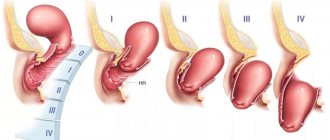
Types of pelvic organ prolapse in women
Lateral anterior prolapse
- if the leading point of prolapse is the anterior wall of the vagina with the posterior wall of the bladder (cystocele).
Lateral posterior prolapse
- if the posterior wall of the vagina or the anterior wall of the rectum predominates.
Central or apical prolapse
- predominance of cervical prolapse, sagging of the vaginal vault.
When the uterus is removed and there is prolapse or sagging of intestinal loops through the vaginal stump, they speak of enterocele
as a variant of apical or central prolapse.
These terms are relative, but the definition of the predominant compartment is important when choosing the type of treatment.
The boundary of the exit of organs beyond the pelvis is the plane of the hymen or hymen. To understand how prolapse occurs, you need to understand the normal anatomy and mechanisms that keep the vagina in good condition.
Possible complications
What is the threat of the disease? If treatment in elderly women and women of childbearing age is not carried out in a timely manner, the consequences may be as follows:
- ulcers of the cervix and the vagina itself, as well as severe swelling;
- endocervitis;
- contact bleeding;
- increased risk of possible infection;
- ulceration or strangulation of a prolapsed part from the vaginal canal;
- development of varicose veins;
- bedsores directly on the vaginal walls;
- the occurrence of cystitis;
- strangulation in the area of intestinal loops;
- blood stagnation;
- the occurrence of endometriosis, which can smoothly lead to infertility;
- tissue necrosis and infection of the body with toxins.
Therefore, illness after childbirth or for a number of other reasons requires immediate treatment.
Anatomy of the pelvic organs in women
Anatomical support for the pelvic organs in women is provided by the interaction between the pelvic floor muscles and the connective tissue fascia and ligaments connecting the pelvic bones to the organs. Together, these muscles and ligaments provide stable support to the pelvic organs while maintaining elasticity. Also a powerful stabilizing factor is the complex of the uterosacral and cardinal ligaments of the uterus.
DeLancey Pelvic Support Levels:
First level
- this is the supporting apparatus of the uterus in the form of the uterosacral and cardinal ligaments, fixing the uterus and the upper third of the vagina to the sacrum and the lateral wall of the pelvis. They allow the uterus to be held upright. The destruction of these ligaments, for example, as a result of traumatic childbirth, leads to prolapse of the cervix, and then the entire uterus, along with the upper third of the vagina.
Second level
support - a complex of fascial structures lateral to the vagina or located along the length of the vagina and passing to the levators and the white line of the fascia of the pelvis. Damage to these structures leads to prolapse of the bladder and anterior vaginal wall.
Third level
– the body of the perineum, including the superficial and deep muscles of the perineum, supporting the distal third of the vagina. Damage to these structures anteriorly leads to hypermobility of the urethra, and posteriorly to a rectocele or prolapse of the posterior vaginal wall with the anterior wall of the rectum.
The innervation of the supporting apparatus through the spinal cord is important. Certain nerve fibers form the pudendal or pudendal nerve. The upper bundles of the pudendal nerve supply the levators, pubococcygeus muscle, and urogenital diaphragm, and below the pudendal nerve itself innervates the anal sphincter.
Diagnosis of uterine prolapse
If uterine prolapse is detected during a gynecological examination, specialists may prescribe plastic surgery. This expands the range of diagnostic procedures, so you additionally need to undergo:
- Excretory urography.
- Ultrasound or genital organs.
- Culture and general urine analysis.
- Curettage of the uterus.
Additionally, smears are taken to check microflora and look for infections in the vagina. To exclude rectocele, an examination by a proctologist and urologist is prescribed. Differential diagnosis is required to exclude neoplasms and uterine inversion.
Risk factors for developing prolapse
Risk factors for pelvic organ prolapse in women include vaginal births and number of births, age and obesity. Risk factors for recurrence of prolapse after surgical correction include damage to the levator ani muscles, treatment of advanced forms of prolapse, and familial forms of the disease.
Number of births
The risk of prolapse increases with the number of vaginal births in history.
The Oxford Family Planning study, which followed more than 17,000 women for 17 years, found that compared with nulliparous women, the risk of hospitalization for prolapse increased markedly after the first (4-fold) and second (8-fold) birth. and then it grew more slowly: after the third birth by 9 times, the fourth by 10 times, and so on.
Factors associated with labor and the development of prolapse include high fetal birth weight, prolonged second stage of labor, and maternal age less than 25 years at first birth. However, vaginal prolapse can also occur in nulliparous women.
Elderly age
The risk of developing prolapse increases with age.
In the Women's Health Initiative study (more than 27,000 women), there was a small but statistically significant progressive increase in the prevalence of rectocele with age (50 to 59 versus 60 to 69 and 70 to 79 years).
Obesity
Women who are overweight (BMI ≥25–29.9 kg/m2) and obese (BMI ≥30 kg/m2) have an increased risk of developing prolapse compared to their normal-weight counterparts. However, whether weight loss leads to regression of prolapse remains controversial, but there are reports of regression of prolapse in women after bariatric surgery.
Hysterectomy
The role of hysterectomy in the development of subsequent pelvic organ prolapse is controversial. The risk may depend on age, presence of prolapse before hysterectomy, and surgical approach.
Retrosymphyseal urethropexy or "suspension" procedure
(fixation of the uterus to the posterior surface of the symphysis pubis) can lead to a greater anterior deviation of the anterior vaginal wall, which changes the distribution of force along all vaginal walls. As a result, the apex and posterior wall of the vagina may become prone to the development of support defects, including enterocele or rectocele.
Increased intra-abdominal pressure
Chronic constipation and other conditions that cause repeated increases in intra-abdominal pressure, such as chronic obstructive pulmonary disease, can stretch and damage the pudendal nerve.
There is currently no reliable data regarding whether the risk of prolapse is increased in women who lift weights. One study of more than 1,000 women found that women doing physically demanding jobs had significantly more severe prolapses than other categories of women.
Connective tissue pathology
Some connective tissue diseases (eg, Ehlers-Danlos syndrome) or congenital abnormalities (eg, bladder exstrophy) contribute to the development of prolapse. Women with hypermobile joints have a higher prevalence of prolapse than women with normal joint mobility.
Family history
Potential genes and patterns of inheritance are unknown. Most likely, we are talking about connective tissue dysplasia as the cause of prolapse.
Causes
The main cause of pelvic organ prolapse is damage to the supporting apparatus of the pelvic floor. The main elements of the latter are ligaments and fascia, which intertwine the pelvic organs and fix (suspend) them to the walls of the pelvis. This can be compared to the lines of a parachute. The pelvic muscles and perineum act as support for the ligaments and fascia.
That is why at a young age, with preserved muscle tone, pelvic organ prolapse is quite rare, while at the same time, after 50 years, every second woman suffers from it. At the moment, there is no consensus on the cause of the development of this disease; most likely, like most pathologies, it has a multifactorial nature. However, the following main reasons can be identified:
- Pregnancy and childbirth. During this period, the qualitative composition of the pelvic floor tissues changes - they become more elastic and stretchable. In some patients, unfortunately, restoration of the previous properties of ligaments and fascia does not occur. On the other hand, during childbirth, some of the fascia, ligaments and muscles are damaged. This is especially true in the case of complicated births (large fetus, rapid labor, episiotomy (perineal incision), use of obstetric forceps, vacuum, etc. during childbirth).
- Hard physical work. Here a process similar to childbirth develops - the supporting structures of the pelvis simply cannot withstand the load and tear.
- Chronic constipation, respiratory diseases (accompanied by constant cough). This also includes obesity, which is also accompanied by increased loads on the ligamentous apparatus of the pelvic floor.
- Of course, hereditary weakness of connective tissue also contributes. Often such women have concomitant diseases such as hemorrhoids, varicose veins of the lower extremities, and pathology of the musculoskeletal system.
| Most patients receive care for free (without hidden additional payments for “network”, etc.) as part of compulsory health insurance ( under the compulsory medical insurance policy ). | Application for treatment under compulsory medical insurance |
Symptoms of pelvic organ prolapse in women
- sensation of a foreign body and heaviness in the perineum, discomfort in the vagina
- urination disorders (cystocele and urethrocele): frequent urination, lack of satisfaction with the act of urination, urge to urinate, urinary incontinence when coughing and any exertion, etc.
- disorders of defecation and stool (rectocele, enterocele, sigmoidocele, perineocele, rectal prolapse): fecal incontinence, rectal bleeding.
- sexual dysfunction.
Low back or pelvic pain is often associated with prolapse, but studies have not confirmed this association.
Symptoms of prolapse are often related to body position: they are less noticeable in the morning or when lying on the back and worsen during the day when women are active and upright.
Many women with prolapse have no symptoms and treatment is usually not indicated. Some women themselves see the protrusion of organs beyond the genital opening.
Symptoms
Symptoms of the disease directly depend on the organ that was involved in the pathological process. Taking this fact into account, the following symptom complexes can be identified:
- Associated with bladder prolapse: Difficulty urinating, feeling of incomplete emptying of the bladder, frequent urination, urination in small portions, sudden (imperative) urge to urinate, loss of urine due to physical activity or urgency
- Associated with rectal prolapse: difficulty defecating, the need to help with your hand (press on the prolapsed vaginal walls) during defecation.
- Associated with uterine prolapse: nagging pain in the lower abdomen, discomfort during sexual intercourse.
At the same time, the main symptom characteristic of all patients and leading them to the doctor is the feeling of a foreign body in the vagina. Moreover, most patients have a violation of the support of several organs at once, and therefore the clinical picture may be more multifaceted than described above.
| anonymously to the doctor, through the feedback form, we will try to help you. | Ask a Question |
Treatment
Treatment is indicated for women with symptoms of prolapse or symptoms accompanying prolapse (impaired urination and bowel movements or sexual dysfunction).
Establishing the patient's goals is central to determining treatment tactics. The method is selected individually in accordance with the symptoms and their impact on the quality of life. It is important to set realistic expectations, taking into account comorbid medical conditions that influence the perception of symptoms.
The choice of therapy depends on the woman's preferences, as well as her ability to comply with recommended conservative therapy (usually exercise) or undergo surgery.
Watchful waiting is a suitable option for women who are not very concerned about their symptoms and can wait until they decide to undergo surgery. However, patients with grade 3 or 4 prolapse are at risk of additional problems with urination and bowel movements, and therefore regular monitoring is recommended.
Vaginal pessaries
The main alternative to prolapse surgery is the use of vaginal pessaries.
Pessaries are silicone devices of various shapes and sizes that support the pelvic organs. Pessaries should be removed and cleaned regularly.
Pelvic floor muscle training (Kegel exercises).
Randomized trials have demonstrated the benefits of such exercises, especially when individually taught and/or supervised. Therefore, biofeedback therapy has become widespread. The lower the degree of prolapse, the more effective the training programs are.
Estrogen therapy
There are no data to support the use of systemic or topical estrogen as primary therapy for prolapse. At the same time, the introduction of estrogen into the vagina in the perioperative period increases the production of mature collagen, increases the thickness of the vaginal wall and reduces the activity of degradative enzymes.
Surgery
Candidates for surgical treatment are women with symptoms of prolapse who cannot perform conservative measures or consciously refuse them.
Surgeries for pelvic organ prolapse are performed through vaginal and abdominal approaches using local tissues and synthetic materials.
The choice of surgical approach depends on the severity of symptoms, the extent of the prolapse, the experience of the surgeon, and the patient's expectations. One of the problems with prolapse surgery is the recurrence rate. The risk of re-surgery when using local tissues, according to various sources, reaches 30%. Therefore, technologies using synthetic prostheses have found wide application
Sacrocolpopexy and strengthening of the middle third of the urethra are methods that have proven effective when using mesh materials. Other technologies, especially the use of synthetic materials through vaginal access, are controversial and even “forbidden” in different countries.
Thus, the use of local tissues and a suburethral sling for vaginal access, as well as sacrocolpopexy and Burch’s operation (fixation of the anterior vaginal wall to the Cooper ligament of the pubic bone through access to the space of Retzius) for abdominal access are considered today as operations that have proven their validity in accordance with with clinical international recommendations.
Operation
Of course, they will not replace damaged ligaments and fascia. Surgical treatment for severe forms of prolapse is the only effective treatment method. The most popular, studied and natural operations are those performed through the vagina. In this case, it is possible to restore all parts of the pelvic floor and achieve excellent cosmetic results with minimal risks for the patient.
hybrid techniques have become widespread.
, which allow you to restore the natural anatomy of the pelvic floor through a combination of organ-preserving techniques, maximum use of the patient’s own tissues and targeted/targeted use of synthetic materials in the busiest areas.
Prevention of prolapse
Strategies for preventing prolapse and its progression have not been sufficiently studied. There is evidence that the following can help prevent prolapse:
- vaginal pessary,
- weight loss,
- treatment of chronic constipation,
- refusal of hard physical work,
- estrogens or drugs with estrogenic effects alone or in combination with other treatments,
- postpartum rehabilitation.
Although vaginal birth is associated with an increased risk of prolapse, it is not clear whether a cesarean section will prevent it from occurring.
Postpartum rehabilitation to restore muscle tone, the use of exercise equipment, biofeedback therapy for minimal degrees of prolapse, preventive mini-surgical vaginal plastic surgery are procedures aimed not only at the aesthetic restoration of the perineum, but also to prevent the progression of prolapse and the need for more complex surgical interventions in case of relapses.
What tests need to be done to diagnose prolapse?
The doctor evaluates the type and stage of prolapse during a gynecological visit, conducting an examination in a gynecological chair, and also taking into account your complaints, which are sometimes enough to plan treatment. During the exam, your doctor may ask you to tense your abdomen and cough to assess the extent of the prolapse and evaluate what treatment to offer. Depending on the patient’s age and complaints, the following may be performed: oncocytological examination, ultrasonography, aspiration biopsy of the uterine cavity. If complaints are related to defecation disorders, then the doctor may prescribe defecography to assess the condition of the intestine and rule out a possible proctological disease.