Pulmonary embolism (PE) is a serious, potentially life-threatening condition. Pulmonary embolism occurs due to blockage of blood vessels by thrombotic masses in the lungs. Pulmonary embolism (PE) can cause symptoms such as chest pain and/or shortness of breath. Also, in some cases, PE may have no symptoms at all, and it is difficult to detect without specialized examination. Massive pulmonary embolism can cause collapse and death. PE usually occurs due to the formation of a thrombosis in the lower extremity - deep vein thrombosis (DVT).
Pulmonary embolism (PE)
Prompt treatment is important and can save lives. Pregnancy, various medical conditions and medications, immobility, and major surgery all increase the risk of PE. Anticoagulant therapy, including heparin drugs, direct oral anticoagulants, or warfarin, is the usual treatment for PE.
General information
Thrombosis is the formation of a blood clot in a blood vessel that interferes with blood flow.
Its danger lies in the fact that there is a danger of a blood clot or its fragment moving through the bloodstream - an embolism and blockage of another vessel occurs. For example, supplying the brain or heart. Pulmonary embolism often occurs, which leads to severe organ dysfunction or death. What is pulmonary embolism in medicine? Pulmonary embolism is an acute occlusion (blockage) of the pulmonary artery trunk or its branches (main, lobar or segmental). Occlusion occurs more often due to embolization of a thrombus from the right half of the heart or veins of the lower extremities. The incidence of this disease increases with age and the age of such patients is 62 years.
Pulmonary artery thrombosis is an emergency in cardiac resuscitation and is often the cause of patient death. Seriously ill patients with a high risk of pulmonary embolism and death are patients with cardiac arrhythmias, cancer pathology , and thrombosis of the veins of the lower extremities . Diagnosis is often difficult, so the disease is often not recognized. Early diagnosis and initiation of intensive treatment are important in the prognosis of this disease. The code for pulmonary embolism according to ICD-10 is I 26.
What is TELA
Pulmonary embolism (PE) is a life-threatening condition in which blood clots block the lumen of the pulmonary artery, causing acute pulmonary circulatory disorders.
These blood clots usually form in the veins of the lower extremities. PE is not an independent disease; this syndrome is a complication of venous thrombosis (approximately 80% of all observations), as well as rheumatism, myocarditis, coronary heart disease and other pathologies affecting the cardiovascular system.
According to statistics, pulmonary embolism is one of the most common causes of death - on average, 1 out of 10 people die from a blockage of the pulmonary artery. A timely diagnosis reduces the probability of death to 10%, but the complexity of the situation is that it is quite difficult to determine the prerequisites for the development of this condition.
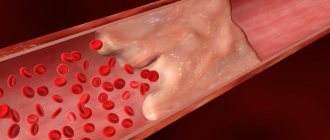
Figure 1. Simplified mechanism of pulmonary embolism. Source: medicalstocks/Depositphotos
The fact is that the most reliable diagnostic methods not only require large financial costs, but also take a lot of time, and pulmonary embolism often develops rapidly. This is one of the main reasons for the high mortality rate during the development of this condition.
Pathogenesis
The main thing in the pathogenesis of pulmonary embolism is occlusion of the pulmonary artery and its branches by embolism, which leads to disruption of hemodynamics and gas exchange. During occlusion, the pressure in the pulmonary artery increases by almost 50% due to vasoconstriction associated with the release of serotonin and thromboxane A2 . A sharp increase in pulmonary resistance causes expansion of the right ventricle, stretching of myocytes and tension of the ventricular walls. Lengthening the time of its contraction towards diastole causes protrusion of the septum into the left ventricle. Therefore, left ventricular filling becomes more difficult, cardiac output decreases, and systemic hypotension .
Massive infiltrates are found in the ventricular myocardium, which further destabilizes hemodynamics. Right ventricular failure due to pressure overload is a leading cause of death. Respiratory failure is also associated with hemodynamic disturbances. A decrease in cardiac output causes desaturation of venous blood. The appearance of zones of reduced blood flow causes a mismatch between perfusion and ventilation. Small emboli in the periphery do not affect hemodynamics, but cause pulmonary hemorrhage with hemoptysis, pleurisy and pleural effusion (“pulmonary infarction”).
Complications
Source: Wirestock/Depositphotos
Acute pulmonary embolism is the most dangerous - it can lead to pulmonary infarction or cardiac arrest, which leads to sudden death. In the case of gradual development, blockage of the lumen of the small and medium branches of the pulmonary artery occurs - this increases the pressure in the pulmonary artery and increases the load on the right atrium and ventricle. In medicine, this condition is called chronic thromboembolic pulmonary hypertension (CTEP).
Characteristic clinical manifestations of CTEPH are weakness, fatigue and severe shortness of breath even with minor physical exertion. CTEPH is especially dangerous for people suffering from diseases of the cardiovascular system, since weakened compensatory mechanisms aggravate the course of the disease.
Classification of pulmonary embolism
The 2008 classification of the European Society of Cardiology identifies:
- Low risk pulmonary embolism.
- Intermediate.
- Tall.
Clinical classification takes into account the caliber of the pulmonary arteries and the percentage of pulmonary involvement:
- Massive (cessation of blood flow in less than 50% of the pulmonary bed). It is of great clinical importance because it is accompanied by shock or decreased pressure, pulmonary hypertension. With occlusion of the trunk, pronounced cardiorespiratory disorders develop. Under such conditions, the right ventricle cannot perform the function of a pump and its cavities quickly expand, and tricuspid valve insufficiency develops. The septum between the ventricles shifts to the left (towards the left ventricle), which is accompanied by poor filling in diastole. Due to the cessation of blood flow, the pulmonary parenchyma is not supplied with blood, but is ventilated. In the affected area, obstruction of the bronchi occurs, the alveoli collapse and surfactant is not formed in them, which contributes to the development of atelectasis (collapse) of the lungs on days 1-2 of embolism. Such hemodynamic disturbances and impaired pulmonary function often lead to the death of the patient.
- PE of small branches of the pulmonary artery (cessation of blood flow is noted in less than 30% of the pulmonary bed). In this case, there is occlusion of lobar and segmental small branches. The disease is not severe without hemodynamic disturbances and patients only need anticoagulant therapy. The pulmonary circulation has compensatory capabilities and there is a possibility of independent dissolution of blood clots when fibrinolysis .
- Submassive—thromboembolism of the branches of the pulmonary artery (cessation of blood flow in less than 30-50% of the bed). It manifests itself as right ventricular failure, and hemorrhagic infarctions form in the lungs.
Classification
Source: Thirdman: Pexels
In modern clinical practice, it is common to use several classifications of pulmonary embolism. For convenience, we present them in table No. 1:
| Criterion | View | Manifestations |
| According to development options | Acute | Sudden onset, chest pain, shortness of breath, drop in blood pressure |
| Subacute | Gradually developing signs of respiratory and heart failure, hemoptysis, signs of pulmonary infarction | |
| Recurrent | Recurrent cases of pulmonary embolism | |
| According to the degree of blockage (occlusion) of the vessel | Small | Occlusion of less than 30% of the total cross-section of the vessel. The patient has shortness of breath, rapid breathing, and dizziness |
| Moderate | Occlusion reaches 50%. A sharp decrease in blood pressure, chest pain, weakness, hemoptysis. | |
| Massive | Occlusion within 70%. The listed symptoms are accompanied by moderate cyanosis (blueness of the skin), swelling and swelling of the neck veins | |
| Supermassive | Occlusion exceeds 70%. Loss of consciousness, severe cyanosis, convulsions, respiratory arrest. | |
| According to the development of complications | "Infarction pneumonia" | Pulmonary infarction: severe shortness of breath, rapid heartbeat, hemoptysis, chest pain. Occurs when embolism of large branches of the pulmonary artery occurs. |
| "Acute cor pulmonale" | Occurs when embolism of small branches of the pulmonary artery. Cardiogenic shock, suddenly developing shortness of breath, and chest pain are noted. | |
| "Unmotivated shortness of breath" | Recurrent embolism of small branches of the pulmonary artery. Shortness of breath develops suddenly and goes away just as suddenly. Decreased blood pressure, chest pain. |
Table 1. Classification of pulmonary embolism
Some experts also use a classification based on the location of the blood clot:
PE of segmental arteries.
PE of the lobar and intermediate arteries.
PE of the main pulmonary arteries and pulmonary trunk.
It should be noted that there is no consensus among experts regarding the validity of the criteria of existing classifications. For example, the classification based on the degree of occlusion used throughout the world has been increasingly criticized in recent years. This is due to the fact that such definitions as “small”, “moderate”, “massive” and “supermassive” seem to modern experts to be “insufficiently informative and misleading.” In 2021, the European Society of Cardiology proposed a unified risk classification:
Low risk pulmonary embolism
Medium-low risk pulmonary embolism
Medium-high risk pulmonary embolism
High risk pulmonary embolism
Causes of pulmonary embolism
Considering the causes of pulmonary embolism, it is necessary to highlight a number of diseases and conditions that are accompanied by the formation of blood clots, which are the basis of embolism:
- Varicose veins and phlebothrombosis of the deep veins of the lower extremities. This pathology causes thromboembolism in 90% of cases. The threat is posed by floating blood clots, which are freely located in the lumen of the vessel and are connected to the vein wall in only one part.
- Congestive heart failure , overstretching of the right ventricle, which creates conditions for the formation of blood clots in the cavity of the right ventricle.
- The use of oral contraceptives and pregnancy , which are associated with an increased risk of blood clots.
- Antiphospholipid syndrome (autoimmune thrombotic vasculopathy ), manifested by venous and arterial thrombosis . Vessels of different sizes may be affected - capillaries and large arterial trunks. Deep vein thrombosis of the lower extremities is a typical manifestation of antiphospholipid syndrome. Repeated pulmonary embolisms are typical.
- Central venous catheterization.
- The presence of malignant diseases.
- Carrying out chemotherapy .
- Spinal cord injury.
- Forced immobilization after surgery, during a stroke , fractures of the pelvis and limbs.
- Hip replacement.
- Atrial fibrillation.
- Polytrauma and extensive surgery.
- Hereditary predisposition to thrombosis ( thrombophilia ), which is caused by mutations of certain genes, deficiency of antithrombin III, deficiency of protein C and S.
Considering pulmonary thrombosis , it is necessary to note the risk factors for this condition:
- Damage to the venous endothelium.
- Obesity.
- Age.
- Hypercoagulation.
- Slowing of venous blood flow.
- Infection.
- Blood transfusions.
- Migraine.
- The combination of several factors is accompanied by a high risk of thrombus embolism .
Symptoms of pulmonary embolism (PE)
Making a diagnosis in the early stages is difficult, only in the acute course the symptoms of pulmonary artery thrombosis appear manifestly and suddenly: shortness of breath , chest pain , tachycardia , decreased blood pressure. In this case, the patient has risk factors for thromboembolism - varicose veins and phlebothrombosis .
Hypotension and shock indicate central thromboembolism . Severe acute shortness of breath also develops with central pulmonary embolism. With the same localization, chest pain is angina-like in nature . Massive thromboembolism is accompanied by signs of right ventricular overload - this is the bulging of the jugular veins in the neck and the right ventricular gallop rhythm.
Signs of PE in subacute cases are not very specific. Respiratory and right ventricular failure progresses, infarction pneumonia and hemoptysis appears. With a recurrent course, repeated attacks of shortness of breath , there are signs of pneumonia and periodic fainting occurs. If the thrombus blocks small arteries in the periphery, shortness of breath is minor and transient. Only in the case of chronic lung pathology or heart failure does shortness of breath worsen. Sometimes PE is asymptomatic.
The clinical picture depends on the caliber of the blocked vessel and, accordingly, the degree of involvement of the pulmonary vascular bed. Massive pulmonary embolism (most often thrombosis of the main branch ) occurs with symptoms of shock or a decrease in pressure by 40 mm Hg. Art. for a short time that is not associated with arrhythmia , sepsis , or decreased blood volume. Characteristic shortness of breath , cyanosis , and sometimes fainting .
Submassive pulmonary embolism (obstruction of lobar or segmental branches) is manifested by right ventricular failure (swelling of the neck veins, pallor, cyanosis), but without arterial hypotension. The patient develops shortness of breath , tachycardia , pulmonary infarction (fever, cough, pulmonary-pleural pain, sputum streaked with blood). In non-massive cases, there are no signs of right ventricular failure, and the pressure is normal.
Symptoms of pulmonary embolism
Pulmonary embolism has no specific clinical manifestations - all of them can occur in pulmonary or cardiovascular pathologies. Typically, the following symptoms occur with pulmonary embolism:
- dyspnea;
- cyanosis;
- fast fatiguability;
- dizziness;
- noise in ears;
- fainting;
- chest pain;
- swelling of the lower extremities;
- hemoptysis;
- cough.
In some cases, atypical manifestations are possible:
- increased body temperature (febrile syndrome);
- vomiting, hiccups and pain in the right hypochondrium (abdominal syndrome);
- skin rashes (immunological syndrome).
The listed symptoms are not always found in full in an individual patient. Most often, the clinical picture is limited to two or three symptoms, such as shortness of breath and chest pain.
Tests and diagnosis of pulmonary embolism
Instrumental diagnostics of this condition includes:
- Chest X-ray . In the lungs, discoid atelectasis , a raised dome of the diaphragm, or pleural effusion . All these signs are nonspecific, but exclude various causes of pain and shortness of breath.
- ECG.
- Echocardiography . It is of key importance in diagnosis, especially in patients with unstable hemodynamics. This test directly detects blood clots in the right side of the heart, and blood clots in the large arteries of the lungs (trunk and main branches). An indirect sign of pulmonary embolism detected by echocardiography is overload of the right chambers. An indirect sign of pulmonary artery thrombosis is identified - overload of the right ventricle: expansion of the ventricular cavity, unusual movement of the septum between the ventricles and a D-shaped left ventricle.
- Ultrasound of the deep veins of the extremities.
- A special research method is ventilation-perfusion scintigraphy . This is a safe study that involves the intravenous administration of albumin microspheres that are labeled with technetium. Albumin microspheres block pulmonary capillaries and lung perfusion is assessed based on this feature. This study is complemented by a ventilation study, which increases the specificity of the examination (in case of thrombosis, ventilation in segments of the lungs in which there is poor blood supply remains normal). That is, a discrepancy between ventilation and perfusion is detected. Radioactive radiation during scintigraphy is lower than during CT angiography. Perfusion scintigraphy alone can be performed in patients with a normal radiograph.
- CT angiography . This study has become the method of choice for diagnosing pulmonary vascular pathology. The pulmonary arteries can be viewed down to the segmental branches. The specificity of the method is 96%. The technique is optimal for diagnosing a patient whose condition is stable. In another case, the patient cannot be transported from intensive care.
- Pulmonary angiography is considered the gold standard for diagnosing PE. However, it is rarely performed since a less invasive test, CT angiography, has become available. Diagnosis is based on identifying a blood clot that causes a defect in the filling of the pulmonary artery branch or is completely absent. The method allows you to obtain images of peripheral pulmonary arteries and detect blood clots of 1-2 mm in the smallest arteries. A contrast agent is injected for the study.
ECG signs of PE and radiographic signs
Blood tests:
- D-dimer is a fibrin degradation product. Its increase in plasma is observed during acute thrombosis - this is explained by the activation of fibrinolysis and coagulation. A normal D-dimer level makes the diagnosis of PE unlikely. Also, this indicator is nonspecific, since fibrin overproduction is observed during inflammation, bleeding, myocardial infarction , aortic aneurysm , oncological processes, trauma, and surgery. The specificity of D-dimer for thrombosis decreases with age. This indicator is paid attention to during treatment, since an increase in its level after the end of anticoagulant treatment indicates a risk of relapse.
- of brain natriuretic peptide increases , which is associated with distension of the right ventricle. The degree of increase is proportional to the severity of the patient. However, an increase in this marker is nonspecific, since it can be observed with myocardial ischemia , left ventricular hypertrophy , sepsis and tachycardia . However, the absence of a significant increase indicates a favorable prognosis for pulmonary embolism.
Diagnostics
The list of diagnostic methods used for pulmonary embolism is quite extensive, and their choice depends on the degree of likelihood of pulmonary embolism and the general condition of the patient. The most common criteria for assessing the clinical probability of pulmonary embolism are:
- fractures or surgeries suffered within the previous 3-4 weeks;
- the presence of malignant tumors;
- a sharp decrease in blood pressure (from 90/50 mm Hg);
- hemoptysis;
- increased heart rate;
- unilateral pain in the lower limb;
- age over 65 years.
These criteria are also called clinical markers.
It is important to exclude heart and lung diseases that may cause symptoms similar to PE. For this purpose, separate diagnostic studies are prescribed. When diagnosing pulmonary embolism, the following methods are used:
- Collection of complaints and assessment of the patient’s general condition to determine the likelihood of pulmonary embolism.
- Urine and blood tests (biochemical and general).
- Coagulogram – assessment of blood clotting indicators.
- Determination of D-dimer in blood. This study determines the intensity of formation and destruction of fibrin clots. D-dimer is an indicator that helps determine the intensity of fibrin destruction. With thrombosis of veins and arteries, due to increased thrombus formation, it will be increased.
- Scintigraphy is a two-dimensional imaging technique using radioactive isotopes to study blood flow in the lungs. Visualization is based on determining the radiation of isotopes introduced into the body of the subject.
- ECG in dynamics. Carried out to exclude myocardial infarction and other diseases of the cardiovascular system
- X-rays of light. This study is necessary to rule out rib fractures, air accumulation in the pleural cavity, and pneumonia.
- Angiopulmonography. To determine the size and location of the blood clot, a contrast agent is injected into the pulmonary arteries.
- Ultrasound examination of the veins of the lower extremities.
- MRI - three-dimensional imaging helps determine the location of arterial occlusion, if any. Used infrequently due to high cost. As a rule, the patient is referred for an MRI if the ECG or ultrasound confirms the doctor's suspicions about a possible thromboembolism.
In children
Thrombosis in children occurs much less frequently. For their occurrence, a combination of acquired and congenital factors is necessary. Of the hereditary ones, it is worth noting the hereditary decrease in the activity of antithrombin III and proteins C, S, which are natural anticoagulants. Acquired factors:
- severe somatic diseases
- infectious diseases;
- systemic connective tissue diseases;
- malignant tumors;
- connective tissue dysplasia ;
- hemolytic anemia;
- antiphospholipid syndrome.
The most important factor in thrombosis is the use of an intravascular catheter. Up to 80% of thromboses are associated with catheterization. In children, pulmonary embolism is often associated with deep vein thrombosis. Venous thrombosis in children is preceded by infection, thrombocytopenic purpura , antiphospholipid syndrome , and in some, excessive insolation. Recurrent pulmonary embolism also occurs, but the source of thrombosis cannot be identified. PE in children is often mistakenly regarded as pneumonia .
Prevention of pulmonary embolism
- Primary prevention of embolism after surgery on the pelvic organs and orthopedics.
- If the risk of thromboembolism is low, prevention involves the use of compression stockings or elastic compression with an elastic bandage of the lower extremities.
- enoxaparin or fondaparinux or dabigatran until discharge .
- If the risk is high, these recommendations should be followed for a month.
- New oral anticoagulants are registered for primary prevention after orthopedic surgery.
There are also non-surgical patients (chronic heart failure class III-IV), who are also at risk for pulmonary embolism. Their choice of anticoagulant is the same. The standard of treatment is enoxaparin .
Secondary prevention is the prevention of recurrent thromboembolism. Without prophylaxis, recurrence of pulmonary embolism within the first three months is observed in 20-45% of patients. With prevention, the number of relapses is reduced to 1%. Warfarin is used for prevention , and for the first six months, cancer patients are prescribed low molecular weight heparins ( Fraxiparin , Fraxiparin Forte , Clexane , Enixum , Fragmin , Daltep ), then they are transferred to oral medications ( vitamin K antagonists - Warfarin , Warfarex ).
How long should I take them? To do this, the risk of bleeding is assessed based on risk factors (age 65 years or older, history stroke malignant tumor , renal and liver failure , diabetes mellitus , low platelet levels, anemia and others). The risk of bleeding is high if more than two risk factors combine.
It is also possible to use “new” anticoagulants for secondary prevention, which are included in the American Guidelines for the prevention of pulmonary embolism. Rivaroxaban ( Xarelto ) is superior in long-term treatment and can be prescribed for 6-12 months with a low risk of bleeding, providing protection against relapse.
Treatment of pulmonary embolism
Treatment of a patient with pulmonary embolism consists of two tasks: 1) saving the patient’s life, 2) restoring the vascular bed, if possible, to a normal state.
Currently, one of the main methods of treating severe pulmonary embolism is the dissolution of the blood clot with special drugs - thrombolytic therapy.
The prospects for treatment largely depend on the massiveness of the pulmonary embolism and the severity of the patient’s condition.
The prognosis for grades I and II of PE with adequate treatment is usually favorable. PE of III and especially IV degree can quickly lead to death if timely and effective assistance is not provided.
Prevention of pulmonary embolism
All patients, both surgical and therapeutic, who have an increased risk of developing this complication, need prevention of pulmonary embolism.
In severely ill patients, functional prevention of phlebitis and phlebothrombosis of the legs and pelvis should be constantly carried out by getting up early and walking as hard as possible. The most important role, especially in bedridden and operated patients, is played by elastic compression of the legs (elastic bandages or special knitwear). In addition, if there is a high risk of developing embolic venous thrombosis, drugs that reduce blood clotting should be used.
Consequences and complications
- Hemodynamic disturbances (increased vascular resistance in the pulmonary artery system and increased afterload on the right ventricle).
- Respiratory failure.
- Hypoxia.
- Pulmonary-pleural complications ( atelectasis , pleurisy , lung abscess , pulmonary infarction , pneumonia , pyopneumothorax , pleural empyema ).
- Post-embolic pulmonary hypertension .
List of sources
- Vatutin N.T., Sklyannaya E.V., Eshchenko E.V. /Pulmonary embolism. Review of recommendations of the European Society of Cardiology for diagnosis and treatment (2014 // Practical Angiology. - 2015. - No. 1 (68). - P. 5-18.
- Russian clinical recommendations for the diagnosis, treatment and prevention of venous thromboembolic complications // Phlebology. — 2015.— No. 4, issue 2. 46 p.
- Vatutin N.T. Emergency cardiology. - Donetsk, 2011. - 236 p.
- Vatutin N.T., Kalinkina N.V., Perueva I.A. /Pulmonary embolism // Practical angiology. – 2011. – No. 2. – P. 32-40.
- Vatutin N.T., Kalinkina N.V., Eshchenko E.V. and others. Pulmonary embolism (basic information and own observation) // Heart and Vessels. – 2013. – No. 1. – P. 120-123.