Mycoplasma hominis - what does it mean in women?
Mycoplasma hominis is the causative agent of urogenital mycoplasmosis.
In women, this microorganism can cause inflammatory processes in the genitourinary system.
In 1986, Mycoplasma hominis was classified as a sexually transmitted infection.
But in the international classification of diseases there is no diagnosis of mycoplasmosis.
Therefore, an appropriate diagnosis can only be made if:
- Mycoplasma hominis was found in the woman’s genitourinary tract
- there is active inflammation
- no other pathogens have been found that could cause it
In 2006, mycoplasmosis appeared in the WHO etiological classification of sexually transmitted diseases.
True, Mycoplasma hominis was not included in the list of pathogens.
Only Mycoplasma genitalium is listed.
This is due to the fact that M. hominis is less pathogenic and can be present in the urogenital tract for a long time without causing any inflammatory diseases.
Therefore, it belongs to the transient flora.
Features of Mycoplasma hominis:
- has a high prevalence among the sexually active population
- low contagiousness - the risk of transmission of infection during one sexual contact is minimal
- Asymptomatic carriage is common
- cases of self-healing are often observed when Mycoplasma hominis disappears even without treatment, under the influence of the immune system
- the bacterium rarely causes inflammation
- if they occur, then only in the presence of predisposing factors
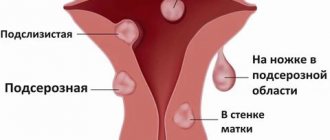
In women, Mycoplasma hominis can cause:
- bacterial vaginosis
- cervicitis
- colpitis
- urethritis
- postpartum endometritis
- post-abortion fever
- puerperal fever
- adnexitis
Very often, mycoplasmas cause pelvic inflammatory diseases.
One study showed that women with PID excreted these bacteria 4 times more often than the average population.
A study to identify the causative agent of urogenital mycoplasmosis (Mycoplasma hominis), during which the genetic material (DNA) of mycoplasmas in a sample of biomaterial is determined using the real-time polymerase chain reaction (RT-PCR) method.
Synonyms Russian
The causative agent of mycoplasmosis, mycoplasma.
English synonyms
M. hominis, DNA.
Research method
Real-time polymerase chain reaction.
What biomaterial can be used for research?
Prostate secretion, the first portion of morning urine, rectal scraping, urogenital scraping.
General information about the study
Mycoplasma hominis (mycoplasma hominis) is a representative of mycoplasmas - microorganisms that can parasitize the membrane of sperm and the epithelium of the mucous membrane of the genitourinary organs. The main route of transmission of mycoplasma is sexual. Infection is possible through the common use of household items, as well as vertical transmission - from a sick mother to a child during pregnancy or childbirth. The source of infection is a patient with mycoplasmosis or an asymptomatic carrier of Mycoplasma hominis.
Mycoplasma hominis is considered an opportunistic microorganism, dangerous to humans only under certain conditions during rapid reproduction. Mycoplasma is often detected in bacterial vaginosis (gardnerellosis). The incubation period is 3-5 weeks. Symptoms of mycoplasma infection are nonspecific and often absent. With decreased immunity, Mycoplasma hominis in women and men can cause inflammatory diseases of the pelvic organs (non-gonococcal urethritis, chronic prostatitis, orchiepididymitis, endometritis, adnexitis, cystitis). For pregnant women, mycoplasma hominis is dangerous due to premature termination of pregnancy, postpartum or post-abortion endometritis, as well as intrauterine infection of the fetus, meningitis and sepsis of newborns.
In addition, when immunity is reduced, Mycoplasma hominis can lead to respiratory diseases.
Mycoplasmosis is often accompanied by diseases caused by opportunistic flora, co-infection with gonococci, trichomonas, ureaplasma, and HIV.
The only way to diagnose Mycoplasma hominis is the polymerase chain reaction method, which allows you to identify the DNA of a specific mycoplasma species in the biomaterial being studied. Its principle is based on a multiple increase in the number of copies of a DNA section specific to a given pathogen.
What is the research used for?
- To establish the cause of inflammatory diseases of the genitourinary or respiratory system.
- For differential diagnosis of diseases that occur with similar symptoms, for example chlamydia, gonorrhea, ureaplasma infection (along with other studies).
- To evaluate the effectiveness of antibacterial therapy.
- For preventive screening examination.
When is the study scheduled?
- If you suspect a mycoplasma infection, including if you frequently change sexual partners.
- For indolent inflammatory diseases of the genitourinary system (especially in the absence of gonococci, chlamydia, trichomonas and Mycoplasma genitalium).
- For respiratory diseases with unknown causes.
- When planning a pregnancy (for both spouses).
- For infertility or miscarriage.
- 1 month after antibiotic therapy.
- For HIV.
What do the results mean?
Reference values: negative.
Positive result
- Detection of M. hominis DNA with symptoms of inflammation and the absence of pathogenic pathogens (gonococci, chlamydia, trichomonas, M. genitalium) indicates the presence of mycoplasma infection.
- If Mycoplasma hominis DNA is detected in small quantities in people without signs of pathology of the genitourinary system, this is regarded as carriage (mycoplasma positivity).
Negative result
- Infection with Mycoplasma hominis is unlikely.
What can influence the result?
- Antibacterial therapy.
Mycoplasma hominis - what does it mean in men?
Scientists first discovered Mycoplasma hominis in 1942 in men with urethritis.
In 1946, it was first suggested that mycoplasmas are one of the main causative agents of inflammatory diseases of the urethra.
In 1981, WHO recognized mycoplasma as the causative agent of urethritis.
Statistics show that every fifth case of inflammation of the urethra in men of non-gonococcal etiology is caused by mycoplasma.
Mycoplasma hominis is highly adhesive.
It can attach to various cells.
Including attaches to the surface of spermatozoa.
Therefore, Mycoplasma hominis is very dangerous for women.
The main task of sperm is to get into the uterus, then into the fallopian tubes, and fertilize the egg there.
Whether there is an egg or not, sperm will still move upward through the woman’s reproductive organs.
Mycoplasmas are attached to them.
Therefore, they can immediately penetrate the uterus and fallopian tubes.
Subsequently, this may result in inflammation of these organs.
In men, Mycoplasma hominis causes:
- urethritis
- chronic prostatitis
Mycoplasma hominis – symptoms of infection, disease, complications
Mykoplazmatyczne infections in women include the cervix and urethra. They are often asymptomatic, which facilitates infection of sexual partners. In women, infection with mycoplasmosis leads to the development of inflammation of the cervix. The most common symptoms of this disease:
- uncharacteristic, cloudy discharge from the genital tract;
- bleeding or spotting that occurs after sexual intercourse and/or between periods;
- frequent urination, accompanied by burning and pain.
Bloody discharge
Mycoplasma hominis
can also lead to the development of bacterial vaginosis. The woman is concerned about the following symptoms:
- copious gray or white vaginal discharge;
- the discharge has an unpleasant odor;
- feeling of discomfort, burning in the urethral area.
Bacterial vaginosis can lead to pelvic inflammatory disease. A woman is worried about pain in the abdominal cavity, which intensifies during sexual intercourse, and is accompanied by fever, nausea, and diarrhea.
With urethritis, a whitish secretion appears from the urethra, frequent urination, accompanied by pain, burning, and itching.
In men, Mycoplasma hominis
leads to the development of inflammation of the urethra.
Symptoms of this infection: pain and burning during urination, unusual discharge from the head of the penis. The infection may be asymptomatic. If left untreated, urethritis can lead to inflammation of the prostate gland and epididymis. Urethritis
In persons with reduced resistance or immunodeficiency (for example, those infected with HIV, after organ transplantation), mycoplasma can lead to bacteremia and the development of reactive arthritis.
Mycoplasmosis is dangerous due to its latent, asymptomatic course, resulting in the development of chronic inflammatory processes in the pelvic organs. Mycoplasma hominis infection
if left untreated, it can lead to inflammation of the ovaries and fallopian tubes; as a result of the chronic inflammatory process, adhesions develop, which is the cause of infertility.
In men, chronic prostatitis, complicated urethritis leads to inflammation of the epididymis (epididymitis). If left untreated, epididymitis may be accompanied by orchitis. Tissue damage, scarring, suppression of testicular secretion occurs, which leads to infertility.
Mycoplasma hominis during pregnancy
Mycoplasma hominis is dangerous for pregnant women.
She calls:
- early spontaneous abortions
- insufficient fetal weight
- chorioamnionitis
- neonatal infection
- postpartum infectious complications (most often endometritis)
In newborns, mycoplasmas can cause:
- pneumonia
- bronchopulmonary dysplasia
- meningitis
- sepsis
Therefore, if Mycoplasma hominis is detected at the stage of pregnancy planning, it is advisable to undergo a course of treatment.
This avoids pregnancy complications.
How is Mycoplasma hominis transmitted?
Mycoplasma hominis has several routes of transmission.
The main one is the sexual route.
The contagiousness of this bacterium is low.
The infection usually occurs in a subclinical form.
Mycoplasma hominis simply lives in the urogenital tract, and for the time being does not bother anyone.
During this period, a person is minimally contagious.
But the risk of transmission increases if Mycoplasma hominis causes inflammation.
Then its population increases.
The bacterium begins to actively release into the external environment.
Only the usual type of sexual contact leads to infection.
During oral or anal sex, the risk of infection is minimal.
Even if the bacterium is isolated from the oral cavity using PCR, it will not live long in the mouth and does not cause pathological symptoms.
Another route of infection is vertical.
Mycoplasma can penetrate fetal tissue in utero.
It also infects the baby during childbirth.
Theoretically, Mycoplasma hominis can be transmitted through household contact.
In practice, such cases have not been registered.
They are unlikely, given the low contagiousness of the infection and the weak stability of the bacterium in the external environment.
Even the likelihood of infection during one-time sex is minimal.
It is almost impossible to get infected from the wall of a public toilet or in a swimming pool.
After infection, an incubation period begins.
It lasts on average 1 month.
Although it can last much longer.
Sometimes symptoms do not appear for several months after infection.
Mycoplasma hominis and genitalium - differences
Mycoplasma genitalium differs from hominis in its higher pathogenicity.
It is the causative agent of urethritis, colpitis, and cervicitis in women.
Associated with pregnancy pathology.
In men, they are common causative agents of non-gonococcal urethritis - approximately 20% of cases.
In women, Mycoplasma genitalium is detected in the presence of signs of inflammatory damage to the pelvic organs in 10% of cases.
The prevalence of Mycoplasma hominis in the population is wider.
This microorganism is less pathogenic.
It does not always cause inflammatory processes.
Often present in the urogenital tract without causing any problems or symptoms.
Although, as populations increase, they can cause inflammation.
Mycoplasma genitalium is found not only in the urogenital tract.
It is also sometimes detected in swabs from the oropharynx.
This confirms that mycoplasma can also be transmitted during oral sex.
But this bacterium does not cause any symptoms in the mouth or respiratory tract.
The Mycoplasma genitalium cell has a terminal organelle.
Thanks to it, it attaches to epithelial cells, as well as red blood cells.
Until 2002, this bacterium was considered the smallest on the planet.
Although today it is Carsonella ruddii, discovered later.
Mycoplasma does not have its own cell wall, so it attaches to other cells.
Antibodies to mycoplasma lgG, Mycoplasma hom. IgG quantity
Antibodies to mycoplasma lgG, Mycoplasma hom. IgG quantitative
— allows you to detect IgG antibodies to the bacteria Mycoplasma hominis.
Mycoplasmas
are a group of intracellular microorganisms - gram-negative bacteria that live on plants and in the body of animals and humans.
There are 16 types of mycoplasmas living in the human body. Of these, 6 species live on the mucous membranes of the genital organs and urinary tract; the remaining 10 species are in the mouth and pharynx. The size of these bacteria is 115–200 nm. They do not have a dense cell wall and are covered with a three-layer cytoplasmic membrane.
Mycoplasma hominis
- a group of mycoplasmas that cause lesions of the urogenital tract in men and women. These are conditionally pathogenic microorganisms, in other words, they are one of the components of the normal bacterial microflora of the mucous membranes of the urinary tract of a healthy person, but when immunity is reduced and a certain threshold concentration of microorganisms is exceeded, they can cause inflammatory diseases of the urogenital tract. Mycoplasmas are characterized by polymorphism and a unique life cycle.
The source of infection is a person with mycoplasmosis or a healthy carrier of mycoplasmas. The infection can be hidden for a long time, or manifest itself under the influence of various factors, for example due to hormonal changes, decreased immunity and the addition of concomitant infections.
Mycoplasma infections of the urogenital tract occupy one of the leading places among STIs. They are often combined with gonococci, trichomonas and opportunistic microorganisms, transmitted through sexual contact, and can cause non-gonococcal urethritis and prostatitis, pelvic inflammatory diseases, pathology of pregnancy and fetus, infertility in women and men, as well as perinatal infection of newborns.
Clinical picture of mycoplasma infection
The clinical manifestations of mycoplasma infection are different, which is associated with the anatomical features of the structure of the female and male genital organs. Men are characterized by the manifestation of urethritis or prostatitis, accompanied by itching, burning and frequent, painful urination. For women - the development of mycoplasma vaginitis or cervicitis, which is manifested by itching, burning, a feeling of discomfort in the lower abdomen and genital area, mucous discharge from the genital tract, pain during sexual intercourse.
Long-term chronic mycoplasma infection can lead to pregnancy pathologies and even infertility. Transmission of the infection from mother to child is also possible - transplacentally during pregnancy or during childbirth. In this case, mycoplasma infection in a newborn manifests itself in the form of meningitis, septicemia and respiratory tract infections.
Antibodies for mycoplasma infection
In response to infection with mycoplasma, the immune system begins to produce a number of specific immunoglobulins: IgA, IgM and IgG.
The production of IgG to Mycoplasma hominis begins approximately 2–4 weeks after infection, and continues for a long time: up to a year or more. The presence of class G immunoglobulins to Mycoplasma hominis in the blood indicates the presence of an acute or past disease, as well as reinfection and a chronic inflammatory process. Indications:
- in a complex of studies for non-gonococcal urethritis in men;
- inflammatory diseases of the pelvic organs;
- infertility in women;
- epidemiological screening.
Preparation
It is recommended to donate blood in the morning, between 8 am and 12 pm. Blood is drawn on an empty stomach, after 4–6 hours of fasting. It is allowed to drink water without gas and sugar. On the eve of the examination, food overload should be avoided.
Interpretation of results
Units of measurement: UE*
A positive result will be accompanied by an additional comment indicating the sample positivity rate (SP*):
- CP >= 11.0 – positive;
- CP <= 9.0 – negative;
- CP 9.0–11.0 is doubtful.
*Positivity rate (PR) is the ratio of the optical density of a patient's sample to the threshold value. CP - positivity coefficient, is a universal indicator used in enzyme immunoassays. CP characterizes the degree of positivity of the test sample and can be useful to the doctor for the correct interpretation of the result obtained. Since the positivity rate does not correlate linearly with the concentration of antibodies in the sample, it is not recommended to use CP for dynamic monitoring of patients, including monitoring the effectiveness of treatment.
Mycoplasma hominis DNA
Real Time PCR is used to diagnose mycoplasmosis
This microorganism has a high prevalence in the population.
Especially for women.
Studies show that in different populations among the female population, Mycoplasma hominis is detected in 20-50% of cases.
In men, the bacterium is detected less frequently.
The carriage frequency in the population does not exceed 2-5%.
Given the high prevalence of the microorganism, not every case of its detection is an indication for treatment.
There are several criteria by which the doctor determines whether therapy is needed.
One of them is quantitative indicators of laboratory tests.
A quantitative or semi-quantitative test for Mycoplasma hominis DNA will fail.
When performing a quantitative test, the number of DNA copies in clinical material is shown.
The threshold value above which inflammatory processes can begin is considered to be 104 copies.
If the number of mycoplasmas is above the threshold, the form indicates “detected.”
If below this value, then “not detected”.
They are tested for Mycoplasma hominis DNA according to the following indications:
- presence of symptoms of inflammation of the urogenital tract
- detection of leukocytes in a smear for flora
- pregnancy planning
- early pregnancy
- immunodeficiency states
- infertility
- history of perinatal losses
PCR is performed not only for primary diagnosis.
The study is also prescribed after treatment to evaluate the results of therapy.
Mycoplasma hominis - diagnosis
To diagnose mycoplasmosis, laboratory tests are necessary. The main and most informative method for detecting mycoplasma is PCR (polymerase chain reaction). PCR detects the genetic material of a bacterium. A smear from the urethra, cervical canal is analyzed, and urine testing is possible. Before smear analysis, patient preparation is necessary. Two days before the study, you must abstain from sexual activity and refuse vaginal irrigation. Before submitting urine for analysis, it is not recommended to wash the genitals; it is better to take morning urine.
PCR analysis
Serological blood testing is much less common. The serological test determines the level of immunoglobulin M (IgM) antibodies. Their presence in the blood indicates a fresh infection and persists for up to 1-2 months. The material for serological testing is blood taken strictly on an empty stomach; the preliminary period of fasting should be at least 10-12 hours.
Culture for Mycoplasma hominis
Culture is another effective way to directly detect the microorganism.
The study also allows us to evaluate quantitative indicators.
Therefore, it can be used to determine indications for treatment.
Sowing also makes it possible to assess the sensitivity of the flora to antibiotics.
Most often, the bacterium is highly sensitive to the following drugs:
- clindamycin
- lincomycin
- josamycin
- doxycycline
- levofloxacin
Low sensitivity or resistance to ofloxacin and azithromycin is common.
Therefore, it is better not to use these drugs for therapy without sensitivity assessment.
Mycoplasma hominis norms
Many sources report that the norm for Mycoplasma hominis is 10 to 3 copies per sample or CFU per ml.
If the bacterium is detected in a concentration of 10 to 4 degrees or higher, then treatment is required.
Most doctors disagree with this.
There is no norm for Mycoplasma hominis.
Because there are no reliable ways to determine its amount in the genitals.
When a doctor takes a smear, he can take it from different parts of the urogenital tract from the same patient.
In this case, the results will be completely different, from the lowest numbers to the highest.
Therefore, many doctors are skeptical about quantitative indicators.
The presence of Mycoplasma hominis is in any case not the norm.
Another question is how dangerous this microorganism is in this particular patient.
If it is concluded that mycoplasma poses a threat, treatment is carried out.
If a woman does not plan to become pregnant, change her partner, or does not suffer from inflammatory diseases, antibiotics are usually not prescribed.
When is treatment for Mycoplasma hominis required?
Mycoplasma hominis is detected on average in 40% of women.
Most of them have no symptoms and do not complain about anything.
Therefore, the discovery of this bacterium is not always an indication for therapy.
The sensitivity of modern DNA tests is very high.
Therefore, they detect mycoplasmas even in minimal concentrations.
Indications for treatment are clinical and epidemiological.
Treatment is usually carried out in such cases:
- The woman has symptoms of inflammation of the vagina, bladder, and internal genital organs.
In this case, there are no other pathogens that can cause a pathological process.
- Mycoplasma hominis is present in concentrations of more than 10 to the power of 4 DNA copies per ml.
- Pregnancy is planned.
- The patient changes sexual partner.
To avoid infecting it, it is better to undergo treatment.
- Infertility.
In men, treatment is often prescribed even if they have no symptoms and the concentration of Mycoplasma hominis is not high.
Because the bacterium can cause chronic prostatitis.
And it will be much more difficult to cure than mycoplasma urethritis.
Antibiotics penetrate the prostate very poorly.
Other doctors do not prescribe therapy for everyone.
They use antibiotics only for absolute indications.
These are considered:
- male infertility
- asthenozoospermia
- nongonococcal urethritis
- orchiepididymitis
- systemic infection due to HIV or other immunodeficiency
Drugs for the treatment of Mycoplasma hominis
The basis of treatment is antibiotics .
Mycoplasma hominis can be completely destroyed in 5-7 days.
After successful therapy, it is not detected at all in the urogenital tract.
Antibiotics used:
- clarithromycin
- doxycycline
- josamycin
- levofloxacin
In most cases they work.
If not, the patient may not have been fully complying with medical prescriptions.
Or antibiotic resistance has developed.
In this case, a repeat course of therapy is required.
They use a different drug.
If treatment is ineffective, it is advisable to do a culture test to determine sensitivity to antibacterial drugs.
Josamycin is prescribed for pregnant women.
Fluoroquinolones and tetracyclines are prohibited during pregnancy.
They negatively affect the fetus.
Azithromycin can be used.
But mycoplasma hominis is not always sensitive to it.
Additional treatments:
- instillation of the urethra with silver solutions
- physiotherapy – for prostatitis and chronic inflammation of the pelvic organs
- massage of the prostate and seminal vesicles
- enzymes - to enhance the effect of antibiotics
- immune drugs
Miramistin and chlorhexidine are not used topically.
They are ineffective against Mycoplasma hominis.
There is no point in using herbs and other folk remedies.
What is Mycoplasma hominis?
The content of the article
Mycoplasma hominis
– atypical bacteria, belong to the genus
Mycoplasma.
These are microorganisms that lack a cell wall, which makes them resistant to many antibiotics.
Mycoplasma hominis
- can colonize the genitourinary tract. Colonization by these bacteria is most often accompanied by hormonal changes in women, for example, during menopause, as well as with frequent unprotected sexual intercourse.
Control tests after treatment with Mycoplasma hominis
Control of cure can be carried out using one of two methods:
- sowing tank
- PCR
PCR is most often used.
This method is more accurate and faster.
The timing of the control study depends on what antibiotics were used for treatment.
They can be bacteriostatic or bactericidal.
Bacteriostatic inhibits the growth of bacteria.
Bactericidal - kills them.
The most commonly used drugs are josamycin or doxycycline.
They are largely bacteriostatic.
After using these drugs, control of cure is carried out after 6 weeks.
This period of time is equal to two life cycles of ureaplasma.
Fluoroquinolones are sometimes used to treat mycoplasmosis.
They are bactericidal.
Therefore, control of cure can be carried out as early as 3 weeks after completion of the course of treatment.
Treatment of infection
Treatment of infection caused by the bacterium Mycoplasma hominis
requires the use of antibiotics. The most commonly used are tetracyclines and macrolides. Prescribe Unidox Solutab (doxycycline) 100 mg twice a day for 10 days. Vilprafen (josamycin) at a dosage of 500 mg three times a day, course – 10 days.
Macropen (midecamycin) 400 mg three times a day, course of treatment for 14 days. The use of the drug Sumamed (azithromycin) is effective; on the first day, take 500 mg once, then 250 mg in the next four days, also once a day. Treatment is accompanied by the use of means to normalize the microflora, stimulate the immune system, and vitamins.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Reasons for the failure of treatment for Mycoplasma hominis
Sometimes, after treatment, a person still develops ureaplasma.
The reason for this may be:
- ineffective treatment regimen
- patient non-compliance with medical prescriptions
- reinfection
- antibiotic resistance
Most often, the reason is the patient’s lack of scrupulous compliance with the doctor’s prescriptions.
The drugs are prescribed in tablets, not injections.
Therefore, the doctor cannot control the correctness of the treatment 100%.
Very often patients:
- are not completely cured
- use smaller doses
- forget to take pills from time to time
- change the drug to another
Re-infection and relapse of the disease require an additional course of therapy.
For this purpose, an antibiotic of a different pharmacological group is selected.
Prevention of Mycoplasma hominis
To prevent infection with Mycoplasma hominis it is necessary:
- limit the number of sexual partners
- use condoms
- Avoid sex with people who have signs of inflammatory processes in the urogenital tract
As part of secondary prevention, it is necessary to be tested for Mycoplasma hominis.
This should be done annually if you are sexually active.
At the same time, screening for other STIs is carried out.
It is important to undergo diagnostics at the stage of pregnancy planning.
Because Mycoplasma hominis poses a risk to the fetus.
Routes of infection
The most common route of infection with Mycoplasma hominis
– sexual intercourse without using a condom. Often, infection with mycoplasmosis is accompanied by other sexually transmitted diseases.
These include: ureaplasmosis (caused by Ureaplasma urealyticum), chlamydia (caused by Chlamydia trachomatis), gardnerellosis (Gardnerella vaginalis). Infection from mother to child during childbirth is possible. The household route of infection as a result of the general use of personal hygiene items (underwear, towels, bedding) is quite rare.