Gastritis is divided into several stages; as it develops and without treatment, it flows from one form to another.
The first stage of the disease is superficial gastritis. This form of gastritis is considered the most harmless: inflammation of the gastric mucosa is superficial, there are no focal lesions, and the deep tissues of the stomach and duodenum are not affected. The disease occurs in most cases of treatment and does not fall into the category of dangerous and complex. But at this stage, gastritis must be treated immediately, since it can progress to the next stage, becoming a chronic condition. To prevent this, you need to contact a gastroenterologist in a timely manner.
Definition
Superficial gastritis is a common pathology characterized by inflammation of the gastric mucosa.
At the initial stage of the disease, cell atrophy does not occur; changes affect only the upper layer of the epithelium. The disease lasts a long time, and if left untreated, the pathological process becomes chronic. The Department of Gastroenterology at the Elena Malysheva Clinic in Izhevsk provides a full range of advisory and diagnostic services in the treatment of diseases of the gastrointestinal tract.
Experienced specialists will select an effective treatment regimen for superficial gastritis, preventing further dystrophic changes and disturbances in the secretion of gastric juice.
Complications of gastritis
If you do not take into account the doctor’s recommendations, inadequate treatment can cause serious consequences:
- Peptic ulcer disease. Most often it appears in the erosive form of the disease.
- Atrophic gastritis. Due to the low concentration of hydrochloric acid, the glands of the mucous membrane almost completely lose their ability to produce secretions and begin to be replaced by connective tissue. Refers to precancerous conditions.
- Gastric bleeding due to ulcers or erosions. It is characterized by shortness of breath, pale skin, weakness, the presence of blood in the vomit and black liquid stool. Refers to conditions requiring emergency medical care.
- Lack of vitamin B12 and folic acid. It occurs in the autoimmune form of the disease or in the advanced stage of atrophic gastritis, when the stomach glands stop producing the protein responsible for the absorption of vitamin B12.
- Anemia. It develops as a result of acute or chronic blood loss, as well as due to poor absorption of vitamin B12 from food by the body.
Causes
The development of gastritis is largely due to the lifestyle of modern people. Chronic inflammation is caused by the following factors:
- improper and irregular nutrition;
- bad habits;
- chronic stress;
- metabolic disorders;
- reflux of bile into the stomach (gastroesophageal reflux);
- infection with the bacterium Helicobacter pylori;
- autoimmune disorders;
- food poisoning.
Hereditary factors or unsystematic use of medications play an important role in the appearance of superficial gastritis.
What to do
Once the diagnosis is determined, treatment should begin as quickly as possible. After all, the sooner help is provided, the greater the chance that negative consequences and complications will not appear.
“Those who have been diagnosed with gastritis are advised to follow a diet and monitor their diet,” says Alexey Povalyaev. Here they usually talk about fractional meals - 5-6 times a day. Naturally, you will have to give up traditionally harmful foods, such as fatty, fried, smoked, spicy, and soda. You should also give up bad habits that further worsen a person’s well-being.
Additionally, drug therapy may be prescribed, but only at the discretion of the doctor.
It is worth understanding that if treatment is not carried out, complications may develop. For example, the formation of ulcers, the transition of the disease to the chronic stage, the development of pancreatitis, as well as intoxication.
Symptoms of superficial gastritis of the stomach
The acute form of the disease is manifested by a number of characteristic symptoms:
- lack of appetite;
- feeling of heaviness, pain in the upper abdomen after eating;
- nausea, vomiting, heartburn;
- bitter-sour taste in the mouth;
- upset stool, flatulence, bloating;
- deterioration of general health, weakness, irritability.
The intensity of the pain syndrome varies - from unpleasant, nagging sensations to acute, cramping attacks of pain in the stomach. Ignoring the problem leads to insufficient absorption of nutrients and dysfunction of the digestive system. It is necessary to treat superficial gastritis when the first alarming symptoms appear. Specialists at Elena Malysheva’s clinic will stop the progression of the disease and help prevent unwanted complications.
Classification
According to the form of the disease, the disease is classified into:
- Acute superficial gastritis.
- Chronic superficial gastritis . In the absence of timely adequate therapy, the chronic form can turn into atrophic, which is characterized by a high risk of malignancy (transition to oncological forms).
At the location of the inflammatory process:
- the pathological process is localized in the outlet part of the stomach (antrum), which is why it got its name - antral gastritis ;
- damage to the body of the stomach;
- damage to the working day of the body of the stomach - fundic;
- damage to all parts of the stomach - pangastritis .
By scale they distinguish:
- Diffuse superficial gastritis . The diffuse type is characterized by the spread of the inflammatory process throughout the mucous membrane of the organ.
- Focal superficial gastritis . The focal form is characterized by damage to only certain areas of the stomach.
Classification by reason of occurrence:
- Dosage form . Develops as a side effect in response to taking certain medications.
- Endogenous form . It occurs in response to the influence of several internal factors at once.
- Bacterial form . It is formed as a result of the entry into the body of a bacterium such as Helicobacter pylori. According to statistics, in 85% of cases it is this microorganism that causes the development of gastritis.
- Reflux gastritis . It develops in response to the entry of highly acidic and bile from the duodenum into the stomach. This form is considered the most dangerous, because characterized by gradual metaplasia - the transition of cells into a foreign form, and the further development of the oncological process.
Classification by acidity level:
- with normal secretion;
- with increased secretion (hyperacid);
- with reduced secretion (hypoacid).
Diagnostics
Treatment of superficial gastritis requires a competent approach. At the first stage, it is necessary to undergo a comprehensive diagnostic examination:
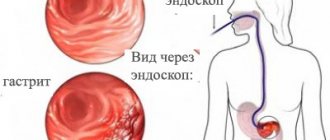
- FGDS procedure - endoscopic examination of the stomach;
- biopsy (endoscopic) - the biopsy is examined for signs of superficial inflammation in the cells of the mucous membrane;
- x-ray with double contrast (if necessary) – reveals a violation of the secretion of gastric juice and motor-evacuation function;
- breath test - allows you to determine the presence of Helicobacter pylori infection.
Additionally, the doctor may prescribe a blood test to detect antibodies to the bacterium Helicobacter Pylori, a urine and stool test (coprogram).
Why is gastritis dangerous?
Left unattended, gastritis can develop more and more severe consequences. Over time, the superficial inflammatory process can cause deep tissue damage - erosions and ulcers, which can lead to life-threatening gastric bleeding. Certain strains of Helicobacter significantly increase the risk of developing stomach cancer. The same complications occur in patients with chemical gastritis. Autoimmune gastritis is more characterized by mucosal atrophy and pernicious anemia with vitamin B12 deficiency.
Treatment of superficial gastritis of the stomach
Treatment includes taking medications and following a special diet. Taking into account the severity of the pathological process, the gastroenterologist will select drugs with enveloping, analgesic, and antispasmodic effects. The patient will be prescribed antacids, digestive enzymes, and medications that reduce the production of hydrochloric acid.
To normalize stool, the treatment regimen for superficial gastritis includes medications for diarrhea or drugs that improve intestinal motility. An important point in therapy is nutritional adjustments. The gastroenterologist will definitely recommend a special diet that eliminates irritation of the gastric mucosa.
IMPORTANT! The attending physician selects all medications individually, taking into account the patient’s condition, clinical picture of the disease, and possible contraindications. You should not self-medicate; unsystematic use of medications can aggravate the condition and provoke complications.
Advantages of treatment at Elena Malysheva’s clinic
At the medical center, patients are treated by highly qualified specialists with extensive experience in the field of gastroenterology. The clinic is equipped with advanced diagnostic equipment and offers innovative treatment regimens for gastrointestinal diseases. A professional approach, attentive and sensitive attitude towards each client is our main advantage!
You can make an appointment with a gastroenterologist at any convenient time by phone or through a special online application form on our website.
Prevention
Prevention of chronic gastritis involves preventing factors that can cause damage to the mucous membrane. These are hygienic measures against Helicobacter infection: thoroughly washing dishes, using each family member’s own cups, plates and cutlery. Care must be taken when handling medications and chemicals that are potentially harmful to the health of the digestive system.
If you do get gastritis, it is important to take timely measures to prevent it from becoming chronic. The main goal of prevention in this case is to maintain a favorable microbiome (microflora) of the digestive tract.
To prevent the development of the disease you should:
- eat small portions often,
- avoid foods that may irritate the stomach,
- reduce or eliminate alcohol consumption,
- quit smoking
- avoid stress.
Innovation
Scientists have begun searching for substances that are less traumatic for the body and effective in combating Helicobacter.
And in the course of numerous studies, it turned out that a pronounced positive effect is observed when taking certain beneficial bacteria. Among the numerous beneficial bacteria that have a positive effect on the microflora of the stomach and intestines, there are those that also fight “bad” bacteria, in particular Helicobacter. They have also been shown to increase the effectiveness of drug therapy in the treatment of gastritis and reduce the side effects of taking antibiotics.
The search for truly effective and safe remedies against Helicobacter took many years.
Chronic gastritis with normal and increased secretory function of the stomach
This type of disease is typical for young men. The surface epithelium of the stomach is affected; as a rule, no destruction occurs in the mucous membrane. Patients feel pain similar to that of an ulcer. After eating, they have a feeling of internal heaviness. Patients constantly complain of heartburn and unpleasant belching. The majority of them suffer from constipation. All these phenomena intensify at night.
Publications in the media
Chronic gastritis is a long-term disease characterized by the development of a number of morphological changes in the gastric mucosa and accompanied by various disorders of its basic functions. Prevalence. 50–80% of the entire adult population, the incidence of chronic gastritis increases with age. Incidence of gastritis and duodenitis: 287.2 per 100,000 population in 2001.
Classification
• By etiological factor • Microbial: Helicobacter pylori, etc. • Non-microbial •• Autoimmune •• Alcoholic •• Post-resection •• Caused by exposure to NSAIDs •• Caused by exposure to chemical agents • Unknown factors, incl. microorganisms.
• By type • Non-atrophic (type B, superficial, diffuse antral, hypersecretory) • Atrophic (type A, diffuse gastric body, associated with B12-deficiency anemia) • Special forms •• Chemical •• Radiation •• Lymphocytic •• Giant hypertrophic ( Ménétrier's disease, adenopapillomatosis) •• Granulomatous •• Eosinophilic •• Other infectious.
• By localization • Antral gastritis • Body gastritis • Pangastritis.
Etiology • Chronic non-atrophic gastritis in 85–90% of cases is caused by Helicobacter pylori • The development of chronic atrophic (autoimmune) gastritis is associated with the genetically determined production of autoantibodies to the lining cells of the gastric mucosa • The most common causes of chemical (reactive) gastritis are bile reflux and long-term use of NSAIDs • The etiology of eosinophilic gastritis is unknown, some patients have a history of bronchial asthma, eczema and other allergic diseases • Granulomatous gastritis is found in 10% of patients with sarcoidosis, 7% of patients with Crohn’s disease, with tuberculosis, mycoses, foreign bodies in the stomach • Etiology of giant hypertrophic gastritis is unknown.
Clinical picture
• Chronic non-atrophic gastritis • The pain syndrome often resembles that of duodenal ulcer (pain in the epigastric region that occurs on an empty stomach, but is usually less intense). The pain can be acute, cramping or aching, not intense; sometimes occur soon after eating • Dyspeptic syndrome - heartburn, sour belching, less commonly nausea, vomiting of gastric contents.
• Atrophic gastritis • Often combined with B12-deficiency anemia, thyroiditis, thyrotoxicosis, primary hypoparathyroidism • Sometimes the disease is latent • The most common manifestations are heaviness in the epigastric region after eating, a feeling of overeating, fullness of the stomach, belching of food and air, unpleasant taste in the mouth , loss of appetite, possible flatulence, unstable stool.
• Chemical (reactive) gastritis • Characterized by a triad of symptoms: pain in the epigastric region, intensifying after eating, vomiting with bile, bringing relief, weight loss.
• Giant hypertrophic gastritis • Pain in the epigastric region of varying intensity, often aching, occurs after eating and is accompanied by a feeling of heaviness in the stomach • Vomiting and diarrhea are possible; appetite is often reduced, sometimes even to the point of anorexia • In most patients, body weight decreases (by 10–20 kg) • In 25–40% of patients, peripheral edema is detected due to significant loss of protein with gastric juice (more than 8 g/day) • Gastric bleeding from erosions • Gastric carcinoma develops in 10% of cases.
Diagnostics
• OAC: B12-deficiency anemia in chronic gastritis type A
• Stool analysis: possible presence of hidden blood, as well as undigested food debris with reduced secretory activity of the stomach.
• X-ray examination does not allow diagnosing the main forms of chronic gastritis; but with its help it is possible to identify ulcers, cancer, polyposis, duodenal gastric reflux, giant hypertrophic gastritis, chronic obstruction of the duodenum • Chronic obstruction of the duodenum - delay of the contrast mass in the intestinal lumen for more than 45 s, expansion of the intestinal lumen, the presence of duodenum gastric reflux •• Giant hypertrophic gastritis (Menetrier's disease) - pronounced thickening of the folds of the mucous membrane in a limited area (with a local variant) or throughout the stomach (with a diffuse variant). The stomach wall in the affected area is elastic, peristalsis is visible.
• FEGDS •• Non-atrophic (superficial) gastritis: the mucous membrane is shiny (sometimes with a coating of fibrin), edematous, hyperemic, submucosal hemorrhages •• Atrophic gastritis: the mucous membrane is thinned, pale gray in color, with translucent blood vessels, the relief is smoothed •• Reflux -gastritis: the pylorus is gaping, the gastric mucosa is hyperemic, edematous; bile is present in the stomach •• Giant hypertrophic gastritis: there is a large amount of mucus in the stomach, the mucous membrane is easily vulnerable, erosions and hemorrhages are often found.
• Study of the secretory function of the stomach •• Chronic non-atrophic gastritis, reflux gastritis: the secretory function is normal or increased •• Chronic atrophic gastritis, giant hypertrophic gastritis: the secretory function of the stomach is reduced.
• Detection of Helicobacter pylori •• Invasive methods: it is necessary to perform FEGDS with a biopsy of the gastric mucosa; at least five biopsies are taken (two each from the antrum and fundus and one from the angle of the stomach). To confirm the success of eradication, the study is carried out no earlier than the 5th week after completion of the course of treatment ••• Bacteriological method ••• Histological method (detection of bacteria during microscopic examination of stained preparations) ••• Biochemical method (urease test) •• Non-invasive tests •• •Immunological methods (detection of antibodies to Helicobacter pylori) •••Breath test ••PCR diagnostics in biopsy samples of the gastric mucosa (invasive method) and in the patient’s feces (non-invasive method).
• Detection of antibodies to parietal cells and intrinsic factor and hypergastrinemia are a sign of atrophic autoimmune gastritis.
• Floor manometry of the upper gastrointestinal tract: with reflux gastritis, an increase in pressure in the duodenum to 200–240 mm water column is detected. (normally - 80–130 mm water column).
TREATMENT
Chronic non-atrophic gastritis
• Diet: for hypo- and achlorhydria, diet No. 2 is prescribed, for hyperacid conditions - diet No. 1.
• For gastritis caused by Helicobacter pylori - eradication (course of therapy - 1-2 weeks) •• Triple therapy ••• bismuth tripotassium dicitrate 120 mg 4 times / day for 28 days ••• metronidazole 200 mg 4 times / day in for 10–14 days ••• tetracycline 500 mg 4 times/day for 10–14 days •• Quadra-therapy ••• omeprazole 20 mg 2 times/day ••• tripotassium bismuth dicitrate 120 mg 4 times/day •• • tetracycline 500 mg 4 times a day ••• metronidazole 500 mg 3 times a day.
• In the absence of Helicobacter pylori and increased secretory function of the stomach •• Antacids, preferably non-absorbable, 1-2 hours after meals 3-4 times / day and before bed • Selective m-anticholinergic blockers (pirenzepine - 50 mg 2 times / day) • Blockers Histamine H2 receptors: ranitidine (150 mg 2 times a day orally or intramuscularly), famotidine (20 mg 2 times a day orally or intravenously) •• H+,K+-ATPase blockers (proton pump blockers) ) - omeprazole, rabeprazole 20 mg 2 times / day, lansoprazole 30 mg 2 times / day.
• Drugs that protect (envelop) the mucous membrane •• Sucralfate •• Bismuth tripotassium dicitrate (also has an antimicrobial effect against Helicobacter pylori).
Chronic atrophic gastritis • Drug therapy is carried out only during the period of exacerbation • Replacement therapy for secretory gastric insufficiency: natural gastric juice, pepsidil, hydrochloric acid with pepsin, acidin-pepsin (these drugs are contraindicated in the presence of erosions of the mucous membrane) • Replacement therapy for decreased excretory function of the pancreas glands (cholenzyme, pancreatin + bile components + hemicellulase, pancreatin, panzinorm forte) • Treatment of B12-deficiency anemia • Herbal medicine: herbal remedies that have an anti-inflammatory effect - infusion of plantain leaves, chamomile, mint, St. John's wort, valerian (1 tbsp. per glass of water) orally, 1/3–1/4 glass 3–4 times a day before meals for 3–4 weeks; plantain juice 1 tbsp. or plantaglucide 0.5–1 g 3 times a day • Drugs that improve tissue trophism and enhance reparative processes: nicotinic acid (1% solution IV from 1 to 10 ml for 10 days or IM 3–5 ml 20 days), solcoseryl 1–2 ml IM 20 days, inosine 0.2 g 3 times a day 40 minutes before meals 20–30 days, thiamine, pyridoxine, folic acid • Blockers of central and peripheral dopamine receptors for pain and severe dyspeptic symptoms (see below Reflux gastritis).
Reflux gastritis • Treatment is aimed at normalizing gastrointestinal motility and binding bile acids • To prevent the reflux of duodenal contents into the stomach, dopamine receptor blockers are prescribed (domperidone, metoclopramide, cisapride 10 mg 3 times a day 30 minutes before meals for 2-3 weeks ) • To neutralize bile acids that have a damaging effect on the gastric mucosa, chenodeoxycholic and ursodeoxycholic acids are used • To protect the mucous membrane from bile acids - antacids in the usual daily dose (aluminum-containing antacids have the ability to bind bile acids, so they are more effective).
Giant hypertrophic gastritis • Long-term treatment (2-3 months) • High-calorie, protein-rich diet • Antisecretory therapy • For treatment-resistant hypoproteinemia, repeated bleeding, surgical treatment (gastric resection) is indicated.
ICD-10 • K29 Gastritis and duodenitis
Application. Eosinophilic (allergic) gastroenteritis is a chronic disease characterized by predominantly eosinophil infiltration of the lamina propria of the gastric antrum mucosa, epithelium, pit glands with the formation of eosinophilic abscesses; characterized by damage to the small and large intestines, esophagus; often accompanies allergic diseases. Clinical picture: chronic diarrhea, abdominal pain, nausea, vomiting, weight loss, eosinophilia. Treatment: exclusion of allergy-provoking foods; diet No. 1; GCs provide long-term remission. ICD-10. K52.8 Other specified non-infectious gastroenteritis and colitis.