We have cured more than 2,000 patients who were considered hopeless. Most of these patients were treated unsuccessfully for a long time (some for 35 years) in leading clinics both in our country and in foreign clinics in Israel, Germany and Switzerland. Moreover, we treated all of them on an outpatient basis - not a day of bed rest was required.
If you have an urgent question or acute pain, you can contact the doctor by phone:
8 Andreev Dmitry Yurievich
Examples of patients with trophic leg ulcers treated in our clinic (photos before and after treatment):
See all patient reviews
Over the past 20 years, we have managed to come a long way - from the creation and use of tissue extracts containing growth factors, to cellular technologies and the development of a series of original wound dressings with recombinant growth factors. In the photographs you can see the patents we received for these developments.
What is a trophic ulcer
The traditional medical description of a trophic ulcer is not always understandable to the common man. Experts define this pathology as “a hard-to-heal tissue defect, mainly in the lower extremities.”
To put it simply, a fairly deep open wound forms on the skin in the area of the foot, ankle or lower leg, which does not heal for weeks.
Traditional treatment with antiseptics or ointments has virtually no effect; moreover, an infection can get into the wound, which will aggravate the situation.
Diet
Your diet should be balanced and rich in all essential vitamins and minerals.
If you are overweight, then try to get rid of it. Follow one of the many weight loss regimens, reduce the amount of carbohydrates and fats.
Raising the lower limbs
This is one of the most important aspects of the prevention of trophic varicose ulcers of the legs. Elevate your legs above heart level, thereby improving circulation and reducing venous congestion. This will speed up the healing process of ulcers and prevent their reoccurrence after healing.
Let us recall here that raising the lower limbs on a stool while sitting on a chair is a waste of time and a useless exercise, since it does not contribute to the return of blood from the legs to the heart.
Pathogenesis (mechanism of initiation and development of the disease)
Most often, trophic ulcers occur when there is a violation of blood circulation in the arteries and veins of the lower extremities or difficulty in the outflow of lymph through the capillaries.
Also, a trophic ulcer can occur due to varicose veins. In varicose veins, blood flow slows down, pressure increases, tissues receive less nutrition and metabolic products accumulate.
Due to stagnation of blood, the walls of the veins can swell and blood clots form. This makes the situation worse. Blood circulation in small capillaries of the skin and subcutaneous tissue suffers especially severely, and the processes of skin renewal and regeneration are disrupted. In such a situation, any minor defect leads to the fact that the wound cannot heal normally.
Trophic ulcers can occur when arteries or lymphatic capillaries are damaged.
If the arteries become narrowed or clogged with atherosclerotic plaques, blood circulation in the legs is disrupted, and the tissues cannot fully regenerate. As a result, the slightest wound on the skin does not heal for a long time, becoming larger and deeper. Damaged cells and ichor released from the wound are a breeding ground for bacteria that increase inflammation, provoke suppuration and complications.
A trophic ulcer heals very poorly; without complete treatment and active treatment, infection may spread, even leading to gangrene and sepsis. And with reduced sensitivity (for example, due to diabetes), a person may not notice the wound for a long time, which will lead to suppuration and the formation of an ulcer.
Diagnostic measures
To diagnose a trophic ulcer, a doctor only needs to conduct a routine visual examination. It is much more important to identify what exactly caused its development.
Laboratory research
1. Submission of general and biochemical blood tests. The results of this analysis reveal an increased number of red blood cells, which makes the blood more viscous and impairs blood circulation. An increased number of leukocytes indicates the presence of an infection.
2. Coagulogram is a comprehensive blood test that allows you to evaluate its coagulation ability, as well as the biochemical systems responsible for the balance of coagulation and fibrinolysis
3. Bacteriological study. A smear from the affected area will help determine whether there are pathogenic bacteria, their type, the level of microbial contamination of the lesion, and the sensitivity of bacteria to antibiotics in order to select appropriate antibacterial therapy.
4. Histological examination. A very important test that allows you to exclude oncological pathology and assess the depth and extent of microscopic changes
5. Rheumatic tests. Especially in young patients and in unclear clinical situations, the analysis determines the autoimmune process due to which the connective tissue is affected. As is known, autoimmune disease also contributes to damage to the bloodstream.
Instrumental research methods
After a conversation with the patient and a routine examination, an ultrasound duplex angioscanning of the veins of the lower extremities is mandatory. At the same time, the patency of deep and subcutaneous venous vessels, the severity and extent of reflux, as well as the condition of the perforating veins of the leg are assessed. Ideally, the ultrasound is performed by the vascular surgeon himself. Thus, the information content and diagnostic value of the technology significantly increases. This is evidenced by personal long-term clinical experience. In parallel, we can always evaluate the patency of the main arteries, which plays an important role in choosing the optimal treatment. Ultrasound is accessible, low cost, simple, and non-invasive.
MSCT angiography. It is a special CT method that will help to study in detail the bloodstream along its entire length. In 3D mode (the so-called “virtual angioscopy”), a detailed study is carried out of the condition of the blood vessels, and any structural change in the arterial and venous walls is revealed. The technique is especially indispensable for high occlusions of the venous bed, lymph circulation disorders, various anomalies in the structure of veins and vascular malformations. It should be noted that MSCT angiography is unsafe for health, since it is associated with a high radiation dose, which limits the frequency of use.
Magnetic resonance imaging (MRI angiography). The modern high-tech method is expensive, but provides more accurate and detailed information. It reveals the condition of the internal organs and soft tissues, as well as the vascular bed, and how they function. It is not associated with ionizing radiation, since it has a completely different physical nature.
Laser Doppler flowmetry. Detects the slightest disturbance in the microcirculation of the wound area. This rather labor-intensive technology has not yet received general clinical application.
Types and classification of trophic ulcers
In the ICD-10 classification, trophic ulcers are assigned a separate code - L98.4. However, if ulcers that occur with varicose veins are described, they are coded as I83.0, I83.2. Depending on the specific cause of the formation of a trophic ulcer, other codes may be used.
Trophic ulcer: stages of disease development
The classification of trophic ulcers according to ICD-10 depends on the cause of its occurrence, stage of development, severity and associated complications.
Due to their development, trophic ulcers are classified into:
- Venous . They develop with varicose veins and deep vein thrombosis.
- Arterial . Such ulcers form when arteries are damaged by atherosclerotic plaques.
- Diabetic . They are formed due to high blood sugar levels, damage to the capillaries (microangiopathy) and nerves (polyneuropathy).
- Hypertensive . Martorell's syndrome - local arteriovenous shunts;
- Ulcers developing due to systemic diseases (blood diseases, metabolic diseases, collagenosis, vasculitis).
- Neutrotrophic . Occurring during denervation due to diseases or injuries of nerve trunks in areas of excess pressure.
- Scar-trophic . Formed on the surface of postoperative or post-traumatic scars.
- Phagedenic - progressive epifascial gangrene.
- Stagnant . They are formed against the background of circulatory failure and edema syndrome in cardiovascular pathology.
- Pyogenic . They develop against the background of purulent diseases of the skin of the extremities when personal hygiene rules are not observed.
- Specific and infectious - syphilitic, tuberculosis (Bazin's disease), leprosy, Buruli ulcer, tropical ulcer, tropical phagedenic ulcers, leishmaniasis, rickettsiosis, onchocerciasis.
- Malignant - skin neoplasms.
- Ulcers due to Lyell's toxic epidermal necrolysis.
- Ulcers with congenital malformations of the vascular system - angiodysplasia.
- Radiation.
- Ulcers that develop as a result of exposure to physical factors (burns, frostbite).
- Artificial . Artificial ulcers for the purpose of simulation and self-harm.
In the overwhelming majority of cases, trophic ulcers have a venous etiology and account for about 70% of the total structure of ulcers of the lower extremities i Dubrovshchik O.I. Trophic ulcers of venous origin: modern treatment options / O.I. Dubrovshchik [and others] // Journal of the Grodno State Medical University. - 2016. - No. 2. - P. 107-111. . The prevalence of trophic disorders and trophic ulcers in chronic venous insufficiency is 15-18% and occurs in 1-2% of the working population; with age, the frequency increases to 4-5% among patients over 65 years old i Kruglova L.S. Trophic ulcers of venous origin / L.S. Kruglova [and others] // Russian Journal of Skin and Venereal Diseases. - 2014. - No. 1. - P. 21-25. .
Based on the depth of tissue damage, there are 3 degrees of severity of trophic ulcers:
- I degree – initial tissue damage: erosions form, the upper layers of the skin are damaged.
- II degree – the defect extends to the skin and subcutaneous tissue.
- III degree – deep, severe defects with damage to the skin and tissue, as well as fascia and muscles. In extremely severe cases, tendons, joint capsules, and bone are damaged.
Uncomplicated trophic ulcers according to the classification (according to V. Ya. Vasyutkov, 1993) are divided into clinical stages:
- Stage I – a superficial ulcer appears. It is located on the skin, the surrounding tissues are bluish and thinned. The wound is dry, the tissue is swollen in the center, and pain is felt.
- Stage II – tissue destruction in the wound area intensifies, all layers of the skin are affected, unevenness and lumpiness are formed. The skin acquires a blue-violet tint at the edges, and in the center there is a weeping, purulent wound with plaque.
- Stage III – the bottom of the ulcer and its walls become denser, the surrounding tissues are swollen and painful.
- Stage IV - the ulcer grows to the sides, the surrounding tissues are pale, the edges of the wound bleed when touched, and a constantly weeping surface forms.
- Stage V – the ulcer area gradually clears and the healing process begins.
- Stage VI – the ulcer heals completely and scars form.
Skin care
There are many skin problems associated with varicose veins. One of them is varicose eczema. It is important to note here that ointments and creams alone cannot rid you of this problem. This should be combined with wearing compression stockings.
Frequent (several times a day) raising the lower extremities also helps to improve the situation.
Varicose veins and venous insufficiency over the years lead to trophic changes in the skin of the lower leg, followed by darkening (brown, dark brown, bluish, etc.). This pigmentation is the result of the release of blood elements from the lumen of the diseased vein into the surrounding tissue. Unfortunately, they are permanent in most cases and become lighter only after treatment.
Hyperkeratosis is another problem that gives the skin a scaly appearance. Frequent washing and treatment with moisturizing creams after the ulcers have healed gives the skin a healthier appearance.
Localization of trophic ulcers
Most often, trophic ulcers occur on the legs (leg, ankle or foot). The lesion can be single (one ulcer on one leg) or multiple (2 ulcers located on both legs or more). Ulcers can be symmetrical, located on the same areas of both legs or in different places.
Diabetic trophic ulcers most often affect the big toe on the plantar side, the upper part of the phalanges, the heel area and the plantar part.
Localization of trophic ulcers on the lower extremities
Causes of trophic ulcers
The most dangerous trophic ulcers are formed due to venous insufficiency, the formation of blood clots in the deep veins of the legs. They account for up to 70% of all cases.
Diabetic trophic ulcers occur quite often, especially when not only blood vessels are damaged, but also nerves. Less commonly, ulcers occur when arteries or lymphatic vessels are damaged.
Venous trophic ulcers are a complication of varicose veins, deep vein thrombophlebitis or postthrombotic disease. Such ulcers are formed due to serious circulatory disorders, blood clots and inflammation, tissue swelling.
In obliterating diseases of the arterial vessels, ulcers occur due to impaired blood flow to the tissues. This occurs when blood vessels narrow, lose elasticity, or in the presence of large atherosclerotic plaques.
Trophic ulcers in diabetes mellitus develop due to a sharp and prolonged increase in blood glucose. High blood sugar damages small vessels and nerve fibers, the sensitivity of the foot is impaired, the patient does not notice small wounds that do not heal for a long time and turn into ulcers.
Trophic ulcers occur when lymphatic capillaries are narrowed or completely blocked. The causes may be systemic diseases that damage the vascular wall (vasculitis, collagenosis), coagulation pathologies, thrombosis or hemorrhagic diathesis.
Non-healing trophic ulcers are possible with eczema, some forms of dermatitis (due to impaired functioning of the immune system) and infected wounds that were not treated correctly (for example, all affected tissue was not removed during surgical treatment).
The formation of a trophic ulcer is possible with extensive burns or frostbite, exposure to electric current or radiation.
Long-term non-healing ulcers are a symptom of certain chronic infectious diseases (leprosy, rickettsiosis, leishmaniasis, syphilis), cancer, and the toxic effects of drugs or chemicals.
Factors that increase the risk of trophic ulcers
Not all patients with the diseases listed above develop trophic ulcers. In addition to the main causes, there are risk factors in which ulcers occur more often or heal worse:
- excess body weight;
- long-term heavy loads;
- sedentary lifestyle;
- forced long stay in a supine position (for example, after a serious injury).
In the presence of these factors, blood circulation in the legs is often disrupted and tissue is damaged.
Trophic ulcers are more common in older people. It's connected with:
- chronic circulatory disorders (coronary artery disease, hypertension, atherosclerosis);
- overweight;
- lack of mobility;
- age-related changes in the immune system;
- slow skin regeneration.
An important factor that increases the risk of trophic ulcers is minor injuries, especially with diabetes mellitus or intermittent claudication.
In addition, neglect of personal hygiene rules, pustular skin infections, fungal infections of the nails and skin on the foot, wearing uncomfortable shoes and the formation of calluses are all additional factors in the formation of trophic ulcers.
Exercises
Exercises that improve blood circulation help ulcers heal faster and prevent relapses after treatment. Exercise helps improve circulation and return venous blood to the heart (in a word, it eliminates stagnation).
Try not to stand or sit for long periods of time without moving. If this is unavoidable, get up periodically and do exercises, or work your feet and toes, flexing and straightening them, to improve blood flow.
It is good to purchase an exercise bike and other home devices of this kind.
Symptoms of the onset of peptic ulcer disease
In order to recognize a dangerous condition in time and contact a specialist, it is important to know how trophic ulcers arise.
Initially, a focus of increased pigmentation appears; the tissues darken due to the accumulation of hemosiderin, a product of the breakdown of hemoglobin. After some time, a thickening of the skin and underlying tissues forms in the center of the dark area, the skin turns pale and shiny (white skin atrophy or pre-ulcerative stage).
Gradually, the skin atrophies, cells die, plasma leaks through the walls of blood vessels, which permeates the tissue, forming edema. Burning and itching appears, the tissues become inflamed.
When scratching damaged skin, scratches are formed, and then an ulcer, the edges of which gradually widen and the bottom deepens.
The size of a trophic ulcer is from 1-2 ruble coins to 10-20 cm in diameter, with uneven edges. Ichor or blood appears on the surface of the wound. If a microbial infection gets into the wound, then pus, dirty gray or greenish deposits appear, and the wound begins to emit an unpleasant odor. The edges of the wound are inflamed, the tissue around is swollen. Any touch causes pain.
When healing occurs, bright red bumps and nerves—granulation tissue—form in the center of the wound. The edges of the ulcer shrink and the size decreases. The pain decreases, the surface of the wound dries out. With proper treatment, the ulcer heals completely, but later, if blood circulation is not restored, it may reappear in the same place or in another area.
In the absence of treatment, the area and depth of the ulcer increases, a perifocal inflammatory reaction of soft tissues occurs - acute indurative cellulitis, and secondary infection occurs with the development of local and widespread purulent-inflammatory complications i Kruglova L.S. Trophic ulcers of venous origin / L.S. Kruglova [and others] // Russian Journal of Skin and Venereal Diseases. - 2014. - No. 1. - P. 21-25. .
Symptoms
By carefully monitoring the condition of the skin and their own well-being, patients who are at risk can independently predict the likelihood of TU. The following are considered warning signs of a problem:
- increasing pain in the legs;
- the appearance of severe swelling;
- decreased sensitivity;
- the formation of a bluish spot.
If the described signs are present, it is likely that a trophic ulcer will soon form on the leg, the stages of which will then increasingly replace each other.
Changes in skin quality speak volumes. When toxic substances accumulate, the coverings on the legs thicken and adhere much more tightly to the fiber. They cannot be pinched or even moved with your fingers. Pronounced pigmentation, dryness, and unnatural shine appear.
Over time, atrophy and active cell death are observed. The walls of the vessels allow plasma to pass through, filling the tissues and forming edema. Inflammation develops in the tissues, accompanied by itching and burning. The desire to scratch a blemish does not leave a person a chance not to violate the integrity of the affected area. The slightest damage, caused, for example, by shoes or clothing, opens the TP, which rapidly increases in both area and depth.
Methods for diagnosing the disease
If an ulcer appears, you should contact a surgeon or phlebologist. The doctor conducts an examination, prescribes tests and examinations to determine the cause of the development of trophic ulcers. The set of studies is determined individually, taking into account the main cause of the defect, the patient’s age, the number of ulcers, their location and concomitant diseases.
The first to be performed are standard laboratory tests - blood tests (general, biochemistry) and urine. It is necessary to determine blood sugar and cholesterol levels. If the wound becomes wet, the doctor does a culture of the discharge to determine the composition of the microflora. In some cases, cytological and histological techniques are used to diagnose the malignancy of a trophic ulcer, as well as to objectively assess the cellular composition of the ulcer base i Turkin P.Yu. Venous trophic ulcers: current state of the issue / P.Yu. Turkin [etc.] // Medicine. - 2021. - No. 1. - P. 41-45. .
An ultrasound examination of venous blood flow in the lower extremities (USDG) is performed. Doppler ultrasound allows you to obtain information about the state of the valve apparatus of the superficial as well as deep venous system, map perforating veins and correlate their location with the location of the trophic ulcer.
If arterial problems are suspected, arteriography or multislice tomography, MRI with contrast are prescribed to determine the specific location of the vessel damage.
Treatment methods for trophic ulcers
Treatment of trophic ulcers is an impact on the cause of the ulcer, restoration of blood circulation (or lymph circulation) in the affected tissues and elimination of the consequences. If blood flow is not restored, the ulcer will heal extremely slowly, and relapses are possible.
Doctors use a conservative approach using various medications or surgical interventions - treatment of ulcerative defects or excision of ulcers.
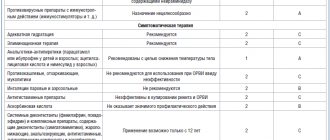
Conservative treatment
If the patient does not have indications for emergency surgery, the doctor prescribes conservative treatment. The basis of conservative treatment of trophic disorders of venous etiology is compression therapy, for which elastic bandages and compression hosiery are used. Compression therapy is complemented by a wide range of medications.
Drug treatment consists of local therapy (debridement) and the use of drugs that stimulate healing, suppress inflammation and prevent infection. In addition, systemic treatment is carried out - ingestion or injections of drugs with anti-inflammatory, venotonic, trophic effects, and the use of antibiotics.
If the wound is red, has severe inflammation, fever, or purulent discharge, antibiotics are used.
Local use of antibiotics is ineffective, so tablets or injections are used. They are selected according to the most likely pathogen. After receiving the culture results, the drug is replaced with a more effective one. The duration of therapy is from 2-3 weeks to 2 months. In some cases, antimicrobials may be combined with antifungal therapy.
For severe inflammation and pain in the wound area, nonsteroidal anti-inflammatory drugs are used, and painkillers are recommended.
To improve microcirculation and normalize metabolic processes, Actovegin, Pentoxifylline, antioxidants and agents that normalize the rheological properties of blood (antiplatelet agents) are used. Treatment is supplemented with desensitizing agents. They help eliminate itching and burning in the wound area and reduce swelling.
If trophic ulcers form against the background of varicose veins, then venotonics (for example, Phlebodia 600, Troxevasin, Detralex) and drugs that normalize blood circulation are indicated. These drugs are usually combined with antiplatelet agents that prevent blood clotting.
To treat trophic ulcers, local therapy (treatment of the affected area) is also necessary.
The ulcer area is treated with antiseptic solutions - hydrogen peroxide, chlorhexidine, miramistin. Gels or ointments for healing are used, a bandage, sterile wipes with silver ions, and ointments for healing are applied. As the wound heals, they switch to special patches for healing trophic ulcers. Any bandages should not be tight to ensure oxygen access and accelerate tissue healing.
Surgical treatment
If the lesion is extensive, the size of the ulcer exceeds 50-70 mm, and there is tissue necrosis or pus, then surgical intervention is indicated. The main goals of surgical treatment are to stop venous retrograde blood flow, cleanse the ulcer of fibrin and necrotic tissue, and, if necessary, replace the existing skin defect through skin transplantation.
In emergency situations, the edges of the ulcer are excised and all necrotic tissue is removed to prevent complications. The wound is treated with antiseptics and covered with bandages. An operation is performed to restore blood circulation in the affected vessel.
If the defects are extensive, skin grafting is performed from the thigh or bikini area. It covers the area of a large ulcer. Decompression fasciotomy can be performed to eliminate circulatory disorders in the lower leg and foot area and reduce swelling.
For complications of trophic ulcers on the foot, amputation of the toes or part of the foot may be indicated.
As an alternative to open surgical techniques, endovasal techniques for obliteration of the trunk of the great saphenous vein are currently used, such as radiofrequency ablation, endovasal laser coagulation and the use of cyanoacrylate glue VenaSeal i Turkin P.Yu. Venous trophic ulcers: current state of the issue / P.Yu. Turkin [etc.] // Medicine. - 2021. - No. 1. - P. 41-45. .
Physiotherapy
For the effective treatment of trophic ulcers of venous etiology, physiotherapeutic treatment methods are used, aimed at activating regenerative and reparative processes in the area of the ulcerative defect. Among them:
- infrared irradiation;
- SUV irradiation;
- UHF therapy;
- Microwave therapy;
- magnetic therapy;
- ultraviolet irradiation;
- darsonvalization;
- laser therapy;
- ozone therapy;
- medicinal electrophoresis.
The choice of one or another treatment method depends on the task at the rehabilitation stage and the stage of the wound process.
Folk remedies
On the recommendation of a doctor, it is possible to treat trophic ulcers at home.
The doctor will tell you in detail how to cleanse a trophic ulcer from pus, and select an ointment that is suitable to speed up healing and reduce pain and inflammation. Lotions with decoctions of medicinal herbs, compresses, or treatment of the defect area can be used.
Treatment of trophic ulcers at Dr. Gruzdev’s clinic:
Plastic surgery of trophic ulcers As varicose veins progress due to venous insufficiency, non-healing open wounds - trophic ulcers - can form on the legs.
More details
Endovasal laser coagulation (EVLC) If you have varicose veins, this does not mean that you will have to have surgery! New medical technologies make it possible to get rid of this disease without surgery.
More details
Adhesive obliteration of veins VenaSeal Non-surgical treatment of chronic venous insufficiency and varicose veins using VenaSeal bioadhesive.
More details
Magnetotherapy Vascular diseases nowadays occupy one of the leading positions in the general list of diseases.
More details
Laser therapy Laser is a focused beam of light that affects tissue, relieving inflammation, eliminating stagnation in tissue.
More details
General rules during treatment
1. Conscientiously follow medical prescriptions;
2. If possible, prevent the increase in swelling of the tissues of the lower leg and foot. To remove excess fluid from the body, you need to:
- follow a certain diet, that is, do not eat salty, fatty foods. Maximum salt restriction.
- Make sure that the daily urine output matches the amount of fluid you drink.
- In relatively rare cases, taking diuretics is allowed. Which medicine should be agreed with your doctor. This should only be used as an aid, and not the main method of getting rid of edema (!).
- Use compression garments. The compression class and type of knitwear (stockings, knee socks) depend on the severity of hemodynamic disturbances in the veins of the affected limb. As a rule, in this situation, compression stockings of classes II-III are prescribed. It is allowed to wear a special anti-ulcer kit from well-known manufacturers. ULCER X (Sigvaris, Switzerland) with a working pressure in the lower leg of about 34-46 mm Hg is ideal;
3. Normalizing body weight is a fundamental task that we usually immediately set for a patient with venous TU. It is known that with excess weight there is an increase in the likelihood that a trophic ulcer will appear, and the prognosis for its treatment worsens. With normal weight, there is no overload of the venous bed or disruption of the venous outflow of blood. When reaching optimal weight, a person must make every effort to maintain these indicators;
4. Completely give up bad habits that impair blood circulation. That is, do not smoke, do not drink alcohol, etc.;
5. Do not overcool your feet; buy soft, comfortable shoes. The ideal option is semi-sports shoes with laces (imitation of elastic compression) plus individual orthopedic insoles. It is preferable that it be made from natural materials. All this, in combination with compression hosiery, optimizes the work of the muscle pump of the lower leg and foot;
6. If the localization of the ulcerative defect is the sole of the foot or toes, the patient is recommended to use a special splint or specially selected relief shoes. Thanks to this, the risk of injury and anaerobic infection is reduced. While walking, a person uses a stick or crutches. This reduces the load on the affected area;
7. Carefully observe hygiene measures. A warm, hygienic shower is mandatory for patients with TU. Liquid neutral soap with an antibacterial component is recommended. It is mandatory to regularly clean the affected area and the ulcer itself using modern antiseptics (lavasept, octenisept, meramistin). Thus, wetting the feet is permitted. Otherwise, the likelihood of developing a dried purulent crust increases, which, in turn, is a springboard for pathogenic microorganisms. The product that the patient will use to treat the affected area should be prescribed exclusively by the treating specialist. You should purchase the treatment drug only at specialized pharmacies.
Duration of treatment for trophic ulcers and when to expect improvement
All stages of treatment are controlled by a doctor. Some procedures are carried out in a hospital or surgical office; the patient performs certain manipulations daily at home. The duration of therapy depends on how the defect heals, on the stage of the disease, the type of drugs used, and the severity of the general condition.
Antibiotics can be prescribed for a period of 2 weeks to 2 months, venotonic drugs are used in courses from 2 to 6 months, antiplatelet agents, for example, Aspirin Cardio, can be recommended for continuous use.
The first signs of improvement and regeneration processes begin 2-3 weeks from the start of treatment. Complete healing of the ulcer requires up to 3-6 months or more.
Treatment of trophic ulcers: “before” and “after” photos
Why surgery is needed
In complex therapy, conservative and surgical techniques are used. Conservatively, with the help of medications and dressings, small ulcerations (2–3 cm in diameter) are quite successfully treated. However, even if they heal, there is a high probability of relapse, because the cause of the disease is a violation of venous or lymphatic outflow, but it has not been eliminated. The use of microsurgical technologies allows you to quickly change the course of treatment for the better - to normalize venous outflow, restore microcirculation, and accelerate the healing of the defect.
Possible consequences and complications of trophic ulcers
Due to various reasons for the formation of trophic ulcers, the severity and depth of defects, the addition of a microbial infection (less often fungal), the range of complications is extensive.
The most common severe complication is purulent inflammation with melting of surrounding tissues and an increase in the size of the ulcer. It is typically characterized by the appearance of purulent discharge, an unpleasant odor, increased inflammation around the edges of the wound, and the appearance of constant or throbbing pain. If adequate treatment is not carried out, cellulitis or sepsis is possible.
Gangrene may occur in diabetes mellitus. More often it is a dry form, with tissue atrophy and blackening of the limb. The formation of wet gangrene is also possible, rapidly spreading upward, with severe intoxication and a real threat to life.
With varicose veins, thrombophlebitis often occurs - thrombosis of the affected veins and an inflammatory process in their walls.
Rare complications of trophic ulcers:
- skin eczema;
- erysipelas;
- cellulite (damage to subcutaneous fat);
- osteomyelitis (inflammation of the periosteum);
- arthrosis of the ankle joint.
Prevention of trophic ulcers
To prevent trophic ulcers, timely treatment of diseases that provoke circulatory disorders in the extremities is necessary.
A healthy lifestyle is important, weight control through a rational diet with the consumption of sufficient fiber, fresh vegetables and fruits.
With the initial manifestations of venous or arterial insufficiency, a rational regime of work and rest, selection of comfortable shoes so that they do not rub the feet or squeeze the toes, and protective clothing to prevent minor injuries are necessary.
For people who spend a long time on their feet and have a hereditary predisposition to varicose veins, special compression hosiery with an individually selected pressure level is recommended.
Statistics
Let's talk about venous tumors of venous etiology, which are the most common in the practice of a vascular surgeon. Let us immediately note that TU is not a diagnosis or an independent disease! This is a complication of the underlying vascular disease (most often, varicose veins), developing in the absence of adequate treatment. The difference between these particular ulcers is the minimal tendency to heal on their own. In most clinical observations, in the absence of radical correction of impaired blood flow, venous ulcers recur. In addition to physical suffering and a sharp decrease in quality of life, long-term non-healing venous leg ulcers also cause enormous financial damage. This is a colossal item of domestic healthcare expenditure. According to a number of researchers (S.N. Yakushkin, 2019), the costs of the vast majority of such patients for the purchase of medications (phlebotonics) and expensive dressings in Moscow exceed 50,000 rubles per year.
Reviews from patients of our clinic
Baraboshkin N.D.
Thanks to the entire team of the Gruzdev clinic and especially to A.A. Suleymanov. for your sensitive attention and professionalism. Thanks to Aziz Alisherovich, it was possible to cure a severe case of a trophic ulcer on the leg.
Belogrudova E.I.
I was admitted to the phlebology department of the Gruzdev clinic with a diagnosis of a trophic ulcer. The ulcer was healed. In this regard, special thanks to this young and wonderful doctor and wishes for success in his grateful work. At the same time, I want to thank the nurses for their humane work.
I would like to note the positive direction in the Clinic’s activities:
- use of modern medical technology;
- providing periodic discounts on honey. services;
- Providing Clinic transport to transport patients from home and back after treatment.
I wish the Gruzdev Clinic success in their grateful work.
Elena
My grandmother had a trophic ulcer on her right leg that did not heal for several years. My leg hurt a lot and I had to bandage it every day. We went to the clinic, to different clinics, but the ulcer did not heal, but only grew larger. I heard about your clinic on the radio and decided to contact them, although they didn’t believe in much. The grandmother was recommended to undergo a course of treatment. We started going to the clinic every other day for IVs, ozone therapy, and intravenous laser blood irradiation. In 20 days, surprisingly, the ulcer cleared up, the pain went away, the unpleasant smell went away, but healing was still far away and we were recommended to perform plastic surgery on the ulcer and we agreed. As a result, the ulcer healed and the grandmother was very happy. I was pleasantly surprised by the attitude of the staff! Attentive doctors, responsive nurses. Thank you all very much from me and from grandma!
Read all reviews about the clinic
View all patents
Venous ulcers | Ulcers in atherosclerosis | Diabetic trophic ulcers | Ulcers due to obliterating endarteritis | Ulcers in hypertension | Ulcers due to congenital vascular malformations | Ulcers due to lymphedema | Pyoderma gangrenosum | Hydrostatic ulcers | Ulcers due to malignant skin tumors
There are different definitions of the concept of “trophic ulcer,” but its main criteria are, firstly, damage to the skin over the entire thickness, that is, the absence of sources for epithelization at the bottom of the ulcer and, secondly, the low healing rate. Trophic ulcers of the lower extremities are a common pathology. They affect about 1% of the total adult population, and among elderly people (over 65 years old) this figure increases to 5%. Currently, in developed countries, the incidence of ulcers is increasing, which is associated with the aging of the population and the spread of risk factors for atherosclerosis obliterans, such as smoking, diabetes and obesity. Few people know that the diagnosis “Trophic ulcer” does not exist. A trophic ulcer is not a diagnosis, but a CONSEQUENCE of advanced diseases, of which there are more than a hundred. And they are treated differently. Trophic leg ulcers account for 3 pathologies in 95% of cases:
1. Venous insufficiency of the lower extremities due to varicose and post-thrombotic diseases: approximately 55% of all ulcers; 2. Obliterating atherosclerosis of the arteries of the lower extremities: approximately 15% of all ulcers; 3. Diabetes mellitus: approximately 20% of all ulcers; Combinations of the above reasons: approximately 10% of all ulcers.
The remaining diseases, of which there are more than a hundred, lead to ulcers, which occur in approximately 5% of cases. But it is precisely these 5% of cases that cause the greatest difficulties in diagnosis and treatment.
FAQ
Which doctor treats trophic ulcers? Who should I contact?
Uncomplicated cases of trophic ulcers are treated by a phlebologist. If serious complications, suppuration, or the size of the defect occur, surgeons are involved in treatment.
Is a trophic ulcer contagious?
No. Trophic ulcers are caused by prolonged disruption of blood flow in the affected area, deficiency of oxygen and nutrition in the skin and underlying tissues.
Is it possible to smear trophic ulcers with brilliant green?
Brilliant green solution is a local antiseptic. It is used to treat the skin around the wound to prevent infection. It is permissible to use it only on the skin around the wound, but in no case in the area of affected tissue. For trophic ulcers, the use of brilliant green is ineffective.
Can trophic ulcers be treated with hydrogen peroxide?
A solution of hydrogen peroxide is used for local treatment of the wound, cleansing it of dead cells and pathogenic microbes. This manipulation is carried out twice a day before applying a bandage. You can replace hydrogen peroxide with a 0.05% chlorhexidine solution.
Is it possible to treat trophic ulcers with streptocide?
Although there are many recipes on the Internet for treating trophic ulcers using streptocide powder, doctors do not consider this treatment method effective. Moreover, due to foreign particles entering the wound, additional irritation and increased inflammation are possible.
Is it possible to wash trophic ulcers with chlorhexidine?
A solution of chlorhexidine 0.05% is used for local treatment of the wound, cleansing it of dead cells and pathogenic microbes. This manipulation is carried out twice a day before applying a bandage. Can be replaced with hydrogen peroxide.
Is it possible to smear trophic ulcers with insulin?
There is no evidence in the scientific literature that this treatment method is effective. Moreover, the use of any substance in the area of an open wound without the advice of a doctor can lead to worsening, increased inflammation and suppuration.
Is it possible to wet trophic ulcers with water?
There is a myth that you cannot wet a trophic ulcer until it has completely healed. However, proper body hygiene is extremely important for a speedy recovery. It is important to avoid swimming in natural bodies of water, where the water may be dirty and contain a high number of pathogenic bacteria. Regular tap water is not dangerous. When taking a shower, you should wash the skin around the wound with soap, being careful not to get it on the area of the ulcer itself. After bathing, you need to treat the area of the ulcer with antiseptics and apply a bandage, or follow the recommendations given by the doctor.
Can trophic ulcers be washed with laundry soap?
Some recommendations for the management of patients with trophic ulcers describe the method of washing wounds with laundry soap. But not all patients tolerate such manipulation well. Therefore, rinsing can be done with plain water, and then treating the wound with hydrogen peroxide or chlorhexidine solution.
Can trophic ulcers be treated with potassium permanganate?
A solution of potassium permanganate has a disinfecting, drying or cauterizing effect depending on the concentration. At home, it is difficult to prepare the required concentration of the solution, and treatment with a more concentrated composition can lead to a feeling of dryness, tightness, and burning. And if not all crystals dissolve, you can get a tissue burn. Therefore, it is better to discuss this method of wound treatment with a doctor or use safer antiseptic compounds.
Can trophic ulcers be treated with fucorcin?
Fucorcin solution, or Castellani paint, is an antiseptic drug that is effective in many inflammatory skin processes. Its use for trophic ulcers is acceptable, but it has a significant disadvantage - it has a bright pink color and stains the skin, and can stain clothes.
Popular questions from clinic patients
Which doctor treats trophic ulcers?
A phlebologist treats uncomplicated ulcerations that appear due to problems with the veins. If they are complicated, large, accompanied by necrotic and purulent inflammatory processes, surgeons are involved.
Where are trophic ulcers treated in Moscow?
Lesions of the skin and soft tissues, as well as the cause of their appearance, can be treated in any center where there is a phlebologist, endocrinologist and other specialists in the underlying disease. But a multidisciplinary team can offer a full range of diagnostics, effective therapy and prevention. Competent treatment of trophic ulcers, the prices of which depend on the complexity of their course and the nature of the methods used, is guaranteed in this medical center.
Trophic ulcers hurt – what to do?
This is an open wound that definitely causes discomfort and pain. Therefore, during therapy, general and local painkillers are used.
Is it possible to get it wet?
It is possible to wet a trophic ulcer as part of daily hygiene procedures. You just can’t swim in natural bodies of water, where there is a high risk of dangerous infection. When washing in the shower, you need to thoroughly clean the areas around the ulceration, but try not to let the soap get into the wound. After water procedures, it is necessary to treat the tumor with antiseptics and cover it with a bandage, following all the recommendations of the chosen doctor.
Is it possible to wash affected areas with soap?
It's possible, but not necessary. Contact of an open area with laundry soap is painful, so for disinfection it is enough to treat with peroxide or chlorhexidine.
List of sources
- Babadzhanov B.R. Complex therapy of long-term non-healing trophic ulcers / B.R. Babajanov, I.Yu. Sultanov // Angiology and vascular surgery. - 2002. - No. 3.
- Bogachev V.Yu. Local treatment of venous trophic ulcers / V.Yu. Bogachev [and others] // Consilium medicum. – 2001. – No. 2. – P. 45–50.
- Bogdanets L.I. Local treatment of venous trophic ulcers / L.I. Bogdanets [and others] // Gideon Richter. – 2000. – No. 2. – P. 58-60.
- Dubrovshchik O.I. Trophic ulcers of venous origin: modern treatment options / O.I. Dubrovshchik [and others] // Journal of the Grodno State Medical University. - 2021. - No. 2. - P. 107-111.
- Kirienko A.I. Treatment of trophic ulcers of venous etiology / A.I. Kiriyenko // Consilium medicum. – 2000. – T.2. – No. 4.
- Komarova L.N. Results of treatment of patients with varicose veins of the lower extremities over 10 years / L.N. Komarova [and others] // Archives of Internal Medicine. - 2021. - No. 3. - P. 215-218.
- Kruglova L.S. Trophic ulcers of venous origin / L.S. Kruglova [and others] // Russian Journal of Skin and Venereal Diseases. - 2014. - No. 1. - P. 21-25.
- Obolensky V.N. Trophic ulcers of the lower extremities - review of the problem / V.N. Obolensky [and others] // Russian Medical Journal. - 2009. - No. 25. - P. 1647-1663.
- Turkin P.Yu. Venous trophic ulcers: current state of the issue / P.Yu. Turkin [etc.] // Medicine. - 2021. - No. 1. - P. 41-45.