Back to list Previous article Next article
24.08.2012
Tags:
gastrointestinal diseases, colitis
( 4 ratings, average: 5.00 out of 5)
Colitis is one of the most common pathologies of the gastrointestinal tract. It is an inflammatory disease of the large intestine (or rather, its mucous membrane) with pronounced symptoms , which we will talk about later. The disease can be complicated by inflammatory processes in the stomach and small intestine . It often accompanies some other acute and chronic diseases (influenza, pneumonia, typhoid, mumps, malaria, etc.).
It happens that this disease, due to similar symptoms, is confused with irritable bowel syndrome and for this reason is sometimes misdiagnosed. But since irritable bowel syndrome is not associated with the colon, then, accordingly, it cannot have anything in common with colitis.
Colitis
“Hand in hand” with dysbiosis
There are two forms of colitis - acute and chronic . In both the first and second cases, the infectious component plays a special role in the occurrence and development of the disease - most often bacterial dysentery . It can be triggered by other representatives of pathogenic microflora (for example, coli bacteria, staphylococci, streptococci, bacteria of the Proteus group, etc.). In other words, colitis goes “hand in hand” with dysbacteriosis. Inflammation can also be caused by previous intestinal infections and poor diet, as well as inadequate therapy with various medications. As practice shows, the causes of inflammation are indeed multiple. Let's summarize the main factors :
- infection in the gastrointestinal tract;
- infection with salmonella, staphylococci and other pathogenic microflora due to consumption of poor-quality food;
- the presence of worms (but not in all cases);
- inadequate, monotonous diet (mainly carbohydrates);
- allergies to certain types of food;
- chronic constipation;
- alcohol abuse;
- neglect of personal hygiene rules (for example, touching food with dirty hands);
- long-term use of certain antibiotics that can provoke dysbacteriosis;
- intoxication (poisoning with lead, arsenic and its preparations, mushrooms);
- nervous and emotional tension, stress.
Colitis ulcerosa - all Stages
Diagnostics
The complex of mandatory diagnostics includes macro- and microscopy of stool, coprogram, detection of helminth eggs, as well as bacteriological culture of stool. A general blood test is prescribed to determine the presence of signs of inflammation.
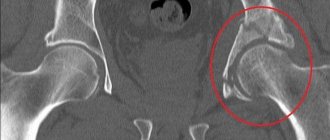
Contrast irrigoscopy is also performed to visualize the anatomical and functional features of the large intestine. Colonoscopy makes it possible to thoroughly examine the condition of the mucous membrane of the entire colon. During this study, it is also possible to obtain biopsies of the intestinal mucosa necessary for histological examination.
To exclude hemorrhoids, anal fissures, paraproctitis and other proctological pathologies, the proctologist performs a digital examination of the anus.
Acute colitis: causes, symptoms, treatment
This form of the disease is caused by staphylococci, streptococci, salmonella and dysentery microorganisms . It also occurs as a result of common infections (influenza, acute respiratory viral infections, acute respiratory infections, measles), allergies or intolerance to certain medications (usually antibiotics). Often, with acute colitis, the stomach and small intestine become inflamed. As a result, according to the “domino principle,” the normal functioning of other organs of the gastrointestinal tract is disrupted. Depending on the nature of the damage to the large intestine, doctors diagnose several types of acute colitis, namely: catarrhal, ulcerative, erosive, and sometimes fibrinous .
The main symptoms include:
- cramping abdominal pain and bloating;
- the presence of mucus and blood in the stool;
- diarrhea (diarrhea).
The disease usually begins suddenly and, as a rule, with a bowel disorder. Patients feel sick and have no appetite . I am tormented by vomiting and constantly thirsty. They complain of general weakness, a sharp deterioration in health and fever . However, vomiting and diarrhea have their advantages: doctors attribute these manifestations to protective reactions. That is, in this way the body tries to get rid of the poisons that have gotten inside.
Symptoms of acute colitis may depend on the location of the inflammation. For example, when the left half of the colon is affected, pain manifests itself most sharply. Before defecation, they usually intensify and radiate to the perineum and sacrum. Stools are very frequent, up to 20 times a day (sometimes more). The stool has an uneven consistency: dense masses “float” in blood or copious mucus. The areas of the descending and sigmoid colon are painful to palpation. This is where rumbling and splashing sounds are detected.
Colitis
This symptomatology can manifest itself over several weeks and, if left untreated, the acute form usually becomes chronic. Such undesirable developments can be prevented with timely assistance.
Thus, treatment of acute colitis includes the following measures :
- drinking plenty of fluids to replenish fluid losses in the body . It is recommended to drink a specially prepared solution that is well absorbed by the intestines: add a teaspoon of salt and seven to eight teaspoons of sugar per liter of warm boiled water. You can drink mineral water and weak tea, but coffee is undesirable because it affects intestinal motility and increases diarrhea. In some severe cases, fluid is administered intravenously.
- therapeutic fasting for one to two days. Then a strict diet is indicated until the symptoms of the disease completely disappear.
- taking activated carbon. Prescribed for the absorption of toxins in the large intestine.
- taking enzyme preparations, enveloping and adsorbent substances.
- physiotherapeutic treatment.
Causes
The causes of colitis can be a violation of the character and diet:
- poor eating habits;
- irregular poor nutrition;
- alcohol abuse;
- eating poor quality food.
Colitis often occurs as complications of gastrointestinal diseases (pancreatitis, chronic gastritis, hepatitis), and they can also result from food poisoning or intestinal infections. Taking various medications often has a negative effect on the intestinal flora; the resulting dysbiosis provokes inflammation in the large intestine. The reasons for the development of colitis include congenital pathologies of human development and functional insufficiency.
About the causes, symptoms and treatment of chronic colitis
Chronic colitis is a disease where the leading provoking factor is the presence of infection in the gastrointestinal tract . Its manifestations are “many-faced”. It occurs in the form of periodic exacerbations. The latter occur as a result of consuming foods that irritate the colon; manifestations of allergies; long-term use of various antibiotics; general fatigue.
The main symptoms of chronic colitis include:
- cramping pain in the abdomen (but does not always occur, more often accompanying the act of defecation);
- diarrhea alternating with constipation;
- secretion of mucus (in some cases mixed with blood);
- lack of appetite;
- nausea, belching of air, unpleasant taste in the mouth;
- a feeling of heaviness and distension in the abdomen (as a result of flatulence);
- a feeling of pressure in the epigastric region (often manifests itself in connection with gastritis);
- deterioration in general health (weakness, poor sleep, headaches, irritability, depressed mood).
Chronic colitis sometimes occurs as a consequence of functional disorders of the intestines (for example, with prolonged constipation). The causes also include dyskinesia (impaired motor function), which is associated with reflex effects from the gallbladder, bladder, prostate and other organs.
The basis for the treatment of chronic colitis (regardless of its etiology) is a dietary regimen. Drug therapy is effective only in cases where the cause is clearly established. When constructing a diet, the nature of dyspepsia (putrefactive or fermentative) and the state of the pancreas and its secretory function are taken into account . A too strict diet is not needed, as there is a risk of exhaustion and the development of hypovitaminosis, which will only complicate the course of colitis.
Strict dietary restrictions are allowed only during periods of exacerbation of the disease . Then foods that irritate the intestines both mechanically and chemically are excluded . Food is consumed boiled or pureed. Meals are split (6-7 times during the day). The consumption of table salt is limited (up to 8-10 g). Allowed: non-rich meat broth, steamed cutlets from lean meats, boiled fish (also low-fat), non-acidic cottage cheese, water porridge, juices, jelly. There is a strict taboo on black bread, spicy dishes, and various smoked foods. It is undesirable to eat lard and pork, goose meat and milk, sour cream, eggs, canned food, etc. Patients prone to diarrhea should not eat cold food, and the same applies to drinking.
If chronic colitis is accompanied by constipation, then the diet must include foods to stimulate intestinal function: minced meat, boiled vegetables and fruits.
Etiology and pathogenesis
The cause of chronic colitis is quite often the causative agents of intestinal infections - Shigella, Salmonella, Campylobacter, Yersinia, Clostridia, etc. Chronic colitis can be caused by helminths, protozoa (amoebas, Giardia, Trichomonas, Balantidia), as well as opportunistic and saprophytic flora. When chronic colitis occurs, the pathogen may not be detected, but dysbacteriosis remains, changes not only in the motor and enzyme-secreting functions of the intestine, but also in the structure of the mucous membrane, intensify, which contributes to the chronicity of the process.
Colitis of nutritional origin is quite common. They are caused by a violation of the diet, a monotonous diet containing a large amount of carbohydrates or proteins, a diet devoid of vitamins, frequent consumption of indigestible and spicy foods, and alcohol abuse. There are also “drug-induced colitis”, which occur with prolonged and uncontrolled use of a number of medications (laxatives containing anthraglycosides, antibiotics, salicylates, digitalis preparations, etc.).
Colitis of an allergic nature is possible (with food and drug allergies), and the allergic component is also inherent in the so-called post-infectious colitis, in which there is increased sensitivity to certain representatives of the intestinal microflora, the products of their vital activity and decay.
Colitis can be caused by congenital enzyme deficiency, in particular disaccharidase deficiency, due to constant irritation of the colon mucosa by products of incomplete breakdown of food. A similar mechanism, along with viscero-visceral reflexes, underlies some “secondary” colitis, such as colitis accompanying atrophic gastritis, pancreatitis with impaired exocrine function of the pancreas, and chronic enteritis. Developing dysbiosis contributes to the occurrence of an inflammatory process in the colon, but can also be its consequence, as is secondary disaccharidase deficiency.
In the pathogenesis of the disease, damage to the mucous membrane of the colon as a result of prolonged exposure to mechanical, toxic, and allergic factors is essential. The nervous apparatus of the intestine is involved in the pathological process, which leads to disruption of the motor and secretory functions of the colon and aggravates trophic disorders in the intestinal wall. Dysbacteriosis is of great importance, characterized by a decrease in the number of microorganisms constantly present in the intestine (bifidobacteria, E. coli, lactobacteria), a violation of the ratio of bacteria in various parts of the intestine, increased proliferation of opportunistic flora and the appearance of pathogenic flora. Secondary fermentopathy occurs. All this leads to the development of intestinal dyspepsia, immune disorders with the appearance of autoantibodies to antigens of the colon mucosa. The likelihood of autoimmunization in the progression and chronicity of the process is quite high.
Prevention of colitis
They say that disease is easier to prevent than to treat. Therefore, preventive measures are very important.
Prevention of acute colitis consists of following the norms of proper nutrition and a healthy lifestyle, maintaining hygiene and sanitary rules.
In the prevention of chronic colitis, special attention is paid to the prevention and timely treatment of acute colitis and especially dysentery. A large role in the prevention of diseases of the gastrointestinal tract is played by high-quality nutrition and, accordingly, maintaining the intestinal microflora in a healthy state . Not to mention the good condition of the chewing apparatus and strengthening of the nervous system.
Back to list Previous article Next article
Symptoms
Pain syndrome. Colitis pain is dull, aching, localized in the lateral and lower parts of the abdomen (usually on the left side). Sometimes the patient is not able to clearly localize the source of pain. They intensify after eating and weaken after passing gas and defecation. In addition, shaking, walking, and a cleansing enema can be causes of increased pain. Some patients complain of a feeling of heaviness, flatulence, and bloating.
Stool disorders. As a rule, stool disorders are characterized by constipation, sometimes alternating with diarrhea. Chronic colitis is characterized by diarrhea with the release of watery feces streaked with mucus.
Tenesmus. The so-called false urge to defecate is one of the characteristic symptoms of colitis. Often the result is the release of mucus.
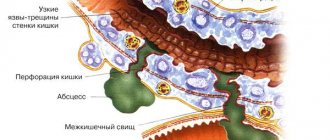
Possible complications of nonspecific ulcerative colitis
In complex cases of ulcerative colitis, various complications can develop, even threatening the patient’s life. These include intestinal ruptures, bleeding, severe infectious processes, accompanied by severe inflammation with high fever and general intoxication of the body. It is known that patients with UC have an increased risk of colorectal cancer.
If anti-inflammatory therapy does not have an effect, surgery is prescribed. Complications after surgery can include the occurrence of various infections - against the background of a general weakening of the body, progression of the disease in non-removed areas, or due to a rupture of the reservoir.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Sigmoidoscopy | 2 500 |
| Colonoscopy (video colonoscopy) | 7 000 |
| Irrigoscopy | 7 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Survey
Colonoscopy
- Cost: 24,400 rub.
More details
Diagnosis begins at a consultation with a gastroenterologist with examination and questioning. The nature of pain and discomfort and their duration play a big role. When diagnosing colitis, a whole range of instrumental studies is used:
- Colonoscopy. The most common endoscopic examination of the intestine.
- Sigmoidoscopy (examination of the rectum and anal area).
- Laboratory examination of stool (scatology, bacterial examination, inflammatory markers - calprotectin and others).
- X-ray examination using a contrast agent (irrigoscopy). Allows you to detect the exact localization of inflammation.
- Biopsy of the mucosa for histological examination. Allows you to clarify the diagnosis and exclude the possibility of a malignant neoplasm, which often manifests itself with the same symptoms as colitis.
Diagnostics is aimed at collecting the maximum amount of data about the disease. The doctor tries to find out the cause (it must be eliminated during treatment) and to clarify the localization of the inflammatory process. The more accurate the examination, the easier it is to choose effective treatment tactics.
Treatment
In 85-90% of cases, ulcerative colitis is treated conservatively. Features of the course of the disease are of primary importance in determining treatment tactics. The prevalence of the process, the severity of the attack during exacerbations, and the presence of complications are taken into account.
The diet for ulcerative colitis should exclude irritating factors for the intestines. The foods consumed should not cause the development of excessive fermentation processes in the intestines. At the same time, its goal is to ensure a complete supply of nutrients to the body. Especially proteins. Dietary table number 4. Very hot or cold food, food with a rough consistency is not recommended. Spicy, hot, fatty foods and alcohol are excluded. Some studies have suggested a beneficial role for oleic acid supplementation (eg, from uncooked olive oil) in the treatment of ulcerative colitis.
In the treatment of ulcerative colitis they use (as prescribed by a doctor):
1. Preparations of 5-aminosalicylic acid;
2. Some immunosuppressants, cytostatics;
3. Glucocorticosteroid drugs.
Classification of the disease
Depending on which parts of the intestine are affected by the inflammation, the following are distinguished:
- typhlitis;
- transversit;
- sigmoiditis;
- pancolitis;
- proctitis
The most common form is pancolitis. It affects the entire large intestine.
Due to their occurrence, they are distinguished:
- infectious;
- medicinal or toxic;
- ischemic - typical for patients after 55-60 years;
- radiation or radiation;
- ulcerative is the most common type.
Pathology can occur with the formation of erosions, ulcers, necrosis and hemorrhages. This is how catarrhal and erosive ulcerative colitis manifests itself.