There is an opinion among people that it is almost impossible to become infected with HIV through oral sex.
This thesis guides teenagers who avoid the risks of vaginal sex.
So are adult men and women, who usually have their own preferences in choosing a method of intercourse.
However, years of research show that unprotected oral sex is not so safe.
HIV is still transmitted through such contacts.
How high is the risk, what does the danger depend on and whether it can be reduced to zero - read below.
Risk factors for HIV transmission
Doctors pay special attention to HIV infection from the moment it is identified.
And at the present stage of development of medicine, a lot of data has already been accumulated regarding this infection.
The asymptomatic carrier stage, which lasts for several years, is the main factor in the spread of the disease.
Three biological fluids are dangerous in terms of infection:
- blood
- sperm
- vaginal discharge
At advanced stages, HIV infection actually transforms into AIDS.
Then the viruses penetrate the salivary glands and appear in saliva, due to which the infectiousness of the sick person increases significantly.
During unprotected oral sex, people actively exchange all these biological fluids with each other.
Therefore, the risk of HIV transmission always exists.
But sometimes it is very high, and sometimes it is negligible.
Health worker - dangers of the profession
All health care workers should be aware of the dangers of various viruses and infections and treat each patient as if they are suspected of being infected with HIV and consider all body fluids to be contaminated with dangerous diseases. In this case, the risk of contracting dangerous diseases will be minimized.
Violation of safety rules in the work of medical personnel can lead to a needle stick and infection with a retrovirus. Hospitals and clinics have special “Anti-AIDS” first aid kits, the contents of which will help staff take the necessary measures in emergency cases. Such a first aid kit should contain:
- Hydrogen peroxide 3%;
- Iodine;
- Ethyl alcohol 70%;
- Albucid 30%;
- Patch;
- Fingertip;
- Scissors.
If a healthcare worker pricks himself with a used needle, he needs to squeeze out the blood from the wound and disinfect it. Then wash your hands well and cover the wound with a bandage.
It is very important to record your injury in the Accident Log. Then it is obligatory to contact the AIDS center for testing to determine whether the person has antibodies to the retrovirus
The test results of health workers are anonymous. The chairman of the commission on nosocomial infections and the head of the medical institution must be informed about injuries and preventive measures taken.
Risky sexual behavior with HIV
In the 20th century, at least 8 clinical studies were conducted to determine how high the likelihood of HIV transmission is through oral sex.
The official figures were shocking.
It turned out that about 7% of new cases of infection occurred precisely through this form of satisfying sexual passion.
And although the mathematically calculated risk of infection for one act alone is approximately 0.04%, it cannot be considered zero.
If only because this is an average over several thousand episodes.
Unfortunately, many people still mistakenly neglect such knowledge.
And they begin to think about the problem only when they learn about their positive status.
Of course, it is possible to help such patients, but it is much better to take into account the risk of infection and danger factors.
There are several of them:
- ejaculation in mouth
- concomitant sexually transmitted diseases (STIs)
- mucosal injuries, ulcers and wounds in the mouth
- weak immune status of the passive partner
- high viral load in the active partner
This applies to this type of contact when oral sex (blowjob or cunnilingus) is provided to an HIV-infected person (man or woman).
In the opposite case, when services are provided by an infected person, there are slightly fewer risk factors:
- bleeding ulcers and wounds in the mouth
- advanced stage of HIV infection - AIDS
- aggressive act with elements of biting
Next, we will consider each risk factor in more detail, since a lot depends on their knowledge.
First of all, it is a chance to maintain health and protect a loved one from infection.
HIV and AIDS - differences, duration of development, forecasts
AIDS is the final stage of HIV, which is characterized by severely reduced immunity. It is important not to confuse these two concepts. From the moment of HIV infection, the disease can develop to the AIDS stage without treatment within 9-11 years (on average). Once diagnosed with AIDS without treatment, life expectancy is short - on average up to 19 months.
If you start treatment on time, you can live a very long life at the HIV stage - the life expectancy of such patients thanks to modern treatment is 20-50 years. And although at the AIDS stage the situation is much more complicated, many patients, with proper treatment and a strong body, can live more than 10 years.
It is obvious that taking therapy is the most important factor for treating HIV and living a full, long life. Moreover, it is treatment that can significantly reduce the viral load and make the infected person harmless to the partner, as well as family members.
Risk of ejaculation
Each episode of oral sex with an HIV-positive man poses a fairly serious risk.
And ejaculation of the inserting partner into the recipient’s mouth increases the risk several times.
And that's why.
The saliva of a healthy person has some protective mechanisms that help inactivate any viruses, including HIV.
This is both the hypotonic nature of saliva and some immunoglobulins contained in this fluid.
However, the virucidal effect is realized too slowly.
And it cannot inactivate all virions that enter the mouth, if there are a lot of them.
This is exactly the case when a man ejaculates into his mouth.
You can't expect that spitting out the sperm rather than swallowing it reduces the risk.
Of course, the longer the seminal fluid stays in the mouth, the greater the danger.
But both of these ways of getting rid of it are imperfect.
Since the biological material of the man remains on the mucous membranes of the mouth.
Human immunodeficiency virus is one of the new infections. Civilization encountered it only half a century ago, and doctors studied the disease it causes from scratch. It is not surprising that myths and irrational fears surrounded HIV infection. Some people in the Soviet Union were even afraid to buy bananas because “they grow in banana groves where Africans with AIDS go to die.”
Since then, our knowledge of HIV has expanded dramatically. Medicine knows everything about the ways of its transmission and has learned to suppress it in the host’s body. Thanks to treatment, people with HIV can live full lives into old age and give birth to healthy children. But many phobias are still alive in society and serve as a source of unnecessary anxiety.
The downside is a frivolous attitude towards HIV. Without thinking about the danger, a person subconsciously denies its existence and ignores reasonable rules - and as a result, he can become infected. Let's see if you were at risk of getting HIV infection!
REMEMBER! Only a medical test can accurately determine your HIV status!
I've only had unprotected sex once in my life. It's not scary, is it?
One penetrative sexual contact with an HIV carrier is enough to become infected. The risk is not 100%: much depends on the viral load in the partner’s body, the type of sex (anal or vaginal), the condition of the mucous membranes and personal susceptibility to the virus. But this is a dangerous lottery! Even after one unprotected contact with a person whose HIV status is not precisely known, it is recommended to get tested for the human immunodeficiency virus - and for other sexually transmitted infections.
I always use a condom, but I still worry. They say they don't always work?
Formally, the condom protects against infections (including HIV) with 98% effectiveness. The remaining 2% is mainly due to errors in its use and “accidents” when the condom breaks or slips. Latex loses its elasticity in cold and high temperatures. To prevent condoms from breaking, it is best to store them at room temperature and not use them after the expiration date. You should not keep them in a cosmetic bag with manicure accessories or in a tool box - sharp objects can damage them through the packaging.
You cannot put on 2 condoms at once - this will cause them to break faster, use one condom twice, use fatty lubricants - they destroy latex (it is better to choose a water-based or silicone-based lubricant). There are different types of condoms for vaginal and anal sex. And, of course, the condom should protect the mucous membranes from contact during the entire sexual intercourse, and not just during ejaculation.
If you use condoms correctly, your protection is close to 100% and there is no reason to worry. However, it is recommended that all sexually active people get tested for HIV annually.
I am a virgin/virgin. Am I taking risks during first sex?
Virginity does not provide any special immunity to HIV. Men at the first sexual intercourse without a condom risk the same as during all subsequent ones, and girls – even more so: possible microtrauma and bleeding of the mucous membranes during defloration (rupture of the hymen) increase the risk of infection.
I take hormonal pills. Am I protected?
Contraceptive hormonal drugs affect the mechanism of egg maturation in the female body and, when taken correctly (a course without skipping), protect against unwanted pregnancy. But they do not provide any protection against HIV or other sexually transmitted infections.
We kissed a guy, but I don’t know his HIV status! Could I have gotten infected?
Even deep wet kisses are completely safe from the HIV point of view. Small wounds in the mouth (for example, due to stomatitis or tooth extraction) do not affect the degree of risk. For HIV transmission, a certain concentration of the virus is required in the biological fluid with which contact occurs. For saliva, the infectious dose is 3 liters, and when kissing, partners exchange a volume of about a teaspoon. In addition, salivary enzymes themselves have a depressing effect on HIV.
But it’s quite possible to get herpes, mononucleosis, human papillomavirus, syphilis and a number of other sexually transmitted infections, not to mention influenza, coronavirus and all types of acute respiratory viral infections through a kiss.
There are rumors that my office colleague is infected with HIV. What to do?
There is nothing to be afraid of. Compared to many other viruses, HIV is less contagious. For example, the flu virus is 3000 times more contagious. HIV is not transmitted either by airborne droplets, or through household contact, or through skin-to-skin contact - only through blood and unprotected sexual contact. In the open air and from sunlight, this virus quickly dies.
People with HIV at home or at work are not dangerous to others. You can shake hands with an HIV-positive colleague, share a table and stationery with him, have lunch together in the cafeteria, drink coffee, hug and dance at corporate parties - all this is not contagious.
People with HIV are members of society like everyone else. Discriminating against them and even disclosing their diagnosis are crimes that can be taken to court.
I used someone else's toothbrush/comb/razor while visiting. Could I have become infected with HIV?
Since HIV is not transmitted either through saliva or through the skin, infection with it through a toothbrush or comb is in principle impossible. With a razor, there is a theoretical chance that the virus will be transferred to the blade if a person with HIV is accidentally cut with it. But in the external environment, the human immunodeficiency virus dies very quickly: even if someone else is then cut with the same razor, he will not get sick.
But these objects are quite capable of transmitting other infections. Through someone else's toothbrush, you can “borrow” caries or gingivitis, herpes or a respiratory infection. Through a comb - ringworm, lice or pustular infections of the scalp. And a razor is dangerous with the risk of transmitting hepatitis B and C. So no one has canceled the sanitary rules: personal hygiene products are intended exclusively for individual use.
I go to the fitness club/swimming pool/sauna/banya. Is there a danger of catching HIV there?
There is no danger. Water quickly inactivates and destroys HIV; chlorinated or soapy water destroys the virus almost instantly. In a pool or bathhouse, no matter what happened there before your arrival, the concentration of the virus that gets into the water in any case will not be sufficient for infection. Sharing exercise equipment or yoga mats is even safer: human skin is an insurmountable barrier to HIV.
I do martial arts, and sometimes I get injured. Can I get HIV from a sparring partner's blood?
Let's say your sparring partner is HIV positive, you both have cuts in your eyebrows and are bleeding. Infection will be possible if infected blood enters the direct bloodstream of a healthy person. To do this, one would have to press the bleeding wounds against each other or rub someone else's blood into the injury. In real life, such a situation is difficult to imagine. Blood containing HIV is not dangerous if it comes into contact with the skin.
Could I get HIV from a mosquito?
No. Neither mosquitoes, nor lice, nor ticks, nor bed bugs, nor other blood-sucking insects are capable of transmitting HIV, otherwise humanity might have died out. Firstly, the bloodsucker’s mouthparts are designed in such a way that it sucks blood through one tube and injects saliva into its victim through another. These channels do not communicate, so there is no chance that a mosquito will inject you with the blood of a previous bite.
Secondly, HIV quickly dies in the mosquito’s intestines. In addition, even if a mosquito worked like a small syringe, it simply would not physically fit the dose of infected blood necessary for infection.
I use drugs, but I always use a personal syringe. I'm safe?
Of course not. Firstly, HIV is transmitted not only through a syringe, but also through an injection mixture that could be prepared in a contaminated container, or which someone could draw with a contaminated syringe before packaging.
Secondly, psychoactive substances - even non-injectable ones - weaken self-control, while increasing sexual desire. This often leads to risky sexual behavior - and therefore increases the chances of contracting HIV through sexual contact. Finally, it is worth recalling that, according to statistics, even without a connection with HIV, the life expectancy of drug addicts is 10-15 years after starting to take drugs.
My partner was diagnosed with HIV. So, am I sick too?
If you have practiced sex without condoms, this is very possible. It all depends on the partner’s viral load, the nature of contacts and personal luck. It is necessary to take an HIV test as soon as possible and repeat it 3 months after the last unprotected sexual intercourse.
A member of my family became infected with HIV. Are we all going to die now?
Not now and not from HIV. Living under the same roof with an HIV-positive person does not pose any danger. Infection with the human immunodeficiency virus in everyday life is impossible. The virus is not transmitted either by airborne droplets, or through bedding, food, dishes, towels, plumbing, touching, kissing - only through blood and sexual contact. Therefore, if we are not talking about spouses, no additional precautions are needed. But your relative now definitely needs psychological support from loved ones.
Concomitant sexually transmitted infections
In modern conditions, HIV (especially at the stage of asymptomatic carriage) often coexists with other pathogenic microorganisms.
In sufficient quantities for infection, pathogens are contained in vaginal discharge and in droplets of prostatic secretion, which serves as a male analogue of lubricant.
Pathogenic microorganisms, such as Trichomonas, gonococci, Treponema pallidum, or herpes virus, greatly reduce the protective properties of saliva.
Plus - they violate the integrity of the mucous membrane of the oral cavity and ENT organs.
This weakening of viral defenses greatly facilitates the invasion of HIV into the capillaries.
And syphilis and herpes generally create open gates in the form of ulcers and chancre.
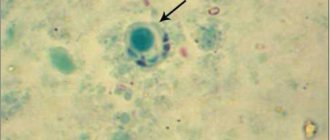
The nature of HIV
The human immunodeficiency virus belongs to the group of retroviruses; it causes a slowly developing pathology - HIV infection. HIV attacks the cells of the immune system, causing it to stop functioning. Acquired immunodeficiency syndrome also progresses, and this leads to the fact that all organs and systems become defenseless against infections and malignant neoplasms.
The virus has a characteristic feature - it can remain in the human body for decades and still not be detected. But at the same time, it poses a huge danger to a healthy sexual partner; the possibility of infection is very high.
The immune system of healthy people is able to repel attacks from pathogenic microorganisms, and the presence of HIV has a depressing effect on its functioning. Therefore, if the virus is undetected, and, consequently, there is no treatment, it develops and at the last stage leads to AIDS.
Sores in the mouth
Sometimes host partners do not take into account such an obvious risk factor as open wound surfaces.
They are usually associated with recent oral and ENT interventions and irritant phenomena:
- dental procedures – tooth extraction, gum dissection
- periodontal disease - in the acute stage or even at the treatment stage
- piercing, which is now so popular among young people
- ENT surgeries , for example - removal of tonsils (tonsillectomy)
- cocaine use , smoking and vaping
There are also more rare variants, for example - a tumor, tuberculous rashes.
Even when there is no blood in the saliva, you should not consider yourself safe when providing oral sex to an HIV-positive man or woman.
Until the doctor says that all the damage has healed successfully.
Regardless of what caused them.
Can I have children?
Yes. Medicines can reduce the risk of mother-to-child transmission of HIV during pregnancy and childbirth to less than one percent. Before fertilization, the sperm of an HIV-positive donor must be cleared of the virus. The main difference will be that you will need a specialist in HIV, fertilization and childbirth. Recently, doctors have been recommending PrEP to prevent partner infection in couples who are trying to conceive. If you want to adopt a child or obtain guardianship, there are protective measures for HIV-positive parents so that your interests will not be infringed.
Yes. Medicines can reduce the risk of mother-to-child transmission of HIV during pregnancy and childbirth to less than one percent. Before fertilization, the sperm of an HIV-positive donor must be cleared of the virus. The main difference will be that you will need a specialist in HIV, fertilization and childbirth. Recently, doctors have been recommending PrEP to prevent partner infection in couples who are trying to conceive. If you want to adopt a child or obtain guardianship, there are protective measures for HIV-positive parents so that your interests will not be infringed.
Weak immunity of the receiving partner during oral sex
Modern medicine has learned to treat many diseases.
But some of them require the use of a number of drugs that reduce immunity.
For example, hormones and cytostatics for systemic diseases (arthritis, systemic lupus erythematosus, etc.) or after organ transplantation.
In addition to many positive aspects, such drugs have one very negative one - a decrease in immune activity.
As a result, saliva cannot cope with even the smallest amount of HIV and infection occurs.
The progression of infection in such people is also noticeably faster.
The first signs of AIDS appear already one or two years after infection.
Healthy man and infected woman
Is infection possible through oral contact when the woman is sick and the partner is healthy? This very relevant question has two aspects. The first option is when oral caresses are performed by a partner who is a carrier of the virus. In this case, the partner has practically nothing to worry about; the likelihood of infection is negligible. This will only happen if there are open wounds on both the woman’s oral mucosa and the man’s penis.
If oral sex is performed by a man on a woman who is a carrier of the virus, then the likelihood of getting the virus from a man becomes much higher, since it is not released with saliva (in the case of blowjob). But during cunnilingus, a man comes into direct contact with a woman’s vaginal secretions, in which HIV is present in large quantities. But, again, infection will only occur if there are wounds on the mucous membrane of the man’s mouth. If a man does not have injuries to the oral mucosa, the virus will end up in the stomach, where it will die in the acidic environment - gastric juice.
Thus, if a partner is a carrier of HIV, mutual affection is almost safe for a man.
High HIV load in active partner
HIV research shows that the activity and aggressiveness of the infection directly depend on such an indicator as the viral load.
This is the number of copies of the virus in 1 ml of blood, calculated using real-time PCR.
In advanced stages of HIV, the number of virions in the blood and biological fluids becomes very massive.
The contamination of lubricant, semen and vaginal discharge increases.
At the same time, the risk of becoming infected during oral sex also increases.
Life of the virus outside the host
The answer to this question is very important if we want to know whether it is possible to become infected with HIV through oral sex. It is known that the virus lives outside the body for a very short amount of time. What is considered this “outside”? This is primarily without contact with blood. If the situation were different, then it would be possible to become infected through household means. However, this does not happen. Until now, such cases have not been recorded in medical practice.
However, let's take a real example. A syringe with the blood of an infected person, how long can a virus from a needle be dangerous? This depends on a number of factors. Depending on the amount of blood in the syringe and the ambient temperature. Under favorable conditions, it can remain active for up to several days. We will definitely come to the answer to the main question, is it possible to become infected with HIV through oral sex, but first we will make one more digression.
Bleeding ulcers and sores in the mouth
It is not difficult to guess that if an HIV-positive partner has fresh injuries in the mouth or ENT organs, then there will be an admixture of blood in the saliva.
And, accordingly, it contains HIV virions.
In this regard, people who have recently had piercings, had their teeth treated, or had their tonsils removed are dangerous.
That is, everyone we have already listed in the section above.
If the mucous membranes and skin of the giving partner remain intact, then the risk is low.
But when is the surface of the genital organs provoked by inflammation (STI) and other negative phenomena?
Then even a small admixture of blood in the saliva can play a role, causing infection.
Clinical observations show that it is STIs, or rather the inflammation caused by them, that are the main factor reducing resistance to HIV.
Particularly dangerous in this regard are herpetic eruptions and syphilitic ulcers.
They represent an almost open wound surface.
How is HIV diagnosed in Moscow?
There are two tests to diagnose the virus: preliminary ELISA and the most accurate immunoblot. The accuracy of ELISA is about 90%. It is recommended to carry out it 3-6 months after contact with the virus, then it gives maximum accuracy. The usual ELISA test is based on a blood test, but there are also rapid tests that help obtain information based on urine or saliva. Such texts are purchased exclusively at the pharmacy (in no case on the Internet!), since it is necessary to use officially approved products.
If the rapid test gives a positive result, you need to go to an infectious disease specialist yourself. In such a situation, as well as when ELISA in a blood test gives a positive result, the patient is prescribed an immunoblot. Its reliability is already 99.9%. Depending on the diagnosis, the diagnosis is made either on the basis of two repeated tests or a combination of both. The analysis is rechecked and only after this a diagnosis can be made. This is necessary in order to exclude false positive results that may occur during the diagnostic process.
Important: the test does not show how HIV is transmitted in a particular situation - that is, you can determine the route of infection only by analyzing your own actions.
Advanced stage of HIV infection and oral sex
In people with a long history of infection and/or active replication of the virus in the blood, sooner or later it begins to be detected in all biological fluids.
Including in saliva.
By this time, immunity is usually so reduced that it is not able to disinfect the oral cavity on its own.
Here we can draw an analogy with a high level of viral load, which will also be true.
Under such conditions, infection can occur even without the presence of open wounds and erosions in the oral cavity.
Naturally, people with wounds on the genitals are at greater risk of becoming infected.
What tests should I take for HIV?
Even if symptoms do not appear, people who do not have a regular sexual partner, as well as those who practice unsafe sex, should be tested.
You can confirm or deny a virus infection in the following ways:
- ELISA (ELISA) test. Basic test to detect the presence of HIV. Based on the detection of antibodies against HIV in blood serum. The information content and sensitivity of the test is 98%.
It takes at least 2 weeks for the body to produce antibodies. Until this time, there is a so-called serological window, when the test gives a negative result, even if the test subject is a carrier of the virus.
- PCR analysis. The test is based on the determination of viral nucleic acids—the virus itself in the body.
Interpretation of the results is carried out with an indication in the analysis: “positive” or “negative”.
A negative test means that there was no HIV infection. No HIV antibodies or viral antigen were detected in the blood sample tested.
A positive test may indicate the presence of a virus, as well as pregnancy or an autoimmune disease. A positive result means the test must be repeated using a confirmatory test called immunoblotting.
Aggressive oral sex with HIV
Perhaps everything is clear here.
Even when the vulva or penis are not damaged and are protected from infection by microdoses of HIV, biting causes these same injuries.
Creating a gateway for infection to enter the blood.
The risk of infection is increased by all manipulations that in one way or another damage the genitals and are practiced in the field of BDSM: pinching, pricking, spanking, squeezing, and so on.
Am I required to disclose information about my diagnosis?
One reason to tell your sexual partners that you have HIV is to protect them from contracting the virus. If you use a condom or your viral load is below detectable levels and your partner is using PrEP, this precaution may seem unnecessary. It may also not be of much importance from a health or interpersonal perspective. However, there is also a legal reason why disclosing this information may be very important. In many states (***as well as in Russia) there are laws requiring information about one’s HIV status, and in some states this obligation applies regardless of whether the partner became HIV-positive as a result of contact or not. You need to be aware of the laws in your state to avoid breaking the law.
HIV during oral sex: risk group
Despite many years of observations and research, the question of how dangerous oral sex is in terms of infection has not yet been settled.
Thus, there are observations that even taking oral contraceptives can increase susceptibility by weakening the cellular component of immunity.
But thanks to such research, it is possible to roughly determine the categories of people who are at greatest risk.
In some cases, the probability of infection with each contact reaches 18%.
The first, obvious factor is that all these people love to perform oral sex.
Not so obvious criteria:
- sex workers , whose existence is stubbornly ignored by the authorities
- truck drivers who, on long flights, prefer to receive oral satisfaction from a woman, in the belief that this will protect them from HIV and other STIs
- serving sentences in places of deprivation of liberty - in men's and women's colonies, oral sex is practiced quite widely, and when a person is released, he may not even suspect that he has become infected with HIV
There are several more narrow layers of people in whose lives oral sex plays an important role.
For example, transgender people, of whom there are a lot in Thailand.
Not only do they actively practice oral sex, but they are also forced to take hormones in connection with gender reassignment operations.
And all this is a very high risk of contracting HIV.
Is there a cure for HIV?
No. There is only one known “cured” patient who continued to live without HIV for more than five years: Timothy Brown, also known as the “Berlin patient.” He was cured as a result of a bone marrow transplant during treatment for cancer. After this case, there were several reports of other people being cured, but these cases were not confirmed by research or did not stand the test of time - the virus reappeared in many people who were considered cured. As David Margolis, head of the End AIDS Research Collaborative, explains, “Timothy Brown is probably cured, which is wonderful. However, approximately 80 million people have been infected worldwide over the last century. So one chance in 80 million is not too much. This is just a proof of principle that treatment is possible. But I don’t want to disappoint expectations and suggest that we look at the process of finding treatment realistically: this will not happen soon.”
Barrier methods
HIV viruses do not pass through the pores of quality latex.
And now there are not only male, but also female condoms.
When the genitals or oral cavity do not even come into contact with each other, this is the best way to prevent HIV and other STIs.
When used correctly, oral sex becomes 100% safe.
Low-quality products and aggressive sex, when the latex of a condom can be damaged by the actions of a partner, can weaken the effectiveness of protection.
Now there are already developments in the use of special polymer sprays.
They create a film on the genitals impenetrable to microorganisms with complete preservation of sensory sensations.
Prevention of infection
Since HIV can be present in the body for decades without showing itself in any way, to avoid infection during oral sex, you should follow simple recommendations from doctors:
- Before oral sexual intercourse, at least two hours should pass after oral hygiene procedures - during this time, unnoticeable bleeding from microcracks stops;
- You should not eat foods that can injure the mucous membranes of the mouth and gums;
- If there is damage to the oral mucosa, sex should be postponed until the wounds are completely scarred;
- With a non-regular sexual partner, sex should only be with a condom.
Additionally, although HIV transmission during oral sex is rare, it is important to use condoms to avoid contracting more common sexually transmitted diseases.
Living together with a carrier of the virus is not dangerous, since its content in saliva, tears, and sweat is low. It has been established that physical affection and ordinary household contact do not lead to transmission of the virus. Infection is caused only by the presence of blood particles in seminal fluid, saliva and urine.
If a person is sexually active with different partners, he should undergo periodic examinations with a doctor. Timely diagnosis will reveal AIDS at an early stage, which will not only allow the patient to receive treatment, but will also protect his loved ones from infection.
Post-prevention of HIV during oral sex
Using safe antiseptics helps increase the chance of not getting infected.
Immediately after the act of oral sex, the sperm must be spat out from the mouth.
Rinse your mouth immediately with one of the oraseptics: chlorhexidine, orasept, miramistin.
Treat the genitals with the same solution: for a man, thoroughly treat the head, the area of the coronary sulcus and the preputial sac.
For women, wash the vulva, labia majora and minora.
Some antiseptics can and should be used by douching - insert 2-10 ml into the vagina.
If such activities are carried out within a few minutes after oral sex, then the likelihood of contracting HIV and other STIs will decrease several times.