Trichomoniasis, also known as trichomoniasis or trichomonas urogenital infection, all terms are absolutely equal. It is a well-known sexually transmitted infection, which people are not very afraid of contracting, and there is an explanation for this - it is easily treated. But this is still a sexually transmitted infection, and like all infections of this localization, it can cause inflammation of the organs responsible for reproductive capabilities, and under unfavorable clinical circumstances, lead to infertility.
Trichomoniasis (trichomoniasis) is a sexually transmitted disease, and according to the law, you cannot obtain a medical certificate without testing for this infection. If you have ever had sex without a condom, you may have trichomoniasis. The fact is that in the vast majority of women it does not manifest itself in any way.
Among all those suffering from sexually transmitted infections, every tenth person suffers from trichomoniasis, and often other urogenital infections coexist with it. It is estimated that a little more than 150 million people in the world suffer from trichomonas infection every year; in Russia, in every thousand adult citizens there is one patient with trichomoniasis, and in recent years the incidence has been decreasing. True, no one can guarantee that this frequency of the disease corresponds to reality, because no more than half of those suffering from trichomoniasis come to doctors. The other half does not even suspect that they have the simplest microorganism Trichomonas vaginalis.
When did trichomoniasis appear?
The first to see Trichomonas 180 years ago was the French professor of microscopy at the Paris College de France, Alfred Francois Donnet, who studied human secretions. He found Trichomonas in the genital secretions of women in the half-world. Moreover, Trichomonas in one organism could peacefully coexist with syphilis and gonorrhea. Professor Donne did not know that it was Trichomonas; it was an unknown organism with no name yet. Two years later, the German zoologist Christian Gottfried Ehrenberg, whose life’s work was the simplest ciliates, for which he even traveled to Siberia, established the nature of vaginal “living creatures” - the simplest of the class of ciliates and gave its name. We stopped there, deciding that, like most ciliates, this one is also quite harmless, lives in the vagina and absorbs everything unnecessary.
So three and a half decades passed until the Russian obstetrician Ivan Pavlovich Lazarevich compared the frequent detection of Trichomonas with inflammation of the mucous membranes of the genital tract, identifying the microorganism as a possible culprit of the pathological process. But there was little interest in Trichomonas; worldwide recognition as a natural representative of the normal vaginal flora came to Trichomonas only in 1916, exactly 70 years after its first “publication.” Another 20 years later, again, our compatriots realized that Trichomonas is not a purely female microorganism, but a universal one, because they found it in the secretion of the prostate gland and even in the blood. However, it was only before World War II that Trichomonas was recognized as pathogenic—harmful to humans. And after another two decades they wondered how they became infected with it, whether it came from dirty water.
Treatment
Source: jarmoluk/Pixabay
A dermatologist-venerologist deals with the treatment of trichomoniasis in men. Before starting treatment for trichomoniasis, it is recommended:
- Confirmation of the diagnosis by laboratory methods and examination for all possible STIs.
- Examination of all sexual partners to sanitize them and determine the possible period of infection.
Drug treatment
To treat trichomoniasis, drugs are used that kill protozoa. These include drugs of the nitroimidazole group and its derivatives (ornidazole, tinidazole).
In the case of mixed sexually transmitted infections, combined therapy is carried out with nitroimidazoles and sensitive antibiotics or sequential treatment with antitrichomonas drugs, then with antibacterial drugs.
Medicines are usually taken in the form of tablets, but in severe complicated cases of trichomoniasis, the doctor may prescribe intravenous medications.
In addition to anti-trichomonas drugs, in the presence of complications in men, symptomatic drugs are used. For example, non-steroidal anti-inflammatory drugs in the treatment of epididymitis, alpha-blockers and muscle relaxants in the treatment of prostatitis.
Important! The combination of taking anti-trichomonas drugs with alcoholic beverages is unacceptable due to the risk of developing undesirable reactions: nausea, vomiting, headache, tachycardia, drop in blood pressure.
At the present stage, systemic enzyme therapy, immunomodulatory therapy and therapy with local antiseptic drugs are not recommended.
Physiotherapy
Physiotherapeutic techniques and folk remedies are not used in the treatment of trichomoniasis, since there is no evidence of their effectiveness. At the slightest suspicion of the possibility of infection, it is important not to waste time and contact a specialist.
ethnoscience
Products in this category are ineffective. Any ways to get rid of trichomoniasis using poultices, homemade ointments, spells and other traditional medicine will not lead to a cure, and can only worsen the situation. If you have trichomoniasis, you should consult a doctor.
Where does Trichomonas come from?
At the end of the fifties of the last century, several international conferences were held to discuss where Trichomonas comes from in the reproductive tract. They decided that this single-celled organism can be obtained not only through sexual contact, but also from a bath bench or basin, and even from swimming pool water and just tap water, not to mention wells. Bath accessories were blamed because trichomoniasis was practically not detected in men due to the absence of clinical symptoms. If a woman complains of inflammation, and a man is fine, then apparently the woman “caught the infection” somewhere else.
Where can a decent and faithful woman become infected with a sexually transmitted infection? Of course, in a public bath, where she is completely defenseless. And at that time, personal bathrooms were very rare; citizens went to the baths to wash themselves. Another five-year-old mankind was convinced that Trichomonas brought into a family was not at all a consequence of the infidelity of one of the spouses, but evidence of a woman’s failure to observe personal hygiene. One good thing is that this misconception helped save the family, because the infection happened through “non-sexual” means.
But in the mid-60s, scientific proof of the extremely poor survival of Trichomonas outside the human body came from Soviet Estonia, therefore infection by any other method other than sexual intercourse is simply unrealistic. Trichomonas does not like sunlight and hot water, and is immediately killed by any antiseptic. Indeed, Trichomonas is so delicate, so demanding of the external environment that even in the secretion of the genital tract collected for the purpose of research, it often dies before it is brought to the microscope. Since that time, the disease caused by Trichomonas vaginalis has been recognized as a venereal disease.
The main route of transmission of Trichomonas in adults, of course, is sexual, but oral sex does not contribute to infection, in any case, they could not prove this possibility of transmission. A woman in labor with trichomoniasis can infect her child, more often this happens to girls. This route of transmission of infection is called vertical. And today, 2–17% of newborns have trichomonas vaginitis or, in the old way, colpitis inherited from their mother. It is quite possible, because tests are taken from pregnant women several weeks before giving birth.
At risk for trichomoniasis are citizens who have multiple sexual partners, workers in the illegal sex industry, drug addicts and HIV-infected people, socially disadvantaged people, in general, comrades. True, citizens are still actively using the idea of contracting trichomoniasis in the pool, the main thing is to get treatment, and let them decide for themselves how to explain the appearance of Trichomonas vaginalis to their partner.
Diet and restrictions
Also, while taking medications, the specialist will recommend a diet and introduce some restrictions. In particular, recommendations may be of the following nature:
- Eliminate fried, fatty, spicy foods from the diet;
- Add fermented milk products that help restore lactobacilli;
- Strictly refrain from intimacy, since during treatment the flora is most vulnerable and there is a risk of getting an additional infection or fungus.
Following these recommendations will speed up treatment and achieve the best result with minimal discomfort to the body.
Symptoms of trichomoniasis
Trichomoniasis can often be completely asymptomatic, and this is especially true for men. For life, Trichomonas vaginalis chooses the flat epithelium of the reproductive tract and urinary tract - the urethra; in 90% there is a combined lesion of the urethra and genitals, and only five out of a hundred have an isolated lesion of the urethra.
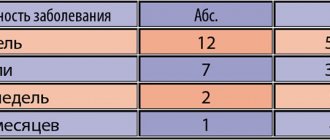
The infection does not appear immediately after infection, but on average after two weeks, although there are known cases of a very short, literally 2 days, and quite long incubation period. The disease in women usually manifests itself acutely with the appearance of copious cloudy and foamy discharge with an unpleasant odor, which is accompanied by itching in the vagina or urethra. The acute period lasts a week or two, after which the discharge of the previous nature is not so abundant. Men complain of itching and burning in the urethra.
If left untreated, the process may involve the mucous membranes of the external genitalia, where itchy red spots appear, sometimes with the absence of the surface layer of the epithelium - erosion. Sexual intercourse may be accompanied by pain, and there may be pain in the urethra when urinating. Gynecologists see swelling and redness of the mucous membrane, and hemorrhages on the cervix, and the cervical mucosa itself is very similar to a ripe strawberry. But such a clinical picture occurs only in some of the infected, while others peacefully coexist with Trichomonas, which is called carriage.
Case from practice
At the beginning of my medical career, I worked in a antenatal clinic as a pediatric gynecologist. The youngest patient who was brought to me to be treated for trichomonas colpitis was a 5-year-old girl! Her parents were in a pre-divorce situation and each led their own personal lives. But the girl slept in the same bed with her mother - and this was enough for the child to get such an unpleasant infection!
Trichomoniasis is a multifocal disease. The main site of Trichomonas parasitism is the vagina, but they also penetrate the urethra, bladder and even the upper urinary tract - the ureters.
Is this a peaceful carrier?
Why someone develops violent symptoms of damage to the genital tract by Trichomonas, and someone does not even suspect that the protozoa is present, cannot be said with certainty. Most likely, this is due to both the ciliate strain and the characteristics of the host. But in men this state of clinical affairs is observed an order of magnitude more often than in women.
It is assumed that the immune response to the introduction of Trichomonas can be very sluggish, because its genes are somewhat similar to red blood cells - erythrocytes. Or perhaps, on the contrary, the local immunity is so strong that it is not capable of completely killing Trichomonas vaginalis, but does not allow it to go away, not allowing it to actively manifest itself.
However, the absence of clinical symptoms does not make the carrier harmless to a sexual partner; he is the same source of infection as a person who recognizes himself as having a sexually transmitted infection. Trichomonas carriers are dangerous because, not feeling a venereal disease, they do not consider it necessary to limit their sexual behavior. It is to Trichomonas carriers that we owe a fairly significant spread of the disease.
Carriage of Trichomonas allows for much easier infection with other sexually transmitted infections and HIV, since the protective properties of the mucous membrane with trichomoniasis are lower, damage occurs in the mucous membrane of the genital organs, through which other pathogens easily penetrate. There is a suspicion that although Trichomonas itself rarely affects the cervical canal, it increases the likelihood of developing not entirely benign changes in the cervical mucosa - cervical neoplasia.
Anamnesis
During the survey, we find out the connection of the disease with the onset of sexual activity, change of partner, and unprotected sexual intercourse.
When examined with the help of speculum, an abundance of liquid, foamy, pus-like leucorrhoea, hyperemia, swelling of the vaginal mucosa and the vaginal part of the cervix are detected. Inflammatory erosion of the cervix often occurs.
Complications of trichomoniasis include ascending infection of the urinary tract and kidneys (cystitis, pyelitis, pyelonephritis).
Trichomonas can be found in the uterine cavity, fallopian tubes, and ovarian cysts. Trichomoniasis leads to pregnancy complications - early rupture of membranes, premature birth.
Diagnostics
The presence of Trichomonas in the genital tract must be proven by detection under a microscope or by growing it in a special nutrient medium.
They specifically look for Trichomonas vaginalis in women who complain of discharge from the genital tract, with long-term and drug-resistant inflammation of the vaginal mucosa, and, of course, in the risk group. A swab is taken from the genital tract and immediately examined under a microscope. For men, urine or discharge from the penis is tested.
If trichomoniasis is detected, then it is worth checking for other sexually transmitted diseases: it is quite possible that they were transmitted at the same time as trichomoniasis.
Growing the pathogen in a nutrient medium is a more effective method for detecting Trichomonas vaginalis, but even better - 100% results are obtained by polymerase chain reaction - PCR, which detects Trichomonas DNA.
Preventive measures
Prevention of trichomoniasis involves avoiding casual sexual relationships and constant use of barrier contraceptive methods. Men and women should pay close attention to personal hygiene before and after sexual intercourse.
During treatment for trichomoniasis and for three months after completion of the therapeutic course, you must abstain from sexual intercourse. Patients are advised to undergo regular examinations by venereologists and undergo tests when the first signs of genitourinary system infections are detected.
Prevention
Limiting the number of sexual partners and timely checks with a gynecologist is the best way to prevent the development of trichomoniasis or other STIs. It is also important to remember to use a condom.
If you have the slightest suspicion of infection, you should consult a doctor as soon as possible for a full diagnosis and undergo appropriate treatment, strictly following the recommendations of a specialist. An annual preventive examination for STDs will not hurt, even in the absence of complaints and symptoms.
Photo: romanzaiets / freepik.com
About the pathogen
The organism Trichomonas vaginalis is classified as a protozoan. It has a flagellum, so it actively moves. Infection occurs from a sexual partner if personal hygiene rules are not observed. The microorganism lives and multiplies in the urogenital tract, parasitizing the integumentary cells.
The incubation stage ranges from 3 to 28 days. The problem is that often the disease occurs without pronounced symptoms, and when cross-infected, it is masked by the manifestations of other diseases.
Unexpressed symptoms lead to ignoring the onset of the pathology and its transition to a chronic form. Patients often experience exacerbation when their immune system is weakened or after severe stress. Under such conditions, microorganisms begin to multiply intensively and the first symptoms appear.