- home
- Coloproctology
- Sigmoid colon cancer
Sigmoid colon cancer
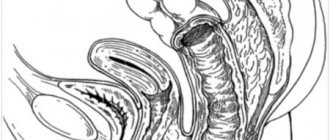
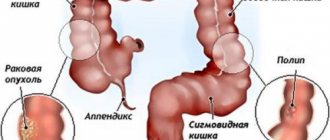
Sigmoid colon cancer is an oncological disease of part of the colon, in which a malignant tumor is formed from the epithelium of the mucous membrane. The sigmoid colon, located above the rectum, according to statistics, is one of the organs most often affected by cancer. Most of the oncologist's patients are people aged 45-65 years, with more cases among men.
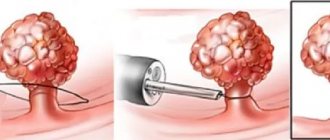
Depending on the direction of growth, an exophytic form of cancer is distinguished - a formation on a thick stalk grows into the intestinal lumen, and endophytic cancer, when the process spreads along the intestinal wall. In this case, ulcerations appear, the lumen of the intestinal tube narrows, the movement of intestinal contents is difficult.
Tumors of this location also differ in histological structure. Adenocarcinoma is more common - its poorly differentiated variety has an unfavorable prognosis and is characterized by early metastasis. Signet ring cell carcinoma, which is less common, also has a poor prognosis.
Among the negative factors that can lead to illness:
- diverticula, benign polyps susceptible to malignancy;
- diseases of the colon: colitis, Crohn's disease, atony, etc.
- digestive disorders: constipation, problems with peristalsis;
- alcohol abuse, smoking, unbalanced diet;
- some diseases: obesity, diabetes, etc.;
- hereditary predisposition.
Causes
Most of the reasons for the development of sigmoiditis, as an independent disease, lie in the anatomical and physiological characteristics of the sigmoid colon.
Firstly, the main function of the sigmoid colon is the final formation of feces, which can irritate the intestinal mucosa, contributing to the development of microdamages, and therefore creating the preconditions for inflammation.
Secondly, unlike other parts of the large intestine, the sigmoid colon has a curved shape, which delays the passage of intestinal contents through it. This structural feature increases the duration of irritation of the mucous membrane by feces, which increases the likelihood of inflammation.
In addition, reasons also include:
- intestinal infections, such as dysentery and amoebiasis. The bacteria that cause these infections produce toxins that destroy intestinal cells, forming erosions or ulcers. Due to the characteristics of the sigmoid colon, with such damage it is most vulnerable to the inflammatory process.
- intestinal dysbiosis. Among other things, the microflora in the intestinal lumen performs a protective function. With dysbacteriosis, the natural microbial environment is disrupted, which creates conditions for the proliferation of aggressive bacteria, and, consequently, for the development of inflammation.
- nonspecific intestinal ulcers, for example, Crohn's disease or ulcerative colitis. These diseases arise due to allergic factors, and can cause ulceration similar to that of intestinal infections.
- intestinal circulatory disorders (intestinal ischemia). The most common cause of such damage is atherosclerosis. With atherosclerosis, plaques form in the lumen of blood vessels, reducing the amount of blood passing through, thereby interfering with the nutrition of organs and tissues. In the intestine, under the influence of ischemia, areas of necrosis (necrosis) appear, which become the primary foci of inflammation.
- exposure to ionizing radiation – radiation sickness. Under the influence of radiation, some cell structures are destroyed, and free radicals appear - toxic compounds that can damage healthy cells of the body.
Chronic intestinal colitis, symptoms
Acute colitis of the sigmoid colon and rectum passes into the chronic stage if the disease is not cured in time. Symptoms appear from time to time, and in the chronic stage they bother the patient every day.
The following signs of the chronic stage of proctological disease are distinguished:
| 1. problems with bowel movements; | In chronic intestinal colitis, both diarrhea and constipation are common symptoms. Constipation occurs much more often, and is accompanied by colic in the stomach, bloating, and flatulence. Increased secretion of intestinal gases occurs after eating. |
| 2. disturbed structure of feces; | Feces have a strange greenish tint and a sour smell. The stool contains mucus, streaks of blood, and pus. |
| 3. nausea and vomiting; | If toxins enter the bloodstream during intestinal inflammation, nausea and vomiting occur. There is an unpleasant odor coming from the mouth. |
| 4. skin rashes; | In some cases, with colitis, intoxication occurs in the body. As a result, rashes appear on the skin, which requires the attention of a dermatologist and proctologist. |
| 5. weight loss; | Due to digestive problems, the patient loses his appetite. He is rapidly losing weight, which leads to hypovitaminosis and decreased immunity. |
| 6. impaired metabolism; | With colitis, metabolism is disrupted, anemia or anemia is observed. |
| 7. problems with blood vessels; | Colitis is accompanied by dizziness, low and high blood pressure. General weakness and drowsiness appear. |
Symptoms of intestinal colitis in men appear with excessive physical activity, drinking alcoholic beverages, and smoking. Painful sensations appear in the stomach and chest. Often these symptoms are confused with heart problems.
Kinds
Like most inflammatory diseases, sigmoiditis can be acute or chronic. In addition, there are the following types, differing in the nature of intestinal damage:
- Catarrhal sigmoiditis. The mildest form, in which only the upper layer of the intestinal epithelium is damaged.
- Erosive sigmoiditis. It is a continuation of untreated catarrhal disease and is characterized by the destruction of the intestinal epithelium with the formation of erosions on it - open, unprotected areas of the mucous membrane.
- Ulcerative sigmoiditis. This form appears with prolonged irritation of erosions on the surface of the intestine, as a result of which they turn into ulcers - deeper defects of the mucous membrane.
- Perisigmoiditis. It is the most severe form of the disease. Through the ulcerative surface, inflammation penetrates into the deep parts of the intestinal wall, reduces its mobility, and the adhesive process begins in the abdominal cavity (the process of connecting intestinal loops to each other).
CONSEQUENCES OF THE DISEASE
Lack of timely treatment is dangerous for the rapid development of complications, which often pose a threat to the patient’s life. The most common complications of the pathological process in the sigmoid colon include:
- toxic dilatation (expansion) of the large intestine;
- malignancy (malignancy) of the inflammation zone;
- perforation of the wall of the sigmoid colon with the development of internal bleeding;
- obstruction of the colon;
- purulent peritonitis of the abdominal cavity;
- septic blood poisoning;
- thrombosis of the mesenteric artery.
All these conditions are dangerous with a high risk of death. Therefore, if symptoms of sigmoiditis appear, you should immediately seek medical help.
Symptoms of sigmoiditis
Due to the variety of forms and causes of sigmoiditis, symptoms can vary greatly, but there are three main manifestations characteristic of any type of disease:
Pain in the left iliac region (lower left corner of the abdomen). The pain is intense and can often radiate to the leg or lower back. It should be remembered that the sigmoid colon initially has high mobility, which may result in a change in the localization of pain closer to the central line of the abdomen, or higher, towards the diaphragm.
Changes in the frequency and nature of stool. Diarrhea occurs most often, constipation occurs somewhat less frequently. Sigmoiditis is characterized by an increase in the frequency of the urge to defecate, which is explained by intestinal irritation. Feces are most often liquid, have a sharp, unpleasant odor, and you can see blood, mucus or pus in them.
Deterioration of the patient's general condition. Since during a long course of the disease the human body is depleted, loss of body weight, decreased performance and general well-being, and various sleep disorders are possible.
DIVERTICULOSIS: fiber plays the main role in its treatment
Claire Cheek, Fellow of the Royal College of Physicians Simon Radley, MD, Fellow of the Royal College of Physicians Queen Elizabeth Hospital, Birmingham, UK
How does diverticular disease manifest? What complications may develop? Which patients need to be hospitalized?
Colon diverticulosis is an acquired disease. It is believed that it is based on impaired peristalsis, which leads to the appearance of areas with high intraluminal pressure, pushing the mucous membrane through the submucosal and muscular layers. This occurs in relatively weak areas where blood vessels extend into the circular muscle.
Impaired peristalsis may occur due to the frequent passage of small volumes of stool with a low content of undigested food debris. Both circular and longitudinal muscle bundles usually hypertrophy, which leads to thickening and shortening of the colon. Diverticula and muscle hypertrophy are most often observed in the sigmoid colon, but the colon can also be affected in any part or completely.
The term “diverticulosis” simply reflects the presence of diverticula, not necessarily the clinical manifestation of the disease. Diverticulitis is a clinical and morphological concept that refers to inflammation of diverticula. Diverticular disease is a broader term that applies to diverticulosis and its complications.
Diverticulosis is very rare in people under 30 years of age, but its incidence increases with age, and by age 50, up to 30% of the population has colonic diverticula. The frequency of this pathology in men and women is the same.
Only 20% of people with diverticulosis eventually develop symptoms of the disease.
This disease is characteristic of Western countries, its pathogenesis is largely associated with insufficient fiber intake. It is observed less frequently in vegetarians and rural Africans.
Thus, environmental factors are believed to play an important role in the development of this pathology. Nevertheless, genetic factors seem to have a certain significance: in cases where diverticula appear at a young age or when they predominantly affect the right parts of the colon.
Clinical picture. Most patients with diverticulosis do not have any complaints. With uncomplicated diverticular disease, bowel dysfunction may occur, often accompanied by pain such as colic, flatulence and a feeling of fullness in the abdomen. These symptoms can sometimes be difficult to distinguish from irritable bowel syndrome.
Acute diverticulitis is characterized by pain in the left iliac fossa. Typically, there are signs of acute inflammation, namely: tachycardia, fever, local peritoneal phenomena and leukocytosis.
Perforation of an inflamed diverticulum can lead to abscess formation. Such patients often have a fluctuating fever and a painful mass in the affected area.
Diverticular abscesses often resolve spontaneously. However, large or nonabsorbing abscesses may require percutaneous drainage under ultrasound or CT guidance. Perforation of a diverticular abscess into the abdominal cavity causes purulent peritonitis, with local tenderness becoming diffuse.
The local inflammatory process associated with the diverticulum can lead to perforation of the wall of another organ lined with epithelium, resulting in the formation of a fistula. The most common cause of diverticular disease is colovesical fistulas, which occur when a diverticulum perforates into the bladder. When first seeing a doctor, patients with colovesical fistulas sometimes have no complaints of bowel dysfunction, but instead experience frequent urinary tract infections and/or pneumaturia.
Fistulas can also open into other organs - the vagina or loops of the small intestine, and occasionally enterocutaneous fistulas occur.
Diffuse peritonitis associated with diverticular disease is caused by the presence of free pus and/or feces in the abdominal cavity. Fecal peritonitis develops as a result of necrosis of the intestinal wall, leading to leakage of feces. The patient's condition can be very severe, with severe symptoms of peritonitis and septic shock.
Sometimes bleeding occurs from the vessels passing through the neck of the diverticulum, and more often it is profuse. Typically, such bleeding develops from a single diverticulum, located, as a rule, in the right parts of the colon.
Diverticular disease cannot be considered as a cause of occult bleeding from the lower gastrointestinal tract leading to iron deficiency anemia, for which other causes should be sought, such as neoplasms or angiodysplasia.
Inflammatory changes in combination with smooth muscle hypertrophy and scarring from previous attacks of acute diverticulitis may be sufficient to cause complete closure of the colonic lumen and acute obstruction. Incomplete obstruction due to scarring is manifested by unstable stools and abdominal pain such as colic. Using imaging techniques, it can be very difficult to distinguish strictures resulting from diverticular disease from malignancy.
Diagnostic methods. Diverticulosis is easily detected by irigoscopy and computed tomography (CT) with contrast.
| Figure 1. Irigoscopy: uncomplicated diverticulosis of the sigmoid colon | Figure 2. Irigoscopy: diverticular disease of the sigmoid colon. Fistula (arrow) connects the intestine to the bladder (B) |
Double-contrast irigoscopy identifies diverticula (see Fig. 1), any strictures, and can also help detect fistulas (see Fig. 2).
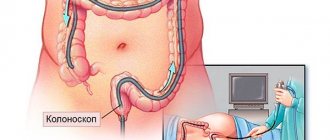
If in areas with severe diverticulosis it is sometimes not possible to reliably exclude small polyps or carcinomas, then it is necessary to perform a colonoscopy or flexible sigmoidoscopy.
Irigoscopy with double contrast can be performed only four to six weeks after relief of acute diverticulitis.
In acute pathological processes, other diagnostic techniques play a major role, such as CT and/or sonography.
Colonoscopy. Colonoscopy is usually performed on an outpatient basis. It allows you to clearly visualize diverticula and any pathology of the mucosa. This is the diagnostic method of choice in cases where the patient is admitted with rectal bleeding or during irigoscopy it was not possible to thoroughly examine the colon.
However, colonoscopy is sometimes difficult to perform because of the spasm observed with extensive diverticular disease, as well as because of rigidity or because of the diverticula themselves.
| Figure 3. Computed tomography with contrast: diverticular disease of the sigmoid colon (S) complicated by the formation of an abscess (A) containing a large amount of gas (arrow) |
Computed tomography and sonography. Contrast-enhanced CT is the study of choice in patients with acute diverticulitis.
Often during this procedure, a characteristic thickening of the walls of the colon with inflammation of the surrounding fatty tissue is detected. In complicated cases, CT scan reveals abscesses (see Fig. 3), gas and/or contrast material outside the bowel loops. Many departments practice drainage of abscesses in the abdominal cavity under CT control, which helps avoid surgical interventions in the acute phase of the disease. Sonography is slightly less sensitive but can detect wall thickening and large abscesses.
Other research methods. Occasionally, cystoscopy may be necessary to detect a colovesical fistula. Angiography and scanning with technetium-labeled red blood cells can help locate the source of blood loss from the colon.
Referral to hospital. Patients with abnormal stools, blood on rectal examination, or recurrent abdominal pain should be examined on an outpatient basis to determine the causes of these symptoms. Rigid sigmoidoscopy and irigoscopy or complete colonoscopy are the main methods used in this case. Asymptomatic diverticula occur in at least one in three people over 65 years of age. Therefore, diverticulitis can be reliably diagnosed only when there is an appropriate clinical picture and when no other diseases, especially malignant tumors, are detected.
A patient with acute diverticulitis without dysfunction of other body systems does not necessarily need to be treated in a hospital. In such cases, home treatment consisting of oral antibiotics (amoxicillin with clavulanic acid and metronidazole for five days) and drinking plenty of fluids is often sufficient. Analgesics and bed rest are also prescribed. If within a few days the pain does not stop or intensifies or becomes more widespread, and also if the patient develops systemic symptoms (for example, tachycardia or fever), then it is necessary to immediately refer him to the hospital.
| Figure 4. Complicated diverticular disease. The probe is inserted into the perforated diverticulum. The mucous membrane looks quite normal |
Patients with diffuse abdominal pain and/or signs of peritonitis should be urgently hospitalized.
Drug and surgical treatment. In uncomplicated cases, special nutrition may be sufficient for treatment. The patient is advised to eat a high-fiber diet and/or take medications that increase stool bulk, such as ispaghula husk. Patients should drink plenty of fluids.
Pain caused by smooth muscle spasms should be relieved with antispasmodics such as mebeverine. The role of surgical resection in uncomplicated cases remains controversial and should be reserved for exceptional cases.
Laporotomy and myotomy (dissection) of hypertrophied smooth muscle of the sigmoid colon have rightly been criticized and are currently only of historical interest.
Elective surgery. In case of complications, such as fistulas or strictures, surgical intervention is required with resection of the segment of the colon affected by diverticula and a primary anastomosis. For patients with recurrent diverticulitis, resection is offered in cases where their physical condition allows such an intervention - if other pathology is excluded.
One third of patients who are hospitalized for an attack of diverticulitis have to be hospitalized again in the next five years with the same pathology.
Elective surgery is associated with much lower complication rates and mortality; Resection and primary anastomosis can usually be achieved, although a stoma may sometimes be required.
Emergency surgery. For patients with generalized peritonitis, effective resuscitation measures with intravenous fluid and antibiotics are required before surgery.
Perforation of the colon is a serious situation, and almost half of patients with fecal peritonitis die. Purulent peritonitis, which develops as a result of rupture of a diverticular abscess, has a lower, but still significant mortality rate.
Patients with acute diverticulitis that does not respond to conservative treatment may also require surgery. In such cases, the inflamed segment with diverticula or phlegmon is resected, and it is usually possible to perform a primary anastomosis.
In case of extensive fecal or purulent contamination of the abdominal cavity, resection of the affected segment is necessary, but primary anastomosis is not always appropriate. In such cases, the rectal stump is sutured and the proximal colon is exposed to the skin as a final colostomy. This intervention is called Hartmann's operation.
After Hartmann's operation, in most cases it is possible to close the colostomy without any risk, and, according to numerous data, in 80% of cases the normal passage of intestinal contents is restored.
If complications develop, then exclusion of the affected segment from the intestinal function is carried out by applying a bypass anastomosis and establishing drainage of the abdominal cavity. But in such situations, this segment is not resected, which leads to a significant increase in mortality compared with primary resection. Therefore, the vast majority of surgeons refused such an operation.
In case of complications of diverticular disease, severe concomitant diseases and old age negatively affect the outcome of emergency surgery.
Literature
- Pemberton JH, Armsrong DN, Dietzen CD Diverticulitis. In: Textbook of Gastroenterology, 2nd edition (Ed. Yamada T). Lippincott. Philadelphia. 1995.
- Keighley MRB Diverticular disease. In: Surgery of the Anus, Rectum and Colon, 1st edition (Eds. Keighley MRB, Williams NS). W. B. Saunders, London. 1993.
Editor's comment
- In accordance with the “Standards for the diagnosis and treatment of diseases of the digestive system,” which are approved by order of the Ministry of Health of the Russian Federation No. 125 dated April 17, 1998, lactulose (Duphalac) is the first choice for diverticular disease with a tendency to constipation.
- In the Russian Federation, mebeverine is registered under the trade name Duspatalin
Note !
- Acute diverticulitis is characterized by pain in the left iliac fossa and is usually accompanied by signs of acute inflammation, namely tachycardia, fever, local peritoneal findings and leukocytosis
- Perforation of an inflamed diverticulum can lead to abscess formation. Such patients sometimes have a fluctuating fever and a painful mass in the affected area.
- Sometimes bleeding occurs from the vessels passing through the neck of the diverticulum, quite often profuse. Diverticular disease cannot be considered a cause of occult bleeding from the lower gastrointestinal tract leading to iron deficiency anemia
- Patients with changes in stool, blood on rectal examination, or recurring abdominal pain should be evaluated in an outpatient setting to determine the cause of these symptoms. Rigid sigmoidoscopy and irigoscopy or complete colonoscopy are the main methods used in this case. In uncomplicated cases, special nutrition may be sufficient for treatment. Patients are advised to eat a high-fiber diet and/or medications that increase stool volume, such as ispaghula husk.
- Pain caused by smooth muscle spasms should be relieved with antispasmodics. The role of surgical resection in uncomplicated cases remains controversial and should be used with great caution
What to tell the patient?
In uncomplicated cases
- The examination did not reveal any severe disease of the colon, including a malignant tumor.
- It is very important to pay attention to nutrition
- It is necessary to eat foods rich in fiber and take medications that increase the volume of stool
- You should drink more fluid
- Increasing the fiber content of your diet may initially increase pain and bloating. Stick to your diet anyway as these symptoms usually go away
- Surgery is risky and may not improve the condition.
For complications
- After the first attack, 30% of patients develop an exacerbation of the disease within five years, requiring hospitalization
- Economical surgery can be recommended for young patients
- When considering the possibility of economical resection for patients in the older age group, one should carefully weigh, on the one hand, the possibility of preventing relapses and relieving symptoms, on the other hand, the significant risk of postoperative complications
- Surgery is indicated for patients with fistulas
- If there are no contraindications, economical resection is recommended for patients with abscesses.
Diagnostics
Diagnosis and treatment of sigmoiditis can be carried out by a general practitioner, gastroenterologist, infectious disease specialist, or surgeon.
The main task in making a diagnosis is to carry out differential diagnosis with other inflammatory diseases of the intestines and abdominal organs, such as paraproctitis, ulcerative colitis, as well as with infectious diseases, such as dysentery, cholera, and intestinal dysbiosis.
The results of the following studies are used for diagnosis:
- Interview and examination of the patient, palpation of the abdominal organs. By conducting these studies, the doctor will be able to establish the exact localization of the lesion and draw a conclusion about which part of the intestine is involved in the inflammatory process.
- General blood and stool analysis. These studies will help to accurately determine the severity and nature of the inflammatory process.
- Sigmoidoscopy is performed to directly examine the mucous membrane of the large intestine. Based on the results of the study, it is possible to draw a conclusion about the form of the disease and the area of the lesion, as well as to exclude oncological diseases.
- X-rays are performed to differentiate sigmoiditis from intestinal obstructions.
- For women, data from a gynecological examination to exclude gynecological pathologies such as endometriosis, adnexitis, tubal pregnancy and some others that can give a similar clinical picture.
After collecting all the information, the doctor makes a final diagnosis and prescribes treatment.
Treatment of sigmoiditis
Treatment is prescribed depending on the cause of sigmoiditis.
1. For the treatment of sigmoiditis caused by intestinal infections, antibacterial therapy (Biseptol, Tetracycline, Ampicillin, Cefran) is prescribed, covered with bacterial drugs to protect against dysbacteriosis (Lactobacterin, Bifidobac and others).
Also, in chronic cases, intestinal antiseptics such as Intetrix or Smecta are prescribed.
2. To treat sigmoiditis caused by nonspecific inflammatory bowel diseases, use anti-inflammatory drugs that eliminate the underlying disease: Salazoperidazine, Prednisolone, Sulfasalazine.
To combat general intoxication processes, infusion therapy with solutions of glucose, blood plasma and iron supplements (for the treatment of anemia) is used. Also, bacterial preparations are prescribed to normalize the intestinal microflora.
3. For the treatment of ischemic sigmoiditis, the same regimens are used as for the treatment of sigmoiditis caused by nonspecific diseases. In some cases, if such therapy fails, surgery to plasticize the vessels feeding the intestines may be indicated.
In addition, as with any diseases of the gastrointestinal tract, a special diet No. 4 is prescribed, which involves the exclusion of spicy, fried, smoked foods, alcohol, and the maximum reduction in fat, carbohydrates and salt in the diet, and preliminary grinding of food before consumption.
Treatment of sigmoiditis is long-term; in most cases, recovery requires 1-2 courses of therapy, lasting from 1 to 3 months.
The nature of the course of ulcerative colitis
- Acute course
(less than 6 months from the onset of the disease):- a disease with a fulminant (sudden and rapidly developing) onset;
- a disease that develops gradually.
- Chronic continuous course
(absence of more than 6-month periods of remission against the background of adequate therapy). - Chronic relapsing course
(presence of more than 6-month periods of remission):- rarely recurrent (once a year or less);
- often recurrent (2 or more times a year).
Prognosis and complications
With proper treatment of sigmoiditis, in most cases it is possible to achieve complete recovery, but it should be understood that the treatment process is long and is accompanied by a lot of dietary restrictions.
If left untreated, inflammation may spread to adjacent sections of the intestine, most often to the rectum (proctitis).
Also, as inflammation progresses, the tightness of the intestine may become compromised, resulting in peritonitis - inflammation of the abdominal cavity, requiring extensive surgical intervention.
Types of intestinal colitis by location
The large intestine is separated from the small intestine using a special valve. This intestine consists of the colon, rectum and cecum. The colon is considered the longest. It is divided into sigmoid, descending, transverse and ascending parts. On average, the length of the large intestine in an adult is one and a half meters.
The following types of colitis are distinguished by location in the intestines:
- Pancolitis - the entire large intestine is affected.
- Typhlitis is accompanied by inflammation exclusively in the cecum.
- Transversitis - the transverse part of the colon becomes inflamed.
- Sigmoiditis - affects the sigmoid colon.
- Proctitis - inflammation of the rectum.
Patients are also diagnosed with rectosigmoiditis . With this disease, the sigmoid and rectum are affected, which is extremely dangerous for human health.
There are also left-sided, right-sided and diffuse colitis. Diffuse colitis is associated with the large and small intestines.