal walls is a weakening of the muscles and structures of the pelvic floor, leading to a change in the normal physiological relationship of the pelvic organs - the uterus, bladder, rectum.
According to statistics, every third woman aged 45 years and older suffers from this disease, and every tenth woman by the age of 80 has been operated on for prolapse.
One of the main causes of uterine prolapse
associated with childbirth: over time, the muscles surrounding and supporting the uterus weaken after childbirth. They are no longer able to keep the uterus with appendages and intestines in their natural state.
Causes and factors contributing to prolapse of the uterus and vagina
Reduced amount of collagen in connective tissue
A slowdown in the rate of production of collagen fibers in the body entails a gradual stretching of the ligaments, and, as a result, leads to prolapse of the pelvic organs.
Decreased muscle tone
The disease occurs when the tone of the muscular structures of the pelvic floor decreases. The process may be due to both physiological changes in the pregnant woman’s body and overload on the pelvic muscles during childbirth, as well as neglect of the doctor’s recommendations regarding the nutrition and physical activity of the young mother. The correct (healthy) location of the uterus is between the rectum and the bladder. If tone is lost, the muscles can no longer prevent the uterus from moving towards the vagina.
Mechanical damage and birth injuries
The position of the uterus is also affected by injuries to the perineum received by a woman during childbirth or for some other reason. In the case of a difficult birth and long-term stress, the abdominal muscles may also suffer.
Age-related changes
As a woman ages, the production of estrogen decreases, which leads to a gradual loss of muscle tone. During menopause, symptoms of uterine prolapse bother women much more often.
Excess weight and gastrointestinal problems
In some cases, uterine prolapse can be provoked by: excess body weight, which creates a constant additional load on all internal organs, as well as chronic pathologies of the digestive system (constipation, etc.).
What is pelvic organ prolapse and how common is it?
The pelvic floor forms a collection of various muscles and ligaments that hold nearby organs in the correct position (Fig. No. 1). The pelvic floor is often compared to the surface of a trampoline, which under the influence of gravity, increased abdominal pressure and other factors can lose its elasticity and weaken. If these muscles and ligaments become too “loose”, then organs descend along the path of least resistance - into the vagina.
It is not known exactly how common this disease is. In some studies in women after hysterectomy, vaginal prolapse is described in 40% of cases. It is estimated that approximately one in ten women will undergo surgery for pelvic organ prolapse during their lifetime.
Symptoms of uterine prolapse
At an early stage, the disease practically does not manifest itself at all, so it is most often recognized during an examination by a gynecologist or using an ultrasound.
In some cases, the process of descent is uneven: for example, only the back or front wall can change location. Therefore, the choice of treatment must be made taking into account all the features of the course of the disease.
In later stages, uterine prolapse is often accompanied by symptoms:
- aching pain in the lower abdomen, aggravated by walking and radiating into the vagina;
- painful or uncomfortable sexual intercourse, sometimes spotting;
- the appearance of odorless mucous leucorrhoea;
- urinary incontinence, pain when filling the bladder and during urination.
With significant prolapse of the uterus, the pain becomes more intense, sharp pain occurs even when trying to sit down.
Diagnostics
If the problem is detected in a timely manner, there is a high chance of preventing the appearance of painful symptoms and surgical intervention.
The set of diagnostic procedures includes:
- examination on a gynecological chair,
- instrumental diagnostics,
- lab tests.
If necessary, the doctor may additionally prescribe: urography, ultrasound of the pelvic organs, colposcopy, tomography, urinalysis. In some cases, the opinions of specialized specialists are required: a proctologist and a urologist.
In what cases of prolapse is colporrhaphy necessary?
At the second stage of prolapse, displacement of the walls of the vagina, bladder, rectum, and sometimes the uterus along with the cervix is quite clearly expressed. In this case, only surgery will help. Depending on which of the vaginal walls is prolapsed, anterior, posterior or combined colporrhaphy is performed.
This method of vaginoplasty allows you to completely restore the vaginal walls and return the displaced pelvic organs to their place. At this stage, the operation can be performed using tissue from the woman’s genital area. But if the disease starts, you will have to do a more complex intervention with the installation of implants - materials that support the pelvic sections.
Treatment of prolapse of the vaginal walls without surgery
- Laser correction of the vaginal mucosa MonaLisa Touch™
Today, laser therapy MonaLisa Touch™ is one of the most modern technologies for vaginal rejuvenation in terms of its safety and effectiveness. The exclusive technology of vaginal rejuvenation was developed by the world's leading manufacturer of laser medical equipment DEKA and has no analogues to date.
The procedure is minimally invasive and no anesthesia is required. One session takes about 15-30 minutes. Under the influence of a CO2 laser, partial evaporation (ablation) of tissues and their thermal heating occur on the mucous membrane of the vagina and vulva. At the same time, regeneration and renewal mechanisms are launched, blood supply improves, the production of growth factors is activated, new vessels are formed (neoangiogenesis), fibroblasts are stimulated and activated to produce new collagen fibers.
Treatment results:
- the pH level and microflora of the vagina are normalized (dryness, itching, burning and discomfort disappear);
turgor and elasticity of the mucous membranes of the genital tract are restored (the volume of the vagina decreases, the lifting of its walls increases);
- Discomfort during sexual intercourse and urinary incontinence disappear;
- the shape and aesthetic appearance of the genital organs are restored;
- libido and quality of sexual life increase.
Prices
- Laser therapy
- Rejuvenation program “Mona Lisa” Touch + autoplasma therapy* (vagina, vulva, perineum)
- 1 category
60 000 ₽
- 2nd category
75 000 ₽
- Treatment of vaginal wall atrophy
- 1 category
25 000 ₽
- 2nd category
35 000 ₽
- Laser lifting
- Laser correction of the anterior (or posterior) vaginal wall
12 000 ₽
- Laser correction of the anterior and posterior walls of the vagina
20 000 ₽
- Vagina lifting
45 000 ₽
- Treatment of vagina and vulva (without skin)
50 000 ₽
- Autoplasmotherapy* as an addition to the procedure
5 000 ₽
* Before the autoplasmotherapy procedure, it is necessary to undergo tests:
- — Clinical blood test with leukocyte formula and ESR
- — Blood test for glucose
- —R.W.
- — HIV
- — Hepatitis B and C
- Kegel exercises for pelvic organ prolapse
Gymnastics helps tone muscles that are not used by women in everyday life. You can perform it anywhere, it is invisible to others. Main goal: prevention of urinary incontinence and uterine prolapse.Before class, you need to empty your bladder. Next, you should lie on your back, bend your knees.
Kegel exercises for uterine prolapse:
- contract the perineal muscles, pull them up, hold the position for 10 seconds;
- The exercises should be repeated daily (morning, afternoon and evening) for 10 approaches, i.e. 30 approaches during the day.
completely relax the muscles for 10 seconds;
If it is difficult to keep your muscles tense for 10 seconds, you can start with 3 and gradually increase it. All movements are performed smoothly, with even and deep breathing. The first results will be noticeable within 2 months. The pelvic floor muscles will become stronger and begin to hold the uterus in the correct position.
Methods of performing different types of vaginoplasty
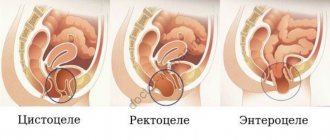
- Anterior colporrhaphy
. In advanced stages, it uses mesh implants to replace stretched, damaged vaginal walls. Excess overstretched tissue is removed and the fascia that supports the pelvic structure is restored. In case of significant defects, this area is sealed using a mesh. The mesh implant is placed under the bladder and secured using special “sleeves”. The method restores the upper vaginal wall and eliminates cystocele – bladder prolapse. - Posterior colporrhaphy
. The rectovaginal fascia, which is responsible for holding the rectum in the correct position, is restored, and the posterior wall of the vagina is “repaired.” Implants are rarely used, as there have been documented cases of complications caused by their installation. A mesh is placed only in situations where the prolapse is so severe that the doctor has no other choice.
Very often, prolapse of the vaginal walls is combined with prolapse of the cervix and uterine body. The process is sometimes so pronounced that the organ completely or partially falls out of the genital slit. In this case, special implants are used to strengthen the prolapsed organ. The installed mesh imitates healthy ligaments and prevents the uterus from moving. Over time, it grows into tissue and continues to perform a supporting function.
The use of a mesh implant for prolapse
Doctors do not recommend removing the prolapsed uterus, except in extreme cases. The fact is that in the pelvic area all organs take their place and are held in place by special structures - ligaments and fascia. When the uterus is removed, the position of the organs changes, which provokes their prolapse, urinary incontinence, and urinary retention.
In addition, removal of the uterus without a comprehensive supporting operation leads to prolapse of its stump. Therefore, doctors try to preserve the organ, avoiding possible complications.
Which treatment method is preferred is decided by the gynecologist surgeon, depending on the patient’s condition and the specific type of organ prolapse.
After surgery, a woman needs to limit physical activity, not play sports, not overheat, and not lift heavy objects. It is necessary to combat constipation, since straining increases intra-abdominal pressure and causes displacement of organs. You can be sexually active only after your doctor’s permission, usually no earlier than 2 months.
Is it possible to slow down the formation of prolapse?
To reduce minor prolapse or reduce the risk of one, you can train the muscles that keep your organs in the right place by doing Kegel exercises.
They are based on repeated tension and relaxation of muscles. To understand which muscles need to be tensed, imagine that you are sitting on a ball and trying to lift it by tensing your muscles. This can be done in any position - sitting, standing or lying down. The goal of the workout is to hold the muscles under tension for approximately 10 seconds and repeat this exercise 8-10 times in one approach. You need to train 3 times a day at least 4 times a week. Follow this regimen for at least 16 weeks. To maintain the effect, this task must be performed over a long period of time, like any muscle training. Over time, you can try to tense your muscles more and hold them in this state for longer. If you are unsure if you are doing these exercises correctly, you may want to see a physical therapist.
Diagnostics
Diagnosis of vaginal wall prolapse consists of performing a standard gynecological examination, which determines the part of the vagina involved in the pathological process and the degree of prolapse. In total, there are 4 degrees of vaginal wall prolapse:
- 1st degree – Characterizes a condition when the walls of the vagina have shifted from their natural position, but do not yet reach the entrance to the vagina by 2 cm or more
- 2nd degree - At this stage of prolapse, the vaginal walls are at the level of the entrance to the vagina.
- 3rd degree - In this case, there is prolapse of the vaginal walls beyond the genital slit, but not more than 2/3 of its length
- Stage 4 – Complete prolapse of the vaginal walls
With the first two degrees, the patient may not feel the prolapse and it is often asymptomatic and requires only observation. 3-4 degree prolapse is an advanced stage of the disease, which requires treatment.
Questions and answers
Question: What is the difference between program 2 and program 7? M.Sh., Nalchik. Answer: Programs 2 and 7 differ in goals: the goals of program No. 2 (treatment of urinary incontinence, treatment of uterine and vaginal prolapse) are to “straighten” the bend, reposition and FIX the UTERUS in the correct position, eliminate urinary incontinence during sexual intercourse, physical activity, stress and etc., i.e. mainly medicinal. The goals of program No. 7 (recovery after childbirth and narrowing of the vagina) are to improve the quality of life and develop the uniqueness of the feminine. Depending on the condition of the muscles and the level of training, various techniques are used.
Question: I have developed URINary INCONTINENCE WHEN COUGHING and RAISING BAGS. A friend who was treated by you said that it was prolapse of the uterus. I’m embarrassed to go out in public, I can’t go to the market, I started to feel ashamed of myself. An inferiority complex will soon form. But I'm only 54 years old. I HAVE HEARD A LOT OF GOOD THINGS ABOUT YOUR CLINIC. How can I get treatment? With uv., F.D., Makhachkala. Answer: Judging by the complaints, uterine prolapse is very likely. You should not lift more than 3 kg. Reception for examination and treatment by appointment by phone 8 (calls within Russia are free) or.
Question: I treated vaginal and uterine prolapse in your clinic a couple of years ago. I've been working a lot lately and I'm starting to notice that it feels like I'm feeling it again. Is a relapse possible, what should I do? L.A., St. Petersburg. Answer: If you continue heavy physical activity with straining, lack of regular training of the muscles of the vagina and perineum, and failure to comply with preventive measures, RECURRENCE OF VAGINAL AND UTERUS PROPRESSION, uterine and vaginal prolapse, and urinary incontinence is possible.
Question: I was diagnosed with Uterine Prolapse. But I myself DO NOT FEEL ANYTHING, I do not experience any health problems. Could this be possible? A.M., Baksan. Answer: Very often, hardworking and patient women do not pay attention and do not consider the “minor symptoms” of uterine prolapse to be a problem: rapid fatigue of the “lower back”, periodic pain in the lower abdomen and groin areas in the evening and at the end of physical activity, rapid filling and the feeling of incomplete emptying of the bladder , drip urinary incontinence when coughing, laughing, fast walking, straining, discomfort and pain during intimacy, etc. THE HABIT OF “ENDURING”, everyday life and bustle do not allow you to stop and look at yourself in a new way...
Question: Today is the 22nd day after giving birth. THE CERVIX IS VISIBLE IN THE VAGINA. Please tell me, is this the norm? Will she rise? Answer: Prolapse of the cervix extremely RARELY stops (disappears) on its own. It is DESIRABLE after the end of lochia (bloody discharge from the genital tract after childbirth) to REPOSITION THE UTERUS (return the uterus to the correct anatomical position). At the Resort WOMEN'S HEALTH CLINIC, this treatment is carried out within 7 DAYS.
Question: Before pregnancy, the uterus was bent backwards; after a complicated birth and curettage, a forward bend formed on the seventh day after birth. Now, when the pelvis is raised and, sometimes, DURING SEXUAL INTERACT, AIR gets in and comes out with a “fart.” Is this related to the curvature of the uterus and what can be done about it (it is impossible to play sports because of this “farting”)? Answer: The release of air from the vagina is associated with weakness (insufficiency) of the perineal muscles and an increase in the capacity (volume) of the vagina. WITH THE PURPOSE OF SOLVING this problem, the Clinic has developed Program No. 7 Recovery after childbirth and narrowing of the vagina. WE ARE READY TO RECEIVE YOU.
Question: Do you accept treatment on HOLIDAYS? Answer: The resort clinic for women's health is open seven days a week and on holidays and accepts treatment, tel. (calls within Russia are free).
| ONLINE information about the treatment of vaginal prolapse can be found here. REGISTER ONLINE for treatment here. |
Sign up
Question: WHAT DOCUMENTS ARE REQUIRED for vaginal reduction and treatment in your clinic? Answer: It is advisable to have copies of the results of a previously conducted clinical and laboratory examination (copies of ultrasound, laboratory and other studies), copies of epicrisis (conclusions) of surgical and conservative treatment. In other words, the most complete amount of medical information about your health status. If necessary or desired, it is possible to perform a clinical and laboratory examination in our Clinic.
Question: Is it possible to issue a sick leave certificate at the Clinic for the period of treatment? Answer: At the Women's Health Resort Clinic, sick leave (sick leave) is not issued.
Question: How to get to the Clinic UNDER THE POLICY? What is needed for this: a referral from a gynecologist, or is just desire and an insurance policy enough? Answer: You should contact your insurance company to obtain a cover letter. By providing a cover letter, you will be able to undergo examination and treatment of vaginal prolapse in our Clinic. At the appointment you must have your passport and insurance policy with you. Sincerely, Chief Accountant of the Women's Health Resort Clinic.
Question: Do you provide documents to obtain a tax deduction for treatment? Answer: The Women's Health Resort Clinic provides documents to obtain a tax deduction for treatment (13% tax refund).
We work WITHOUT WEEKENDS and holidays:
Monday - Friday from 8.00 to 20.00, Saturday, Sunday, holidays from 8.00 to 17.00.
Treatment of vaginal prolapse in Pyatigorsk by appointment by multi-channel telephone (calls within Russia are free) or +7 (928) 022-05-32.
The cost of treatment for prolapse of the anterior vaginal wall is 17,150 rubles.
The cost of vaginal reduction with vaginal threads is 55,000 rubles.
| ONLINE information about the treatment of prolapse of the anterior vaginal wall can be found here. REGISTER ONLINE for treatment of prolapse of the anterior vaginal wall here. REGISTER online for treatment of prolapse of the anterior vaginal wall according to |
Sign up
Subsections
- Program No. 1. Treatment of inflammatory and infectious processes of the pelvis
- Program No. 2. Treatment of urinary incontinence, treatment of uterine and vaginal prolapse
- Program No. 3. Treatment of female infertility
- Program No. 4. Cervical treatment
- Program No. 5. Treatment of uterine fibroids
- Program No. 6. Treatment of cervicitis and endocervicitis
- Program No. 7. Recovery after childbirth and narrowing of the vagina
- Program No. 8. Treatment of chronic cystitis
- Program No. 9. Treatment of menopause
- Program No. 10. Treatment of mastopathy
- Program No. 11. Treatment of endometriosis
- Program No. 12. Treatment of hydrosalpinx
- Program No. 14. Treatment of polycystic ovary syndrome
- Program No. 15. Preparation for IVF, ICSI, artificial insemination
- Program No. 16. How to remove belly fat
- Program No. 17. Treatment of kraurosis
- Program No. 18. Treatment of vulvar leukoplakia
- Program No. 19. Prevention of mastopathy
- Appointment with a gynecologist to “check for EVERYTHING”
What complaints does pelvic organ prolapse cause?
In the case of pelvic organ prolapse, complaints are the determining factor in choosing the necessary treatment method. This may be a feeling of pressure in the pelvis, sometimes even pain; often the patient feels or can feel a formation protruding from the vagina, on which abrasions can form over a long period. If you experience urinary incontinence when coughing or laughing, a sudden urge to urinate, or after urinating you have to push the protrusion back into the vagina, prolapse may be to blame. When the intestine protrudes, defecation problems may occur. Usually, the stronger the prolapse, the more pronounced the complaints, which may intensify over time. When contacting a doctor, it is important to accurately describe your existing complaints so that the specialist can offer you the most suitable treatment method.
Address risk factors, exercise, get counseling
Pelvic organ prolapse is a common problem that can not only significantly reduce the quality of life, but also cause functional impairment of the organs if the prolapse is not corrected in a timely manner.
To reduce the risk of prolapse, women of any age are advised to promptly address possible risk factors and perform Kegel exercises in advance to strengthen the pelvic floor. Unfortunately, pelvic organ prolapse cannot be predicted. Sometimes, even after a completely normal and non-traumatic birth, complete uterine prolapse can occur. It is important to remember that this is not a normal situation, and in such cases, consultation with the operating gynecologist is necessary. The good news is that there is a solution to this problem for women who want to maintain the ability to bear a child. We believe that laparoscopic sacrocolpopexy is the most effective method, but the complaints and needs of each woman must be assessed individually. If you want to live a full and high-quality life, then perhaps only a pessary or simple corrective surgery of the anterior vaginal wall will be enough.
The work of the Gynecology and Surgery Clinic JV klīnika is based on the knowledge accumulated by Dr. Juris Vitols during his professional career, as well as the excellently organized work of the team, which is an important component of comprehensive patient care. Since the first laparoscopic gynecological operation performed by Dr. Juris Vitols in 1994, he has performed more than 10,000 endoscopic procedures. Already in 1995, Dr. Juris Vitols was the first in Latvia to perform laparoscopic hysterectomy. Also, Dr. Juris Vitols is a pioneer in the laparoscopic treatment of endometriosis. Thanks to the excellent cooperation with the surgeon Dr. Kaspars Snipis, JV klīnika can be proud of the largest experience in laparoscopic treatment of deep endometriosis in Latvia, including in cases where resection of part of the intestine is necessary.
The son of Dr. Juris Vitols, Jurgis Vitols, has been involved in the work of the clinic for 5 years now. He also specialized in gynecological surgery, especially laparoscopy and hysteroscopy. He gained additional knowledge during an internship in France, as well as during regular visits to European congresses and seminars on endoscopic gynecology.
JV klīnika offers the widest range of laparoscopic gynecological operations. We offer surgical treatment of endometriosis, including in cases where it is necessary to cut out large, deep lesions, which can often cause severe pain. We also offer: laparoscopic correction of uterine prolapse, removal of fibroid nodes of various sizes while preserving the uterus, enucleation of ovarian cysts, restoration of patency of the fallopian tubes, separation of adhesions, correction of urinary incontinence, creation of a vagina in women with a congenital absence of it, correction of suture insufficiency after cesarean section (niches), as well as other complex laparoscopic operations. Surgical treatment for postpartum perineal injuries is also available.