General characteristics of the disease
Leprosy is a chronic disease of infectious nature. Refers to granulomatous diseases. Leprosy is accompanied by damage to the skin, peripheral nervous system, eyes and respiratory organs.
The pathogen enters the human body through damaged skin and mucous membranes of the respiratory system. Constant contact with lepers who do not receive treatment provokes the onset of the disease.
If leprosy is diagnosed in time and treated, you can completely get rid of this disease. It is a myth that leprosy is incurable and death is inevitable.
The disease is not highly contagious. Leprosy affects 7% of people, the rest are immune to it. Leprosy is not inherited and does not become infected in the womb.
Types and their symptoms
According to various sources, today there are from three to ten million patients suffering from leprosy in the world, and more than 600 thousand new diseases are diagnosed annually.
There are several approaches to classifying leprosy, used by different organizations. But the distinguished species are not very different; rather, in some classifications one of the forms is simply omitted.
- The World Health Organization distinguishes two forms of the disease, based on the number of pathogenic bacteria in the body: oligobacillary (up to 5 lesions on the body) and multibacillary (more than 5 lesions).
- The International Leprosy Association scale is based on the Ridley-Jopling classification (based on the immune response) and has five grades: tuberculoid, borderline tuberculoid, borderline, borderline lepromatous and lepromatous leprosy.
- ICD-10, although developed by WHO, also takes the Ridley-Jopling principle as a basis, but adds an additional vague form.
- MeSH uses three groups, which are described below with a photo.
The lepromin test is an intradermal injection allergy test with lepromin (the contents of tissue lesions of patients with lepromatous leprosy). The local reaction is assessed after 2-4 weeks. The test is performed to diagnose the form of leprosy for the subsequent selection of a treatment regimen. Simply put, the lepromin test is like the manta test that everyone does in childhood, only here, instead of tuberculosis bacteria, the causative agent of the most terrible form of leprosy is introduced, after which the immune reaction is observed on the skin.
Lepromatous (sarcoid)
Considered the most dangerous. There are a huge number of bacteria in the body. The disease begins with damage to the epidermis - granulomatous nodes called “lepromas” form on the surface of the limbs, forehead, eyebrows, cheeks and nose (sometimes on the torso and even internal organs). Over time, large folds form, transforming the patient’s face into a “lion’s face.”
The tubercles are hard to the touch and range in size from a match head to a kidney bean. These nodes contain a huge number of mycobacteria: per 1 cm3 of affected tissue - up to one billion bacilli.
Initially, the disease affects the lining of the nose, especially the septum separating the right and left parts of the nostril is involved in this process. It is from this part that a laboratory scraping or puncture is taken and, in the presence of leprosy, a Hansen bacillus is isolated.
On the part of the eyes, negative changes occur in the cornea (ulceration, scarring) and without medical assistance this leads to blindness.
The nervous system is also involved in the pathological process. Patients experience neurotic reactions, changes in sensitivity, and movement disorders.
One of the severe complications is delamination of the skeletal bones - the hands and feet become soft; in a severe stage of the disease, the phalanges of the fingers may fall off, and the nose will become deformed.
Lepromine test is negative.
Border
This is the most common form of leprosy. The disease is characterized by a small number of spots with an unclear border. Often the borderline form of leprosy is mistaken for chronic dermatosis. The patients' well-being at the onset of infection was not affected. As the disease progresses, trophic disorders and sensory disturbances become more pronounced.
The lepromine reaction can be negative or positive. In the first case, there is a high risk of the disease transitioning to the sarcoid form. With a positive reaction, the pathology, as a rule, takes on a tuberculoid course.
Tuberculoid
Damage to the skin, peripheral nerves and internal organs is observed.
In the tuberculoid form, instead of nodes, one to several asymmetrical spots are formed on the epidermis, painless to the touch, red-brown in color with clear boundaries and blanching in the center.
Nervous diseases and polyneuritis have similar symptoms to the lepromatous form, but are much milder. Along with this, there is an early impairment of tactile and temperature sensitivity. The affected areas appear shiny and “greasy”; hair loss is also observed in these areas.
The tuberculoid form of leprosy has a low infectivity compared to the lepromatous form.
When performing the lepromin test, a weak delayed reaction is noted.
Eyebrow loss is one of the symptoms
Features of the course in children
In children, leprosy can occur as a juvenile type. In other words, the disease has some features of the lepromatous, tuberculoid and borderline forms, and the manifestation of erythema nodosum is also possible.
History of leprosy
Previously, leprosy was called a “slow disease” and was mentioned in the Old Testament. The peak occurred in the 12th–14th centuries. It did not spread like a plague, in the form of a pandemic, and gradually affected Medieval Europe. The name “leprosy” comes from the word “to show off” - to make the face or body ugly.
Since leprosy was considered an incurable disease, patients were forcibly expelled from society, thereby doomed to death. It was believed that leprosy was transmitted by touch. Lepers wore bells that warned them of approaching healthy people so that they would have time to escape.
Patients were deprived of their rights; they could not be in crowded places, drink water from common containers, swim in the river, or touch healthy citizens. The disease of leprosy was a permissive reason for a spouse to divorce. The leper was buried in church, funeral events were held, and a black robe was put on him. During life, a person was considered dead.
Later, leper colonies appeared to isolate the sick. The institutions provided medical care, food, and a roof over their heads. Monks looked after lepers, and leper colonies were opened on the territory of monasteries. Patients here were isolated for the rest of their lives. The creation of such institutions made it possible to reduce the spread of the disease.
Today there are three leper colonies in Russia: in Astrakhan, Krasnodar and Stavropol.
In 1873, a doctor from Norway, Gerhard Hansen, discovered the causative agent of leprosy. In 1948, the Order of Mercy for leprosy patients was created, and five years later a day of assistance to leprosy patients was established.
Historical facts
19th-century drawings depicting leprosy patients.
On the left, a person has facial paralysis. The woman in the center has, in addition to the nodules, loss of her eyebrows and what appears to be scarring in her right eye. The woman on the far right (in the description of the picture it was stated that she is 28 years old) has many large nodular formations (leproma). Humanity has been familiar with leprosy for a long time. The first mentions of the disease found in written monuments date back to the 15th–10th centuries. BC. Leprosy was also described in the Bible (Old Testament) and in the Ebers papyrus (one of the oldest medical manuscripts of Ancient Egypt).
Previously, people with leprosy caused fear and disgust, so they were called “ lepers .” In ancient times, the disease could not be treated; victims faced inevitable disability and, in many cases, death.
In Europe, the peak of the disease was observed in the period from the 12th to the 14th centuries. Due to suspiciousness and leprophobia, the victims became real outcasts - they were forbidden to visit crowded places and use running water, they were also afraid to be near them or even talk to them. Leprosy was considered a significant reason for the separation of a marriage, and at the first sign, church funerals were held for a still living person.
leper colonies were later invented , which were built on the territory of monasteries. There, patients received medical care and died in “humane” conditions. Such institutions helped reduce the peak incidence, and by the 16th century, leprosy had disappeared from many European countries.
Today, leprosy is a well-studied disease. It has been proven that it is not transmitted by contact with the skin (given the integrity of the epidermal layer) and, if left untreated, is not always fatal.
French journalist Raoul Follero founded the Order of Charity in 1948, and in 1966 the Federation of European Leprosy Associations. Thanks to his contributions, a new holiday appeared on the calendar - the Day of the Rights of Leprosy Patients, which is celebrated on January 30.
What causes leprosy?
The causative agent of leprosy is the rod-shaped bacillus Mycobacterium leprae with rounded ends. The bacterium does not respond to treatment with alcohol solutions. The properties of the microorganism are similar to those of tuberculosis. The differences lie only in the inability of the leprosy causative agent to reproduce in an artificial nutrient medium and its non-manifestation over a long period of time. The incubation period can reach 20 years.
The activation of the pathogen is provoked by environmental factors: poor diet, dirty water, bacterial infectious disease. Pathogenic microflora is found in saliva, urine, feces, semen, and breast milk. Bacteria, getting on the mucous membranes, penetrate the body, reaching blood vessels and nerves. Mycobacteria spread throughout the body through the bloodstream.
Due to the length of the incubation period, leprosy begins to be treated late. Previously, it was difficult to diagnose the disease.
In 2008, scientists discovered a new bacteria, Mycobacterium lepromatosis, common in the Caribbean. Microorganisms provoke ulcers on the skin and affect nerves and internal organs.
Reasons for development
The causative agent of leprosy was discovered in 1874 by the Norwegian scientist A. Hansen. Mycobacterium leprae is a gram-positive bacteria that belongs to intracellular parasites, the morphological properties of which are highly similar to Koch's bacillus (causes tuberculosis).
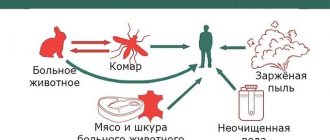
Transmission routes
Contrary to popular belief, leprosy is not very contagious.
The source of infection is sick people. The bacillus is excreted in nasal mucus, feces, urine, and saliva; Leprosy also releases bacilli from the ulcerated surface into the environment. Infection most often occurs through direct skin contact (mycobacteria penetrates through microcracks or wounds). Also, transmission of the disease can occur through kissing, sexual intercourse or bites of blood-sucking insects. It is also believed that the infection can be transmitted through a patient's cough.
People with strong immune systems are resistant to leprosy. The disease in this case is less contagious and infection can occur only through prolonged close contact. The incubation period (the time from infection to the appearance of the first signs) lasts on average from three to seven years.
Epidemiology
Leprosy is a low-contagious disease. When a pathogen enters the body, infection occurs with a 20% probability. Strong immunity guarantees protection against the development of leprosy.
There is a high risk of infection for people who live in areas where armadillos live. The disease is provoked by the following factors:
- unsanitary conditions;
- alcohol abuse;
- poor nutrition;
- weak immunity.
Leprosy is common in economically disadvantaged countries, areas, and among poor categories of the population.
How is leprosy (leprosy) transmitted?
Transmission of infection occurs by airborne droplets. The pathogen enters the body through the respiratory system. There are rare cases where leprosy was transmitted during tattooing and surgical operations through insufficiently disinfected instruments.
Less commonly, mycobacteria enter the body through the skin through constant contact with the patient. Penetration of the pathogen occurs through microcracks, wounds, and scratches.
Sources of infection other than humans can include buffalos, armadillos and monkeys. People can contract the disease through scratches from animals or their meat. At risk are craftsmen who make figurines and souvenirs from armadillo shells.
What do lepers look like?
Lepers are people with leprosy (leprosy) or chronic granulomatosis. Since the disease has been known since the times of the Old Testament, it is not surprising that methods of treating and avoiding this disease began a very long time ago. The attitude of healthy people towards lepers has always been the same - people try to avoid contact with the sick so as not to contract the infection. However, modern medical knowledge helps to avoid cruel methods.
How lepers were treated, then and now:
- In ancient times, lepers were subjected to severe persecution. They were expelled from the settlements, their homes and belongings were destroyed by burning. A leper (outcast) had to avoid contact with healthy people, wear torn clothes and not cover his head, and those with leprosy were also forbidden to create families. Thus, lepers became outcasts and wretched.
- In the Middle Ages, during the leprosy epidemic, leper colonies began to be organized - settlements for patients and their families. The creation of leper colonies meant clinics where lepers would undergo treatment. In fact, the patients were placed in strict quarantine, where contact with lepers was only limited in a closed area. Since no treatment was provided, and contact with infected people was not interrupted, the sick only lived out their days.
- Modern science has discovered almost everything about leprosy. One such knowledge is the fact that leprosy is not transmitted by light touch to the patient, and does not always lead to death. It is also known that 93-95% of the world's population have strong immunity to infection, and there is no risk of infection for them. Having this information, people no longer react so violently to infected patients, although there is inner fear in everyone.
Nowadays, drug treatment of lepers is carried out quite successfully. Depending on the treatment, it takes place in a specialized infectious diseases hospital, and after the course of treatment they must undergo regular medical examination.
In cases where the disease is detected at an early stage, positive treatment results can be expected within 2-3 years; in more advanced stages, treatment can take decades. You should also know that characteristic external signs can also occur in other pathologies: leishmaniasis, tertiary syphilis, toxicerma, tuberculosis and sarcoidosis of the skin, erythema nodosum and erythema multiforme.
There is a fairly quick and simple method for diagnosing leprosy (it may not be accurate): inject 1 ml of a 1% solution of nicotinic acid into the area of the leprosy rash; if the result is positive, within 3 minutes swelling and redness will appear at the site of the rash. For a more accurate result, it is necessary to undergo a full diagnosis.
Leprosy symptoms
At the end of the long incubation period, the latent stage of the disease begins. At the beginning of the development of leprosy, the following symptoms appear:
- malaise;
- neuralgia;
- pain in muscles, joints;
- weakness;
- stomach upsets;
- fever.
Further symptoms increase depending on the type of leprosy. In the tuberculoid course of the disease, the surface of the skin and the nervous system are affected. The skin becomes covered with spots of varying shapes and clarity. They are located randomly throughout the body.
With further spread of the disease, the spots acquire a denser shape, some merge into a single formation with purple hues. Depigmentation and peeling may occur around the spots.
Damage to the peripheral nervous system is manifested in the formation of dense cords in the area of nerve fibers. With tuberculoid development of leprosy, changes in the NS occur more easily than in other forms.
Further progression of leprosy is accompanied by a lack of sweating, hair loss, and impaired thermoregulation.
The lepromatous variety of leprosy is more complex in its symptoms. Large nodules called lepromas appear on the skin. Mycobacteria multiply in them. The nodes deform the nose and superciliary part of the patient’s face, which visually makes him look fierce and aggressive. Lepromas have a cherry tint with a greasy sheen. A sharp deepening of wrinkles is observed.
Often, with the lepromatous form of the disease, finger loss occurs due to disruption of the integrity and destruction of the joints. Damage to the eyes is also observed and the person may go blind. Bones are destroyed, the function of sweating is lost, the functioning of the endocrine system is disrupted, and internal organs are destroyed.
The concept of “lion face” in medicine
The term arose due to the similarity of the patient's face with the muzzle of a lion. Scientifically, this condition is called leontiasis. Presents a distorted face with signs of progressive lepromatous leprosy. Symptoms manifest themselves in thickening of the skin, the appearance of deep furrows on the forehead and cheeks. The name “beautiful leprosy” is often used, but in reality it is not such.
During the formation of the “lion face” the following changes occur:
- drooping earlobes;
- roughness of the skin;
- eyebrow hair loss.
Symptoms of “lion face” are also observed in other pathologies:
- heart failure;
- swelling due to kidney diseases;
- hypoalbuminemia.
With the undifferentiated type of leprosy, there is no eye damage. Spots appear on the skin everywhere, but after some time they go away on their own.
Today, with the help of cosmetology, it is possible to get rid of this feature on the face, but it is first important to completely recover from leprosy.
Types of leprosy
There are three types of leprosy, differing in the degree of damage, treatment method, and transition to the chronic stage:
- Tuberculoid.
- Lepromatous.
- Uncertain.
Tuberculoid leprosy is benign. It is characterized by small skin lesions. In some places the skin becomes pale and sensitivity is lost. In this case, mycobacteria are not detected, and the body has a high degree of resistance to the disease.
After healing, characteristic scars from the spots remain on the body. The peripheral nervous system is often affected. When leprosy enters the chronic stage, pathogens of the disease are detected in the area where the spots appear.
The lepromatous variety of leprosy is considered malignant. Extensive areas of spots are observed on the skin. Damage occurs to internal organs, nasal mucosa, and respiratory organs. The face takes the shape of a lion's muzzle.
Five years after the onset of leprosy, active hair loss begins, including eyelashes, eyebrows, mustaches, and beards. Eye damage is observed and vision loss is possible. In the lymph nodes and liver, the active formation of lepromas—nodules with pathogens—continues.
The indeterminate shape is accompanied by spots with blurred boundaries spreading over the body. The presence of the causative agent of leprosy is not determined. The condition resembles a chronic stage, the patient's condition is stable. Damage to the nervous system occurs.
What is leprosy
Leprosy (the modern medical name is “Leprosy”) is a disease caused by infection and occurs in a chronic form. The causative agent of the disease is considered to be the gram-positive microbacterium leprosy. It affects the skin, mucous membranes and PNS (peripheral nervous system) of the patient.
Many people think that leprosy is an epidemic from past centuries, but it has not yet been defeated and is found in all corners of the world.
Most often, tropical countries suffer from leprosy, although in Europe the disease makes itself felt. In Russia, the last recorded case was in 2015 in Astrakhan. The infection is transmitted from an infected person to a healthy person through prolonged skin contact or through mixing of mucous membranes and other body fluids.
Methods of infection:
- Prolonged physical contact;
- Saliva;
- Lactation;
- During sexual intercourse;
- Urine;
- Mucus from nasal passages;
- Blood;
- From animal carriers (monkeys, armadillos).
The disease has a fairly long incubation period. It can take from 5 to 25 years from the time of infection to the onset of symptoms.
Diagnosis of leprosy
Leprosy can be suspected by the appearance of characteristic spots on the skin and decreased sensitivity. If leprosy is suspected, an infectious disease doctor will prescribe the following tests:
- serological;
- bacterioscopic;
- histological.
When the nervous system is damaged, it is important to exclude diseases with similar symptoms.
Description of leprosy diagnosis:
- Examination of the skin and mucous membranes of the respiratory system.
- Palpation of nerves.
- Examination of the limbs for atrophy.
- Sweating test.
- Histamine test.
- Test with nicotinic acid.
- Pathohistological examination of the affected skin area.
Based on the data obtained, the doctor makes a final diagnosis.
Diagnostics – testing doctors’ knowledge
Even today, leprosy is not a forgotten disease and is encountered from time to time in modern medical practice. Its definition can cause particular difficulties in countries where this disease is very common, despite developed medicine (for example, in the USA).
To diagnose a disease caused by Mycobacterium leprae, highly specialized doctors are involved: infectious disease specialists, dermatologists, neurologists. In addition to patient complaints and external signs, laboratory tests are taken into account; the most accurate is bacterioscopic detection of the Mycobacterium leprae bacillus or by detecting DNA using polymerase chain reaction. A scraping is taken from the nasal mucosa and affected areas of the skin; material isolated from the tubercles and lymph nodes is also studied.
It is important for the doctor to be attentive, since at first leprosy can be confused with another pathological process. In this case, a series of laboratory tests should be performed to clarify the diagnosis.
Diseases whose dermatological manifestations are highly similar to leprosy (taking into account the nature of the rash and spots):
- tertiary syphilis;
- erythema multiforme;
- toxicoderma;
- neurofibromatosis;
- lichen planus;
- tuberculosis and sarcoidosis of the skin;
- leishmaniasis;
- Erythema nodosum.
There is another way (not always effective, but simple and harmless) for differential diagnosis of leprosy - a test with nicotinic acid (injected 1 ml, 1% solution). 1-3 minutes after the procedure, the spotted leprosy rash turns red and swells.
Treatment
The first cure for leprosy was created in 1950. It was slow to act and eventually became useless as mycobacteria developed immunity to it.
Today, leprosy can be easily cured if you consult a doctor in a timely manner and begin therapy. Antibiotics are used for treatment. Medicines for leprosy:
- Rifampicin;
- Dapsone;
- Clofazimine;
- Methyluracil;
- gamma globulin;
- Lampren.
In the case of a severe form of the disease, complex therapy is prescribed using three drugs at once. Treatment lasts within six months, but can reach several years.
Additionally, glucocorticosteroids and vitamin complexes are prescribed to maintain immunity and prevent atrophy.
Treatment methods
Today, leprosy is a curable disease. If the infection is severe, the patient is placed in specialized anti-leprosy institutions. In other cases, the patient receives therapeutic care at home.
For the treatment of leprosy, etiotropic therapy is used. Drug treatment involves the use of sulfone drugs that have an antibacterial effect on Mycobacterium leprae. The most common drugs are “Solusulfone” (it is administered intramuscularly twice a week), “Diaminodiphenylsulfone”, “Sulfametrol”. Dimotsifon is also effective, providing both an antimicrobial and immunomodulatory effect.
Broad-spectrum antibiotics (Rifampicin, Ofloxacin), vitamins, and hepatoprotectors are also prescribed. Due to a decrease in the body's protective functions, there is a high probability of developing tuberculosis, so patients are often prescribed unscheduled BCG vaccination.
To prevent disability, physiotherapeutic procedures are recommended: massage, electrophoresis, UHF, therapeutic and preventive gymnastics and physical education. In order to prevent orthopedic diseases, it is recommended to wear special aids (insoles, ties, staples, bandages and orthoses).
Complications
Lack of treatment leads to the development of extreme skin lesions, damage to the mucous membranes of the eyes, nose, and respiratory tract. If the disease is neglected, the person may remain blind forever.
Complications include:
- glaucoma;
- swelling, ulcers on the face;
- infertility in men;
- weakness, muscle atrophy;
- nosebleeds;
- nerve damage.
The latter complication leads to loss of sensitivity. When injuring parts of the body, the patient does not feel pain.
Disease prognosis
The prognosis for leprosy depends on the type of disease, stage, therapy, and medications used. Before the use of sulfone drugs, leprosy patients lived no more than 15 years from the onset of symptoms.
The cause of death was the following factors:
- asphyxia;
- cachexia;
- uremia.
By the time of death, the patient is disabled with severe mutation of the limbs, blindness, paralysis, and facial deformities.
It was also not uncommon for patients to live 40 years after the onset of clinical signs. There are cases in history where self-healing was observed without medical intervention, but the consequences were characterized by severe disability.
Since the introduction of leprosy chemotherapy into medical practice, death rates have decreased.
Early diagnosis of leprosy allows the patient to have no visible consequences after recovery. Late diagnosis of leprosy leads to the fact that reduced sensitivity, amyotrophy persists, muscle strength decreases, and the person is limited in the ability to work normally.
A disease of the poor?
Leprosy is considered a disease characteristic of disadvantaged sections of the population. Foci of infection in most cases occur in poor countries: India, Brazil, Angola.
But the disease also affects ordinary people if they have been in contact with sick people. This means that any person is susceptible to the disease, not just residents of disadvantaged areas.