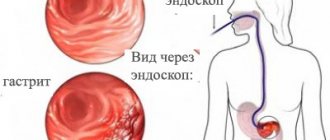
In the vast majority of cases, gastritis is caused by the bacterium Helicobacter pylori. Primary infection usually occurs in the family: through kissing, sharing dishes, unwashed hands... For several years after infection, no signs of the disease may be observed. However, inflammatory changes in the gastric mucosa are already underway, and at some point pain and disorders appear. Most often, this time coincides with studying in middle or high school. During this period in a child’s life, additional prerequisites for the occurrence of gastritis appear: great psycho-emotional stress and neglect of proper nutrition - lunch is replaced with chips, washed down with soda. A more rare cause of “school” gastritis can be stress. As soon as you “tease” the stomach with the same psycho-emotional stress, physical fatigue, the blood circulation of the gastric mucosa worsens, first, pinpoint hemorrhages and then erosions appear on its surface... At the same time, the test for Helicobacter gives a negative result. If the child also does not eat properly, then such gastritis is often accompanied by biliary dyskinesia and even such an “adult” disease as chronic pancreatitis (inflammation of the pancreas). Note to mom Signs of exacerbation of gastritis:
- aching, nagging pain in the pit of the stomach after eating (does not always occur);
- belching, unpleasant sour breath;
- a feeling of rapid satiety and rapid fullness of the stomach while eating;
- decreased appetite.
Treatment Diagnosis of gastritis in children is usually based on an analysis of clinical manifestations, gastroscopy results and Helicobacter testing. If the analysis shows that the disease is caused by Helicobacter, the doctor will prescribe various medications, including antibiotics. Correctly carried out therapy will rid the child of harmful bacteria. Sometimes parents ask whether it is possible to cope with such gastritis with diet alone? After all, he was treated somehow earlier, before antibiotics were created. It’s probably possible, but you’ll just have to create ideal conditions for the patient: exclude strong emotions; pick up from school to relieve stress; take you to the village, away from the bad environment and the influence of civilization; feed with fresh meat, milk from the cow and vegetables from your garden. But, alas, this will only help to avoid exacerbations. But it will not get rid of the infection that has settled in the stomach. And as soon as the teenager gets nervous, the unpleasant sensations return. Therefore, you still need to take modern medications. However, today's treatment methods do not negate either diet or folk recipes with herbs. Gastritis caused by stress is a little easier to treat. However, to remove the cause of the disease, it is necessary:
- provide the child with such a regime that he gets enough sleep;
- reduce psycho-emotional stress both at school and at home, stop stimulating games on the computer at least 1.5 hours before bedtime;
- strengthen the child’s autonomic nervous system, which communicates between the cerebral cortex and the digestive organs (by the way, a contrast shower in the morning and rubbing with a hard towel are very useful for strengthening);
- ensure that the child eats regularly and properly;
- see a gastroenterologist.
Important It is advisable that if gastritis caused by the bacterium Helicobacter pylori is detected in a child, all family members undergo examination and treatment. The likelihood of re-infection after a course of antibiotics is small, but it still exists.
Classification of gastritis
Gastritis can be acute or chronic. Both diseases differ in duration, course, causes and symptoms. In addition, acute gastritis can be cured, but it is impossible to get rid of chronic gastritis; with the help of nutritional correction and treatment, you can only achieve stable remission (temporary weakening or complete disappearance of symptoms).
Acute gastritis is an acute inflammation of the gastric mucosa that occurs due to exposure to a strong irritant that enters the stomach cavity.
Chronic gastritis is a disease characterized by chronic inflammation of the gastric mucosa with the gradual development of atrophy (reduction in the size and weight of an organ or tissue with weakening or complete cessation of their activity) of the gastric glands, which leads to a deterioration in the functions of the stomach. It is often accompanied by duodenitis - inflammation of the duodenal mucosa. The combination of gastritis and duodenitis is called gastroduodenitis.
Chronic gastritis has its own classifications, so it is worth talking about it separately.
About the disease
Gastritis is one of the most common diseases of the gastrointestinal tract (GIT), which occurs more often in children, starting from school age.
The disease is characterized by the formation of a focus of inflammation in the gastric mucosa. This is how characteristic clinical symptoms appear, which can be provoked by both external and internal causes. The pathology can be acute or chronic. The danger of the disease lies in the disruption of digestive function and the possible development of serious complications that worsen the patient’s quality of life. If left untreated, gastritis progresses from childhood into adulthood.
Chronic gastritis
According to the causes of chronic gastritis, there are:
- Primary (exogenous). As an independent disease.
- Secondary (endogenous). As one of the manifestations of other somatic pathologies.
By localization:
- Focal (fundal). When it affects the bottom of the stomach;
- Common. Affects several sections, most or all of the stomach (pangastritis);
- Combined (gastroduodenitis). It causes inflammation of the stomach and duodenum.
With the flow:
- Latent (hidden, asymptomatic);
- Monotonous (symptoms are always present);
- Recurrent (alternate periods of exacerbations and remissions).
By stages (phases) of the process:
- Exacerbation (severe symptoms);
- Incomplete clinical remission (unexpressed symptoms, inflammation of the stomach is visible during FGDS);
- Clinical remission (there are no symptoms, but during FGDS inflammation of the mucous membrane is detected);
- Clinical and endoscopic remission (no symptoms, no traces of inflammation during instrumental examination).
According to changes in the mucous membrane:
- Superficial (without atrophy);
- Hypertrophic (with the growth of the mucous membrane, the formation of cysts and polyps);
- Hemorrhagic (tendency to bleeding from the walls of the stomach);
- Erosive (with the formation of stomach ulcers);
- Subatrophic (slow small-focal atrophy);
- Atrophic;
- Mixed.
Development mechanisms
Causes of acute gastritis in children:
- Foodborne illness (a gastrointestinal disease that occurs after eating food containing bacteria and their toxins. Often occurs due to the consumption of rotten foods, unwashed fruits or dirty water);
- Long-term use of certain medications (salicylates, sulfonamides, glucocorticoids, digitalis preparations, etc.);
- Poisoning with household poisons;
- Allergy.
When a large number of bacteria enter the gastrointestinal tract, inflammation occurs. Excess fatty, spicy and poorly chewed food slows down the evacuation (removal) of stomach contents and worsens the secretory function of the organ (the secretion of digestive juice for digesting food). The food lump lingers in the stomach, it is saturated with enzymes, after which it disintegrates due to the action of bacteria, and the fermentation process begins.
Which leads to aggravation of the course and chronicity of the process.
Causes of chronic gastritis in children:
- The presence of the bacterial flora Helicobacter pylori (the same bacterium leads to ulcers). In 80-85% of cases it is what causes gastritis;
- Poor nutrition (eating rough, too hot or cold, fatty, spicy or poorly chewed food);
- Dry food;
- Eating 1-2 times a day or less often;
- Lack of vitamins, complete proteins and fats in the diet;
- Endocrine diseases;
- Kidney damage;
- Diseases of the cardiovascular system;
- Long-term use of medications (salicylates, sulfonamides);
- The source of infection in the oral cavity (disease of teeth and gums);
- Burdened heredity;
- Allergies.
The factors that cause acute and chronic gastritis are similar or even coincide. The main difference is the duration of their effect on the body. In acute gastritis, one contact with an irritant (expired cottage cheese or a large portion of fast food) is enough for an attack. In chronic gastritis, an irritating factor acts on the gastric mucosa for a long time and repeatedly, gradually leading to a decrease in the activity of the digestive glands.
Diet features
Proper nutrition is the key to minimizing relapses of gastritis.
- Regular fractional meals in equal portions.
- Only high-quality food, freshly prepared.
- Lack of fatty, spicy, smoked, fried foods containing a lot of spices and additives, raw vegetables, buns, legumes.
- Eating steamed or boiled foods.
- The presence in the menu of cereals, mashed potatoes, chicken, lean meat and fish, weak tea, cocoa with milk, honey, crackers, etc. on the recommendation of a doctor.
Symptoms of gastritis
Manifestations of acute gastritis begin to bother the child 8-12 hours after exposure to the etiological (causal) factor. Intoxication in children is more pronounced than in adults, so the clinical picture in children is more pronounced than in adolescents and adults.
The main symptoms of acute gastritis in children:
- General malaise (the child becomes lethargic, moody, sleepy or restless);
- Pale skin;
- Loss of appetite;
- Nausea and vomiting;
- Feeling of fullness or pain in the epigastrium (upper abdomen, above the navel);
- Chills;
- Increase in body temperature to 38°C;
- Belching with an unpleasant odor;
- Short-term diarrhea.
The duration of the disease is from 2 to 10 days.
Complaints from patients with chronic gastritis may be absent if the digestive process is not disturbed. That is, the mucous membrane is affected, but the compensatory mechanisms are sufficient to maintain the normal secretory function of the stomach, so that the person does not feel discomfort or changes in the gastrointestinal tract.
A clear clinical picture is characteristic of the exacerbation stage.
The main symptoms of chronic gastritis:
- Abdominal pain after eating (subsides within 1-2 hours);
- Feeling of heaviness in the epigastrium (upper abdomen, above the navel);
- Belching;
- Heartburn (discomfort and burning sensation behind the sternum);
- Unpleasant taste in the mouth;
- Vomiting, diarrhea (diarrhea), flatulence (bloating) are rare.
The duration of exacerbation ranges from several days to several months.
Gastritis in children: causes and treatment
Diseases of the digestive system are highly prevalent, and in the structure of pathology in children with MS (I) they occupy second place after diseases of the respiratory system.
The most common is gastritis. Gastritis is an inflammation of the gastric mucosa, which in turn leads to disruption of its functions. Like many other diseases, it can be acute or chronic.
What is gastritis?
Gastritis is an inflammation of the gastric mucosa, which in turn leads to disruption of its functions. Like many other diseases, it can be acute or chronic.
Acute gastritis occurs brightly, with pronounced manifestations, but after proper treatment you can forget about it forever. But chronic gastritis is a companion for life, and is characterized by periodic exacerbations. Stomach disease leads to the development of concomitant pathology of the entire digestive tract - diseases of the liver, biliary tract, pancreas, intestines, impaired absorption of certain foods and especially vitamins A, C, B vitamins, and the development of anemia.
Causes of gastritis in children
There are many reasons why this disease occurs. They should be known to all parents - after all, if you know about the causes of the disease, you can prevent its development or sound the alarm in time.
You can get gastritis. More recently, it was still believed that all gastritis is of non-infectious origin. But it has now been established that this is not the case! Infectious gastritis occurs as a result of the action of the infectious agent Helicobacter pylori. Therefore, parents suffering from this disease can simply infect their child through kissing, sharing cups and spoons, and simply through the toys they play with the baby.
Gastritis is a consequence of poor nutrition. Another common cause of gastritis in young children is poor nutrition. Frequent changes of formula in “artificial” babies, incorrect, irrational and untimely introduction of complementary foods - all this puts a huge strain on the fragile stomachs of the babies. Fast food also makes its harmful contribution. Eating chips, French fries, and Coca-Cola is an excellent breeding ground for gastritis.
Irrational and irregular nutrition, long intervals between meals, dry food, as well as characteristics of adolescence, when symptoms of increased secretion appear, are a predisposing factor for the development of gastritis in school-age children.
Overeating is one of the causes of gastritis in children. Many mothers literally force food into their child, believing that they bring him only benefit. But in fact, all this leads to the fact that the stomach cannot cope with the load, irritation appears, and then inflammation and gastritis.
Chocolate, cookies. The development of this disease in children is also facilitated by the consumption of chocolate, large quantities of cookies, hot and spicy foods. Pediatricians generally believe that chocolate can be given to children after 3 years of age, and even then in strictly limited quantities. Whereas some kids start enjoying candy from the age of one! Dear parents, remember that your child’s nutrition is the basis of his health.
Gastritis in children is caused by stress. Quite often, gastritis develops in young children due to stress. They can be caused by conflicts in kindergarten, and by an unfavorable environment at home (for example, when parents constantly quarrel with each other or often scold the child). Unpleasant conversations during meals have a particularly bad effect on the state of the gastrointestinal tract. Watching horror cartoons on TV is also not beneficial. Creating a calm, friendly atmosphere for a child is an excellent prevention of gastritis.
The causes of acute gastritis are often food allergies and poisoning. Therefore, carefully monitor the quality of the foods your child eats.
Chronic gastritis is most often the result of untreated acute gastritis. Therefore, do not self-medicate; let a doctor prescribe therapy.
In some cases, the cause of gastritis may be diseases of other organs of the gastrointestinal tract. For example, pancreatitis, cholecystitis, hepatitis, etc. Gastritis can also be provoked by foci of chronic infections - nephritis, caries, sinusitis, etc. Scientists have found that lamblia and worms, injuring the mucous membrane of the digestive tract, cause irritation and inflammation, which subsequently leads to gastritis.
Gastritis and heredity. But the role of heredity in the development of many diseases, including gastritis, cannot be denied. A mother or father suffering from this disease with genes can pass on a predisposition to increased secretion and gastritis to their children. In such a situation, a small error in nutrition is enough and the child gets sick.
Consequences of taking medications. Taking certain medications causes irritation of the gastric mucosa. Drugs that cause the development of gastritis include: salicylates, reserpine, some antibiotics, glucocorticoid hormones, cytostatics, etc. If irritation by drugs occurs day after day, then inflammation and gastritis develop. Unfortunately, in some cases the use of such drugs cannot be avoided (for example, when a child needs to undergo an entire course of therapy due to some disease). But sometimes parents independently treat the baby, give him all kinds of pills at their discretion, without thinking about the possible consequences. As a result, taking pills can cause gastritis. Therefore, make it a rule not to “prescribe” medications to your child, guided only by your own considerations. Medicines for a sick baby should be prescribed only by a qualified specialist - a pediatric doctor.
Gastritis often develops in school-age children, provoked by poor diet, long periods between meals, and stress.
Symptoms of gastritis in children
Parents need to know about the signs of gastritis in children. Usually, with gastritis, small children become restless and cry. They complain of pain in the stomach and grab it with their hands. Children refuse to eat, do not want to play and do not sleep well. Mothers also notice that the child becomes more lethargic and less active than usual. The child's skin is pale, bruises appear under the eyes, and the tongue is coated with a whitish coating. Nausea and vomiting are possible. Often such attacks of gastritis are accompanied by fever, diarrhea and headache.
All these signs should be a serious reason to see a doctor. After all, only a qualified specialist can conduct a full examination and prescribe adequate treatment.
The examination includes an examination of a small patient, if necessary, an examination of his stomach - gastroduodenoscopy, which is performed if necessary at any age.
Treatment of gastritis in children
In order for the treatment of gastritis to be successful, the first step, of course, is to establish the cause that led to the occurrence of this disease and eliminate it.
The main condition for treating gastritis is to create a calm, kind atmosphere around the baby so that he lives without stress, swearing and quarrels. Normalization of nutrition also plays a very important role. The child should eat food every day at the same time - this is how the food regime is created. Also make sure that your child chews his food thoroughly.
Drug treatment of gastritis in children is carried out only as prescribed by a doctor. Self-medication is unacceptable! After all, as we have already said, untreated acute gastritis gives rise to chronic gastritis.
The doctor selects the necessary medications, and according to indications, physiotherapeutic treatment is prescribed, which helps reduce pain and accelerates the recovery of the gastric mucosa.
Nutrition for gastritis
The child's diet must strictly correspond to his age. Complementary foods must be introduced according to a specific plan, under the supervision of a pediatrician.
If you have already introduced all complementary foods into your baby’s diet, you can use the following list of dishes:
Porridge. They need to be prepared in liquid, boiled form; puddings are also suitable.
Bakery products . White bread croutons and dry biscuits are suitable.
Soups. Only mucous, pureed vegetable or milk soups are suitable for babies. Rich meat and fish broths are contraindicated.
Meat and fish. Choose low-fat, well-chopped, cook it in the form of steam cutlets and meatballs.
Dairy products . Offer your child pureed cottage cheese, steamed cheesecakes and casseroles.
Eggs. They should be given to the patient in the form of a steam omelette.
Vegetables and non-acidic fruits are useful when baked or pureed.
Eat food at least 5-6 times a day, excluding black bread, hot and cold liquid dishes, fried foods, dough products, fatty and spicy foods from the diet.
Prevention of gastritis in children
Doctors never tire of saying that gastritis is easier to prevent than to cure. Therefore, make every effort to ensure that this misfortune passes your child.
The child requires strict adherence to the daily routine: he must sleep a lot (at least 10 hours), walk in the fresh air and play. It is not recommended to sit in front of the TV for a long time.
The family atmosphere should be calm and friendly. Try to completely protect your child from stress, do not yell at him or swear in his presence.
For a child under one year old, introduce complementary foods strictly in accordance with his age. And declare war on fast food in your home!
Make sure your baby always eats at the same time. The nutritional regimen improves the functioning of the gastrointestinal tract and promotes their full functioning.
Rushing, talking and playing while eating is unacceptable. Some children insist on watching cartoons while eating, and mothers agree, as long as the child does not act up. It is unacceptable! Be firm, calmly and gently explain to your baby that he will watch TV immediately after eating. The child should eat in a calm environment, without distractions and chewing food thoroughly.
Monitor your child’s health, promptly treat emerging diseases, visit a pediatric dentist, and fight pockets of chronic infection.
Contact Victory Baby !
The multidisciplinary private clinic Victory Clinic offers comprehensive medical care to both adult patients and children with various pathologies of the digestive system - from gastritis, cholecystitis, dysbiosis to peptic ulcers, inflammatory liver diseases and various types of neoplasms. Highly qualified gastroenterologists and hepatologists specialize in the prevention, diagnosis and treatment of diseases associated with disorders of the esophagus, stomach, duodenum, salivary glands, diseases of the small and large intestines, gall bladder and biliary tract, pancreas and liver.
Victory Baby has created all the conditions for early detection of diseases and their treatment. The team of pediatric doctors includes leading pediatricians and specialists in the field of child health.
Victory Clinic (multidisciplinary clinic)
Lenin Ave., 61/2
421-000
425-000
Victory Baby (children's multidisciplinary clinic)
Lenin Ave., 3/1
421-000
425-000
There are contraindications. Consultation with a specialist is necessary.
Diagnostics
Gastritis in children is treated by a pediatric gastroenterologist, but patients initially turn to a pediatrician, who refers the child for examination and then to a specialist.
At the appointment, the gastroenterologist interviews the child and parents to find out what is bothering the patient. In addition to assessing the data obtained, the doctor conducts an examination and identifies additional symptoms of gastritis in children:
- Moderate pain on palpation (palpation) of the epigastric region (upper abdomen);
- White coating on the tongue;
- Flatulence (bloating);
- Rumbling and feeling of “transfusion” in the stomach.
Additional diagnostic methods for gastritis:
- Complete blood count (signs of inflammation: leukocytosis - increased white blood cells, increased ESR).
- Biochemical blood test (markers of damage to other organs).
- Coprogram (determination of fat in feces, digested muscle fibers, occult blood).
- Fibrogastroduodenoscopy (FGDS). Visual assessment of the condition of the gastric mucosa. If necessary, a biopsy is simultaneously performed (a piece of tissue is taken) for histological examination. In the laboratory, the nature of the cells in the biomaterial is determined (cancerous or not).
- Fractional study of gastric contents. The stomach glands are artificially irritated with drugs, then the amount of enzymes they produce, hydrochloric acid and the pH level (acidity) are assessed.
- X-ray of the stomach. Changes in the relief of the gastric mucosa and its motor function are assessed.
- Electrogastrogram. The muscular activity of the stomach, that is, its motility, is studied.
A conclusion is drawn about the secretory, acid- and enzyme-forming functions of the organ.
Online consultation with a pediatrician
consultation cost: 500 rubles
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
Treatment
The treatment plan for gastritis in children depends on the form of the disease and its severity.
Therapy for acute gastritis includes:
- Bed rest for 2-3 days;
- Gastric lavage;
- Hunger in the first 8-12 hours after the onset of symptoms, then switching to liquid food (puree soups, low-fat broths, crackers without spices and salt, jelly and porridge), on days 5-7 the child is transferred to normal food;
- Drink plenty of fluids (preferably special solutions for rehydration);
- In case of severe dehydration, saline solution with 5% glucose solution is administered intravenously;
- Laxative for constipation;
- Antiemetics for vomiting;
- Antibiotics for infection;
- Additionally: B vitamins, enzymes for the gastrointestinal tract.
For chronic gastritis, the following is additionally prescribed:
- Eradication therapy (a special treatment regimen for the destruction of Helicobacter pylori (omeprazole + amoxicillin + imidazole/metranidazole/clarithromycin). Duration - 10 days. If ineffective, the regimen is changed.
- M-cholinergic receptor blocker to relax the smooth muscles of internal organs and suppress the secretion of the digestive glands.
- Antacids, histamine H2 receptor blockers to reduce gastric secretion.
Treatment is carried out until remission occurs, the duration of which is variable: from several months to several years.
Bacterial gastritis: is Helicobacter pylori really dangerous?
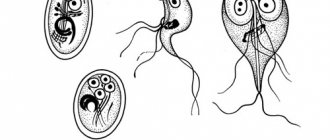
As we have already noted, bacterial gastritis, the culprit of which is the bacterium Helicobacter pylori (Helicobacter), is common in 80-90% of cases of all gastritis. This bacterium is transmitted through household contact (through dishes, kisses), and in the stomach it exhibits extremely aggressive behavior. In a short time, it multiplies in the mucous membrane and secretes destructive enzymes - urease. Under their influence, urea, which is contained in the stomach, turns into ammonia. Thus, Helicobacter breaks down the protective mucus, exposing the stomach wall, and then provokes inflammation, ulcers and metaplasia, which carries an oncological risk.
The bacterium Helicobacter pylori has been studied relatively recently. It was discovered in 1979 by Robin Warren
- Pathologist at the Royal Perth Hospital.
He studied the contents of the stomachs of patients with gastritis and accidentally discovered in many of them a spiral-shaped bacterium that multiplied safely even in a very acidic environment. A few years later, a desperate scientist-enthusiast named Barry Marshall
drank a test tube of Helicobacter cultures, after which he almost died from severe gastritis. In 2005, both researchers were awarded the Nobel Prize for their discoveries.
Today, WHO names the bacterium Helicobacter pylori as the No. 1 cause of stomach cancer worldwide. But don’t rush to get scared!
It is interesting that carriers of this bacterium in developed countries are 25-30% of the population, in Russia and Japan - 60-80%, and in Africa - 100%. And this has been going on for several millennia. Yes, predisposition to gastritis also depends on the population. In the body of a healthy person, there is a constant war between the immune system and Helicobacter pylori. The bacterium wins only sometimes, so many Helicobacter carriers do not develop inflammation of the stomach wall.
However, according to the European consensus recommendations and the Kyoto global agreement, treatment and observation for Helicobacter pylori is still necessary. Especially for residents of countries with a high risk of developing stomach cancer (Russia and Japan), as well as patients who are at risk for gastritis, that is, with poor heredity, concomitant pathologies, vitamin B12 deficiency, etc.
The gold standard for diagnosing Helicobacter are special test strips based on contact of blood with a reagent, as well as a 13C-urease breath test. If the result is positive, the patient is prescribed a gastroscopy. To get rid of Helicobacter pylori, a course of antibiotic therapy is usually sufficient. However, as we already know, antibiotics are not good for our stomach, since they also kill beneficial microorganisms. Therefore, only a doctor can select the necessary medications after studying the anamnesis and examination. The presence of Helicobacter pylori itself usually does not provoke gastritis - additional triggers are needed.
To prevent Helicobacter pylori invasion in the stomach, you should regularly visit the dentist (since this bacterium lives comfortably not only in the stomach, but also between the teeth, in tartar) and, of course, keep your hands, dishes, vegetables and fruits clean. If one of the family members is diagnosed with Helicobacter, this does not mean at all that you need to panic, quarantine the carrier of the virus and urgently treat everyone in the family.