Types of croup
There are two types of croup (depending on what infections accompany the painful condition) - true and false. The second type is much more common.
True croup develops exclusively against the background of diphtheria. It is this form of the disease that mainly occurs in adult patients.
False croup is characterized by the “capture” of a larger territory. Not only the area of the child’s vocal cords suffers, but also the mucous membrane of the larynx located below. Croup is most often caused by viruses (influenza, measles, parainfluenza, whooping cough, adenoviruses, chickenpox), less often by bacteria (pneumococci, staphylococci, Haemophilus influenzae and streptococci). Allergic croup is even less common (this type of false croup can be observed in adults).
The most common painful condition is a complication or manifestation of the following pathologies:
- ARVI;
- acute respiratory infections;
- chicken pox;
- measles;
- scarlet fever;
- pharyngitis;
- adenoiditis;
- acute rhinitis.
There are four degrees of severity of false croup (depending on the degree of laryngeal stenosis and respiratory failure):
- 1st degree (compensated stenosis): the patient experiences anxiety, shortness of breath and cough appear only during excitement or physical exertion, and are absent in a calm state. This is a moderate condition. The child may experience hoarseness, but not in all cases.
- 2nd degree (subcompensated stenosis). Shortness of breath and cough are observed not only with anxiety and physical exertion, but also at rest. The patient's skin acquires a bluish tint. The patient suffers from sleep disturbances, is often agitated, and has hoarse and wheezing breathing. The general condition of the child’s body is serious.
- 3rd degree (decompensated stenosis). The patient can be either in an excited or inhibited state. Due to swelling of the larynx, it is difficult for him to inhale, and exhalation is much shorter than usual. The patient becomes covered in cold sweat, turns pale, and is sometimes in a confused state. With this degree of stenosis, the patient's general condition is very serious.
- 4th degree (asphyxia). The skin becomes bluish, the pupils dilate, the patient breathes silently, but shallowly. The patient is unconscious, and in some cases convulsions are observed. This is an extremely serious condition that can be fatal.
False croup can flow from one stage to another quite quickly and imperceptibly. Therefore, it is necessary to urgently seek medical help for any symptoms of this disease.
In children
At the beginning, the disease manifests itself as a common cold, but after a few days the child becomes hoarse or even loses his voice, his breathing becomes noisy, and even with slight physical exertion the child develops shortness of breath. At night the baby gets worse, a barking cough appears, the child cannot clear his throat, so he cannot sleep.
During a cough, a whistling sound is characteristic when the child wants to draw air into the lungs, which passes with difficulty, since the inflamed channels of the larynx and trachea are narrowed. This whistling sound is called inspiratory stridor. Due to difficulties with coughing, the abdominal muscles tense, which then hurt, as if after a long workout.
Symptoms of croup
Signs of the disease state depend on its type. True croup has the following symptoms:
- increase in body temperature to 38.5 degrees;
- redness of the throat mucosa;
- swelling of the tonsils;
- grayish-white dense coating on the tonsils.
With false croup, the following signs are observed:
- inflammation and swelling of the larynx, trachea;
- pale skin;
- increased body temperature;
- blue lips;
- hoarseness of voice;
- difficulty breathing when inhaling;
- barking cough;
- whistling, bubbling breathing;
- dyspnea;
- the patient's refusal to eat;
- difficulty swallowing saliva;
- anxiety, excitement.
False croup usually develops on days 1-5 of an infectious disease.
Character of the current
According to the nature of the course, croup is divided into uncomplicated and complicated (when other respiratory tract diseases are added to the croup). False croup (acute laryngitis) is divided according to the type of disease in the respiratory tract into the following types of laryngitis:
- edematous, when the throat becomes red and swollen. Where the folds of the tonsils are located, small gray ridges are visible that narrow the lumen of the glottis;
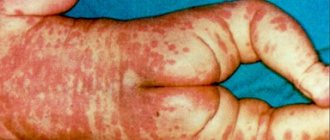
- hemorrhagic, when there are a lot of hemorrhages on the mucous membrane of the throat in the area of the trachea and larynx, there are edematous ridges in the subglottic area, due to which the lumen of the larynx becomes very narrow, bloody crusts;
- catarrhal-edematous – swelling of the throat is accompanied by a hoarse voice and rhinitis;
- ulcerative, when there is swelling in the subglottic area, the lumen of the larynx is very narrow and a lot of pus accumulates in it.
Diagnosis of croup
The main method of diagnosing this painful condition is to examine the patient by a doctor. The doctor collects anamnesis, listens to internal organs, evaluates clinical manifestations, and performs laryngoscopy (examination of the larynx). If the collected data is not enough to assess the degree of croup or identify the causative agent of infection and choose a treatment method, the patient is prescribed blood tests and bacteriological studies. The patient may also be referred for rhinoscopy, x-ray of the sinuses and lungs, otoscopy, puncture, pharyngoscopy.
To identify the causes of croup and eliminate them, consult an otolaryngologist.
Treatment of croup
Treatment is prescribed individually and comprehensively. Methods can be divided into two groups: treatment aimed at eliminating the underlying disease (infection) and methods that help cope directly with croup. Infections are treated with antiviral drugs or antibiotics.
Treatment methods for croup itself depend on the type of disease:
- With true croup, the patient is hospitalized. In addition to treating diphtheria (with a special serum), intoxication is removed.
- For false croup, inhalations (steam or ultrasound) are used, antitussives and sputum expectorants are prescribed, and, if necessary, antihistamines. In severe cases of stenosis, hormonal therapy can be carried out, in which the swelling of the mucous membrane and spasm of the laryngeal muscles are relieved with the help of medications and inflammation is eliminated. If the patient has increased excitability, antipsychotic or sedative medications will also be needed. The following may also be prescribed: laser therapy, exercises to restore voice, as well as procedures to improve immunity.
Surgical treatment is performed very rarely. This operation is called tracheotomy and is performed in case of severe narrowing of the lumen of the larynx and the threat of asphyxia (suffocation).
Since croup always accompanies other diseases, diagnosis and/or treatment may require the help of specialists such as a pediatrician or therapist, phthisiatrician, pulmonologist, or venereologist.
Introduction
Viral infection occupies a leading position in the etiology of acute diseases of the upper and lower respiratory tract among initially healthy people of any age.
In patients with chronic diseases of the bronchopulmonary system, a viral infection exacerbates the process [1]. In the pediatric population, acute conditions accompanied by obstruction of the upper respiratory tract (URT) play a significant role. The presence of fever often helps to distinguish a group of infectious diseases.
And the appearance of symptoms from birth is typical for children with a congenital anomaly of the respiratory system. However, in practice, viral infections are not always accompanied by high fever, the onset of congenital pathology is not always observed from birth, and other respiratory disorders in children in the first 3 years of life can occur suddenly, without any obvious reason. Therefore, both pediatricians and nursing staff in acute pediatrics should be as alert as possible regarding the possibility of the situation changing in a matter of seconds with the development of severe respiratory distress syndrome, incl. with a fatal outcome [2].
Medical workers, especially outpatients, who are less likely to encounter severe acute conditions, need to constantly improve their skills, incl. in specialized simulation centers, in order to ensure timely diagnosis of upper respiratory tract obstruction to improve the quality of care. Such tactics have repeatedly justified themselves both in Russia and in other countries [3, 4].
The most common symptom of pathology in any part of the respiratory tract is cough. Often, only on the basis of the timbre, frequency, and time of cough onset, one can with a high probability suspect a particular disease.
Among a large group of coughing children, patients with laryngeal stenosis stand out clearly. The clinical picture of typical laryngostenosis is quite characteristic: stridor, inspiratory dyspnea, hoarseness and a rough cough. Different terms are used to characterize it: “ringing,” “barking,” “guttural,” but once heard, it cannot be confused with anything else. However, in clinical practice we have to deal with completely different situations. Sometimes children are admitted to the hospital with typical mild stenosis who received unacceptable therapy at home. And sometimes children with a seemingly typical clinical picture of laryngotracheitis “sound” a little differently or their condition does not improve with standard therapy, then it is necessary to exclude other pathologies of the upper respiratory tract.
Croup
One of the most common causes of respiratory distress in young children is acute inflammation of the mucous membrane of the larynx and trachea. With the exception of a small percentage of situations, the cause of inflammation is infection, which is accompanied by hyperemia, edema, necrosis and epithelial sloughing [5].
Taking into account the diameter of the lumen of the child’s larynx, even slight swelling of the mucous membrane leads to a significant concentric narrowing of its cross section [6]. Children compensate for this by breathing more frequently and deeply. As the process progresses, the effort expended on inhalation leads to the opposite result: the air flow in the larynx becomes turbulent, and during inhalation the walls of the subglottic space close. Characteristic clinical symptoms appear: inspiratory stridor, hoarseness, and a rough “barking” cough. Rapid progression of stenosis without timely assistance leads to the inability to synchronize the respiratory movements of the muscles of the chest and abdomen. The child quickly becomes exhausted and develops hypoxia and hypercapnia with respiratory distress and possible death [6, 7]. Laryngotracheitis, laryngotracheobronchitis and spastic croup are included in the croup syndrome in children [6].
Epidemiology
As stated above, the main cause of inflammation of the mucous membrane of the larynx and trachea is an infection, in the vast majority of cases viral. The most common respiratory viral pathogens are considered to be human rhinovirus, RS (respiratory syncytial) virus, influenza, adeno-, coronavirus. However, relatively little attention has been paid to the human parainfluenza virus, which is tropic to the mucous membrane of the respiratory tract, often leading to illness in children of the first year of life and patients with immunodeficiency conditions. In initially healthy adults, parainfluenza is accompanied by mild upper respiratory tract symptoms. But it is this virus that is associated with croup, especially its severe course [1].
Parainfluenza is an RNA virus belonging to the paramyxaviruses. It usually circulates in late autumn or early spring, but sporadic cases can be recorded throughout the year. Croup is most often associated with serotypes 1, 2, 3 and 4 [8]. For example, in Vietnam, in children under 2 years of age, serotypes 1 and 3 were most often isolated with croup (p < 0.005) [9].
Interestingly, type 1 mainly circulates once every 2 years, while types 2 and 3 circulate annually [10].
There is no doubt that at least up to 75% of cases of croup are associated with parainfluenza virus [11, 12].
Less commonly, it is provoked by other respiratory viruses: RS-, influenza A, metapneumo-, adenovirus [8]. Even less frequently, a number of authors indicate the role of Mycoplasma pneumoniae, coronavirus, enterovirus, rhinovirus, measles virus, and mumps. Don't forget about the so-called true croup associated with Corynebacterium diphtheriae [13].
According to the Department of Diagnostics and Rehabilitation Treatment of the Federal State Institution NNPCZD of the Ministry of Health of the Russian Federation, among hospitalized children the cause of croup in 72% of cases was the parainfluenza virus, then RS and adenovirus were isolated with almost the same frequency, and influenza A virus was isolated in only 2% of children [14].
With such a wide range of pathogens and the extreme prevalence of respiratory viruses is also associated a high incidence of morbidity. Every year, about 3% of children suffer from croup [12].
For example, in the USA, 8,481 children under the age of 5 years are hospitalized annually for stenosing laryngotracheitis, i.e. 0.4 per 1000 children per year, which costs $58 million. Most cases occur in children under 2 years of age [10].
There is evidence that croup occurs almost 2 times more often in boys, mainly between the ages of 6 months and 3 years with a peak in the second year of life. However, cases of the disease have been described in children 3 months of age and adolescents [8, 15].
Clinic
As a rule, laryngotracheitis is not severe and is stopped without any active interventions. Therefore, most children can receive treatment at home. However, in some cases, rapid progression of subglottic edema occurs, which can lead to life-threatening obstruction [12].
In Canada, up to 4% of children with croup are hospitalized due to the severity of the condition; moreover, 1 in 170 hospitalized children requires intubation and assisted breathing [16].
According to other data, up to 9% of children (average age 18 months) required intensive care, while croup recurred in 3% within 30 days [7].
The duration of intubation for severe croup can be up to 60 hours, and 30% of cases are associated with parainfluenza virus. In 6.5% of children, repeated deterioration of the condition can be expected after extubation, which, according to some authors, is not associated with either the duration of intubation or the child’s body weight/age [17].
Severe stenosis, accompanied by a decrease in saturation less than 95%, as well as a history of intubation, significantly increase the length of hospital stay (p <0.05) [18].
Classically, the first symptoms of croup occur suddenly, usually in the evening or at night, which appears to be related to the circadian rhythm of serum cortisol levels, which increase from 23:00 to 04:00 with a peak concentration at 8:00 a.m. Rarely, symptoms may progress throughout the day. The child develops a rough cough, sometimes with a metallic tint, inspiratory stridor, and hoarseness, usually with a low temperature. Stridor is usually present only during inspiration. With rapid deterioration, it also manifests itself on exhalation with the development of mixed shortness of breath. However, at least several hours pass before the onset of clinically significant distress, which allows measures to be taken to improve the child’s condition [8].
The duration of the disease in 60% of cases does not exceed 2 days; rarely, in some patients, symptoms can persist for up to 5–6 days. Laryngeal stenosis may be preceded within 24–48 hours by nonspecific manifestations of a respiratory viral infection: fever, rhinitis, cough [8, 12].
In the classical course, the diagnosis of croup is not in doubt and can be established on the basis of anamnesis and physical examination without additional examination. In cases of doubt, lack of response to treatment, or development of severe distress, blood tests and chest x-rays are performed [7, 19].
Despite the lack of recommendations for conducting virological and bacteriological studies to confirm this diagnosis, in the USA, for example, an analysis of more than 6,000 relevant case histories showed an almost 5-fold increase in the number of prescriptions for additional research methods or drugs [20].
Differential diagnosis
Croup should be differentiated from conditions accompanied by stridor and sudden obstruction of the upper respiratory tract: epiglottitis, bacterial tracheitis, foreign body of the respiratory tract or esophagus, retropharyngeal or peritonsillar abscess, respiratory tract injury, diphtheria, angioedema, spasmophilia, burn with caustic substances [7].
Not in terms of frequency, but in terms of the severity of the course and possible undesirable consequences of inspiratory dyspnea, it is necessary to exclude epiglottitis - acute bacterial inflammation or phlegmon of the epiglottis. In most cases of epiglottitis, it is possible to isolate Haemophilus influenzae type b, much less often - streptococci and pneumococci.
It is characterized by a sudden onset, always with high fever, dysphagia, salivation, toxicosis, and anxiety. The voice is muffled, but there is no hoarseness and the “barking” cough typical of croup. A distinctive low-pitched expiratory sound and moderate inspiratory stridor are common. As a rule, older children get sick. However, with the beginning of vaccination against Haemophilus influenzae and pneumococcus, cases of epiglottitis began to occur less frequently [7].
In general, modern healthcare pins great hopes on vaccine prevention in terms of significantly reducing the incidence of pneumonia, croup and bronchiolitis in children in the first year of life [10].
If phlegmon of the epiglottis is suspected, the child should not be disturbed under any circumstances; pharyngoscopy must be performed with extreme caution, without touching the root of the tongue and especially the epiglottis with a spatula, so as not to provoke its sharp swelling. Therefore, it is better to carry out this manipulation without a spatula or in the presence of a resuscitator ready for intubation. Also, if epiglottitis is suspected, sedation and inhalation should not be used, therefore, if it is impossible to completely exclude viral croup, it is better to give the hormone orally. The patient is necessarily hospitalized for close observation with readiness for intubation, and parenteral administration of an antibiotic is urgently started [7, 21].
A study was conducted in Korea to identify differential criteria for viral croup and epiglottitis. In addition to the signs described above, the ratio of boys to girls with croup was 1.9:1, with epiglottitis - 2.3:1, the average age was 2.2-2.0 and 5.6-5.8 years, respectively. The seasonality of croup was recorded with a peak in July, epiglottitis - in May. Cough, fever and dyspnea were observed in both groups. But with epiglottitis, dyspnea, sore throat and vomiting were significantly more common (p<0.05) [15].
One alternative diagnosis for inspiratory stridor may be bacterial tracheitis. A severe bacterial infection requiring treatment may possibly complicate croup. Typically, bacterial tracheitis begins with a sudden worsening of symptoms after an episode of croup with a sharp increase in temperature, toxicosis and failure of previously administered therapy. The condition is fraught with occlusion of the respiratory tract due to the pronounced production of viscous secretions. Treatment is carried out in a hospital and includes parenteral antibiotic therapy and respiratory monitoring. Sometimes intubation with ventilatory support may be required [7, 21].
A foreign body in the respiratory tract or esophagus, as well as viral croup, most often occurs in boys under 3 years of age. If the parents did not note an episode of sudden coughing against the background of complete health, further complaints can be very diverse: prolonged cough, broncho-obstruction, dysphagia or loss of appetite, as well as stridor. The available literature contains many publications devoted to cases of laryngotracheitis due to a foreign body. For example, a case of croup that lasted a week due to a foreign body in the larynx [22], or croup that was intractable for 2 weeks and decreased appetite in a 20-month-old boy, followed by the removal of a loquat seed from the esophagus [23].
Hemangioma of the respiratory tract often occurs with inspiratory stridor [24].
Differential diagnosis of viral laryngeal stenosis is also carried out with a retropharyngeal abscess, thermal or chemical burn of the respiratory tract, angioedema and other conditions.
Viral and recurrent croup
It was previously mentioned that croup syndrome in children includes laryngotracheitis and laryngotracheobronchitis, which acutely arise against the background of a viral infection. There is also spastic, or recurrent, croup [6], which is not always associated with a viral infection and is not necessarily accompanied by a prodrome or fever. It develops suddenly, also usually at night, usually ends faster, but often recurs.
Despite the fact that both types of croup are well known and have long been described, there are still virtually no publications based on well-designed randomized evidence-based studies that present a clear algorithm for the differential diagnosis of these conditions [5].
Spastic and viral croup are pathogenetically different conditions with the same symptoms. Therefore, recurrent croup cannot be a diagnosis and requires verification of the etiological factor [24].
There is evidence that spastic croup is more common in children with bronchial asthma or atopy. In the presence of a burdened allergic history or in children at risk of developing bronchial asthma, relapses of croup can also occur against the background of a respiratory viral infection. However, it is believed that in such a situation, swelling of the mucous membrane does not occur in response to infection, but as an allergic reaction to a viral antigen. However, routine testing of immunoglobulin E (IgE) in children with recurrent croup did not show its feasibility [7, 26].
In addition, it has been proven that in a large proportion of children with recurrent laryngeal stenosis, the provoking factor is gastroesophageal reflux [27]. According to various sources, the incidence of reflux ranges from 20 [28] to 60% [29] and almost all children respond well to antireflux treatment (p = 0.006) [30].
This frequency of reflux made it possible to apply the tactics of empirical prescription of antireflux therapy for recurrent croup even in the absence of other clinical symptoms. The authors of this opinion believe that it is possible to avoid unnecessary invasive and expensive endoscopic examination in case of a successful response [27].
Certain anatomical features may also cause recurrent episodes of laryngeal stenosis.
An American review of 885 eligible patients who underwent diagnostic bronchoscopy found that, in addition to reflux esophagitis and atopy without significant endoscopic changes, serious pathology was detected in 8.7% of cases. Such findings included tracheobronchomalacia, post-intubation cicatricial stenosis of the larynx, as well as an anatomically narrow subglottic space. Significant endoscopic changes also correlated with age less than 3 years (odds ratio [OR] = 3.22, 95% confidence interval [CI] – 1.66–6.27), with age less than 1 year (OR = 2.86, 95% CI –1.28–6.40) and prematurity (OR=2.90, 95% CI – 1.39–6.06) [28,31].
These data are comparable with the results of other published studies, which showed a clear association of serious endoscopic changes with a history of intubation (p = 0.002) [27] and (p = 0.003) [29], as well as age less than 3 years (p = 0.01) [27] and (p=0.013) [29].
A number of authors indicate that the number of recurrent croup, the cause of which may not be clear, reaches 45% [30].
Malacia of the upper respiratory tract can also be accompanied by chronic stridor [21].
On the one hand, organic changes in the larynx and trachea are not so common in the population, on the other hand, children in this category should be isolated from the general mass and carefully examined due to the need for individual tactics for their management [24].
Severity rating
To assess the severity of croup in Russia, until recently, the V.F. scale was used. Undritsa 1969, in which 4 stages of acute laryngeal stenosis are distinguished according to the presence and severity of clinical manifestations.
In foreign literature, croup is assessed using the no less well-known 3-point Westhley scale of 1978 (The Westhley Croup Score). The degree of severity is determined based on the sum of points (maximum 17) depending on the severity of individual symptoms (see table) [32]. In daily practice, this scale may well be sufficient, because... it reflects the most striking clinical manifestations of the disease and vital indicators [33].
Misconceptions
Humidified oxygen. For more than 100 years, children with croup have been treated with humidified air. Until now, some hospitals use numerous oxygen tents, steam inhalations, etc. In addition to the fact that these manipulations are inconvenient and cause negativity on the part of the child, his excessive anxiety, it has been proven that no significant improvement in the condition occurs during such treatment (A) [34, 35].
The results of a study that included 140 children with severe and moderate croup have been published. The children were divided into three groups taking into account the method of treatment: 1st group - oxygen inhalation was used as a placebo (in terms of humidity it is comparable to room air), 2nd group - oxygen humidified to 40%, and 3rd group - oxygen, humidified to 100%. There were no significant differences in the duration of the disease, the need for hospitalization and additional prescriptions [36].
The results of a study conducted at the National Scientific Research Center for Children's Hospital also long ago showed that improvements in croup symptoms, such as cough, shortness of breath, and anxiety, do not occur with inhalation of humidified air [37].
Therefore, only children with hypoxia, blood oxygen saturation below 92% and severe distress syndrome need oxygen. Oxygen is never given to a child by force, because... this leads to excessive stimulation. If the child refuses inhalation, a mask with a good supply of oxygen can simply be placed next to his face [38].
However, since laryngeal stenosis usually develops at night, parents begin to panic, not knowing how to help their child. Therefore, recommendations for providing assistance at home, for example, before the arrival of an emergency medical team, include hot steam, exposure to cold air for 10–15 minutes, distraction, calming the child, drinking small sips of iced drinks up to several times within an hour. It is forbidden to give cough medicines or smoke in the presence of a child [39].
Helium. Helium inhalations were also actively prescribed for treatment. It was believed that due to its low density, turbulence in the narrowed lumen of the larynx is leveled out and stridor is reduced. However, recent studies of the effectiveness of such treatment show that if helium improves the condition of a child with croup, it is only short-term and subject to parallel administration of corticosteroids [34, 38, 40].
Other data indicate that the improvement in clinical picture with helium inhalation therapy does not have a significant advantage compared with standard treatment [6, 41]. Therefore, today we do not have sufficient grounds for the routine use of helium in children with croup syndrome (C) [34, 40].
Antibiotics. In the discharge summaries of most children hospitalized in our department from other hospitals in Russia with acute or recurrent croup, we see the prescription of systemic antibacterial therapy for each episode of laryngeal stenosis. Currently, both Russian and foreign treatment protocols do not recommend the empirical use of antibiotics, given that croup is a viral disease. Bacterial complications (bacterial tracheitis, pneumonia) occur so rarely (less than 1 in 1000) that prophylactic antibiotic administration is also not recommended [6, 7, 37].
Other drugs. There is also no published data on the use of antipyretics for croup other than to reduce fever and relieve pain. Treatment with antitussives and decongestants is not accompanied by significant improvement. And taking into account that the subglottic space belongs to the URT, there is no physiological basis for the use of β2-mimetics, as well as evidence of their effectiveness [6, 7].
Treatment
Glucocorticosteroids (GCS) are still among the main drugs for the treatment of croup syndrome [34]. The effectiveness of their use is due to a pronounced reduction in swelling of the laryngeal mucosa.
In modern literature, evidence-based studies are presented again and again confirming the effectiveness of their use in the rapid relief of croup symptoms, reducing the need for hospitalization and hospital stay, reducing the risk and duration of intubation, and the need for reintubation.
The number of repeated visits to the doctor and the need for additional appointments (A) are significantly reduced [6, 42, 43].
Traditionally, parenteral administration of dexamethasone is used at a dose of 0.6 mg/kg [44].
Our data show that with only the administration of dexamethasone, croup in 88% of children is stopped within the first day [14].
Until now, there has been no sufficient evidence base for the effectiveness of prednisolone. The results of a study on the treatment of mild to moderate croup with prednisolone 2 mg/kg/day for 3 days compared with 1 dose of dexamethasone 0.6 mg/kg and 2 doses of placebo have now been published. There was no significant difference in the duration of symptoms (2.8 vs. 2.2 days; p=0.63), barking cough (6.1 vs. 5.9 days; p=0.81), related care (2 vs. 7 %; p=0.34), duration of stress (1.39 versus 1.56 days; p=0.51) and the number of sleepless nights for parents (0.68 versus 1.21 nights; p=0.55) [ 2, 45].
Therefore, the administration of prednisolone in acute situations may also be recommended [46].
In addition, almost identical effectiveness of both oral and parenteral administration of dexamethasone has been proven [44, 47]. When administered orally, it is well absorbed with rapid peak concentrations comparable in speed and efficacy to parenteral administration [46].
At the same time, oral administration is certainly less traumatic for the child, which is important when excessive anxiety leads to increased inspiratory dyspnea. An injection solution mixed with sweet syrup can be used orally. With such recommendations, vomiting occurs in less than 5% of cases. Improvement occurs within 1–3 hours and lasts from 24 to 48 hours [48, 49].
Moreover, sufficient studies indicate that a dose of 0.15 mg/kg dexamethasone is comparable in effectiveness to a higher dose [50, 51]. On the other hand, a number of authors still recommend 0.6 mg/kg dexamethasone due to clinically significant responses from a larger number of patients [52, 53].
Pending new studies, definitive dosage recommendations cannot be made, so the clinician may use one dosage or another depending on the severity of the disease. In our department, a dose of 0.3 mg/kg dexamethosan is often used with the same effect as 0.6 mg/kg.
There were no controlled studies to answer the question: is additional hormone administration required after the first dose? Due to the short course of the disease, most patients often require only one administration [34, 54].
In our department, only 15% of patients required more than 1 dose of hormones [14, 37].
Due to their high efficiency and speed of onset of effect, systemic corticosteroids are the drug of choice for acute laryngeal stenosis and many other emergency respiratory conditions in pediatrics with minimal risk of developing serious consequences. Children with immunodeficiency conditions or recent contact with patients with chickenpox will require an individual approach [47, 55].
GCS can also be prescribed inhaled in the form of budesonide through a compressor nebulizer [21]. Budesonide has shown comparable efficacy to oral dexamethasone and can be used for vomiting caused by oral corticosteroids.
If the child’s negativism and fear are pronounced, it may be more difficult to force him to inhale. Although we rarely encounter such situations in practice, especially from older children. But we were convinced that 12 hours after inhalation of budesonide in children the positive effect was persistently maintained and in 85% of cases its single use was sufficient [14]. However, the cost of this drug may limit its use in routine pediatric practice [8].
Epinephrine has been successfully prescribed to children even with severe croup for many decades, reducing the severity of symptoms within 30 minutes and significantly reducing the risk of needing intubation and length of hospitalization [7]. Inhalation of adrenaline leads to a vasoconstrictor effect on the mucous membrane of the subglottic space, reducing its swelling and inflammation. And due to its rapid action in both mild inspiratory stridor and severe distress syndrome, it can be recommended in routine practice (C) [6, 8, 34]. The duration of action sometimes exceeds 60 minutes and ends within 2 hours. After this, the patient’s condition usually returns to its original state, but does not worsen [7].
Traditionally, the racemic form of epinephrine has been used to treat croup in North America. Although today it has become virtually unavailable, some pediatric clinics in the United States and Western Europe continue to report its use.
It is known that L-adrenaline is as effective and safe as racemic [6, 8].
There are some differences in dosage according to different guidelines. Some suggest that children of any age use a standard dose of 0.5 ml of 2.25% racemic epinephrine or 0.5 ml of L-adrenaline at a dilution of 1:1000 [7], others - 0.05 ml/kg (maximum 0.5 ml) racemic adrenaline 2.25% or 0.5 ml/kg (maximum 5 ml) L-adrenaline 1:1000 [6].
A report was published on the development of ventricular tachycardia and myocardial infarction in an initially healthy child with croup who received three inhalations of epinephrine within an hour [56]. Therefore, it is strictly not recommended to use repeated doses, except in cases of significant respiratory failure. Despite the fact that a single use is not accompanied by a significant increase in blood pressure and heart rate - heart rate [46].
Combined treatment of GCS with adrenaline in severe situations can be considered more effective than monotherapy.
A study in Iran showed a significant superiority of parenteral administration of prednisolone followed by inhalation of L-adrenaline in severe croup compared to dexamethosone with placebo in relieving stenosis (p<0.009) and reducing heart rate (p<0.026) [18, 45].
In children with severe distress, co-administration of inhaled budesonide and L-epinephrine may also be recommended, which is more effective than the use of epinephrine alone [8].
However, only one form of synthetic adrenaline is registered in the Russian Federation - R-adrenaline 1 mg/ml, for which subcutaneous, intramuscular and intravenous administration is prescribed. We did not find reliable information about the effectiveness of its inhalation use for croup.
Cases of recurrent laryngeal stenosis that require surgical treatment are quite rare [27,29].
But in unclear, untreatable cases of recurrent croup, the pediatrician should be wary of surgical pathology and promptly refer the child for one or another examination or consultation with a specialist [29].
In cases of endoscopic detection of significant subglottic stenosis (usually post-intubation [57]), otolaryngologists successfully use laryngotracheal reconstruction [58], as well as supraglottoplasty for congenital laryngomalacia with a significant reduction in postoperative need for systemic steroids (before and after 9.8 versus 0. 2 (p=0.003)) [59].
In our department, there were two cases of repeated inspiratory stridor due to a viral infection, in which the “metallic” sound of a cough and the low effectiveness of GCS were alarming. When performing computed tomography of the chest with contrast, in both cases an anomaly of the intrathoracic vessels was revealed with compression of the trachea by abnormally located vascular trunks. These children were successfully operated on by cardiac surgeons and subsequently did not experience relapses of croup syndrome.
Conclusion
Despite the fact that children with stenosing laryngotracheitis are regularly encountered in pediatric practice and in most cases recover safely, there is always the danger of a progressive deterioration of the condition, which requires the coordination of the work of medical personnel and the timely provision of effective care without unnecessary manipulations and useless medication prescriptions.
Even with severe croup, rapid relief is possible due to the wide availability of first aid drugs such as oral, parenteral and inhaled corticosteroids. This is usually enough.
However, in any situation, the pediatrician must be oriented regarding the indications for hospitalization, cases requiring additional examination or consultation with a specialist. Applying a multidisciplinary approach to each specific case will allow you to successfully overcome any difficult situation.
Prevention of croup
To prevent true croup, vaccination against diphtheria is carried out (the first vaccination is given to children at 3 months of age).
There are no specific measures to prevent false croup. In this case, it is recommended to follow the general rules for increasing immunity (after all, infections “settle” in a weakened body):
- to harden;
- monitor your diet (it should be correct and rich in all the beneficial substances the body needs, in particular vitamins D, C, A) and consume a sufficient amount of fluid;
- avoid inhaling tobacco smoke;
- maintain hygiene;
- Regularly ventilate the premises and maintain sufficient air humidity and cleanliness.
Also, to avoid infection, it is necessary to refrain from contact with carriers of infections. If infection does occur, you should immediately seek medical help.
Causes of the disease
The etiology is usually viral - parainfluenza viruses, especially type I, cause the disease in 75% of cases. Relatively common causes of false croup in children are respiratory syncytial virus, adenovirus and human coronavirus. The infection is usually spread by inhaling contaminated air, or by contact with objects that an infected person has come into contact with.
Influenza is a relatively rare cause that requires longer hospitalization and has an increased risk of another attack. Rhinovirus, enterovirus, and herpes simplex are sporadic causes of mild croup.
It is also possible to develop against the background of bacterial infection with mycoplasma, streptococcus, chlamydia, Staphylococcus aureus, etc. Diphtheria was the most common form of fatal stenosing laryngitis in another era, but now this disease is practically absent thanks to vaccination of the population.