general description
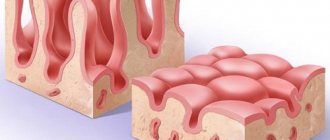
Ulcerative colitis or nonspecific ulcerative colitis is a chronic inflammatory disease of the mucous membrane of the large intestine, resulting from an imbalance of the immune system (antibodies are released to the own epithelium of the mucous membrane).
Cases of morbidity are registered in 0.3-0.5% of people, which is approximately 3-5 cases per 100 thousand population. The disease occurs in both men and women.
Ulcerative colitis can affect people of any age, most often occurring in the 25-35 and 60-80 age groups.
Diagnostics
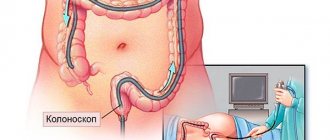
After examining and interviewing the patient with the collection of objective and subjective symptoms, the doctor prescribes a set of instrumental and laboratory tests.
Instrumental diagnostics:
- Colonoscopy, rectosigmoidoscopy - visual examination of the walls of the colon using endoscopic equipment. The technique makes it possible to determine the boundaries of ulcerative lesions, the intensity of inflammation, check for the presence of polyps and narrowing of the intestinal lumen, and also take biomaterial for histology.
- Irrigoscopy is an x-ray of the large intestine with contrast to identify areas of inflammation, narrowing, and neoplasms.
- Hydro-MRI is a contrast tomography to assess the condition of the intestine itself and the tissues surrounding it. Allows you to note the presence of fistulas, infiltrates and other structural changes.
- Ultrasound makes it possible to assess the structure of the intestine (wall thickness, presence of dilatations) and monitor its work over time.
Laboratory methods:
- histological analysis - examination of a biopsy of the intestinal mucosa;
- general blood test - level of leukocytes and erythrocytes, ESR, hemoglobin;
- biochemical analysis - c-reactive protein, immunoglobulin;
- coprogram for occult blood, leukocytes, erythrocytes;
- stool analysis for calprotectin (intestinal inflammation detector);
- culture for bacterial infection.
Causes of ulcerative colitis
Until now, the exact cause of ulcerative colitis is unknown.
Several reasons are considered in the scientific literature, but they are not fully understood:
- Genetic predisposition: close relatives have diseases such as Crohn's disease or ulcerative colitis
- Bacterial and viral infections
- Environmental factors (smoking, adherence to diets, long-term use of oral contraceptives)
Operation
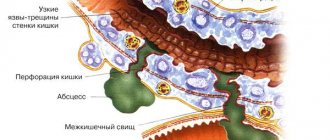
Surgical intervention is performed in exceptional cases, when the degree of damage to mucous tissues leaves no other option. Indications for surgery:
- perforations and fistulas of the intestinal wall;
- extensive blood loss (up to 100 ml per day);
- complication with the formation of megacolon;
- pronounced narrowing of the lumen and poor intestinal patency;
- purulent abscesses;
- cancerous degeneration of intestinal tissue.
Surgical options:
- complete or partial colectomy of the rectum, sigmoid, colon;
- partial excision of the rectum with ileoanal anastomosis - a section of the rectum is left and connected to the ileum for the natural removal of feces.
Are there other surgical alternatives?
Today, a method has been adopted in world practice in which a reservoir is created from the small intestine, connected to the anus. Typically, in this case, it is necessary to form a temporary ileostomy, followed by its closure after a few months.
The reservoir, the so-called pouch, functions as a storage device to reduce the frequency of bowel movements. The use of this technique allows one to achieve physiological stool holding. In cases of complications in the form of inflammation of the reservoir, antibiotic therapy can be carried out, sometimes it is necessary to resort to removal and the creation of a permanent ileostomy.
Treatment
Difficulties in the treatment of ulcerative colitis are associated with the unclear etiology of the disease, therefore the main goal of therapeutic measures is to relieve symptoms, achieve stable remission, prevent relapses, improve the quality of life and alleviate the physical and psychological condition of a person.
The treatment regimen is developed strictly individually depending on the phase and nature of the disease, the condition of the colon, duration of the disease, severity of symptoms, response to previous treatment, allergic status, risk of complications and a number of other factors.
The therapy complex includes:
- drug treatment;
- strict adherence to the diet;
- psychological support;
- surgical treatment for complications and lack of effect from other methods.
Medications
Drug therapy includes four main groups of drugs:
- glucocorticosteroids;
- non-steroidal anti-inflammatory drugs based on 5-aminosalicylic acid;
- immunosuppressants;
- genetically engineered biological products (GEBP).
In addition, symptomatic medications are prescribed: antidiarrheals, painkillers, drugs to replenish iron in the body, vitamins B and C and some others.
The form and duration of taking each type of medicine is selected strictly individually.
Important! Ulcerative colitis is a dangerous inflammatory disease; self-medication is absolutely unacceptable. Uncontrolled use of medications can lead to serious complications and significantly worsen the situation.
Diet
Diet plays a decisive role in the treatment of ulcerative colitis. In the acute phase, with pronounced symptoms, complete fasting with permission to drink only clean water may be recommended. The ban on food intake is tolerated by patients without problems, since during an exacerbation they lose their appetite for natural reasons. In especially severe cases, parenteral nutrition (intravenous administration of a solution with nutrients) is prescribed.
The diet for ulcerative colitis is aimed at normalizing the condition of the intestinal mucosa and stopping diarrhea. The most irritating to the mucous membrane are spicy, sour foods, marinated dishes, large amounts of fiber and roughage, and any alcoholic drinks.
For intestinal inflammation, foods high in protein of animal and plant origin are recommended. The amount of protein in the daily diet is calculated based on the norm of 1.5-2 grams per kilogram of weight. The main sources of protein are lean meat, boiled and baked fish, eggs, and legumes. It is not recommended to fry foods, as dishes prepared in this way severely irritate the mucous membranes of the stomach and colon.
Photo: nataliamylova / freepik.com
Recommendation During the period of exacerbation, many people develop intolerance to milk, so it is advisable to exclude dairy products and dishes based on them.
The optimal menu for ulcerative colitis corresponds to dietary table No. 4. The diet includes soups based on fish broth or lean meat, steamed minced meat dishes, porridge with water, pureed apples, boiled eggs, butter (no more than 5 grams per day), green tea, rosehip decoction and some other dishes and drinks.
Important! Any violation of the diet for ulcerative colitis threatens to worsen the disease!
Folk remedies
Folk remedies cannot be the main ones; they are only a way to alleviate the patient’s condition, but not a replacement for therapy. However, after consulting a doctor, to relieve symptoms of colitis, you can take decoctions of medicinal plants that have an anti-inflammatory effect and normalize stool. For example, to relieve symptoms of inflammation, a decoction of chamomile, an infusion of willow bark, and licorice root syrup are widely used, and to stop diarrhea, infusions and decoctions of oak bark, St. John's wort, quince fruits and seeds, and pomegranate peels are widely used.
Surgery
Surgical treatment is indicated if there is no effect from a strict diet and medications. Emergency surgery is indicated for suspected massive bleeding, peritonitis and the development of other complications.
During the operation, a resection of the large intestine is usually performed and the free end of the ileum is connected to the anal canal. If the situation allows, resection is performed partially while preserving intact areas of the colon. Surgical treatment is indicated in approximately 20% of patients.
Photo: wavebreakmedia_micro / freepik.com
Forecast
The prognosis for ulcerative colitis depends on the severity of the course, the presence of complications and concomitant diseases. With a mild form of the pathology and supportive anti-inflammatory therapy, more than 80% of patients do not experience relapses within a year. The risk of developing malignant neoplasms is limited to 3-10%.
Literature
- Adler DJ, Korelitz BI. The therapeutic e.cacy of 6-mercaptopurine in refractory ulcerative colitis. Am J Gastroenterol 1990;85:717-22.
- Ardizzone S, Molteni P, Imbesi V, Bollani S, Bianchi Porro G, Molteni F. Azathioprine in steroid-resistant and steroid-dependent ulcerative colitis. J Clin Gastroenterol 1997; 25:330-3.
- Bianchi Porro G, Prantera C, Campieri M, Petrillo M, Campanini MC, Gionchetti P et al. Comparative trial of methylprednisolone and budesonide enemas in active distal ulcerative colitis Eur J Gastroenterol Hepatol 1994;6:125-30.).
- Faubion WA Jr, Loftus EV Jr, Harmsen WS, et al.: The natural history of corticosteroid therapy for inflammatory bowel disease: a population-based study. Gastroenterology 2001, 121: 255-260.
- Gionchetti P, Rizzello F, Venturi A, et al. Comparison of oral with rectal mesalazine in the treatment of ulcerative proctitis. Dis Colon Rectum 1998;41:93-7.
- Green JRB, Lobo AJ, Holdsworth CD, et al. Balsalazide is more effective and better tolerated than mesalamine in the treatment of acute ulcerative colitis. Gastroenterology. 1998; 114:15-22.
- Guslandi M, Frego R, Viale E, Testoni PA: Distal ulcerative colitis refractory to rectal mesalamine: role of transdermal nicotine versus oral mesalamine. Can J Gastroenterol 2002, 16:293-296.
- Limann M, Galian A, Rutgeerts P, van Heuverzwijn R, Cortot A, Viteau JM et al. Comparison of budesonide and 5-aminosalicylic acid enemas in active distal ulcerative colitis. Aliment Pharmacol Ther 1995; 9: 557-62.
- Lichtiger S, Present DH. Preliminary report: Cyclosporin in treatment of severe active ulcerative colitis. Lancet 1990;336:16-9.
- Lichtiger S, Present DH, Kornbluth A, et al. Cyclosporine in severe ulcerative colitis refractory to steroid therapy. N Engl J Med 1994;330:1841-5.
- Marshall JK, Irvine EJ. Rectal corticosteroids versus alternative treatments in ulcerativecolitis: A meta-analysis. Gut 1997;40:775-81.
- Mulder CJ, Fockens P, Meijer JW, et al. Beclomethasone dipropionate (3 mg) versus 5-aminosalicylic acid (2 g) versus the combination of both (3 mg/2 g) as retention enemas in active ulcerative proctitis. Eur J Gastroenterol Hepatol 1996;8:549-53.).
- Odes HS, Fich A, Reif S, et al.: Effects of current cigarette smoking on the clinical course of Crohn's disease and ulcerative colitis. Dig Dis Sci 2001, 46: 1717-1721.
- Panes J, Esteve M, Cabre E, et al.: Comparison of heparin and steroids in the treatment of moderate and severe ulcerative colitis. Gastroenterology 2000, 119: 903-908.
- Pruitt R, Hanson J, Safdi M, et al. Balsalazide is superior to mesalamine in the time to improvement of signs and symptoms of acute ulcerative colitis. Gastroenterology. 2000; 118(Suppl 2 Part 1): A120-1.
- Rufle W, Fruhmorgen P, Huber W, Kimmig JM: Budesonide foam as a new therapeutic principle in distal ulcerative colitis in comparison with mesalazine enema: an open, controlled, randomized and prospective multicenter pilot study. Z Gastroenterol 2000, 38:287-293.
- Safdi M, DeMicco M, Sninsky C, et al. A double-blind comparison of oral versus rectalmesalamine versus combination therapy in the treatment of distal ulcerative colitis. Am J Gastroenterol 1997;92:1867-71.
- Sandborn W, Tremaine W, Leighton J, et al. Nicotine tartrate liquid enemas for mildly to moderately active left-sided ulcerative colitis unresponsive to .rst-line therapy: A pilot study. Aliment Pharmacol Ther 1997;11:661-71.
- Sutherland L, MacDonald JK Oral 5-aminosalicylic acid for induction of remission in ulcerative colitis. Cochrane Database Syst Rev (England), 2003, (3) pCD000543.
- Vrij AA, Jansen JM, Schoon EJ, et al.: Low molecular weight heparin treatment in steroid refractory ulcerative colitis: clinical outcome and influence on mucosal capillary thrombi. Scand J Gastroenterol 2001, 234(Suppl): 41-47.