Back to list Previous article Next article
24.08.2012
Tags:
gastrointestinal diseases, colitis
( 4 ratings, average: 5.00 out of 5)
Colitis is one of the most common pathologies of the gastrointestinal tract. It is an inflammatory disease of the large intestine (or rather, its mucous membrane) with pronounced symptoms , which we will talk about later. The disease can be complicated by inflammatory processes in the stomach and small intestine . It often accompanies some other acute and chronic diseases (influenza, pneumonia, typhoid, mumps, malaria, etc.).
It happens that this disease, due to similar symptoms, is confused with irritable bowel syndrome and for this reason is sometimes misdiagnosed. But since irritable bowel syndrome is not associated with the colon, then, accordingly, it cannot have anything in common with colitis.
Colitis
What causes intestinal colitis?
The main cause of the acute condition is various pathogenic bacteria, staphylococci or streptococci. The intestinal mucosa is sensitive and can become inflamed as a result of:
- Food poisoning.
- Allergic reaction.
- The effects of certain medications.
- Severe infectious disease.
The chronic form occurs as a result of the absence or ineffective treatment of acute colitis. Most often, chronic inflammation persists due to low immunity. The pathology can be supported by the presence in the body of other pathological foci in organs adjacent to the intestines.
Other common causes of chronic colitis:
- Worm infestation.
- Diseases of the pelvic organs in women.
- Uncontrolled use of antibiotics.
- Alcoholism.
- Chronic dysbacteriosis.
- Abuse of spices and spicy foods.
- Congenital intestinal defects.
Doctors include a monotonous diet and heavy food consumption as factors that provoke the disease.
Colitis is a common occurrence in children. The reason is that the protective barrier of the outer lining of the intestine is not yet fully formed. As a result, the organ cannot cope with various pathogenic microorganisms and an inflammatory process occurs.
In adulthood, ischemic colitis can occur. They are formed due to disruption of normal blood circulation in the mesenteric arteries (the vessel through which the intestine is attached to the peritoneum). This is a dangerous condition that requires urgent medical attention.
“Hand in hand” with dysbiosis
There are two forms of colitis - acute and chronic . In both the first and second cases, the infectious component plays a special role in the occurrence and development of the disease - most often bacterial dysentery . It can be triggered by other representatives of pathogenic microflora (for example, coli bacteria, staphylococci, streptococci, bacteria of the Proteus group, etc.). In other words, colitis goes “hand in hand” with dysbacteriosis. Inflammation can also be caused by previous intestinal infections and poor diet, as well as inadequate therapy with various medications. As practice shows, the causes of inflammation are indeed multiple. Let's summarize the main factors :
- infection in the gastrointestinal tract;
- infection with salmonella, staphylococci and other pathogenic microflora due to consumption of poor-quality food;
- the presence of worms (but not in all cases);
- inadequate, monotonous diet (mainly carbohydrates);
- allergies to certain types of food;
- chronic constipation;
- alcohol abuse;
- neglect of personal hygiene rules (for example, touching food with dirty hands);
- long-term use of certain antibiotics that can provoke dysbacteriosis;
- intoxication (poisoning with lead, arsenic and its preparations, mushrooms);
- nervous and emotional tension, stress.
Colitis ulcerosa - all Stages
Classification of the disease
Depending on which parts of the intestine are affected by the inflammation, the following are distinguished:
- typhlitis;
- transversit;
- sigmoiditis;
- pancolitis;
- proctitis
The most common form is pancolitis. It affects the entire large intestine.
Due to their occurrence, they are distinguished:
- infectious;
- medicinal or toxic;
- ischemic - typical for patients after 55-60 years;
- radiation or radiation;
- ulcerative is the most common type.
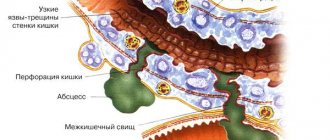
Pathology can occur with the formation of erosions, ulcers, necrosis and hemorrhages. This is how catarrhal and erosive ulcerative colitis manifests itself.
Literature
- Adams, S. M., & Bornemann, P. H. (2013, May 15). Ulcerative Colitis. American Family Physician, 87(10), 699–705. https://www.aafp.org/afp/2013/0515/p699.html
- Khalili H. et al. Physical activity and risk of inflammatory bowel disease: prospective study from the Nurses' Health Study cohorts //Bmj. – 2013. – T. 347. – P. f6633.
- Bressler B. et al. Clinical practice guidelines for the medical management of nonhospitalized ulcerative colitis: the Toronto consensus //Gastroenterology. – 2015. – T. 148. – No. 5. – pp. 1035-1058. e3.
- Fedorak RN Probiotics in the management of ulcerative colitis //Gastroenterology & hepatology. – 2010. – T. 6. – No. 11. – P. 688.
- Koutroubakis IE Recent advances in the management of distal ulcerative colitis //World journal of gastrointestinal pharmacology and therapeutics. – 2010. – T. 1. – No. 2. – P. 43.
- Panaccione R. et al. Treatment algorithms to maximize remission and minimize corticosteroid dependence in patients with inflammatory bowel disease //Alimentary pharmacology & therapeutics. – 2008. – T. 28. – No. 6. – pp. 674-688.
Main signs of colitis
Symptoms vary depending on the type of disease. Acute colitis is characterized by an abrupt onset. A person complains of the following symptoms:
- diarrhea;
- widespread abdominal pain;
- vomiting;
- flatulence;
- cutting or burning pain in the rectal area;
- feverish condition.
Colitis stool usually contains blood or mucus. Due to frequent vomiting, symptoms of dehydration occur: weakness, hypotension, pale skin, thirst.
Chronic inflammation has a sluggish course. Manifestations are mild. Periods of exacerbation and calm are characteristic. The following signs may indicate the presence of inflammation in the large intestine:
- bowel dysfunction;
- aching pain, mainly in the side and lower abdomen;
- characterized by increased discomfort after eating or during active movements;
- constant bloating;
- belching;
- unpleasant taste in the mouth;
- heartburn.
A distinctive feature is that thermal procedures (heating pad, bath, mud procedures) lead to an increase in the intensity of pain. 80% of patients with this diagnosis experience a decrease in appetite.
Gastrointestinal allergies in children
Gastrointestinal allergy is a lesion of the gastrointestinal tract of an allergic nature, which ranks second among the pathologies associated with food allergies [1, 2].
Gastrointestinal allergies are caused by food allergens.
In the first place is an allergy to cow's milk proteins, which contains up to 15 antigens, of which the most active are αS1-casein and γ-casein. In second place is chicken egg white. In third place are fish and seafood.
Among dietary fibers of plant origin, cereals such as wheat, rye, oats, and buckwheat play a role. There are currently many reactions to rice and soy. Allergic reactions can be caused by fruits (citrus fruits, apples, bananas, etc.), berries (raspberries, currants, etc.), vegetables (tomatoes, carrots, beets).
Risk factors for developing gastrointestinal allergies
Risk factors for the development of gastrointestinal allergies include:
- genetic factors - increased frequency of HLA-B8 and DW3 antigens;
- antenatal factors leading to intrauterine sensitization of the fetus: abuse of obligate allergens by a pregnant woman, ARVI, use of antibiotics, occupational hazards, etc.;
- childbirth by cesarean section, which leads to disruption of intestinal microflora;
- early artificial feeding;
- hygienic factors: reduction of antigenic microbial load due to small families and improved living conditions.
The development of gastrointestinal food allergy is based on:
- decreased oral tolerance to food allergens;
- allergic reaction in the gastrointestinal tract;
- development of allergic inflammation in the mucous membrane of the gastrointestinal tract.
Reasons for decreased oral tolerance to food allergens:
In young children:
- functional immaturity, including enzymatic deficiency;
- secretory IgA deficiency;
- excessive intestinal antigenic contact;
- immunosuppressive effects of past viral infections.
In older children:
- a consequence of exposure to intestinal irritants, helminths, and intestinal candidiasis.
Types of allergic reactions that cause gastrointestinal allergies:
- IgE-mediated;
- non-IgE-mediated;
- immune complex and cell mediated.
In response to the allergen, type 2 T helper cells are activated - Th2 cells, which secrete interleukins IL4, IL5 and IL13, which switch the B lymphocyte to overproduce IgE. IgE is fixed on target cells: mast cells, basophils. When the allergen re-enters, an antigen-antibody reaction occurs, the release of preformed mediators (histamine, etc.) and the synthesis of new ones (leukotrienes, prostaglandins), which cause the early and late phases of the allergic reaction. In the early phase of the allergic reaction, mediators act on the mucous membrane of the gastrointestinal tract, which in this case is the shock organ. Mediators cause spasm of smooth muscles (intestinal colic, abdominal pain), hypersecretion of mucus (vomiting, diarrhea) and swelling of the mucous membrane of the gastrointestinal tract. In the late phase of the allergic reaction, migration of eosinophils, activated T-lymphocytes, and production of pro-inflammatory cytokines to the site of inflammation is noted, which maintains chronic allergic inflammation in the mucous membrane of the gastrointestinal tract [3–6].
Less commonly, non-IgE-mediated allergic reactions may occur in the pathogenesis of gastrointestinal allergies:
- Immune complex reactions - in response to an allergen, IgG and IgM are synthesized, immune complexes are formed, complement is activated, which leads to the release of allergy mediators and the development of immune inflammation in the gastrointestinal tract.
- Cell-mediated reactions - sensitized T-lymphocytes are formed, releasing cytokines leading to allergic inflammation.
The non-IgE-mediated type develops: enterocolitis due to food protein, proctitis.
There is a dependence of the clinical manifestations of gastrointestinal allergies on the level of sensitization and the age of the child.
Forms of gastrointestinal allergies
Depending on the level of sensitization, the following forms of gastrointestinal allergies are distinguished:
Oral allergy syndrome
- allergic esophagitis;
- allergic gastritis;
- intestinal colic;
- allergic enteropathy;
- allergic colitis;
- signs of cheilitis, gingivitis, glossitis: swelling of the lips, oral mucosa, tongue;
- recurrent aphthous stomatitis.
Allergic esophagitis
In young children:
- resembles a clinic of pyloric spasm: vomiting within one hour after feeding;
- severe pain during eating.
In older children:
- feeling of numbness, burning along the esophagus;
- pain in the throat and behind the sternum;
- difficulty swallowing due to dyskinesia and edema of the esophagus.
Allergic gastritis
For allergic gastritis, a few minutes after ingesting the allergen:
- cramping pain in the epigastrium;
- recurrent vomiting.
Allergic enteropathy
Recurrent diarrhea that occurs after ingestion of a food allergen.
Intestinal colic
- the onset of an attack after feeding a food allergen;
- loud shrill scream;
- redness of the face, pallor of the nasolabial triangle;
- the stomach is swollen and tense, the legs are pulled up to the stomach, the feet are cold;
- arms are pressed to the body.
Allergic colitis
- abdominal pain 12–36 hours after eating;
- presence of glassy mucus in the stool;
- rectal bleeding - hemocolitis.
Severe forms of gastrointestinal allergies
Severe forms of gastrointestinal allergies include allergic gastroenterocolitis with clinical symptoms such as:
- repeated vomiting;
- bloating;
- frequent loose stools;
- large amounts of mucus and blood;
In older children, prolonged antigenic irritation of the gastrointestinal mucosa can lead to the formation of ulcers.
Features of gastrointestinal allergies
Features of gastrointestinal allergies in children are:
In children under 3 years of age:
- abdominal pain (in infants, intestinal colic is more common);
- flatulence;
- unstable stools (up to 5–6 times a day, liquefied with mucus, sometimes blood);
- regurgitation, vomiting;
- obvious and hidden intestinal bleeding leading to anemia;
- symptoms are associated with ingestion of food allergens and disappear after eliminating them from the diet.
In children from 3 to 6 years old:
- symptoms of gastric dyspepsia are more pronounced: heartburn, nausea, vomiting;
- less often than at an early age, symptoms of intestinal dyspepsia occur: flatulence and diarrhea;
- abdominal pain is less intense than in infants;
- symptoms are associated with ingestion of food allergens and disappear after eliminating them from the diet.
In school-age children:
- the clinical picture is more blurred;
- Abdominal pain is the most common;
- manifestations of gastric dyspepsia (belching, heartburn, nausea);
- manifestations of intestinal dyspepsia (constipation);
- decreased appetite and complete aversion to the product that caused the allergic process.
Diagnosis of gastrointestinal allergies
When diagnosing gastrointestinal [7, 8] allergies, the following is necessary:
1. Collection of allergy history:
- hereditary history of allergies;
- the child has skin or respiratory allergies.
2. Determination of clinical features:
- connection of the disease with food allergens;
- abdominal pain, intestinal colic;
- dyspeptic symptoms (vomiting, loose stools with clear mucus and blood);
- normal body temperature, no intoxication;
- positive dynamics after eliminating the allergen and prescribing antihistamines.
3. Laboratory research methods include:
- complete blood count - eosinophilia;
- coprogram - light mucus and red blood cells in the stool;
- endoscopy: esophagus, stomach, duodenum - pale mucous membrane, mucus, semolina symptom, linear grooves;
- histology ≥ 20 eosinophils per field of view.
4. Specific allergological examination:
- skin tests with food allergens (scarification, prik-test);
- determination of total IgE;
- determination of allergen-specific IgE and IgG4.
Treatment of gastrointestinal allergies
Treatment for gastrointestinal allergies includes:
- diet therapy with the elimination of causally significant allergens (highly sensitizing and individually intolerant foods are excluded);
- pharmacotherapy:
- antihistamines;
- membrane stabilizers;
- enterosorbents;
- enzymes.
Diet therapy in infancy
When breastfeeding: a strict hypoallergenic diet for the mother. Foods with high sensitizing activity and individually intolerable foods are excluded from the diet.
When artificial feeding, only medicinal mixtures are prescribed:
- protein hydrolysates: complete - whey and casein;
- Soy formula is used in children older than 6 months. Their use is limited because sensitization quickly develops to them;
- mixtures based on New Zealand goat milk: Nanny classic from birth to 1 year, Nanny 1 with prebiotics for children from 0 to 6 months, Nanny 2 with prebiotics for children from 6 months to 1 year, Nanny 3 - for children over 1 year.
There are differences in the protein composition of New Zealand goat's milk from cow's milk. It contains virtually no αS1-casein; the main casein protein is β-casein. This proportion is close to the composition of human milk. A less dense clot forms in the stomach. Its digestion is greatly facilitated. The formation of a soft casein curd accelerates the breakdown of whey proteins. The complete digestion of goat's milk proteins explains the low risk of allergic reactions when consuming New Zealand goat's milk.
Benefits of New Zealand Goat's Milk Formulas:
- there is practically no αS1-casein, which is the main protein in cow's milk that causes allergic reactions;
- does not contain sucrose and glucose;
- does not contain flavoring additives or dyes;
- The composition of Nanny formula for children from birth is as close as possible to human milk.
Contraindications to the use of Nenny mixtures:
- lactase deficiency;
- allergy to goat's milk;
- An immunological examination revealed sensitization to goat milk proteins.
Features of introducing complementary foods to children with gastrointestinal allergies
Features of introducing complementary foods to children with gastrointestinal allergies:
- complementary foods are introduced no earlier than 5 months;
- vegetable puree only monocomponent;
- Dairy-free, hypoallergenic porridges, such as buckwheat, rice, corn. If you are not allergic to goat milk proteins, buckwheat and rice Bibikashi based on New Zealand goat milk are recommended;
- rabbit, horse meat, turkey, pork, lamb, beef.
Sample menu for a 7-month-old child with food allergies who is bottle-fed:
- 6 hours. Nanny 2 mixture with prebiotics 200 ml.
- 10 hours. Buckwheat Bibikasha 200 ml.
- 14 hours. Vegetable puree from zucchini 150 ml, meat puree (rabbit meat) 50 g.
- 18 hours. Nanny 2 mixture with prebiotics 200 ml.
- 22 hours. Nanny 2 mixture with prebiotics 200 ml.
Whole goat's milk is not recommended for infants. This is an unadapted product. It contains too high a level of minerals, which puts an increased burden on the child’s digestive system and kidneys, and an insufficient amount of vitamins and especially folic acid, which can cause the development of megaloblastic anemia.
Pharmacotherapy
Antihistamines: from 1 month of age - Fenistil (drops), Suprastin (tablets) 2-3 times a day, from 6 months - Zyrtec (drops) - 1 time a day, from 1 year - Erius (syrup) 1 time a day day. The course of treatment is 2–3 weeks.
Membrane stabilizers in the period of remission - Ketotifen 2 times a day, Nalkrom 3-4 times a day. The course of treatment is 2–3 months.
Enterosorbents. During an exacerbation period, 10-14 days - Enterosgel (paste, gel) 2-3 times a day, Smecta, Filtrum, Laktofiltrum.
Enzymes - Creon, Mezim forte, Pancitrate 2-3 weeks.
Symptomatic therapy: for vomiting - Motilium, for flatulence, intestinal colic - Espumisan, Sab simplex.
Prevention of gastrointestinal allergies
In risk groups for the development of food allergies, which includes children with a family history of allergic diseases, it is recommended:
- observance of a rational diet by the pregnant woman and during lactation. If a pregnant woman has an allergic reaction, highly allergenic foods are excluded from the diet;
- elimination of occupational hazards;
- smoking cessation;
- breastfeeding until at least 4–6 months of life;
- Early (before 4 months of life) introduction of complementary foods is not recommended;
- if breastfeeding is impossible for children at risk of developing allergic diseases, it is recommended to use partial protein hydrolysates or Nanny mixtures based on goat milk: Nenny classic, Nenny 1 with prebiotics, Nenny 2 with prebiotics, Nenny 3;
- formation of the child’s tolerance to the action of common allergens.
Literature
- Baranov A. A., Balabolkin I. I., Subbotina O. A. Gastrointestinal food allergy in children. M.: Publishing house "Dynasty". 2002. 180 p.
- Khaitov R. M., Pinegin B. V. Assessment of human immune status in normal and pathological conditions // Immunology. 2001. No. 4. P. 4–6.
- Gómez-Llorente C., Muñoz S., Gil A. Role of Toll-like receptors in the development of immunotolerance mediated by probiotics // Proc Nutr Soc. 2010, Aug; 69(3):381–389. Epub 2010 Apr 23.
- Shanahan F. Nutrient tasting and signaling mechanisms in the gut V. Mechanisms of immunologic sensation of intestinal contents // Am J Physiol Gastrointest Liver Physiol. 2000, Feb; 278(2):G191–196.
- Van der Sluys Veer A., Biemond I., Verspaget HW et al. Faecal parameters in the assessment of activity in inflammatory bowel disease // Scand J Gastroenterol. 1999; 34(Suppl 230): 106–110.
- Mantis NJ, Forbes SJ Secretory IgA: arresting microbial pathogens at epithelial borders // Immunol Invest. 2010; 39 (4–5): 383–406. Review.
- Brandtzaeg P. Update on mucosal immunoglobulin A in gastrointestinal disease // Curr Opin Gastroenterol. 2010, Nov; 26(6):554–563.
- Chahine BG, Bahna SL The role of the gut mucosal immunity in the development of tolerance versus development of allergy to food // Curr Opin Allergy Clin Immunol. 2010, Aug; 10 (4): 394–399.
T. G. Malanicheva*, 1, Doctor of Medical Sciences, Professor N. V. Ziatdinova*, Candidate of Medical Sciences S. N. Denisova**, Doctor of Medical Sciences
* State Budgetary Educational Institution of Higher Professional Education KSMU Ministry of Health of the Russian Federation, Kazan ** State Budgetary Educational Institution of Higher Professional Education Russian National Research Medical University named after. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow
1 Contact information
What complications can there be?
Without appropriate and timely treatment, inflammation of the mucous membrane can lead to functional disorders. The most common are:
- the appearance of a scar, which leads to a narrowing of the lumen of the large intestine;
- internal bleeding;
- tissue necrosis, which leads to the development of peritonitis;
- non-traumatic perforation or rupture of the intestine;
- acute obstruction due to the formation of adhesions.
These conditions pose a threat to human life. It is important to consult a doctor at the first manifestations of the disease.
Left-sided intestinal inflammation
With left-sided inflammation, the left side is affected. Diagnosed in most cases. This type of colitis is diagnosed when the descending colon, rectum and sigmoid colon become inflamed. The patient is concerned about constipation, increased intra-abdominal pressure, irritation of the mucous membrane and the appearance of anal fissures.
, mucus and blood impurities are found in the stool . The patient feels a frequent urge to defecate, but mucus with small amounts of feces comes out of the body.
Diagnosis of pathology
Only a gastroenterologist can make the correct diagnosis. For this purpose, it is mandatory to order a scatological examination. It includes chemical, microscopic and bacteriological examination of stool in the laboratory. The Gregersen reaction test is also performed. This test aims to detect blood in the stool.
The doctor also recommends the following instrumental studies:
- X-ray of the abdominal cavity.
- Intestinal endoscopy (colonoscopy).
- Irrigoscopy - x-ray with the introduction of contrast into the colon. Allows you to accurately detect the inflammatory process and the boundaries of its spread.
It is imperative to exclude diseases such as polyposis and intestinal cancer. A warning sign is blood during and after bowel movements. This condition requires a comprehensive and thorough study. Consultation with doctors of related specialties is recommended.
What to do if a trial diet excluding cow's milk protein does not work?
- if the child is breastfed, reconsider the mother’s diet (what if hidden milk protein still appears) or try to exclude other, rarer allergens - soy, chicken eggs, wheat
- if the child is on hydrolyzate, switch to an amino acid mixture
Please note - soy is also a common allergen in itself (up to 0.5% of the population), and in people with an existing allergy to milk protein, the frequency of cross-allergy to soy is from 15% to 50%.
We also take into account other reasons for the periodic appearance of blood in the stool:
- Dermatitis around the anus
- Fissure of the anus - usually in the presence of dense stool in a baby, usually on artificial feeding. A visible fissure in the anus in the presence of soft stool does not exclude allergic proctocolitis.
- Infections. Usually, if a child has such classic intestinal infections as salmonellosis or dysentery, the child has obvious signs of intoxication, and with campylobacteriosis, the baby’s well-being may be relatively good.
- Blood clotting disorders (very rare, usually there are other manifestations of bleeding)
How to treat intestinal colitis
During the period of exacerbation, as well as in severe cases of acute colitis, a person must be hospitalized. Treatment on an outpatient basis is carried out only after acute symptoms have resolved and there are no complications.
Therapy is aimed not only at combating inflammation, but also at reducing the sensitivity of the intestinal mucosa. At the first stage, doctors’ efforts are concentrated on eliminating signs of dehydration and normalizing the functioning of all parts of the intestines.
In chronic cases, an important treatment method is to follow a special therapeutic diet.
Diet therapy
Nutrition is adjusted at any stage of the disease. In the acute phase, it is necessary to help the intestines, so all heavy, difficult-to-digest foods are excluded from the diet. The list of prohibited products includes:
- smoked meats;
- sugar, sweets;
- meat, including broths;
- legumes;
- salt, vinegar;
- vegetables fruits;
- all products that are aimed at improving intestinal motility.
The amount of salt per day should not exceed 8-10 grams. Dishes should be served stewed, boiled or pureed. Steaming is allowed, without adding fat. Meals should be frequent, small portions. There are no restrictions on water intake.
During the period of exacerbation, the gastrointestinal tract should be spared as much as possible. To do this, you must strictly follow all the recommendations of your doctor. On average, a special diet is prescribed for 3-5 days. This is enough to relieve acute symptoms.
Conservative treatment
If therapeutic nutrition is ineffective, as well as when concomitant gastrointestinal diseases are detected, a course of antibacterial drugs is necessary.
The dose and duration of the course are selected by the doctor individually. The purpose of antibiotics is to reduce the number of pathogenic microorganisms. When dysbiosis increases, the microflora is restored with the help of probiotics and prebiotics.
If agreed with a doctor, medicinal herbal infusions can be used as an additional treatment. They help control inflammation, reduce pain and manage diarrhea.
If worms and protozoa are detected in the tests, a course of antiparasitic therapy is recommended. Sometimes it is advisable to use sorbents and intestinal antiseptics.
The inflammatory process in the lower intestines is well controlled with local anti-inflammatory treatment. For this purpose, anal suppositories and microenemas are prescribed. They help not only regulate intestinal motor function, but also have a local analgesic and bactericidal effect.
If the patient complains of constipation, laxatives, suppositories or enemas are indicated. To improve local immune forces, vitamins and immunostimulating drugs can be prescribed.
Surgical method of treatment
Surgery is recommended only in exceptional cases when there is a risk to human life. These include all complications of colitis - the development of peritonitis, intestinal rupture, internal bleeding.
Relative indications for surgical treatment may be partial intestinal obstruction or lack of positive dynamics during drug therapy.
Surgery is often performed for advanced ulcerative colitis. To do this, a coloproctectomy is performed - radical removal of the colon.
Intestinal colitis: prognosis and prevention
If you seek medical help in a timely manner and follow the prescribed diet and treatment, the prognosis is favorable. After the acute period is over, performance is fully restored and well-being improves.
But to increase the duration of the remission period, a person with colitis needs to eat properly throughout his life. Long fasting or strict diets are excluded. You should forget about snacks on the run, fast food, as well as fatty, spicy and smoked foods.
It is also necessary to treat all gastrointestinal diseases in a timely manner. It is important for women to visit a gynecologist annually to identify inflammatory diseases in the pelvic organs at the initial stage.
It is recommended to undergo sanatorium-resort treatment in health institutions that specialize in gastrointestinal pathologies.
Boost your immunity and eliminate bad habits. Try to avoid prolonged stress. If you suspect you have colitis, treatment should only be prescribed by a gastroenterologist after a thorough examination.