Epilepsy is a chronic brain disease that manifests itself as uncontrollable seizures. They arise as a result of a pathologically enhanced impulse in the cerebral cortex. The disease is characterized by a wave-like course - after an attack there comes a period of remission. Clinical manifestations of the disease depend on the location of the lesion, the severity and type of seizures. At the Yusupov Hospital, neurologists diagnose epilepsy using the latest methods. For complex therapy, modern medications are used that are effective and have a minimal range of side effects.
Causes
One of the main causes of epilepsy is considered to be a hereditary predisposition: if parents have a history of seizure symptoms, then the child is more likely to develop them. Epilepsy also develops under the influence of the following reasons:
- Traumatic brain injury;
- Cerebrovascular accidents;
- Cerebral vascular dysplasia;
- Volumetric formations in the cerebral cortex;
- Neurosurgical intervention;
- Infectious diseases of the central nervous system;
- Previous ischemic or hemorrhagic stroke.
The occurrence of epileptic attacks is caused by the presence in the cerebral cortex of a stable focus with epileptic activity. Convulsive activity from the primary focus can spread through commissural fibers, cortical neuronal complexes, and the centrencephalic system of the brain. In the presence of increased convulsive activity over a long period of time, secondary lesions arise. They can, under the influence of certain factors, become independent and independent. As a result, the attack in the primary focus fades, but not in the secondary. This picture is observed in patients after two years of illness. Over the course of some time, tertiary foci of seizure activity may develop in the cerebral cortex.
Epilepsy can develop under the influence of the following provoking factors:
- Hormonal imbalances;
- Alcoholism and drug addiction;
- Chronic stress;
- Excessive emotional stress;
- Chronic fatigue.
Secondary attacks of epilepsy occur in patients suffering from brain tumors, cerebral vascular pathology, after hemorrhage in the head, due to poisoning with toxic substances.
It is very important to identify the disease early to reduce the likelihood of complications. Which doctor treats epilepsy? For quality therapy, it is necessary to be observed by a neurologist, epileptologist, or psychotherapist. As clinical symptoms progress, assistance from a physiotherapist or pharmacologist may be required.
Treatment of seizures
Help before diagnosis
Regardless of the cause, seizures are an acute condition that requires qualified medical care. Local painful spasms can be eliminated by self-massage, pinching, or stretching the muscle. When a generalized attack develops, it is important to provide first aid to the victim: place a cushion or pillow under the head, turning it on its side, clear the mouth of foam and mucus, and provide access to fresh air. The ambulance team stops the paroxysm with anticonvulsants; in case of high fever in children, antipyretics are administered.
Conservative therapy
Hospitalization is necessary for everyone who has developed a seizure for the first time, with severe and prolonged paroxysms, or with the presence of aggravating pathology. After verification of the diagnosis, along with symptomatic correction, treatment of seizures involves eliminating the causes and influencing the main pathogenetic moments of their development. Based on the clinical situation, the following groups of medications can be used to relieve attacks and treat the underlying disease:
- Anticonvulsants
. Treatment of partial and generalized epileptic seizures is carried out with lamotrigine, carbamazepine - in monotherapy or in combination with other drugs. Convulsive syndrome in organic pathology of the central nervous system can be treated with valproate, clonazepam; in the neonatal period, the drugs of choice are phenobarbital and diphenine. Refractory epistatus requires the administration of anesthesia (sodium thiopental, propofol). - Electrolytes
. Relief of spasmophilia and hyperkalemia is carried out with calcium preparations. Chloroprivate tetany and hyponatremia are treated with sodium chloride infusions; hypomagnesemia is corrected with magnesium sulfate. To eliminate metabolic alkalosis, saline solution and potassium chloride are used. - Hypotensive
. To correct blood pressure during eclampsia, including renal eclampsia, and hypertensive crises, peripheral vasodilators (sodium nitroprusside), beta blockers (esmolol), and ganglion blockers (pentamine, arfonade) are used. Diuretics - osmotic (mannitol, urea), loop (furosemide) - help eliminate concomitant cerebral edema.
In case of poisoning, antidote, detoxification, and infusion therapy are carried out; withdrawal forms of epistatus are treated with a combination of anticonvulsants and antipsychotics. Detection of neuroinfections requires appropriate antimicrobial (antibacterial, antiviral) correction; hypoglycemia is treated with glucose, pyridoxine-dependent seizures with vitamin B6. In some cases, a high-fat ketogenic diet is recommended to relieve seizure symptoms.
Surgery
Drug-resistant variants of epilepsy are an indication for more radical treatment. Among neurosurgical interventions, resections (temporal and extratemporal, hemispherectomy), disconnection operations (subpial transsections, callosotomy), and transcranial stimulating methods are practiced. As a result, it is possible to achieve a complete cessation of attacks within a year or a significant reduction in their frequency with the achievement of adequate control.
Some symptomatic seizures are also treated surgically. In case of traumatic brain injuries and strokes, early intervention is necessary, aimed at evacuation of intracranial hematoma and decompression of cerebral structures. Abscesses and brain tumors also need to be removed. Intravascular recanalization operations - intraarterial thrombolysis, thrombectomy, angioplasty with stenting - are designed to restore blood flow in ischemic areas of brain tissue.
Frequency of epileptic seizures
The frequency of attacks can vary from once every 2-3 months to single or multiple daily. A seizure can be triggered by sleep disturbances, stress, excessive alcohol consumption, long stays in a stuffy room, sudden flashes of light, etc. At the moment, the specific factor influencing the increase in the frequency of seizures is not yet known.
Expert opinion
Author: Daria Olegovna Gromova
Neurologist
Epilepsy has been considered one of the most dangerous and common diseases for many years. According to WHO statistics, 4-10 people per 1000 population suffer from seizures. Doctors note an annual increase in cases of onset of epilepsy. Thanks to numerous clinical studies, it has been proven that the disease is registered 2-3 times more often in countries with low and medium levels of development. This is due to the presence of a greater number of provoking factors, such as infections and a high level of injuries. According to statistics, 80% of patients with epilepsy live in such conditions.
The exact causes of seizures are still unknown. Doctors distinguish several types of seizures, as well as the factors that cause them. When selecting therapy, neurologists and epileptologists at the Yusupov Hospital take into account all the data. If you follow the rules of prevention and take anticonvulsants, about 70% of patients can live for a long time without seizures. An individual epilepsy treatment plan is developed for each patient at the Yusupov Hospital. The drugs used meet European quality and safety standards. In addition, patients are provided with personalized preventive recommendations that minimize the risk of epilepsy relapse.
SEIZURES AND CONVIVUS SYNDROME IN CHILDREN
Seizures are the most common manifestation of central nervous system damage in childhood. It is believed that up to 2/3 of seizures in children occur in the first 3 years of life. The stages of development (maturation) of the central nervous system have a pronounced influence on the electroencephalographic and clinical features of the manifestations of seizures in children. If a newborn child who has suffered hypoxic-ischemic damage to the nervous system may initially manifest multifocal clonic convulsions, then by the age of six months they can transform into infantile spasms (with a characteristic EEG pattern similar to the so-called hypsarrhythmia), and by 2 years they can acquire the appearance of myoclonic ones. seizures, atypical absence seizures and/or generalized tonic-clonic seizures.
Such an evolution of convulsive syndrome is not uncommon in the practice of pediatric neurologists. In this regard, it is advisable to separately consider seizures in children at different periods of life:
* newborns;
* 1st year;
* early age;
* later life.
Without being able to touch upon all aspects of the diversity of manifestations of convulsive syndromes in childhood in the format of one work, as well as reflect the features of therapy in various clinical situations, below we will present their main age-related differences. When describing therapeutic approaches, we will first touch on some features of the treatment of paroxysmal seizures in children of the neonatal period of development, infancy and early childhood.
Etiology and pathogenesis
A number of numerous endogenous and exogenous factors can lead to the occurrence of seizures. These include:
* infections;
* intoxication;
* injuries;
* diseases of the central nervous system;
* metabolic defects;
* genetic predisposition, etc.
Seizures are a typical manifestation of epilepsy, but their presence does not always indicate this disease. Therefore, in this article we will focus primarily on the description of seizures of both epileptic and non-epileptic origin. The cause of the development of convulsive conditions can be hypoxia, microcirculation disorders, as well as hemorrhagic manifestations.
The pathogenesis of convulsive conditions is determined by their etiology (which, as mentioned above, is multifactorial), therefore it is quite complex and ambiguous in children of any age. In some cases, a whole complex of pathophysiological mechanisms is involved in the pathogenesis of seizures.
The exact pathogenetic mechanisms of seizures are unknown. Nevertheless, a number of neurophysiological factors are important in their development. Firstly, the initiation of a convulsive attack requires the presence of a group of neurons capable of generating a pronounced explosive discharge, as well as a GABAergic inhibitory system. The transmission of convulsive discharge depends on excitotor (excitatory) glutamatergic synapses. There is evidence that excitotor amino acid neurotransmitters (glutamate, aspartate) cause irritation of neurons by acting on specific cellular receptors. Seizures may originate from regions of neuronal death, and these regions themselves may contribute to the development of new hyperexcitable synapses that cause paroxysms. In particular, lesions in the temporal lobes (slow-growing gliomas, hamartomas, gliosis and arteriovenous malformations) cause seizure activity, and when the abnormal tissue is surgically removed, the seizures stop.
Currently, the hypothesis about the existence of the so-called kindling phenomenon (from the English “kindling” - fire) and its role in the formation (or stabilization) of a focus of pathological activity with constant stimulation of the dopaminergic centers of the limbic system under the influence of psychoactive substances and other factors is also being considered.
It is hypothesized that recurrent seizure activity involving the temporal lobes of the brain may produce seizures in the contralateral intact temporal lobe via stimulus transmission through the corpus callosum.
The substantia nigra plays an integral role in the development of generalized seizures. It has been suggested that functional immaturity of the substantia nigra may play a significant role in the increased susceptibility to seizures of the immature brain. In addition, neurons of GABA-sensitive substrates of the substantia nigra can prevent seizure activity by modulating and regulating the dissemination, but not the initiation of convulsive paroxysms.
Seizures in newborns
According to their manifestations in the neonatal period, convulsions in newborns are as follows:
* small (or minimal) convulsions (convulsive activity is noted in the absence of tonic and clonic movements of the limbs: apnea (dyspnea), tonic rolling of the eyes, twitching and trembling of the eyelids, drooling, convulsive sucking and “chewing”);
* multifocal (multifocal) clonic seizures (migratory);
* focal (focal) clonic;
* tonic;
* myoclonic.
In neonatal seizures, importance is given to the actual age of the child. Thus, on the 1st-2nd day of life, seizures are more often caused by perinatal disorders (birth trauma, hypoxia, intracranial hemorrhage). Less common conditions in the first 48 hours of life are: drug withdrawal syndrome, so-called pyridoxine dependence, inborn errors of metabolism. Sometimes there is an accidental injection into the baby's scalp of an anesthetic given to his mother during labor to relieve pain during labor.
On the 3rd day of life, the most common cause of seizures in newborns is hypoglycemia, and on the 4th day and beyond (during the neonatal period) - infections. More often we are talking about generalized types of infections, such as sepsis and/or meningitis, as well as congenital infections such as rubella, toxoplasmosis, cytomegaly, herpes, etc. Other causes of seizures at this age include hypocalcemia, hypo- or hypernatremia, and hypomagnesemia. Kernicterus and tetanus are much less common, as are congenital developmental disorders (for example, arteriovenous fistula, etc.) or porencephaly.
Convulsions in perinatal disorders are a consequence of anoxia with cerebral edema due to birth trauma. Premature newborns are more likely to have microbleeds, while full-term newborns are more likely to have massive ones. With microhemorrhages (intracranial), convulsions in the form of tonic spasms (preceded by clonic twitching) develop on the 1st day of life. With massive hemorrhages, they are usually recorded between the 2nd and 7th days. Such convulsions are most often unilateral.
The first manifestations of hypocalcemia can be observed from the 1st day of life due to the following reasons: feeding with poorly adapted formulas with excess phosphorus content, long-term use of phenobarbital, etc. In addition to seizures, manifestations of hypocalcemia may include fluttering, laryngospasm, tremor, muscle twitching, carpopedal spasm. Between attacks, the condition of the newborns is not impaired. Convulsions are stopped by intravenous administration of 5-10 ml of 10% calcium gluconate solution.
Hypoglycemic convulsions are observed in respiratory distress syndrome, kernicterus, glycogenosis, adrenal hyperplasia, intrauterine growth retardation, Beckwith-Wiedemann syndrome, and also at birth from mothers with diabetes mellitus. In addition to seizures, hypoglycemia in newborns is expressed in tremor, cyanosis, muscle twitching (myoclonus), and apnea attacks.
Generalized convulsions and neuroinfections are observed in newborns with purulent meningitis, sepsis, intracranial hemorrhages (a consequence of disseminated intravascular coagulation syndrome, cerebral ischemia-hypoxia, cardiovascular collapse, disturbances in thermoregulation, electrolyte balance, hypoglycemia, etc.).
Tetanus convulsions are rare these days. They appear on the 5-6th day after birth, when the umbilical cord is cut off without following the rules of antiseptics or when the umbilical wound is infected and are manifested by generalized spasticity (spontaneous or induced by external stimuli), as well as difficulty sucking, tension in the facial muscles, the so-called sardonic smile.
Convulsions in encephalitis are the result of intrauterine infection of the fetus with the rubella virus, cytomegaly or the causative agent of toxoplasmosis, and develop immediately after birth. If the infectious process has died down before the onset of childbirth, convulsions may begin much later (in the 1st year of life). With intrauterine infection with the herpes virus, convulsive manifestations of encephalitis occur by the end of the 1st week of life.
Pyridoxine-dependent seizures develop in newborns whose mothers received pyridoxine for a long time during pregnancy, as well as with a hereditary metabolic defect (with an increased need for vitamin B6). Between attacks, children are restless and react with muscle twitching to external irritations. These seizures do not respond to conventional anticonvulsant treatment, but high-dose pyridoxine (25 mg/kg/day) quickly normalizes the condition.
Convulsions during drug withdrawal syndrome can develop in newborns of drug-addicted mothers who use hard drugs (morphine, heroin, etc.). In addition to seizures, hypersalivation and increased excitability are characteristic.
Convulsions due to electrolyte disturbances, hypo- and hypernatremia due to dehydration (or its improper correction) cause manifest convulsions with persistent neurological disorders. Hypomagnesemia can be suspected if hypocalcemic seizures do not respond to calcium therapy.
Metabolic disorders. Their presence should be suspected if seizures do not respond to standard anticonvulsant therapy.
With galactosemia, convulsions appear after feeding. Additional signs are icteric skin and hepatosplenomegaly.
Convulsions with fructose intolerance occur against the background of hypoglycemia (up to coma) immediately after consuming mixtures containing sucrose or cane sugar, or in older children - fruit and vegetable juices and purees.
Congenital disorders of amino acid metabolism, accompanied (or may be accompanied) by seizures, are extremely numerous. Their main varieties are listed below.
Maple syrup urine disease (valinoleucinuria) is clinically characterized by hypoglycemic seizures associated with poor sucking, persistent metabolic acidosis, progressive neurological impairment, and maple syrup odor in the urine.
Non-ketotic hyperglycinemia is a consequence of insufficient breakdown of glycine. It is more common in ketotic form. Its manifestations can be expected 48 hours after birth in the form of hiccups and/or regurgitation, decreased response to external stimuli, and myoclonic jerks. Multifocal seizures are not responsive to traditional anticonvulsants. A replacement blood transfusion may improve the condition in the short term. The outcome is fatal; among survivors there is mental retardation and profound neurological deficit.
Ketotic hyperglycinemia (varieties: propionic and methylmalonic) are the most common disorders of amino acid metabolism. They occur with clinical severity from the 1st week of life. Their manifestations: metabolic acidosis, vomiting, dehydration, convulsions due to metabolic changes against the background of existing enzyme deficiency. The clinical effect is achieved with the use of adequate diet therapy. In case of methylmalonic hyperglycinemia, the administration of vitamin B12 (i.m.) ensures normal development of children.
Other organic acidemias that may be accompanied by seizures include:
* isovaleric;
* beta-methylcrotonylglycinuria;
* 3-hydroxy-2-methylglutaric aciduria;
* multiple carboxylase deficiency (neonatal form of the disease);
* adenylsuccinate lyase deficiency (usually after the neonatal period);
* short-chain acyl-CoA dehydrogenase deficiency;
* glutaric aciduria type 2.
A number of genetic diseases (defects) are also often accompanied by seizures. Pyridoxine-dependent seizures have already been discussed above.
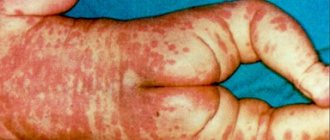
Convulsions in Bloch-Sulzberger syndrome (incontinentia pigmenti), a disease of the central nervous system, ectoderm with damage to the skin, eyes, and (subsequently) teeth. Appear from the 2-3rd day of life (usually unilateral). The disease is 20 times more common in girls. Skin rashes in the form of an erythematous/vesicular rash are characteristic. Seizures can be controlled with standard anticonvulsants.
Convulsions in Smith-Lemli-Opitz syndrome (autosomal recessive) appear from the 3rd day of life due to perinatal hypoxia and structural disorders of the hemispheres and cerebellum. They are accompanied by lethargy, a generalized decrease in muscle tone, and difficulty breathing. Phenotypically: convexity of the nostrils, ptosis, cryptorchidism, hypospadias, syndactyly of the 2nd and 3rd toes. About 20% of patients do not survive beyond 12 months.
Congenital disorders of the central nervous system are often accompanied by seizures. Among them:
* arteriovenous fistula;
* congenital hydrocephalus;
* porencephaly;
* microgyria;
* agenesis of the corpus callosum (corpus callosum);
* hydrocephalus and other types of brain dysgenesis.
Benign “familial” neonatal seizures. In this condition, there is a family history indicating the presence of seizures in the neonatal period in other family members. They are inherited in an autosomal dominant manner and appear on the 3rd day of life or later. Seizures resolve spontaneously (without treatment) after 1-3 weeks. No inborn errors of metabolism are detected.
Treatment.
The newborn should be provided with maximum rest. According to indications, symptomatic treatment is carried out in the form of dehydration and rehydration therapy; measures aimed at normalizing microcirculation, as well as improving tissue metabolism, etc.
Anticonvulsants used in the early neonatal period include phenobarbital (0.001-0.005 g/kg), seduxen (diazepam) (1 mg/kg IV or IM), GHB (up to 50 mg/kg). Subsequently, newborns are prescribed phenobarbital (0.001-0.005 g/kg in 2-3 doses).
If treatment is insufficiently effective, an anticonvulsant mixture can be used, including phenobarbital, diphenine (0.003-0.005 g), papaverine (0.001-0.005 g), borax (0.03-0.05 g), calcium gluconate (0.01-0.05 d), prescribed 2-3 times a day.
For minor and truncal convulsions, the above mixture is alternated with radedorm (0.00012 g 1-2 times a day). If there is resistance to treatment, they resort to the prescription of valproate and/or clonazepam.
Seizures in children of the first year of life
In children older than 1 month, the following types of seizures are more common:
1. Primary generalized (tonic-clonic, grand mal type). They are characterized by a tonic phase lasting less than 1 minute, with the eyes rolling upward. At the same time, gas exchange decreases (due to tonic contraction of the respiratory muscles), which is accompanied by cyanosis. The clonic phase of seizures follows the tonic phase, expressed in clonic twitching of the limbs (usually 1-5 minutes); This improves gas exchange. May be observed: hypersalivation, tachycardia, metabolic/respiratory acidosis. The postictal state often lasts less than 1 hour.
2. Focal motor seizures (partial, with simple symptoms). They are characterized by their occurrence in one of the upper limbs or in the facial area. Such convulsions lead to deviation of the head and diversion of the eyes towards the hemisphere opposite to the localization of the convulsive focus. Focal seizures can begin in a limited area, without loss of consciousness, or, conversely, generalize and resemble secondary generalized tonic-clonic seizures. Indications of the focus are Todd's palsy or abduction of the head and eyes towards the affected hemisphere. They appear after an attack of these seizures.
3. Temporal or psychomotor seizures (partial, with complex symptoms). In approximately 50% of cases they are preceded by an aura. They can imitate other types of seizures, be focal, motor, grand mal, or with frozen gaze. Sometimes they look more complex: with stereotypical automatisms (running - in those who have begun to walk, laughter, licking lips, unusual movements of the hands, facial muscles, etc.).
4. Primary generalized absence seizures (petit mal type). Rarely develop in the first year of life (more typical for children over 3 years of age).
5. Infantile spasms (with hypsarrhythmia - according to EEG data). They most often appear in the 1st year of life and are characterized by pronounced myoclonic (salaam) spasms. Infantile spasms (West syndrome) can develop due to the presence of various neurological pathologies or without any obvious previous disorders. With infantile spasms, psychomotor development slows down, and in the future there is a high probability of severe developmental delay.
6. Mixed generalized seizures (small motor or atypical petit mal). This group of seizure disorders is typical of Lennox-Gastaut syndrome, which is characterized by frequent, poorly controlled seizures, including atonic, myoclonic, tonic and clonic, which are accompanied by an EEG pattern with atypical spikes and waves (less than three spike-waves in 1 s), multifocal spikes and polyspikes. The age of patients often exceeds 18 months, but this syndrome can develop in the 1st year of life following infantile spasms (transformation from West syndrome). Children often have severe developmental delays.
Febrile seizures (FS). They are observed in children starting from 3 months of age, with an increase in body temperature (>38.0°C). As a rule, they are primarily generalized tonic-clonic, although they can be tonic, atonic or clonic.
FS are considered simple if they were noted once, lasted no more than 15 minutes and were not focal. Complex FS are characterized by repeated occurrence, duration, and focality. All patients under 12 months of age require lumbar puncture and metabolic screening.
Risk factors for the development of epilepsy in FS include:
— indications of the presence of neurological disorders or psychomotor development disorders;
- a family history of afebrile seizures;
- complex nature of febrile seizures.
In the absence or presence of only one risk factor, the likelihood of developing afebrile seizures is only 2%. If two or more risk factors are present, the likelihood of epilepsy increases to 6-10%.
Treatment. For primary generalized seizures (grand mal), phenobarbital, phenytoin, and carbamazepine are usually used. As an alternative, valproate or acetazolamide can be used in some cases.
Partial simple seizures (focal). Phenobarbital, phenytoin, carbamazepine, and primidone are used. If necessary, other therapeutic agents can be used (valproic acid preparations.
Partial complex seizures (temporal lobe epilepsy). The priority prescription of drugs carbamazepine, phenytoin and primidone is provided. An alternative to them are phenobarbital drugs, valproate and acetazolamide (as well as methsuximide).
Primary generalized seizures (petit mal, absence seizures). The main antiepileptic drugs AEDs in the described clinical situation are ethosuximide, valproates, methsuximide. Other agents: acetazolamide, clonazepam, phenobarbital.
Treatment of infantile spasms suggests effectiveness from the use of a synthetic analogue of ACTH, valproate, and clonazepam. Other types of therapy include the use of phenytoin, phenobarbital, and acetazolamide. If possible, a ketogenic diet (KD) can be used.
Febrile seizures. The advisability of prescribing anticonvulsants to children for FS has continued to be extremely controversial for many years. Nevertheless, when deciding in favor of preventive therapy using AEDs, phenobarbital drugs are most often used, and valproates are used less often.
Mixed generalized seizures. Main AEDs: phenobarbital, valproate, clonazepam. As alternatives, acetazolamide, diazepam, ethosuximide, phenytoin, methsuximide, carbamazepine, as well as tranxene, etc. can be used.
Dosing of main anticonvulsants (in the 1st year of life)
- diazepam - 0.1-0.3 mg/kg up to a maximum dose of 5 mg intravenously slowly;
— phenytoin — 5 mg/kg/day (2 times, per os);
— phenobarbital — 3-5 mg/kg/day (2-3 times, per os);
- primidone - 5-25 mg/kg/day (1-2 times);
— carbamazepine — 15-30 mg/kg/day (2-3 times, per os);
- ethosuximide - 20-30 mg/kg/day (2 times);
- methsuximide - initial dose 5-10 mg/kg, maintenance dose - 20 mg/kg (2 times, per os);
- valproate - 25-60 mg/kg/day (2-3 times, per os);
- clonazepam - 0.02-0.2 mg/kg/day (2-3 times, per os);
— paraldehyde — 300 mg (0.3 ml/kg, rectally);
- acetazolamide (diacarb) - initial dose 5 mg/kg, maintenance dose - 10-20 mg/kg (per os).
Features of the treatment of seizures in children of the first year of life (including newborns). You should always take into account the fact that phenytoin (diphenin) is absorbed with low efficiency in the neonatal period, although subsequently its utilization gradually improves.
Valproic acid preparations, when administered simultaneously, interact with phenytoin and phenobarbital, leading to an increase in their levels in the blood. With long-term administration of valproate, it is necessary to monitor the indicators of a general blood test, as well as examine the level of liver enzymes (ALT, AST) initially (in the first months of therapy) with a frequency of once every 2 weeks, then monthly (for 3 months), and subsequently - 1 once every 3-6 months.
Almost all currently known anticonvulsants, to a greater or lesser extent, have a so-called rickets effect, leading to the appearance or aggravation of manifestations of vitamin D deficiency rickets. In this regard, children of the first year of life receiving treatment with anticonvulsants should be provided with an adequate supply of vitamin D (D2 - ergocalciferol, or D3 - cholecalciferol), as well as calcium supplements.
Convulsions in young children. Clinical manifestations of West and Lennox-Gastaut syndromes have already been described above. As already indicated, they can also be observed in the first 12 months of life, although they are more typical for young children.
Secondary generalized seizures. These include epilepsy with manifestations in the form of simple and/or complex partial seizures with secondary generalization, as well as simple partial seizures turning into complex partial seizures with subsequent secondary generalization.
Febrile seizures in young children occur with no less frequency than in the 1st year of life. The principles of approaches to their diagnosis and therapeutic tactics do not differ from those in children of the first year of life.
Seizures in children over 3 years of age
Primary generalized absence seizures are not uncommon among children in this age group. Their identification and adequate treatment is entirely within the competence of pediatric neurologists and epileptologists. Pediatricians and representatives of other pediatric specialties should not ignore identified episodes of short-term “disconnection” of children (with a lack of response to treatment) or complaints from parents about what non-specialists more often call “ideas.”
Juvenile myoclonus epilepsy is a subtype of idiopathic generalized disease with manifestations of impulsive petit mal attacks. The appearance of seizures is typical after 8 years of age. A distinctive feature is the presence of myoclonus, the severity of which varies from minimal (regarded as “clumsiness”) to periodic falls, with no disturbances of consciousness noted. However, most of these patients have sporadic tonic-clonic seizures, and absence seizures occur in approximately one third of children with this type of epilepsy.
Catamenial epilepsies. Without dwelling in detail on this group of chronic paroxysmal conditions associated with the menstrual cycle, we note that they can be cited as one of the examples of age-dependent convulsive conditions in relation to female patients who have reached puberty.
Febrile seizures can also occur in children over 3 years of age (in preschool age), although during this period of life they occur with significantly less frequency. The presence of episodes of afebrile seizures (without fever) in this pathology indicates the development of symptomatic epilepsy, which must be treated in accordance with the principles formulated by the International League Against Epilepsy (ILAE).
Benign focal epilepsies of childhood.
Among the pathological conditions that make up the content of this concept, one should consider rolandic epilepsy (central-temporal) with characteristic changes in the EEG, which is not uncommon for children aged 4 to 13 years; as well as Gastaut and Panoyotopoulos syndromes. The prognosis for rolandic epilepsy is favorable, since seizures usually disappear spontaneously with the onset of puberty. Gastaut syndrome is another type of idiopathic localization-related epilepsy in children, in which (in addition to EEG changes) visual symptoms are usually noted at the time of the attack: amblyopia and/or hallucinations. With this type of epilepsy, the prognosis is also quite favorable - by the age of 18, in most children, clinical and electroencephalographic signs of the disease disappear.
Panoyotopoulos syndrome can occur in patients older than 3 years (as well as in young children); its other name is “benign infantile seizures with occipital adhesions with an early onset.” The latter form of the disease is usually diagnosed between 4 and 5 years of age and is more common than the Gastaut variant. Its characteristic symptoms are pallor, sweating, vomiting in combination with rolling eyes and deviation of the head, as well as changes in consciousness of varying severity with partial or secondary generalized convulsions. Most seizures begin at night. Visual impairment (transient) has been reported. In 10% of patients with the described variant of epilepsy, rolandic epilepsy gradually develops.
There is also Janz syndrome - juvenile myoclonus epilepsy, a subtype of idiopathic generalized epilepsy, also called impulsive petit mal and usually clinically manifested after 8 years of age. Symptoms of the disease include morning myoclonic twitches, generalized tonic-clonic convulsions immediately after waking up, etc.
It is not possible to describe all types of convulsive reactions in children of this age group due to their large number, multifactorial nature and diversity of clinical manifestations.
The main types of paroxysmal disorders of non-epileptic origin in childhood
These include, for example, psychogenic convulsions, syncope, migraines, apnea, sleep disorders, tics, shuddering attacks, gastroesophageal reflux, cardiac conduction disorders, etc.
It is the conditions listed above that should be remembered when making a differential diagnosis between epileptic and non-epileptic paroxysmal conditions in children over 3 years of age. For example, psychogenic seizures are rarely observed in children before the age of 6 years.
**
In general, when examining a child with a seizure disorder, it is recommended to try to resolve the following most important questions first:
1. Are the observed attacks convulsions?
2. If yes, what kind of cramps are they?
3. What is the risk of relapse (epilepsy)?
4. If present, what epileptic syndrome should the observed seizures be classified as?
5. If the seizures are related to symptomatic epilepsy, what is their etiology?
Only such an approach allows us to timely and correctly establish the cause of the presence of convulsive activity in children of different ages, based on objective clinical, laboratory and instrumental (EEG, CT, MRI, etc.) research methods.
It is quite natural that when describing the characteristics of convulsive syndromes in children of the 4 age periods we have identified (neonatal, infant, early, and also over 3 years of age), we have made a number of conventions, since paroxysmal states characteristic of school-age children can in some cases observed in patients under 3 years of age, and vice versa.
It is known that in most cases, convulsive episodes in children are isolated (single) and do not require further treatment. Recurrent seizures, most often related to various types of epilepsy, require carefully selected and long-term therapy with anticonvulsants under the supervision of a pediatric neurologist.
Vladimir STUDENIKIN, professor.
Vladimir SHELKOVSKY, candidate of medical sciences.
Svetlana BALKANSKAYA, candidate of medical sciences.
Research Institute of Pediatrics, Scientific Center for Children's Health, Russian Academy of Medical Sciences.
Precursors of epileptic seizures
The first harbinger of epileptic seizures is an aura. It is individual for each patient. Thanks to the constant warning signs, patients can warn others about the onset of an attack or independently move to a safe place.
There are the following types of aura that precede the onset of an epileptic attack:
- Hallucinations;
- Sharp contraction of the muscles of the upper or lower extremities;
- Repeating the same movements;
- Burning, crawling or tingling sensation in various parts of the body;
- Sharp deterioration in mood.
The duration of the aura is several seconds. During this time, patients do not lose consciousness.
Types of seizures in epilepsy
Depending on the cause of occurrence, the following types of epileptic seizures are distinguished:
- Idiopathic – occurring in the presence of epilepsy in close relatives;
- Symptomatic – occur after a traumatic brain injury, infectious or tumor lesion of the brain substance;
- Cryptogenic – the causes of occurrence cannot be determined.
The external manifestations of a convulsive syndrome are determined by its type. If the pathological focus is localized in one hemisphere of the brain, simple or complex seizures occur.
Make an appointment
Simple partial seizures
Against the background of simple convulsions, the patient does not always lose consciousness. Clinical symptoms depend on the location of the pathological focus in the cerebral cortex. The average duration of simple partial seizures is two minutes.
Neurologists identify the following main signs of the disease:
- Emotional lability;
- Hallucinations of various types;
- Twitching in various parts of the body;
- Cardiopalmus;
- Feeling of nausea;
- Frequent feelings of deja vu;
- Difficulty understanding and reproducing words.
Complex partial seizures
The duration of complex partial seizures is one or two minutes. An aura appears before the attack begins. There is uncontrollable crying and screaming, repetition of words, and performance of certain movements. At the end of the seizure, patients are not oriented in space and time. A simple partial seizure of epilepsy can develop into a complex seizure.
Generalized seizures
Generalized seizures occur against the background of total brain damage. They are as follows:
- Tonic;
- Clonic;
- Tonic-clonic;
- Atonic;
- Myoclonic.
With tonic spasms, unconscious muscle contractions occur. Patients are bothered by severe pain in the muscles of the back, upper and lower extremities. Tonic convulsions rarely lead to fainting. The attack lasts no more than twenty seconds. Tonic seizures can occur during sleep.
Patients with epilepsy are less likely to experience clonic seizures. They manifest themselves as uncontrolled paroxysmal muscle contractions. During convulsions, foam is released from the patient's mouth. He loses consciousness. Paralysis may develop. Clonic seizures occur due to severe stress, traumatic brain injury, cerebrovascular accident, or brain tumor. During an attack, short-term muscle tension is replaced by relaxation. The attacks quickly follow each other.
The most typical and characteristic of an epileptic attack are tonic-clonic convulsions. Their duration varies from 1 to 3 minutes. If tonic-clonic seizures persist for a longer period of time, calling an ambulance is recommended. Neurologists distinguish tonic and convulsive phases in the course of an attack. In the tonic phase, the patient loses balance and consciousness, in the convulsive phase, involuntary muscle contractions occur. After the attack is over, patients do not remember what happened.
Tonic-clonic seizures may also be accompanied by the following symptoms:
- Increased salivation;
- Sweating;
- Involuntary tongue biting;
- Injury as a result of uncontrolled actions;
- Involuntary urination or defecation;
- Blueness of the skin.
Atonic seizures occur after a traumatic brain injury, stroke, infectious inflammatory processes, or in the presence of a brain tumor. During an attack, the patient loses consciousness for a while and falls. In some cases, convulsions can be expressed by twitching of the head. The attack lasts about 15 seconds. At the end of it, the patient does not remember what happened.
Myoclonic seizures are characterized by rapid jerking of various parts of the body. The attack resembles jumping inside the body. Most often, muscle contractions occur in the upper half of the body, the area of the upper and lower extremities. Myoclonic spasms can occur when falling asleep or waking up. A symptom of an attack may be hiccups. The duration of the attack is several seconds. During myoclonic seizures, patients do not lose consciousness.
Why do seizures occur?
Causes of tonic seizures
Prolonged muscle tension occurs against the background of excessive excitability of cerebral structures, in conditions of disruption of the cortical regulation of segmental functions. Very often, neurons are negatively affected by toxic, metabolic factors, and endocrine and metabolic disorders. The causes of tonic seizures are the following conditions:
- Infections
: tetanus, rabies, febrile syndrome. - Electrolyte disturbances
: hypocalcemia, hyperkalemia, hypomagnesemia. - Endocrine disorders
: hyper- and hypoglycemia, hyperinsulinism. - Hereditary metabolic diseases
: amino acid (leucinosis, phenylketonuria), carbohydrate (glycogenosis, galactosemia), lipid (Gaucher disease, Norman-Wood disease). - Cardiovascular pathology
: complete atrioventricular block, acute hypotension. - Renal and liver failure
: uremia, bilirubin encephalopathy. - Psychogenic disorders
: hyperventilation syndrome, hysteria. - Epileptic syndromes of childhood
: Lennox-Gastaut encephalopathy, Otahara encephalopathy, infantile spasms. - Intoxication
: alcohol, carbon monoxide poisoning, strychnine. - Overdose of drugs
: morphine, antipsychotics. - The effect of physical factors
: severe overheating or hypothermia, electrical injuries, the influence of radiation.
Sometimes painful spasms are of a professional nature, occurring during prolonged muscle tension in stenographers, musicians, and milkmaids. Leg cramps are common among athletes and people whose work involves standing for long periods of time. They are often observed during pregnancy, with vascular pathology of the lower extremities - varicose veins, obliterating atherosclerosis, endarteritis.
Causes of clonic seizures
Pathological impulses that provoke short-term spasms of skeletal muscles are formed in higher cortical centers, the extrapyramidal system or peripheral motor neurons. Some clonic seizures develop due to focal damage to the brain stem or spinal cord due to tumors and strokes. Other causes of such seizures include:
- Focal epileptic seizures
. - Children's infections
: measles, chickenpox, influenza, parainfluenza. - Severe myoclonic epilepsy of infancy (Dravet syndrome)
. - Diffuse damage to gray matter
: Creutzfeldt-Jakob disease, subacute sclerosing panencephalitis. - Neurodegenerative conditions
: Tay-Sachs, Alpers diseases. - Non-progressive encephalopathies
: with Down syndrome, tuberous sclerosis. - Neonatal paroxysms
: “fifth day seizures”, benign familial epilepsy. - Poisoning
: drugs (piperazine, ergotamine), chemicals (formaldehyde, arsenic).
Causes of tonic-clonic seizures
Often in the clinical picture there is a change from tonic convulsive contractions to clonic ones. Generalized mixed seizures are a typical sign of epilepsy and its severe complication - epistatus. The occurrence of paroxysmal electrical activity of brain neurons is caused by a wide range of damaging factors:
- Cerebral pathology
: vascular disorders (CVA, arteriovenous malformations, aneurysms), traumatic brain injuries, tumors. - Infectious diseases
: polio, cholera, neuroinfections (meningitis, encephalitis, abscesses). - Arterial hypertension
: renal eclampsia, convulsive form of hypertensive crisis. - Toxicoses of pregnancy
: eclampsia. - Hereditary pathology
: leukodystrophy. - Intoxication
: nicotinic, narcotic (amphetamine, cocaine), poisoning (organophosphorus compounds, oxalic acid, lead). - Overdose of medications
: caffeine, atropine, amitriptyline, etc.
Nocturnal epilepsy
In one third of patients, epilepsy attacks occur at night. Pathological signs may appear when falling asleep, during sleep, or during awakening. Nocturnal epilepsy occurs under the influence of the following factors:
- Hereditary predisposition;
- Suffered traumatic brain injury;
- Excessive consumption of alcoholic beverages;
- Sleep disorders;
- Prolonged psycho-emotional stress.
The duration of a nocturnal epilepsy attack varies from a few seconds to five minutes. Most patients do not remember the seizures that occurred. Some people clearly describe the sensations they experience. An epileptic attack that occurs during a dream is accompanied by the following manifestations:
- A sharp, causeless awakening;
- Feeling of nausea, which may result in vomiting;
- Severe headache;
- Tremor;
- Pronunciation of unusual sounds;
- Speech impairment.
During a nocturnal epilepsy attack, patients may perform rash actions. They get down on all fours or pretend to ride a bicycle. You can suspect the presence of a nocturnal attack based on the following indirect attacks:
- Tongue bite:
- Traces of blood on the pillow after waking up;
- Bruises and abrasions on the body;
- Painful muscle syndrome;
- Wet bed due to loss of urinary control;
- Uncontrolled urination;
- Waking up in an unusual place (on the carpet, on the floor).
These symptoms are individual for each patient. They appear with one degree or another. Therefore, neurologists believe that nocturnal epilepsy attacks are very difficult to diagnose.
Rolandic epilepsy
Epilepsy of this type is focal and genetically determined. It manifests itself in rare attacks at night, they affect one half of the face with the tongue and pharynx. The Rolandic type is characterized by partial epileptic seizures without loss of consciousness.
The first sign of onset is tingling or numbness on one side of the face, lips, gums, or tongue. Afterwards motor paroxysms develop.
Make an appointment
Local clonic seizures
The reasons for periodic twitching of a particular muscle may be the most unexpected. For example, strong emotional experiences, stress, due to which excitation in our body begins to prevail over inhibition, various neuroses arise.
Or heredity, due to which we inherited easily excitable muscles. If your grandmother or mother often complained of local convulsions, this is from them. An unhealthy diet lacking essential micronutrients (crash diet) can also cause these symptoms. On the one hand, they do not cause serious concern, but they are not easy to get rid of.
What to do? The problem of muscle fasciculations becomes significant for the doctor and the patient when twitching occurs too often and really interferes with life. In this case, you should contact a neurologist. The course of treatment may take some time and include taking vitamins and minerals, medications that affect the nervous system (including sleeping pills and antidepressants), physiotherapy and massage.
Alcoholic epilepsy
This type of epilepsy develops in patients who abuse alcohol. Seizures occur due to irreversible pathological processes in the cerebral cortex. Epilepsy attacks caused by alcohol intoxication most often occur in patients suffering from the following concomitant diseases:
- Atherosclerosis;
- Consequences of traumatic brain injury;
- Brain tumors;
- Residual effects of previously suffered infectious and inflammatory diseases of the brain.
The cause of the disease may be aggravated heredity. The symptoms of alcoholic epilepsy have some peculiarities. The disease does not necessarily begin with a convulsive syndrome. Initially, the following pathological signs appear:
- Increased salivation;
- Marked weakness throughout the body;
- Paleness of the skin;
- Blueness of lips;
- Dizziness;
- Strong headache;
- Loss of consciousness;
- Nausea, vomiting;
- Uncontrolled urination;
- A spasm of the vocal cords that causes a person to emit a high-pitched scream.
An attack of alcoholic epilepsy can result in respiratory arrest and death.
Epilepsy of newborns
Up to one year, a baby may experience the following types of epilepsy seizures: small, large and nocturnal. During a minor attack, the child throws back his head and freezes in one position. His gaze is directed to one point. The baby does not respond to stroking and sound and rolls his eyes. His body temperature may rise.
A major seizure of epilepsy is manifested by the fact that the child stretches out, bends his legs and assumes a fetal position. Convulsions, loss of consciousness and respiratory arrest occur.
During a night attack, the baby suddenly awakens and screams. His face changes. After an attack, the child cannot fall asleep for a long time. Children suffering from epilepsy may lag behind their peers in development, their memory is impaired, and mental health problems occur.
Pediatric epilepsy
Epilepsy in children is manifested by the following symptoms:
- Tonic-clonic seizures;
- Absences (minor seizures);
- Myoclonic convulsions with and without disturbance of consciousness.
This condition occurs due to the immaturity of the child’s brain, when processes of excitation, burdened heredity or organic brain damage predominate. Initially, warning signs of a seizure occur: headache, irritability, and a feeling of fear. In the generalized form of the disease, the child groans, screams and loses consciousness. All his muscles tense, his jaw clenches, breathing stops, his pupils dilate, his face becomes cyanotic.
The child's legs stretch and his arms bend at the elbows. After the completion of the tonic phase of the seizure, clonic convulsions occur. The child's breathing becomes noisy and foam comes out of the mouth. He bites his tongue. Involuntary urination and defecation occur. Minor seizures do not last long.
Absence epilepsy
This is idiopathic generalized epilepsy that occurs in preschool children. Characteristic symptoms: short-term loss of consciousness during the daytime, less often at night. This does not affect neurological status or intelligence in any way.
The attack begins suddenly, the child seems to freeze and does not react to any stimuli, his gaze is directed to the side. This condition lasts no longer than 15 seconds and is rare in isolated form. More often it is supplemented by throwing the head back, rolling the eyes, and possibly repeating some actions: stroking hands, licking lips, repeating words or sounds. The child does not remember what he did.
If severe fatigue, drowsiness are added to the symptoms, and the attack lasts for a long time, then this indicates an unfavorable course of the disease.
Chapter 2.
What are the types of seizures? How they develop and proceed.
You need to have this booklet-memo, since the correct diagnosis and treatment of attacks is primarily determined by how accurately and in detail you can tell the doctor about the attack. Reading the booklet will help you create a written description of the attack, with which you can go to the doctor and receive the correct treatment.
The first page of this booklet will not be used by you to describe seizures - it is just a summary of the main types of seizures. I put it here so that you understand that seizures come in different varieties, and that your description of seizures is of great importance for diagnosis. Do not try to make a diagnosis yourself based on these brief descriptions. The actual diagnosis of seizure type is much more complex.
The most common seizures in adults and children are manifested by various convulsions - in the form of twitching or muscle tension in the limbs and (or) other parts of the body. Convulsions in all parts of the body are usually accompanied by a disturbance of consciousness and are called GRAND SEIZURES. At the beginning of a LARGE ATTACK, a person may scream or freeze in place, then he falls, the body stretches out and twitching begins. Such an attack lasts several minutes.
However, there may be disturbances of consciousness without convulsions - “ABSENCES”. This name translated means “absence” - a person freezes with a fixed gaze for one or several seconds. Those actions that a person carried out before the attack stop or slow down during freezing. So, for example, if he was writing before an attack, he may drop the pen or draw an uneven line instead of letters. Such attacks in children can be repeated during the lesson. If a child who is considered healthy periodically freezes with his gaze fixed on one point, or seems to “daydream” for several seconds, or is often “distracted” in class, he may actually have seizures of the absence seizure type.
Less common are COMPLEX PARTIAL SEIZURES (COMPLEX FOCAL, including PSYCHOMOTOR SEIZURES). With them, the disturbance of consciousness is not so noticeable externally, but is longer lasting (from a minute or longer) and is manifested not by a loss of consciousness, but by unusual or abnormal behavior. You can therefore have time to assess the state of consciousness by asking a child or adult with a seizure a question, for example, “Can you hear me,” and not receiving a clear answer to this. During such a psychomotor attack, a person can talk incoherently, without meaning, laugh, or shout. MOTOR (motor) manifestations of a PSYCHOMOTOR attack in children may consist of getting up from their desks, aimless movements around the classroom, or limited to smacking, sucking movements, unnecessary movements of the fingers or hands, etc. The teacher may confuse such attacks with behavioral disorders or self-indulgence.
During absence seizures and some psychomotor seizures, a person does not remember what was happening around him at the time of the attack, including what others approached him with. Such attacks may be subtle to the person and others. Therefore, in childhood, the teacher must analyze the nature of errors in written work, which may be caused by short-term blackouts.
Many other rarer types of seizures may occur, which usually include some elements of the structure of the seizures described above. In the diagnosis of a seizure type, many other terms may be used, not just those listed above.
WHAT FAMILY AND AROUND SHOULD PAY ATTENTION TO DURING AN ATTACK SO THAT THE DOCTOR CAN CORRECTLY IDENTIFY THE TYPE OF ATTACK AND PRESCRIBE THE CORRECT TREATMENT. SCHEME-QUESTIONNAIRE FOR DESCRIBING AN ATTACK.
To select the most effective anti-epileptic drug, it is necessary to accurately determine the type of seizure, since different drugs have different effects on different types of seizures. Some features of seizures also make it possible to determine in which area of the brain the main epicenter is located.
Therefore, during an attack, do not panic. Firstly, follow the recommendations for help during a seizure (see recommendations: “HOW TO HELP WHEN AN ATTACK OF CONVISIONS OR CHANGES IN CONSCIOUSNESS”). Secondly, carefully monitor the attack and, at the earliest opportunity, immediately after its completion, write down your observations. This must be done not only before the first visit to the doctor, when it is necessary to first establish the type of attack or clarify it. You must describe the attack again after a doctor has diagnosed the type of attack if the nature of the attacks changes or if a new type of attack appears.
It can be quite difficult to accurately describe the epileptic attack itself. The patient himself often has a memory loss at the time of the attack and is unable to describe the attack himself after regaining consciousness. Witnesses of an attack, as a rule, are too shocked, helpless and, out of excitement, do not pay attention to details. Since the details of the attack have different meanings, below is a diagram highlighting the most important points in the description of the attack. Additional comments are provided next to some questions or groups of questions. Use them if you find it difficult to formulate an answer to a question.
If you or your loved one has not one, but several types of attacks, then carry out the description below separately for all types of attacks.
It will be much easier for you to describe the attack if, as quickly as possible after the attack, you write down the answers to the following questions:
QUESTIONS FOR A PERSON WITH SEIZURES:
How does an attack begin? Are you conscious throughout the attack or is there some lapse in memory? Does the blackout end suddenly, literally immediately, or does it take some time for you to feel completely normal? How long does it take you to finally come to your senses? How do you feel during an attack? How do you feel after an attack? Do your muscles hurt after an attack? Are there any bruises after the attack? In what parts of the body? Are there any bites of the tongue, lips, or oral mucosa after the attack?
If the person did not have a memory loss during the attack or the memory loss was incomplete or partial, then he is asked the same questions below as the witnesses of the attack: QUESTIONS FOR THE WITNESSES OF THE ATTACK (AND THE PERSON WITH THE ATTACK, IF HE REMEMBERS ANYTHING ABOUT IT ):
1. BEGINNING OF THE ATTACK. How did you determine the onset of the attack (how did you understand that the attack had begun)? What did you immediately notice? Has your facial expression changed? Is your face turning pale? Are your eyes open? Does the gaze stop (fixed gaze)? Are your eyeballs rolling under your forehead?
1.1. UNILATERALITY OF ATTACK MANIFESTATIONS AT ITS BEGINNING. Do the eyes and/or head turn in one direction? Which way? Is there any other one-sidedness of movement, cramps or sensations at the onset of the attack? Did movements or sensations begin in any isolated part of the body?
Comment: In order for the doctor to determine in which half of the brain the epi-focus is located, you must identify the one-sided manifestation of the attack at its onset. This is indicated by turning the head and eyes in a certain direction before the onset of convulsions, one-sidedness of sensations or the onset of convulsions, etc. A more precise localization of the focus can be established if cramps or sensations begin not in the entire half of the body, but in part of it (in the fingers or hand, corner of the mouth, etc.).
1.2. WAS THERE AN AURA AT THE BEGINNING OF THE ATTACK? If there was, describe it.
Comment: When describing the nature of the attack, it is very important to identify whether the child or adult feels the approach of the attacks and how. These sensations at the very beginning of attacks are called “AURA”. Although the word "aura" is translated as "wind blowing", it can also manifest itself in other sensations. The nature of these sensations at the very beginning of the attack allows an experienced doctor to determine the location of the epi-focus in the brain and use this information to select the most effective treatment. The fact is that an aura is the result of irritation of a certain area of the brain by an epi-focus existing in this area of the brain. In addition, some people manage to prevent the further development of an attack at the time of the aura if they influence their sensations in a certain way (see recommendations: HOW TO HELP DURING AN ATTACK OF CONVISIONS OR CHANGES IN CONSCIOUSNESS. HOW TO HELP BEFORE AN ATTACK).
The sensations that a person experiences during an aura are varied. This may be a sensation of warmth radiating from the abdomen or chest. An aura can be expressed in the form of a sudden appearance of an unusual or familiar smell in the absence of its real cause in the room, sound or vivid visual images (auditory and visual hallucinations). In addition, the aura can manifest itself in a feeling of detachment, novelty when being in a familiar environment, or vice versa - a feeling of the familiar, already experienced, which suddenly appears in an unfamiliar situation. Unusual obsessive thoughts and emotions may be observed (fear, anxiety, depression or euphoria, anger for no reason). There may be other sensations during the aura, which are characteristic only for a given person. There may be more or more familiar sudden sensations - shortness of breath, palpitations, pain in some part of the body, abdominal pain, nausea, dizziness, etc.
Immediately before the attack, a person’s behavior may also change - the child may run up to you or try to lie down, looking for a safe place.
It is necessary to immediately ask the child or adult what he feels at this moment and during the aura, since after the attack he may forget his feelings.
Particularly important is the description of a person’s sensations when he feels an attack (aura) approaching, but for some reason the attack itself does not develop. Such an attack is called PARTIAL ("partial") ATTACK, since the entire picture of the attack is limited to an epi-discharge in a limited part of the brain (aura). Depending on which sense organ (vision, smell, hearing, taste, touch) is represented in this part of the brain, the SENSORY (sensitive) version of PARTIAL ATTACK is limited to such sensations.
The duration of the aura before the onset of the main part of the attack is also important - if the aura lasts 1-2 seconds, then the epi-focus can be located in the temporal region, with a longer aura - in the frontal lobe of the brain.
2. MOVEMENTS DURING AN ATTACK:
2.1. CONVISIONS: Have you had any seizures? If noted, which ones (check among those listed below).
2.1.1. JERKINGS = CLONIC CONVASIONS:
In what parts of the body were clonic twitches noted? Were there twitches on both sides or in one half of the body or face?
Comment: Clonic seizures are rhythmically repeated twitches. Most often, they involve rhythmic flexion or extension of the limbs. These limb movements are of small amplitude or volume. There may be repeated rhythmic tremors of the body, rhythmic twitching of the facial muscles, sometimes with rhythmic squinting (blinking) of the eyes.
2.1.2. JIVERING:
In what parts of the body was trembling noted? Was there shaking on both sides or on one side of the body or face?
Comment: Trembling is a hythmic, very frequently repeated twitching of very small amplitude (without changing the position of the limb). General trembling (chills) occurs if a person is cold (“Trembling from the cold”)
2.1.3. JERKES = MYOCLONIUS:
Were there general shudders (myclonias) of the whole body? Was there one general startle during the attack or several? Was the general flinching accompanied by flexion or extension (throwing) of the torso and limbs? Were there jerks (myclonia) in specific parts of the body or muscles, and not in the whole body at the same time? In what part of the body? How often did the flinching occur?
Comment: Unlike clonic convulsions, myoclonus is a separate (isolated) sharp, very fast (tenths of a second) startle, and not rhythmic repeated twitching. If myoclonic jerks are repeated throughout the attack, then, unlike clonic spasms, not often and at different intervals (not rhythmically).
2.1.4. TONIC CONVASIONS:
Was there at the beginning of the attack or during its course a tonic tension of the whole body with throwing back of the head, extension of the whole body in the form of an arc? Was the body tense during the attack or was it sluggish and limp “like a rag”? Was there a tonic contraction of the limbs or slow involuntary tense movements? In which limbs? In what position were the limbs brought together? Is the corner of the mouth pulled to the side? Was there a facial grimace? Does the skin around the mouth turn blue during an attack? Does your whole face turn blue? Are there any other changes in complexion (pallor, purplish-red coloration)?
Comment: Almost every one of us has experienced non-epileptic tonic cramps in the calf muscles or seen them in our loved ones - the calf muscles become hard (petrified) to the touch, you experience pain, and the foot “cramps” into a flexed position. Epileptic tonic convulsions also consist of muscle tension. The muscles become hard and tense - the limbs and body are pulled out or they freeze in an unusual position. Such tonic convulsions, if they occur in the muscles of the torso, can be accompanied by breath holding due to convulsive contraction of the respiratory muscles - while the person’s face begins to turn blue. “Stationary” tonic convulsions at the beginning of an attack are then usually replaced by variable muscle tension, which is therefore accompanied by slow movements of the body and limbs (the duration of one such tonic movement is 10 seconds or more). During other attacks, muscle tone may, on the contrary, decrease and the body becomes limp, like a “rag.”
2.2. OTHER MOTOR ACTS DURING A SEIZURE:
What repeated stereotypical (all the time the same) manipulations are performed by the patient’s hands: clapping, patting, rubbing, tugging or other movements? If the patient continues to sit during an attack, what do his legs look like: calm or in motion?
If a person remains on his feet during an attack, is he standing still? Does it rotate around the axis of the body? Does it freeze in a certain position? If he doesn’t stand still, how does he move during an attack?
Were swallowing movements, chewing, sucking, or licking lips noted? Is the attack accompanied by any sounds - grinding teeth, smacking, hiccups, slurping, swallowing, meowing, sobbing, moaning, or are individual words heard? Is there a scream, or a strangled growl, or wheezing, gurgling breathing?
Were there general chaotic violent movements during the attack?
Did you urinate during the attack?
2.3. FALL DURING SEIZURE. Did the fall occur during the attack if the patient was standing before the onset of the attack? If he was sitting with support during the attack or was supported, could he fall in the absence of support and support? How did you fall - did you slowly sag? Did your legs suddenly give way? thrown to the floor by a body push? Does it always fall in one direction (which?) or only backwards? or just forward?
Comment: with unexpressed convulsions, a person can stay on his feet or still fall. It is necessary to determine whether the person can independently stand on his feet during any attack without severe generalized convulsions. If a fall occurs, it is important to know whether the person fell sharply or slowly sank to the ground.
2.4. ARE THERE ANY INJURIES AFTER THE ATTACK? Are there any bruises? In what parts of the body? Are there any bites of the tongue, lips, or oral mucosa? Is there a pink color to the saliva during an attack or immediately after it?
3. STATE OF CONSCIOUSNESS DURING AN ATTACK.
Does the person with seizures answer your questions? If he answers, how correctly and clearly? Ask him in detail about his feelings and what happened to him. If he doesn’t answer questions, then does he react in any way to your approach to him by fixing his gaze on you, following your movement, fulfilling your requests and instructions? If consciousness is preserved, is it maintained throughout the entire attack or is it possible that it can be switched off or changed at some point during the attack? If so, how and when does it change?
Comment: it is important to find out whether there is a disconnection or change in consciousness during an attack (whether the person reacts and how to an address to him, whether he follows with his eyes, whether he tries to respond to your address to him). A complete loss of consciousness is a sign of GENERALIZED seizures, in which the “electrical discharge” in the head is not limited to a part of the brain, but spreads (generalizes) to the entire brain. During some attacks there are no convulsions, but only a loss of consciousness is noted. There may also be an altered state of consciousness in the form of unusual sensations, experiences, hallucinations, delusions or unusual behavior
4. SPEECH IMPAIRMENT DURING ATTACK. If the attack occurs without impairment of consciousness, then it is necessary to check whether the person can choose the words correctly and pronounce the words correctly in response to your questions? Does he clearly pronounce sounds and syllables?
5. CONDITION OF CARDIAC ACTIVITY - it is necessary to evaluate the pulse only in case of fainting-like attacks. Is the pulse rapid or slow? Were there any pulse interruptions (pauses between heartbeats)?
6. DURATION OF ATTACK AND CONDITION AFTER ITS END
How does the attack end - suddenly or gradually with fading convulsions and movements? How long did the attack last? Did it last 1-3 minutes? Did it last longer? If you lose consciousness during a seizure, is it possible to establish contact with the person immediately after the seizures (or other movements) stop? If not immediately, then after how long? Does any part of the body remain weak after the attack? How long? Does speech impairment remain after an attack with normal consciousness? What kind of speech impairment (see point 4) and for how long? How many minutes (hours?) after the end of the attack is the person’s condition completely normalized and can he continue his normal activities?
7. WHAT TO PAY ATTENTION TO WHEN AN ATTACK OCCURS DURING SLEEP? At what part of the night do the attacks occur? Right after falling asleep? When you wake up? How many hours after falling asleep? In the morning? Does the attack develop during deep or restless sleep? In general, is sleep itself deep or restless?
Comment: HOW TO DETECT SEIZURES DURING NIGHT SLEEP.
Parents and relatives may not notice nocturnal attacks in a child or adult - their sign may be pain in the mouth and tongue in the morning (when examining the oral cavity, you can find traces of biting the tongue or cheeks, which happened at night due to spasm of the jaws during an attack) or complaints the child has them on them. Sometimes after a night attack you can find traces of saliva on the pillow (including with a pinkish tint). A sign of a nocturnal attack may also be a case of nighttime urinary incontinence that is unusual for a given child or adult. If there were cramps at night, in the morning there may be pain, aches, fatigue or stiffness in those muscles that tensed during the night cramps. Unusual lethargy, fatigue and headache in the morning can also be a consequence of an attack that occurred in the morning.
If you suspect possible night attacks, it is advisable that someone from the family sleeps in the same room with a child or adult, you should leave the doors open at night in order to promptly hear sounds that may accompany an attack: shaking of the bed, wheezing breathing, etc.
8. WERE THERE ANY PREDICTS OF THE ATTACK? If there were, describe them. Comments: There may not only be an aura immediately before an attack; sometimes, several hours or even days before an attack, a person may become lethargic, tearful or irritable. He may have a headache or decreased appetite. Using such PREDICTS, an adult patient or a child’s parents can foresee the possibility of an attack in advance. If you do not notice any warning signs, ask a relative or loved one to observe you. Precursors of attacks are more clearly and reliably identified in the process of more or less long-term observation of attacks, if the attacks are repeated (see and use the “DIARY (CALENDAR) OF ATTACKS”).
9. WHAT CAUSED THE ATTACK? If there was a reason for the attack, describe it. Comment: most often, an attack develops spontaneously, without any external causes, since its development is caused purely by its own processes inside the brain, not related to the external environment. However, in a minority of people, certain “external” causes and influences can contribute to the occurrence of a specific seizure (provoke it). This can occur with reflex epilepsy (read the recommendations “WHAT IS EPILEPSY, EPILEPSY, AND EPI-REACTION. PROGNOSIS FOR SEIZURES”). You should carefully look for these provoking factors and suspicious circumstances that preceded the next attack and record them in your diary (to do this, read and follow the recommendations “LIFE STYLE DURING EPIC ATTACKS”). Identifying some of these triggers and avoiding them in the future may make it possible to reduce the effective dose of the antiepileptic drug taken. The doctor may also prescribe auxiliary means and methods to influence these provoking factors to prevent attacks.
However, most often, attacks can be provoked by a violation of the rules for taking medications set out in the recommendations: “HOW AND WHAT YOU CAN HELP YOURSELF, YOUR LOVED ONE OR CHILD IN THE PRESENCE OF SEIZES. THE MAIN METHOD FOR TREATING ATTACKS.”
Factors causing or provoking attacks are more clearly and reliably identified in the process of more or less long-term observation of attacks, if the attacks are repeated (see and use the “DIARY (CALENDAR) OF ATTACKS”). If you don't know what triggers your attacks, ask a relative or close friend to help you. They may notice the following symptoms:
1) how active (or inactive) were you (or the patient) before the attack began? Were you lethargic (drowsy) or excited (irritated, emotional) before the attack? Did you engage in any active (mental or physical) work before the attack, actively had fun or passively rested. Was the attack caused by any thought, stress, expressed emotion?
2) did you have a “lack of sleep” on the eve of the attack (was the attack triggered by insufficient sleep duration - went to bed late, got up early?)
3) did you drink wine, beer or strong alcoholic drinks the day before the attack? How much did you drink?
4) what did you eat before the attack and how much (too much, too little, some unusual dish or product)? Did the attack occur when you were hungry (skipped your usual meal)?
5) did the development of the attack coincide with any other unusual situation or circumstances?
To the table of contents of the article “Convulsions, epileptic seizures and epilepsy.”
Other types of epilepsy
Temporal lobe epilepsy
It is characterized by the localization of the focus of epileptic activity in the temporal lobe of the brain. It manifests itself in simple and complex partial epileptic seizures. As the disease progresses, secondary generalization occurs. The patient experiences mental health disorders.
Structural focal epilepsy
The onset of the disease occurs in individuals of various age groups. The lesion is located in the temporal zone of the brain. The patient feels time speeding up or slowing down. He perceives a familiar environment as new, and a new incident as something that has been experienced for a long time.
An epileptic seizure is manifested by the following symptoms:
- Preserved consciousness;
- Turning the eyes and head towards the localization of the focus of increased activity;
- The appearance of gustatory and olfactory paroxysms;
- The presence of auditory and visual hallucinations;
- Systemic dizziness.
The patient complains of pain in the heart, stomach, nausea, heartburn, and suffocation. There is a disturbance in the rhythm of cardiac activity, an increased feeling of fear, chills, and pale skin. As temporal lobe epilepsy progresses, a secondary generalized form of the disease develops. The attack is manifested by tonic convulsions in all muscle groups, loss of consciousness.
Post-traumatic epilepsy
Develops as a result of meningitis, encephalitis, traumatic brain injury, asphyxia. The disease is more often diagnosed in children. The attack is not accompanied by loss of consciousness or occurs with impaired consciousness. If the patient loses consciousness, they may experience a secondary generalized seizure. The muscles of the foot and upper limbs are involved in the convulsive process.
Why is an epileptic seizure dangerous?
During a tonic-clonic seizure, breathing stops, and in all other seizures with convulsions, additional trauma is possible due to hitting the head on a hard surface. Falls from one's own height and loss of consciousness are also dangerous. Each seizure that occurs damages the neurons of the brain, which subsequently leads to a decrease in cognitive and mental abilities, and changes in the psyche.
This does not prevent patients with epilepsy from leading an active life. However, some aspects are limited - it is prohibited to drive a car and work in production in workshops, with open fire or at height, as well as in work that requires frequent switching of attention. Properly selected therapy can increase the interictal period by months or even years.
Make an appointment
Reanimatology School of Professor Sergei Vasilievich Tsarenko
Despite the seemingly a priori importance of the prophylactic use of anticonvulsants, the issue of primary prevention of seizures is not resolved with the help of medications. Numerous studies have shown that the prophylactic use of anticonvulsants does not reduce the frequency of seizures (JK McQueen et al., 1983; S. Manaka, 1992). Primary prevention of seizures is timely surgical treatment and prevention of secondary brain damage.
Indications for anticonvulsant therapy are the presence of EEG signs of convulsive syndrome (registration of the so-called peak-wave complexes) and the identification of clinical symptoms - partial seizures, full-blown seizures, a series of seizures and epistatus. In this situation, we are talking about the treatment and secondary prevention of seizures.
Each seizure may be accompanied by a sharp increase in ICP, impaired cerebral perfusion and ischemia. It is surprising that, despite the clear understanding of this thesis by most doctors, it is difficult to imagine another clinical situation that would be accompanied by the same amount of terminological and treatment confusion. Often, resuscitators do not clearly understand the terminology and clinical significance of a detailed neurological diagnosis and do not undertake the “hard” work of describing a seizure. But a detailed description of the seizure pattern allows us to assume the localization of the focus of ectopic activity, which is important for prognosis and choice of treatment tactics! To determine the prognosis, it is important to understand that any seizure is dangerous, but full-blown clinical-tonic seizures are more dangerous than partial ones, since the increase in ICP is much higher and cerebral ischemia is more significant. A series of seizures is more dangerous than a single seizure, and epistatus is more dangerous than a series of seizures. It is appropriate to recall that the difference between a series of seizures and epistatus is not in the number and nature of seizures, but in the fact that with a series of seizures the patient comes to consciousness in the intervals between them, and with epistatus he is in a coma. Naturally, such differentiation is impossible if the patient was in a coma before the seizure.
The second problem is the lack of understanding by doctors which drugs have anticonvulsant properties, what their comparative effectiveness is and the algorithm for clinical use. Without going into a detailed analysis of the problem, we will consider the main antiepileptic drugs. They are shown in Table 11. On the right side of the table, anticonvulsants are arranged in descending order of effectiveness. Since the intravenous form of not all of these drugs is registered in our country, the drugs available in Russian conditions for parenteral administration are also listed on the left side of the table in descending order of effectiveness.
Table 11. Modern anticonvulsants, listed in descending order of effectiveness
* – drugs that have both anticonvulsant and proconvulsant effects
A clear understanding of the hierarchy of effectiveness of anticonvulsants is of great clinical importance. Diazepam (Relanium, Seduxen, Sibazon) is a common emergency medicine, but is far from the most effective anticonvulsant drug. Barbiturates are somewhat outdated and also not very effective means for relieving seizures. In addition, thiopental and hexenal are short-acting, and phenobarbital and benzonal, although they have longer-lasting effects, require enteral administration. Sodium hydroxybutyrate has, in addition to anticonvulsant, in some cases, a proconvulsant effect.
Narcotic analgesics and muscle relaxants do not act at all on the seizure focus in the brain and relieve only the muscle component of seizures. The use of muscle relaxants is necessary only for tracheal intubation and synchronization with a respirator. In all other cases, the use of these drugs confuses the doctor, who believes that the convulsions have been stopped, when in fact, muscle contraction is simply not visible while the activity of the cerebral convulsive focus remains. It would not be worth talking about this if a common mistake in the treatment of convulsive syndrome is the use of muscle relaxants instead of anticonvulsants. At the same time, the administration of muscle relaxants masks the ineffectiveness of stopping seizures. This error leads to prolongation of status epilepticus and an increase in the number of complications.
Before moving on to the characteristics of individual drugs, it is necessary to emphasize two fundamental points.
•The first important point is that convulsions must be completely stopped and the sooner the better. In this regard, if monotherapy is ineffective, it is necessary to use a combination of anticonvulsants. What means and doses of drugs will achieve the effect is of less importance.
•The second important point is that stopping seizures begins with drugs for intravenous administration. If they are ineffective, they switch to the combined use of anticonvulsants - parenterally and through a tube. This algorithm makes it possible to use those effective drugs that are not available in parenteral form, and, in addition, to combine the pharmacokinetic features of the parenteral route of administration - the speed of onset of the effect - and the enteral route - the duration of action.
Lorazepam (Merlit, Lorafen) is a benzodiazepine. It has, unlike diazepam, significantly higher anticonvulsant activity, but is metabolized more slowly. Lorazepam is the best anticonvulsant drug. If an intravenous form is available (registered abroad), lorazepam is administered at a rate of 0.03-0.07 mg/kg; administration can be repeated after 10 minutes if necessary. The duration of the effect when administered intravenously is 150-180 minutes. The drug is used orally at a dose of 0.07 mg/kg 2 times a day. Typically the effect lasts about 12 hours.
Diazepam is the second-line drug of choice (in our country, the first-line drug for intravenous administration). 0.15-0.4 mg/kg is administered intravenously at a rate of 2.5 mg/min. If necessary, the drug can be reintroduced after 10-20 minutes. The duration of the effect when administered intravenously is 180-240 minutes. It is also possible to administer diazepam by drip – 0.1-0.2 mg/kg•h. The effectiveness of diazepam is greatest when used early. Disadvantages of the drug are respiratory depression and hypotension with rapid administration. During the biotransformation of diazepam in the body, three active metabolites are formed, so individual fluctuations in the duration of the drug's effects are possible. Since diazepam metabolites are excreted in the bile, they can be reabsorbed from the intestine into the blood and cause repeated sedation (the so-called “rebound” phenomenon).
Midazolam (dormicum) can successfully replace diazepam, since it has almost the same properties and is administered in the same doses (0.2-0.4 mg/kg). Respiratory depression is somewhat more pronounced. The duration of the effect when administered intravenously is 60-90 minutes. Unlike diazepam, midazolam has only one active metabolite, which makes its action more predictable. As reserve drugs, in the absence of the effect of the above benzodiazepines, it is possible to use drugs of the same series registered in Russia, which have significant anticonvulsant potential. Flunitrazepam (Rohypnol) deserves the most attention. The drug is administered at a dose of 0.015-0.03 mg/kg. The duration of the effect when administered intravenously is 180-240 minutes. The drug has three active metabolites. Side effects and contraindications are the same as for other benzodiazepines.
Equivalent doses of benzodiazepines: 1 mg flunitrazepam = 2 mg lorazepam = 10 mg diazepam = 10 mg midazolam.
Valproic acid (Depakine) is a third-line drug. It is currently available in intravenous form, syrup and tablets. Intravenous administration is carried out over 3-5 minutes at a dose of 6-7 mg/kg, followed by a constant infusion at the rate of 1 mg/kg•hour. If polytherapy with enzyme-inducing drugs (carbamazepine, phenobarbital, phenytoin) is carried out, then the maintenance dose of depakine is 2 mg/kg•h. It is possible to administer maintenance doses not in the form of a constant infusion, but in the form of repeated boluses 4 times a day. The total daily dose is up to 25-30 mg/kg•day. The advantage of the drug is its speed of use (reaching a therapeutic level in the blood in 3-5 minutes) and good tolerability. It has no sedative properties, does not lower blood pressure and does not require monitoring of blood levels. The oral dose is equivalent to the intravenous dose. Contraindications to the use of the drug are acute and chronic hepatitis.
Phenytoin (diphenin) is the fourth choice drug. If there is an intravenous form (registered abroad), it is administered at a dose of 15-18 mg/kg at a rate of no more than 50 mg/min. The usual dose is 1000 mg/day. A water-soluble form of phenytoin, fosphenytoin, has now been created. In Russia, parenteral forms of phenytoin and fosphenytoin are not registered, so administration of phenytoin through a nasogastric tube in a dose of up to 20 mg/kg can be used.
Repeated administration - no earlier than a day later. The advantage of the drug is its prolonged action. It does not have a depressing effect on the level of consciousness and breathing. The disadvantages are the delayed onset of action, as well as the disturbances in the conduction function of the heart that it causes, so ECG monitoring is mandatory when using it. Contraindications to the use of diphenin are atrioventricular block II-III degree and sick sinus syndrome, as well as porphyria and bone marrow diseases.
Carbamazepine (finlepsin, tigretol) is a widely used anticonvulsant of next choice. Usual doses of the drug are 800-1200 mg/day, divided into 3-4 doses. The drug is well tolerated, but with long-term use (more than 2 weeks) it can cause an increase in liver enzyme levels.
This does not reflect serious liver problems and is not an indication for stopping the drug.
During treatment, it is not recommended to reduce doses, as this may lead to subtherapeutic blood concentrations and relapse of seizures. If in this case the decision is made to return to carbamazepine, the doses will have to be increased compared to the initial ones due to the development of tolerance. Thiopental is the third-line drug of choice for intravenous administration in our country after benzodiazepines and depakine. 250-350 mg of the drug is administered intravenously over 20 seconds, then at a rate of 5-8 mg/kg•h. The disadvantage of the drug is the pronounced tendency to cumulation, the development of tolerance and the arterial hypotension it causes. Although some authors point to the possible proconvulsant effects of hexenal and methohexital (Brietal), we have never observed them. Therefore, we believe that these drugs can be used similarly to thiopental, only in different dosages. Hexenal is administered in a dose of 6-8 mg/kg as a bolus, then 8-10 mg/kg•h to maintain the concentration of the drug in the blood. A bolus dose of Brietal is 1-3 mg/kg, maintenance – 2-4 mg/kg•hour. The duration of the effect of thiopental and hexenal is 30-40 minutes, brietal - 10-15 minutes. Propofol and sodium hydroxybutyrate are usually used to control seizures in the same doses as for controlled sedation of patients. It is necessary to remember the possible proconvulsant effect of hydroxybutyrate. ‹ 6.2.3. Correction of intracranial hypertension.Up6.2.5. Treatment of extracranial and intracranial purulent-septic complications. ›
Diagnostics
Diagnosis of the disease occurs by taking an anamnesis. The specialist listens to complaints, on the basis of which a preliminary diagnosis can be made.
After this, the patient is sent for laboratory and hardware examinations, which makes it possible to differentiate epileptic seizures from other pathologies, allows one to find out the cause, the nature of the changes, determine the form and prescribe treatment.
The diagnosis is made by neurologists and epileptologists who determine the causes of epilepsy in adults using indications obtained from a comprehensive comprehensive examination.
Instrumental diagnostic methods
The safest hardware diagnostics is an EEG. It has no contraindications; it can be used to detect areas of paroxysmal activity. These can be sharp waves, spikes, slow waves. Modern EEG makes it possible to identify the exact localization of the pathological focus.
The most informative neuroimaging method is brain MRI. The study allows us to identify the initial cause of the deviation and determine the location of the lesion in the central nervous system.
Laboratory diagnostic methods
Epilepsy occurs under the influence of various reasons; in order to identify the presence of infection, inflammation, hormonal imbalances, genetic defects, the patient needs to take a general blood test, biochemical, molecular genetic, and check the tumor marker.
First aid for seizures
Proper care for an epileptic seizure reduces the risk of complications and injuries. The person who happens to be next to the patient should catch him and prevent him from falling. You also need to do the following:
- Place a blanket, pillow or cushion of clothing under your head;
- Free your neck and chest from constricting objects and clothing (tie, shirt, scarf);
- Carefully turn the patient's head to the side to minimize the risk of inhalation or passive reflux of vomit or own saliva;
- Open your mouth and put a cloth or handkerchief in it to prevent the patient from biting his tongue;
- Do not forcefully open your mouth;
- If breathing stops for a long time, perform artificial ventilation from the mouth to the nose or mouth.
During an attack, the patient may experience involuntary urination or bowel movements. This manifestation of epilepsy should not cause fear in others. After an attack, patients usually experience drowsiness and severe weakness.
Treatment
Neurologists at the Yusupov Hospital provide complex treatment for epilepsy. It is aimed at reducing the frequency of epileptic seizures and stopping medications during remission. According to statistics, in 70% of cases, adequately selected treatment helps to almost completely relieve paroxysmal activity in patients.
To achieve optimal results in treatment, patients are prescribed drugs for epilepsy of the following properties:
- anticonvulsants – help relax muscles, they are prescribed to both adults and children;
- tranquilizers - allow you to remove or reduce the excitability of nerve fibers; the drugs have shown a high degree of effectiveness in the fight against minor attacks;
- sedatives – help relieve nervous tension and prevent the development of severe depressive disorders;
- injections - used for twilight states and affective disorders.
Idiopathic focal epilepsy is benign. It requires symptomatic treatment. In focal forms with seizures that appear in series 2-3 times a month and are accompanied by an increase in mental disorders, neurosurgeons perform surgery.
Is epilepsy curable?
Before starting treatment, a diagnosis should be determined, because loss of consciousness and various convulsions can occur due to a sharp drop in blood sugar, anemia, poisoning, high fever, cerebrovascular accident, calcium deficiency and other conditions. Antiepileptic drugs cannot be prescribed to such patients immediately. The diagnosis of epilepsy is made only when epileptic seizures recur.
With adequate treatment, according to generalized statistics, a good therapeutic effect is achieved in 80-85 percent of patients, and in 60-70 percent of patients seizures can be eliminated completely. And this is a very good reason to stop antiepileptic drugs.
The percentage of patients with epileptic seizures could be significantly lower if patients took medications regularly and did not stop treatment on their own. The decision to discontinue medications can only be made by a doctor, and not earlier than after 5 years of treatment, if during this time the patient has not had epileptic seizures. At the Yusupov Hospital, an epileptologist always monitors how the patient’s illness develops.
CONVASIONS
CONVASIONS
- involuntary contractions of striated or smooth muscles, varying in intensity, duration and prevalence, of a paroxysmal nature. Convulsions are one of the types of hyperkinesis (see).
Based on the nature of muscle contraction, seizures are classified into clonic and tonic. Clonic movements are characterized by short-term contractions and relaxations of individual muscle groups, quickly following each other, which leads to stereotypical rapid movements of varying amplitude. Tonic S. are longer (up to 3, sometimes more than minutes) muscle contractions, as a result of which a “freezing” of the torso and limbs is created in various forced positions. The variety of S. found in wedges, practice, does not fit into the framework of this classification. There are many forms of mixed seizures: when the tonic component predominates in muscle contraction, seizures are defined as tonic-clonic, and when the clonic component is pronounced, they are considered clonic-tonic.
Clonic S. usually occurs when the cells of the cerebral cortex, especially its motor department, are overexcited. This type of S. is characterized by their somatotopic distribution throughout the muscles and muscle groups, according to the location of the motor cortical centers in the anterior central gyrus. So, for example, starting from the muscles of the face, clonic S. seizes successively the muscles of the fingers, hands, forearm, shoulder, legs (so-called cortical epilepsy). Tonic S. occur, as a rule, with excessive stimulation of the subcortical structures of the brain.
Depending on the prevalence, S. is divided into localized in one muscle or group of muscles and generalized, involving many muscles. Generalized S. can be the final stage of convulsive paroxysm of any type.
S. are caused by various exogenous and endogenous reasons. S. of different etiologies are not the same in form, frequency of attacks, their course, characteristics of the post-attack period, combination with other wedges, symptoms and laboratory data. At the same time, S. identical in form can occur in various diseases of the nervous system, accompanied by functional, structural, metabolic and liquorodynamic disorders - meningitis, encephalitis, abscesses, parasitic diseases and brain tumors, cerebral vascular aneurysms, traumatic brain injury, intracerebral, subarachnoid and subdural hemorrhages, vascular spasms, ischemic strokes, etc. At the same time, S. are both generalized and local, in the latter case often indicating the primary localization of patol. hearth. S. are often an early symptom of hereditary degenerative diseases of the nervous system: leukodystrophies (see), etc., occurring with demyelination of the nervous system, progressive senile dementia - Alzheimer's disease (see Alzheimer's disease), Pick's disease (see Pick's disease) and etc.; Huntington's chorea (see Huntington's chorea); torsion dystonia (see), double athetosis. S.'s attacks, beginning with local myoclonus, later generalizing and turning into a general convulsive seizure, are observed in myoclonus epilepsy (see). For tuberous sclerosis and encephalotrigeminal angiomatosis, attacks of localized S. are more characteristic (see Phakomatoses).
Somatic diseases leading to cerebral circulation disorders and hypoxia of brain tissue can also be accompanied by the development of S. S. is often observed with heart defects and pathology of the great vessels, blood diseases (leukemia, blood coagulation disorders, hemorrhagic vasculitis), collagen diseases (systemic red lupus, periarteritis nodosa, rheumatism). S., caused by metabolic disorders in brain tissue and associated with endogenous intoxication, develop in hypoglycemic coma, hepatic coma (see). In these conditions, S. usually have a generalized tonic-clonic character. S. in eclampsia (see) of pregnant women are symmetrical and cover the muscles of the face, trunk, limbs, and may be accompanied by a short-term loss of consciousness. In cases where acute disorders of cerebral circulation occur during eclampsia, large convulsive attacks sometimes develop. Uremic coma (see) is characterized by erratic, asymmetrical contractions of individual muscles or muscle fibers (muscle fibrillations). Sometimes these S. turn into generalized clonic-tonic convulsive attacks. S. in burn shock (see) are usually tonic or tonic-clonic in nature and, as a rule, develop in patients with deep burns, occupying from 5 to 40% of the body surface.
Various exogenous intoxications can lead to S.'s development (see Intoxication). So, for example, carbon monoxide poisoning, accompanied by a coma, can cause tonic S. such as decerebrate rigidity, trismus; Alcohol intoxication can manifest itself as generalized convulsive attacks, which more often occur at the onset of delirium delirium. This group also includes S. for tetanus (see).
Sometimes S. occurs in patients suffering from neuroses with increased excitability of the nervous system. However, S. defined as hysterical always require a special comprehensive study, since S., interpreted as functional, are often based on hidden organic lesions of the nervous system.
The causes of S. in the neonatal period may be perinatal asphyxia, intracranial birth hemorrhage, brain malformations, neuroinfections, metabolic disorders (acidosis, hypocalcemia, alkalosis, hypoglycemia, hyponatremia, hyperbilirubinemia, vitamin B6 deficiency). S. in newborns are often the first wedge. manifestation of hereditary diseases - neurolipidoses (see Lipidoses), encephalotrigeminal angiomatosis (see), tuberous sclerosis (see), familial acidosis (see), etc. The cause of S. in infancy, as well as in the neonatal period, can be organic lesions of the nervous system, neuroinfections, malformations of the brain. S. are observed in almost half of patients with cerebral palsy (see Infantile paralysis). S. in hereditary diseases such as phenylketonuria (see), decarboxylase deficiency (see), leukodystrophy (see), phakomatoses (see), more often occur in infancy in combination with severe retardation of psychomotor development and are much less likely to be the first a sign of disease. S. may accompany preventive vaccinations (post-vaccination convulsive syndrome).
The cause of S.'s development in young children may also be congenital heart disease. The severity of convulsive attacks and their frequency depend on the nature of the heart damage and the severity of general hemodynamic disorders. Older children may experience seizures caused by heart rhythm disturbances.
Children who have suffered a closed craniocerebral injury may experience S. caused by chronic intracranial hematoma, as well as traumatic epilepsy, characterized by a progressive course with the gradual formation of epileptoid personality changes (see Epilepsy).
Pathogenesis
seizures are complex. In connection with the different mechanisms of development of convulsive paroxysms, a distinction is made between a convulsive reaction, a convulsive syndrome and an epileptic disease (see Epilepsy).
A convulsive reaction occurs in response to irritations that are extraordinary for a given organism, caused by infection, intoxication, overwork, staying in a stuffy room (hypoxia), etc. A convulsive reaction can develop in any healthy person, but it occurs more easily with increased convulsive readiness. The degree of convulsive readiness is variable and undergoes individual changes depending on circadian rhythms, under the influence of endogenous and exogenous factors. The level of convulsive readiness also depends on the degree of maturity of the nervous system, its age and genetic characteristics. In childhood, S. occurs 4-5 times more often than in adults. Incomplete differentiation of the child’s brain and, as a consequence, physiological hypersynchronization of the “work” of cells determine the frequent occurrence of convulsive seizures in children under the influence of minor exogenous or endogenous influences. An example of a convulsive reaction is hyperthermic S., which is most often observed in children under three years of age, during a period of increased convulsive readiness. The older the person, the more severe the impact can cause S. An example of a convulsive reaction in adults is S. in insulin shock, poisoning with tetraethyl lead, carbon monoxide, massive alcohol intoxication, etc.
The convulsive reaction is characterized by episodic paroxysms (see).
Convulsive syndrome develops, as a rule, with actively ongoing pathol. processes in the nervous system. In its occurrence, the acquired decrease in the threshold of convulsive readiness of the brain is of primary importance, while the role of exogenous factors in the development of S. is somewhat lower. Convulsive syndrome is characterized by recurrence of paroxysms. Convulsive readiness is physiologically characterized by all the signs of a dominant and represents an extreme degree of central excitation that goes beyond normal limits. Its pathophysiological sign is a change in the electrical activity of the cortex and subcortical formations, consisting in synchronization and hypersynchronization of the theta rhythm, the presence of paroxysms of convulsive potentials in the structures of the limbic system (see), slowdown of synchronized rhythm in the mesodiencephalic reticular formation (see), intralaminar nuclei of the thalamus, caudate nucleus and in the cerebral cortex (epileptiform activity). At the same time, both the background and evoked activity of individual neurons changes. Early and distinct changes in biopotentials are recorded in the hippocampus, which has high excitability and an abundance of bilateral connections, which ensures a large influx of afferent impulses to it. Structures with a low seizure threshold also include the amygdala and the structures of the medial thalamus (see). For the development of convulsive paroxysm against the background of convulsive readiness, an additional influx of afferent impulses to the focus of increased excitability (primary focus) is required, as a result of which a pathological dominant is formed. S.'s paroxysm can occur with irritation of any part of the c. n. pp., subject to increased excitability of brain structures outside the lesion and, above all, increased excitability of the cerebral cortex. Experimental electrophysiological studies have shown that when the cerebral cortex is stimulated, evoked potentials at the height of a convulsive state are recorded not only in the projection zones, but also in other areas. Irritation, which in a normal animal causes the appearance of the usual complex of evoked potential, after the introduction of a subthreshold convulsive dose of camphor leads to the appearance of group discharges, turning into generalized epileptiform activity, and subsequently to the development of seizures. In this case, the excitability of the motor cortex increases 3-4 times compared to the norm. The degree of synchronization of biopotentials in different brain structures reflects the severity and spatial distribution of convulsive readiness. A shift in the wave spectrum towards low-amplitude synchronized oscillations on the EEG is observed long before the onset of convulsive paroxysm and may indicate its future nature (local, general). The spread of excitation from the focus of increased activity occurs not only along the surface of the cerebral cortex, but to a large extent along the reticular structures of the brainstem. In convulsive syndrome, prolonged irritation of limited areas of the cerebral cortex leads to the gradual formation in the subcortical sections of independent foci of excitation of a stagnant nature, which can be active even after the cessation of irritation of the cortex, regardless of the primary focus. The focus of excitation in the subcortical structures, in turn, causes generalized excitation of the cerebral cortex (the so-called recurrent generalization of excitation). An important role in the generalization of excitation belongs to the rostral part of the reticular formation - the midbrain and hippocampus. Changes in the functional state of the mesodiencephalic reticular formation sharply affect the level of convulsive activity. In the crust, time has been shown that weak irritation of the reticular structures contributes to the formation of a stagnant focus of excitation in the hippocampus and facilitates the creation of convulsive readiness and the appearance of S. It is noted that strong irritation inhibits the paroxysmal activity of the hippocampus and leads to a significant decrease in convulsive readiness. It has also been established that high functional tone of the cerebral cortex leads to a decrease in convulsive readiness, and the main role in this process belongs to the frontal parts of the cerebral hemispheres. Intracellular recording of neuronal activity in the pathological seizure focus revealed significant changes in the membrane potential (towards its depolarization) and an increase in synaptic excitation. Depolarization shifts occur in the soma-dendritic regions of the neuron, which have a postsynaptic membrane. They are the result of the summation of excessively enhanced depolarizing postsynaptic potentials. S. of various origins have a significant effect on the metabolism of cellular protein, causing an increase in its breakdown while simultaneously inhibiting synthesis. At the same time, a decrease in RNA content in brain tissue, damage to mitochondria, and disruption of oxidative phosphorylation processes were noted (see).
S. in epilepsy (see) more often arise against the background of a hereditary increase in convulsive readiness of the brain. S.'s attacks usually occur without any noticeable provoking factors.
In many cases, especially in early childhood, the differentiation of epilepsy, convulsive syndrome and convulsive reaction is difficult, since the boundaries of these conditions are arbitrary. So, for example, a convulsive reaction in children can sometimes be an early manifestation of epilepsy, and a convulsive syndrome under the influence of prolonged exposure to an exogenous factor and secondary disorders of brain metabolism and cerebral circulation can transform into epilepsy.
In wedge, practice, along with the pathogenetic classification of convulsive conditions, S. is subdivided depending on the characteristics of muscle contraction (clonic and tonic), their frequency, according to the violation of the biochemical constants of the body, the level of damage to the nervous system, and prevalence (local, generalized).
Depending on the frequency of occurrence, S. is divided into episodic and constant. The latter, in turn, are characterized as periodic (serial) and convulsive status.
S., arising as a result of biochemical disorders, are divided into hypocalcemic (see Tetany), hypoglycemic, hyperbilirubinemic, pyridoxine-dependent, hypomagnesemic (see Spasmophilia), etc.
According to the level of damage to the nervous system, they are conventionally divided into: clonic convulsions of cortical origin; constant arrhythmic clonic convulsions in certain muscle groups (Kozhevnikov epilepsy); tonic or clonic convulsions in the limbs opposite to the lesion in Jacksonian epilepsy (see); stem S.—gaze convulsions, hormetonia (see), myoclonus of the soft palate, tongue, etc.
The localization of S. is different, and S. of the facial muscles is often observed: facial hemispasm - one-sided tonic S. of the facial muscles with the appearance of wrinkles on the forehead, pulling the corner of the mouth outward and upward, with tension in the subcutaneous muscle of the neck on the side of the spasm; facial paraspasm - periodically repeated tonic symmetrical muscles of the face; spasm usually begins with contraction of the orbicularis oculi muscles, then contraction of the orbicularis oris, cheek muscles, chin, neck, and tongue joins; sometimes these spasms are combined with clonic S. muscles of the mouth, neck and are often accompanied by pain; blepharospasm (see) - tonic S. of the circular muscles of the eyes, manifested by painful squinting, less commonly observed clonic S., leading to frequent blinking; platysmal spasm - tonic tension of the superficial muscle of the neck; S. can sometimes spread to the muscles of the chin and the orbicularis oris muscle; S. gaze (see Gaze paralysis, convulsion) - tonic S. of the oculomotor muscles, manifested by involuntary freezing of the eyes in the position of extreme abduction of the eyeballs (to the sides, up, down); sternocleidomastoid muscles - clonic S. of the sternocleidomastoid muscles, characterized by fast, low-amplitude, rhythmic nodding movements of the head; alternating muscle contraction can lead to rotational movements of the head (so-called rotatory S.); S. of the diaphragm is often clonic in nature and is manifested by hiccups (loud, rapid inhalation with a characteristic sound). Clonic and clonic-tonic S. of the muscles involved in the speech act and the respiratory muscles lead to stuttering (see). Tonic S. of the masticatory muscles (see Trismus) lead to a tight closure of the jaws, in which the patient sometimes cannot eat or speak. Local tonic S. can occur in the gastrocnemius, sartorius, abdominal, intercostal and other muscles and are accompanied by sharp pain (cramps); On palpation, muscle tightening is determined. Characteristic tonic S. of the muscles of the hand (“obstetrician’s hand”), muscles of the face, feet (“horse foot”) are observed with spasmophilia (see), tetany (see). Localized static S., or Govers' saltatory spasm, is manifested by rapid rhythmic bouncing due to clonic contraction of the leg muscles. At the beginning of a movement performed with a load, Ryulff's intentional cramp can develop (see Ryulff's intentional cramp), when a clonic contraction of the muscles occurs in the limb producing the movement, then S. spreads to other muscle groups. Local tonic spasm of the muscles of the fingers and hand is sometimes observed during prolonged writing (see Writer's cramp) or when playing musical instruments. S. of the muscles of the thumb and index finger - dactylospasm - is observed in tailors, typists, telegraph operators, milkmaids, saddlers, shoemakers, and hairdressers. KS associated with prolonged professional stress also include blepharospasm in watchmakers and spasm of the leg muscles in ballerinas.
Generalized tonic S. can occur as hormetonia (see) - a type of periodic tonic S. of the trunk and extremities that occurs with extensive cerebral lesions. During hormetonic S., the spine is slightly extended, the arms are extended, they are in a pronation position, and the legs are extended. A type of generalized tonic S. is also decerebrate rigidity (see).
Generalized clonic S. are sometimes manifested by frequent rhythmic shuddering of the torso and trembling of the limbs (previously called convulsions). A type of clonic S., myoclonus, is characterized by asynchronous, chaotic, “lightning-fast” contractions of various muscles. Myoclonus can be generalized and local.
Tonic-clonic convulsions accompanied by loss of consciousness are classified clinically as a grand mal seizure (paroxysm). The structure of a convulsive seizure can combine various tonic and clonic S. The structure of convulsive seizures in newborns, infants and older children has specific features. Convulsive paroxysms in newborns are manifested by lightning-fast, generalized tonic and clonic S., which can easily be mistaken for the normal movements of a newborn: blinking, squinting of the eyelids, moving the eyes to the sides, twitching of the eyeballs, smacking, sucking, hand movements reminiscent of swimming or rowing, leg movements reminiscent of cycling, tonic contraction of individual muscle groups of the limbs. Unlike physiological movements, S. are usually combined with vasomotor and other autonomic disorders and are accompanied by specific changes in the EEG (see Electroencephalography). Tonic seizures with sudden extension of all limbs or flexion of the arms and extension of the legs are characteristic of premature newborns; in full-term infants, such paroxysms often indicate hemorrhage into the ventricles of the brain.
Generalized clonic S.—alternating contractions of individual muscle groups migrating from one part of the body to another, are often observed in full-term newborns.
Myoclonic type S. in newborns is characterized by single or multiple twitching of the upper or lower extremities with a tendency to bend them. These attacks are usually accompanied by screaming and changes in skin color.
After the neonatal period, the motor component of a seizure becomes more pronounced. For infants, general tonic seizures are more typical - the so-called. infantile spasms, characterized by bilateral symmetrical muscle contraction. Flexor spasms are also called propulsive seizures or “salaam seizures.” During paroxysm, a sudden flexion of the neck, torso, and arms occurs, which are bent and brought toward the body (or, conversely, abducted). Extensor spasms (retropulsive seizures) are manifested by a sharp extension of the head and torso, abduction of the arms. Infantile spasms also include partial, fragmented forms of S.—nodding, wincing, flexion and extension of the arms and legs. All forms of infantile spasms can be combined with each other; their distinguishing feature is their tendency to be serial. The duration of S. can be from a fraction of a second to several seconds. A series of attacks lasts from a few seconds to 20 minutes. and more. During the day, the number of paroxysms ranges from a few to several hundred and even thousands. S. occur most often before falling asleep or after waking up. Infantile S. may be accompanied by a scream, a grimace of a smile, a frightened facial expression, rolling of the eyes, trembling of the eyelids, pallor or redness of the face, and temporary cessation of breathing. With frequent serial attacks, children are inhibited, and loss of consciousness is sometimes observed. After the age of three, infantile spasms are rare.
Grand mal seizures in young children are often abortive in nature; the tonic component predominates in the structure of the seizure. Attacks may be accompanied by fever, vomiting, abdominal pain and other vegetative symptoms.
Post-vaccination S. occurs several hours after vaccination or on the 1st–3rd day and only in isolated cases at a later date. S. usually local or small propulsive. After vaccination against measles, S. can be observed during the period of fever on the 6-7th day and are in the nature of single tonic-clonic seizures.
Febrile S. occurs against the background of diseases occurring with high temperature (see Hyperthermia syndrome). The frequency of febrile seizures in children reaches 8-10%. S. can be generalized in nature with a predominance of the tonic component in the structure of the attack, or be focal. In 50% of cases, febrile S. with hyperthermia can recur. In cases of repeated febrile seizures and the appearance of seizures outside the state of hyperthermia, the risk of developing epilepsy in the future increases significantly.
In children with increased excitability of the nervous system aged 7-8 months. up to 2 years of age, respiratory affective symptoms are observed. The occurrence of such symptoms is provoked by fear, severe pain, and anger. During a scream, the breath is held while inhaling (inspiratory cessation of breathing), cyanosis develops, the head is thrown back, the pupils dilate, and consciousness is lost for several seconds. As a result of developing hypoxia, a generalized convulsive seizure may occur. S. can be prevented by switching the child’s attention at the moment of screaming. Approximately 50% of children with affective-respiratory S. have emotional and behavioral disorders.
The diagnosis of convulsive conditions involves, first of all, clarification of the cause of S.’s occurrence, i.e., diagnosis of the underlying disease. For this purpose, all patients who have had at least one convulsive paroxysm undergo a comprehensive clinical examination, including electrophysiological, radiological, biochemical, and cytological studies. An important place belongs to the anamnesis, on the basis of which the premorbid characteristics of the patient, factors contributing to the occurrence of S., the nature of the convulsive syndrome, the presence of S. and their analogues and other neurol are determined. disorders in the patient's relatives. Electroencephalography helps clarify the nature of the underlying pathological process and objectify the presence of convulsive brain activity (see). The EEG with S. records paroxysmal discharges of high amplitude, with a pointed waveform and peaks, occurring in isolation or in combination with a trace slow wave. The form of paroxysm on the EEG depends to some extent on the nature of the seizures. Thus, infantile spasms in the EEG are characterized by irregular high-voltage fluctuations, single and multiple peaks and sharp waves. For larger attacks, symmetrical, intensifying complexes of slow waves are more typical. To identify hidden convulsive readiness, “EEG activation” is performed using hyperventilation, rhythmic light and sound stimulation. In convulsive syndrome, unlike epilepsy, electroencephalographic changes in the interictal period may be inconsistent, which is of great diagnostic importance. In early childhood, identifying signs on the EEG that reflect the convulsive readiness of the brain is difficult due to the instability and unclear picture of biopotentials due to the immaturity of the central nervous system. Therefore, in this period, the main role in diagnosis is given to a thorough wedge and examination of the patient.
S.'s treatment should be carried out in parallel with the treatment of the underlying disease. The choice of anticonvulsants (see) is made based on the patient’s condition and the structure of convulsive seizures. When prescribing drugs, take into account the patient’s age, his weight, and the time of occurrence of attacks (night, daytime).
Treatment begins with small doses of drugs, gradually increasing them to the minimum effective dose. The main anticonvulsant is phenobarbital. For generalized convulsive seizures, hexamidine, diphenine, benzonal, and chloracone can also be used. For frequent attacks, a combination of these drugs is used with tranquilizers (diazepam, chlordiazepoxide, thioridazine, etc.), borax, caffeine, papaverine, belladonna extract, calcium gluconate, etc. For focal cortical seizures, as well as clonic generalized seizures, benzonal or its combination with other anticonvulsants. For small propulsive seizures, suxilep, pycnolepsin, nitrazepam (radedorm), diazepam (seduxen), etc. are used. Hormonal drugs (ACTH, hydrocortisone, prednisolone, dexamethasone) have a good anticonvulsant effect in these forms of paroxysms. S.'s treatment should be carried out for a long time: after the complete disappearance of attacks, anticonvulsant treatment is continued for at least two years. When discontinuing medications, it is important to take into account EEG indicators. Unjustified interruptions in treatment are unacceptable, since sudden withdrawal of anticonvulsants can lead to the development of status epilepticus. It is not recommended to reduce the dose of medications during somatic or infectious diseases. When treating S., along with anticonvulsants, dehydration therapy should be periodically prescribed (see) - diacarb, glycerol, magnesium sulfate, lasix. With long-term use of anticonvulsants, strict monitoring of the patient's general condition and an EEG is necessary.
S. in newborns are an indication for emergency treatment measures, since they can quickly lead to cerebral edema and inhibition of vital body functions. Due to the fact that S. in newborns is most often caused by metabolic disorders, stopping them until the etiol is clarified. factor should be started with parenteral administration of 10-20% glucose solution, 10% calcium gluconate solution, 25% magnesium sulfate solution until C stops. If the introduction of metabolites does not give the desired effect, anticonvulsants are administered - diazepam, 2. 5% solution of aminazine or its combination with a solution of pipolfen and 0.5% solution of novocaine. After the seizures are relieved, they switch to maintenance therapy with phenobarbital and take all necessary measures to make an etiological diagnosis. For febrile convulsions in the acute period, along with antipyretic drugs, it is necessary to prescribe anticonvulsants and dehydrating drugs according to the body weight and age of the child. The question of the advisability of prescribing anticonvulsants after the first febrile seizure in order to prevent repeated seizures and the transformation of febrile seizures into epilepsy should be decided individually depending on the age of the child, his premorbid state, the nature and duration of the seizure, and changes in the EEG. If a child experiences a second seizure that is not associated with hyperthermia, he should be treated for a long time, as if he were a patient with epilepsy.
The prognosis depends on the causes of the seizures, the age of the patient, the nature of the attacks and the effectiveness of treatment. S., arising against the background of organic damage to the nervous system, usually tend to progress. They become polymorphic, become more frequent and always worsen the course of the underlying disease. The prognosis is unfavorable with frequent generalized, prolonged focal seizures and convulsive status. Early differentiated treatment and successful selection of equivalent drug ratios lead to long-term remissions and improve the prognosis.
See also Spasm.
Bibliography:
Badalyan L. O., Zhurba L. T. and Vsevolozhskaya N. M. Guide to neurology of early childhood, p. 417, Kyiv, 1980; Boldyrev A. I. Epilepsy in adults, M., 1971; aka, Epileptic syndromes, M., 1976; Gastaut M. Terminological dictionary of epilepsy, trans. from English, part 1, M., 1975; Grigoryan V. 3. On the pathogenesis of convulsive seizures, Zhurn. let's experiment and wedge, med., vol. 12, no. 5, p. 3, 1972, bibliogr.; Davidenkov S.N. Clinical lectures on nervous diseases, V. 2, p. 5, L., 1956; Dolina S. A. and Arshavsky A. A. Modern ideas about the mechanisms of development and cessation of a convulsive seizure, Usp. physiol. Sciences, vol. 6, no. 2, p. 56, 1975, bibliogr.; Dyachkova A. Ya. On the biochemical essence of the process of excitation and development of seizures, Zhurn. neuropath, and psychiatrist., t. 72, no. 2, p. 161, 1972; Ermakova I. A. Level of osmotic pressure of blood plasma and cerebrospinal fluid during convulsive conditions in children, Pediatrics, No. 6, p. 59, 1971; Karlov V. A. Lectures on epilepsy, M., 1976; Kruglikov R.I., Myslobodsky M.S. and Ezrokhi V.L. Convulsive activity, M., 1970; Okudzhava V. M. Basic neurophysiological mechanisms of epileptic activity, Tbilisi, 1969; Propper N.I. Physiological mechanism of a convulsive seizure, Arch. biol. Sciences, vol. 38, no. 1, p. 49, 1935; Shelikhov V.N. Electro-physiological study of the role of subcortical formations in the generalization of excitation in the cerebral cortex, Zhurn. neuropath, and psychiatrist., t. 60, No. 2, p. 145, 1960; Edi M. J. and Tyrer J. Anticonvulsant therapy, trans. from English, M., 1983; Advances in epileptology, 1977, ed. by H. Meinardi a. AJ Rowan, Amsterdam, 1978; Brain WR Brain's diseases of the nervous system, Oxford, 1977; Dennis J. Neonatal convulsions, Aetiology, late neonatal status and long-term outcome, Develop. Med. Child. Neurol., v. 20, p. 143, 1978; Epilepsy, hrsg. v. H. Doose u. G. Gross-Selbeck, Stuttgart, 1979; Freeman JM Febrile seizures, an end to confusion, Pediatrics, v. 61, p. 806, 1978; Heilman K. M. Handbook for differential diagnosis of neurologic signs and symptoms, NY, 1977; Lacy JR a. Penry JK Infantile spasms, NY, 1976; Rabending G. ua Epilepsien, Lpz., 1981; Rodin EA The prognosis of patients with epilepsy, Springfield, 1968.
L. O. Badalyan, E. L. Golubeva (pat., physics).,
Forecast
The prognosis for epilepsy if you follow medical recommendations and take medications in a timely manner is favorable.
To do this, it is important for a person to maintain a careful attitude towards his health: maintain a daily routine, have adequate sleep, avoid overexertion, and completely give up bad habits such as cigarettes and alcohol. Loss of ability to work depends on the frequency of attacks: if they are episodic and occur at night, then there are no contraindications to performing work functions. Daytime attacks with loss of consciousness cause limited choice of work.
In most clinics, patients with epilepsy are seen by neurologists or psychotherapists, who sometimes find it difficult to understand the details of diagnosis and the intricacies of treatment of this disease. Just one EEG requires enormous experience and skills of a professional. Therefore, the Yusupov Hospital employs highly specialized epileptologists who can answer all your questions. You can make an appointment with them by calling the Yusupov Hospital.
Make an appointment