What is a boil?
A boil develops when a hair follicle becomes inflamed.
Photo: Mahdouch at French Wikipedia (Creative Commons Attribution 1.0 Generic license) Research shows that skin diseases are one of the leading reasons for visits to primary health care. A striking example of a disease in this group is the occurrence of boils, which are purulent-necrotic inflammations of hair follicles and adjacent tissues, including the sebaceous glands. They most often occur in adolescence and early adulthood1.
Localization of boils
In most cases, boils occur in areas exposed to pollution and/or mechanical stress - on the hands, forearms, back of the neck, buttocks, lower back, thighs. In rare cases, ulcers appear in unexpected places - in the ear canal, on the outer and inner surfaces of the nose, labia, etc. However, boils never form on areas of the skin that are devoid of hair - the palms and palmar surfaces of the fingers, soles.
What is the difference between a boil and a carbuncle?
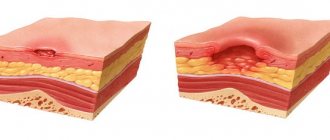
A carbuncle is a purulent-necrotic inflammation of several hair follicles at once, merging into one purulent focus (Fig. 1). Often it is a complication of a boil. Carbuncle occurs much less frequently than furuncle, and the main group of patients consists of middle-aged and elderly people.
Figure 1. How a boil differs from a carbuncle. Source: IQWiG/NCBI
Carbuncle
Carbuncle is an acute purulent-necrotic inflammation of a group of hair follicles united by a common infiltrate. Of all staphyloderma, it is the most severe inflammation. The disease is registered mainly in adults.
The name carbuncle comes from the Latin carbo - coal. In Rus', the disease was called ognevik or uglevik.
Golden and white staphylococci are the main culprits of the disease. The development of carbuncles is facilitated by malfunctions of the immune system, which occurs in patients with severe somatic pathology, diabetes mellitus, obesity and hypovitaminosis, as well as hypothermia, massive skin contamination and non-compliance with the hygienic regime.
The localization and stages of development of the carbuncle are similar to those of a boil.
The areas of the body most susceptible to contamination are most often affected - the back of the neck, back and lumbar region. Carbuncles are most often single.
The carbuncle is a purple or dark red nodule up to 5–10 cm in diameter, not clearly demarcated from the surrounding tissues, with several pustules on the surface. Opening the focus of suppuration is accompanied by the release of a purulent-bloody mass and rejection of necrotic rods. After opening the carbuncle, an extensive ulcer with undermined edges forms on the skin. Its bottom is covered with a coating of mucopurulent consistency and bleeds easily. Gradually, the ulcerative defect is cleared of plaque and filled with granulations. Healing occurs within 2–4 weeks with the formation of a deeply retracted scar.
The disease occurs with severe symptoms of intoxication: chills, elevated body temperature, weakness, loss of appetite and headaches; vomiting and loss of consciousness are less common.
Of the complications, the most dangerous are phlebitis, thrombosis of the cerebral sinuses and sepsis.
At the beginning of the disease, the picture of the carbuncle is similar to that of phlegmon. Sometimes the necrotic crust of the carbuncle makes it look like an anthrax carbuncle.
Rice. 35 and 36. With a boil (photo on the left), one pustule forms on the surface of the infiltrate, with a carbuncle - several (photo on the right).
Rice. 37 and 38. The photo shows large carbuncles on the back.
Rice. 39 and 40. In the photo, the carbuncles are gigantic. Superficial pustules and multi-chamber abscesses are visible, on the surface of which there are numerous holes resembling a “sieve” through which pus is released. The disease is often recorded in patients with diabetes.
Rice. 41 and 42. In the photo there are carbuncles on the neck: giant (left) and multiple (right).
Fig. 43 and 44. The photo shows carbuncles on the face.
Rice. 45 and 46. The photo shows carbuncles on the back.
Rice. 47. The photo shows a carbuncle on a finger.
Rice. 48. The photo shows a huge carbuncle on the buttock.
Rice. 49 and 50. The photo shows carbuncles on the limbs: leg (left) and arm (right).
Fig. 51 and 52. In the photo, phlegmon is a formidable complication of a carbuncle.
Fig. 53 and 54. In the photo on the left is a large carbuncle of the back, on the right - with anthrax.
Causes
A boil develops as a result of infection of the hair follicle by pathogenic bacteria, often in combination with a decrease in local and systemic immunity. In the vast majority of cases, the cause of inflammation is Staphylococcus aureus, less often Staphylococcus pyogenes albus.
One of the important triggering factors in this case is the disruption of the normal composition of the skin microflora, due to which pathogenic staphylococci are able to remain on its surface for a long time. This is primarily due to non-compliance with personal hygiene rules.
Background for the development of the disease
IT IS IMPORTANT TO KNOW!
Staphylococcal infections do not develop out of the blue. Thus, photos with signs of the development of the initial stage of a boil are expected against the background of skin contamination, excessive sweating, contact with aggressive chemicals, as well as with reduced immunity, skin injuries, and hormonal dysfunctions.
Risk factors
Violation of the composition of the skin microflora contributes to the deterioration of the immune system, which can be caused by the following pathologies and factors:
- Infectious diseases: AIDS, chronic tuberculosis.
- Chronic somatic pathologies: hepatitis, bronchitis, pyelonephritis.
- Endocrine diseases: diabetes mellitus, endocrine obesity.
- The presence of malignant tumors in the body and their treatment: radiation or chemotherapy.
- Long-term use of glucocorticosteroids.
- Improper, unbalanced nutrition, leading to hypo- and vitamin deficiency.
Local changes in the skin that contribute to the appearance of boils include:
- Hyperhidrosis – increased sweating.
- Frequent skin trauma, scratches and cuts.
- Dermatological pathologies: eczema, acne, psoriasis.
Stages of boil development
When a hair follicle becomes infected, a pustule is first formed containing neutrophils (white blood cells responsible for the immune response), pathogenic staphylococci and fibrin. Next, the bacteria descend down the follicle, provoking inflammation, which leads to the formation of an infiltrate followed by necrosis (death) of the surrounding tissues. At the same time, tissue melts around the affected area, due to which pus is formed and the boil matures. Purulent exudate accumulates under the epidermis, around the mouth of the follicle. Further, together with the necrotic rod and dead hair, it breaks through and comes out. Over time, a scar forms at the site of the ruptured boil.
Based on pathogenesis and clinical features, it is customary to distinguish 3 successive stages of boil development, which take about 7-10 days. These include:
- Infiltration stage. Accompanied by infiltration (leakage of blood elements and products of the inflammatory process) of the tissues around the hair follicle. Takes 3-4 days.
- Stage of suppuration and necrosis. It begins with the formation of a characteristic purulent-necrotic core. Intoxication syndrome also occurs. At the peak of clinical manifestations, the covering of the purulent core is opened, and purulent masses are released from the resulting hole. After this, the symptoms subside.
- Recovery stage. It begins with the formation of granulation tissue in the form of a crust at the site of opening. 3-4 days after this, a connective tissue scar appears, initially having a red-blue color, but gradually turning pale and acquiring a flesh color. The entire stage takes up to 10 days.
Is a boil dangerous? Possible complications
In most cases, with timely treatment, boils do not pose a serious danger. But when trying to independently squeeze out a purulent-necrotic rod, inadequate local therapy, or the addition of a secondary infection, dangerous complications can develop.
Local complications include purulent lesions of the skin and subcutaneous tissue: furunculosis, carbuncles, abscesses and phlegmon. Damage to adjacent blood vessels and lymph nodes in the form of phlebitis, thrombophlebitis, and lymphadenitis is also possible.
The greatest danger is represented by boils located in the area of the nasolabial triangle and higher on the face and ear canal, since there is a high risk of spread of purulent masses and pathogenic bacteria into the cranial cavity through blood vessels. This can lead to damage to the meninges (meningitis, arachnoiditis) and directly to the brain tissue (encephalitis, brain abscesses). In rare cases, a boil can cause purulent masses and bacteria to enter the systemic circulation with the development of sepsis.
Important! A burst boil that is not treated properly poses a particular danger to the patient and others. An ruptured boil can cause infection of other follicles with the formation of furunculosis, as well as an entry point for secondary infections. In addition, the released purulent masses can become a source of infection for other people who come into contact with it directly or indirectly (through household items).
Furunculosis
Furunculosis is an infectious disease characterized by the appearance of several boils at the same time (acute furunculosis) or the appearance of one boil after another (chronic furunculosis). With chronic furunculosis, the presence of boils at different stages of development is noted. Furunculosis can be limited or widespread. The disease lasts a long time - months and even years. Furunculosis often affects people with reduced immunity and those suffering from diabetes. During treatment, tolerance to the therapy with antibacterial drugs is noted.
Furunculosis complicates the course of many skin diseases.
Causes of furunculosis
The main cause of furunculosis is Staphylococcus aureus. It causes disease in 60 - 97% of patients. In other cases, the cause of the disease is epidermal staphylococci, group A and B streptococci and other types of bacteria.
Recently, more and more staphylococci resistant to a number of antibiotics have been sown from lesions, about 90% of which are staphylococci resistant to penicillin and ampicillin, about 19% to erythromycin.
Risk factors for the development of furunculosis:
- The presence of foci of chronic infection in patients with furunculosis is recorded in 75 - 90% of cases. The most common pathologies are the ENT organs (tonsillitis, sinusitis and pharyngitis) and the gastrointestinal tract (chronic gastroduodenitis and cholecystitis). Dysbacteriosis contributes to the development of furunculosis.
- In 40% of cases, diseases of the thyroid gland, gonads and diabetes mellitus are registered in patients with furunculosis.
- Consumption of large amounts of carbohydrates and diabetes mellitus contribute to the development of furunculosis. An increased amount of sugar in the blood is a good breeding ground for staphylococci.
- In 39% of cases, the patient’s body is sensitized to different types of allergens.
- The development of furunculosis is caused by disturbances in carbohydrate, fat and protein metabolism, as well as by hypo- and avitaminosis. Furunculosis often occurs in weakened, exhausted patients suffering from severe somatic pathology. Anemia, chronic diseases of the gastrointestinal tract, immunodeficiency conditions (HIV infection and oncology) are the main ones.
- Constant physical activity and mental stress contribute to the development of furunculosis.
The presence of Staphylococcus aureus on the skin and weakened immunity are the main factors in the development of furunculosis.
Immune status disorders in furunculosis
The human immune system is designed to protect the body when in contact with infectious agents. The causative agents of furunculosis cause a whole “cascade” of protective reactions, most of which are disrupted during the disease.
- Up to 70% of patients with chronic furunculosis have impaired phagocytosis (capture, absorption and destruction of pathogenic microorganisms).
- A low level of iron in the blood serum causes a decrease in the processes of killing (destruction) of pathogenic microorganisms.
- In the blood of 43% of patients with chronic furunculosis, a decrease in the level of T and B lymphocytes is recorded.
- In the blood of 60% of patients with chronic furunculosis, there is a decrease in the level of immunoglobulins (IgG and IgM).
Severity of furunculosis
Mild severity of furunculosis is characterized by the presence of single boils. The inflammatory reaction is moderate. Relapses occur 1-2 times a year. There are no signs of intoxication. Peripheral lymph nodes enlarge during exacerbations. Indicators of immune status in this category of patients in 70% of cases remain within normal limits.
The average severity of furunculosis is characterized by the presence of single large boils or multiple boils. The inflammatory reaction proceeds rapidly. Relapses occur up to 3 times a year. During exacerbations, inflammation of the lymphatic vessels and lymph nodes is noted. Often the disease occurs with symptoms of intoxication. Violations of the cellular and humoral immunity are noted.
Severe severity of the disease is characterized by the presence of multiple boils with a continuously relapsing course. Furunculosis is accompanied by severe intoxication. Patients experience weakness, malaise, headache, elevated body temperature and sweating. Violations of the cellular and humoral immunity are significant.
Rice. 32 and 32.1. The photo shows furunculosis.
Complications of furunculosis
The penetration of bacteria into the blood causes bacteremia, which is a serious complication of furunculosis. Bacteria settle in the internal organs, causing endocarditis, osteomyelitis, pneumonia, meningitis, kidney inflammation, etc. Septic shock often ends in the death of the patient.
Differential diagnosis of furunculosis
To prescribe adequate treatment for furunculosis, the method of differential diagnosis should be used with diseases such as pseudofurunculosis, hidradenitis, anthrax and carbuncle.
Rice. 33 and 34. The photo shows furunculosis. On the skin of the abdomen and buttocks there are boils at different stages of development.
Symptoms of a boil
In most cases, boils occur with fairly characteristic symptoms, which vary depending on the stage of development. In general, patients may have the following complaints:
- General weakness, increased body temperature up to 38°C, headache.
- Tingling, itching in the area where the boil forms, which after a few days is replaced by sharp pain.
- Redness and thickening of the skin in the area of inflammation, which protrudes cone-shaped above the skin.
- The formation of a small whitish purulent head in the center of the compaction, which opens after a few days.
- Discharge of yellowish purulent contents from the hole formed after opening the pustule. At the same time, pain is significantly relieved and the general condition of a person improves.
- Manifestations of furunculosis can vary depending on the location and are accompanied by uncharacteristic features. For example, when a purulent focus forms in the area of the upper lip or eyelids, pronounced swelling is observed, and when a boil occurs in the area of the auditory canal, a severe headache spreading to the lower jaw, as well as hearing impairment, come to the fore.
How to treat boils -
It is possible to cure boils at home, but only in the cases listed below. In most cases, you should immediately consult a doctor (surgeon), especially if you have concomitant chronic diseases from the list below.
- You can treat it at home - if the size of the boil is no more than 5 mm and you do not have symptoms of intoxication or fever. You must also not have any of the diseases listed below. → if you have diseases: diabetes, oncology, reduced immunity, endocarditis or rheumatoid arthritis, obesity, taking prednisolone (in all these cases you need not only to be treated by a doctor, but also to use antibiotic therapy).
- You definitely need to see a doctor – → if the boil occurs in an infant, young child, → there are symptoms of intoxication, fever, → if a boil occurs on the upper lip, nose, nasolabial folds,
→ if there are symptoms of inflammation spreading: for example, the area of skin redness has increased or red stripes have appeared next to the boil, or another boil is forming nearby.→ if you have diseases from the list above.
When to see a doctor?
In most cases, a person can independently cope with one, uncomplicated boil. However, it is recommended to seek medical help if there is a significant disturbance in the general condition or the first signs of complications.
Alarming symptoms and changes that indicate the need to contact specialists are:
- Simultaneous appearance of more than 1 boil.
- The appearance of a boil on the face.
- Rapid deterioration in health.
- Severe pain in the area of the boil, increased body temperature to 39°C or more.
- Lack of positive dynamics, despite the treatment.
- Persistence of the inflammatory process for more than 2 weeks.
- Constant recurrence of boils.
Diagnostics
The diagnosis of “boil” is usually established on the basis of characteristic clinical changes. However, in order to monitor the patient’s general condition, early detection and prevention of complications, the following laboratory and instrumental diagnostic methods can be used:
- General blood and urine tests (CBC, UAM).
- Biochemical blood test with determination of glucose levels.
- Blood test for HIV using enzyme-linked immunosorbent assay (ELISA).
- Determination of hepatitis B and C virus markers by ELISA.
- Bacterial culture of a sample of purulent masses to identify the pathogen and its sensitivity to main antibiotics.
For recurrent and multiple boils, fluorography or radiography of the chest organs, ultrasound examination of the abdominal organs and kidneys, etc. can be additionally performed.
Differential diagnosis of a boil is carried out with other dermatological and infectious diseases, which may be accompanied by similar symptoms, including:
- Hidradenitis suppurativa,
- Erythema nodosum,
- Anthrax,
- Lupus,
- Actinomycosis.
Disease detection
Diagnosis of the disease consists of conducting the following medical studies:
- Medical examination.
- Dermatoscopy.
- Examination of the boil contents for the presence of microorganisms.
Additional research methods include clinical tests of urine and blood, ultrasound, computed tomography, x-ray of the sinuses, and rhinoscopy.
Treatment of a boil
The boil, in the vast majority of cases, is subject to local treatment, which depends on the stage of its development. The purpose of the therapy is to prevent complications, cleanse the purulent focus and prevent the formation of rough scars.
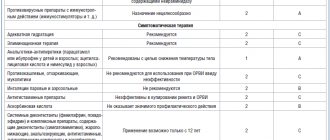
Drug treatment
At the infiltration stage, ichthyol dressings, warming with dry heat and UHF therapy can be used. After opening, bandages with hypertonic sodium chloride solution, turunda with chloramphenicol and methyluracil are indicated.
To reduce body temperature and suppress pain, non-steroidal anti-inflammatory drugs (NSAIDs) can be used: ibuprofen, paracetamol. Depending on the accompanying changes, vitamin complexes, antihistamines, immunomodulators, etc. are used. If complications are suspected, antibacterial drugs can also be prescribed.
Local treatment with ointments
Local remedies are often used to combat boils.
Photo: Genrix20061.mail.ru / Depositphotos Local therapy using various ointments plays an important role in treatment. Considering the large number of topical medications on the market and the stage of the disease, it is better to consult a doctor before choosing a drug, especially if a boil has developed in a child.
At the infiltration stage, it is recommended to use antiseptic ointments with a so-called pulling effect: ichthyol, heparin, synthomycin.
When opening a boil on your own, treatment of the resulting skin defect with antibacterial soap is indicated, after which it is necessary to apply an antiseptic. In order to prevent local purulent complications, bandages with agents that have a local antibacterial effect (levomekol or tetracycline ointment) are used. It is recommended to change the dressing 2-3 times a day until healing, washing the wound with warm water and soap.
Surgery
In some cases, with severe pain or the risk of complications, a decision is made to open the boil. To do this, a small incision is made above the pustule, through which purulent-necrotic masses are removed. After surgery, the affected area is treated with antiseptic solutions, and less commonly, systemic antibiotics are prescribed.
Tips for treatment at home
Small, single boils can be treated at home. To speed up the recovery process and prevent the spread of infection into adjacent tissues and blood vessels, the following recommendations should be followed:
- Use warm compresses. Resorting to warm compresses several times a day for about 10 minutes will help the boil open and quickly release purulent-necrotic masses.
- Minimize mechanical impact on the boil. You should not try to squeeze out or puncture the boil yourself. This can lead to a breakthrough of the purulent-necrotic core into deeper tissues.
- Observe hygiene rules. After handling an opened boil and coming into contact with its discharge, you must wash your hands thoroughly. It is also important to use disposable materials for compresses and bandages and to wash clothing and fabrics that have come into contact with the contents of the boil.
Traditional treatment
Various folk recipes can be used as auxiliary therapy. However, it is important to note that in the absence of positive dynamics and the first signs of worsening local changes or general condition, you must immediately seek qualified medical help.
Some of the most popular folk recipes are:
- Honey cake. To prepare, mix one tablespoon of honey and the same amount of wheat flour. Next, it is applied to the boil until the pustule is opened. It is believed that it helps the purulent focus to clear faster and better.
- Aloe or Kalanchoe. A freshly cut aloe or Kalanchoe leaf is applied with the cut to the skin for several hours to the area of infiltration. This method is suitable for the initial stages of disease development.
- Potato. Peeled, washed potatoes are cut into slices and applied to the boil. This bandage should be changed 3-4 times a day.
To make the boil go away faster, you can use aloe juice. Photo: piyaphunjun.gmail.com / Depositphotos
Treatment of furunculosis at JSC "Medicine" (clinic of academician Roitberg)
Qualified therapists and dermatologists of JSC "Medicine" (clinic of academician Roitberg) in the Central Administrative District of Moscow are ready to receive and examine patients with suspected furunculosis. To confirm the diagnosis, it is recommended to undergo a comprehensive examination in your own laboratory center. Treatment is prescribed on an individual basis, and its progress and results are strictly monitored by specialists. Each client is guaranteed tactful and attentive treatment, confidentiality of personal information, as well as comfort and safety during diagnostic and treatment procedures.
How to open a boil yourself?
Dermatologists categorically do not recommend trying to cope with inflammation on your own, wanting to squeeze out the purulent contents and the core of the boil at home. This is dangerous due to secondary infection, the spread of the inflammatory process to healthy tissue, the formation of new areas of inflammation and blood poisoning. The decision to open a boil is made only by a surgeon at a specialized medical institution, and only he has the right to carry out such manipulations.
What does a boil look like?
A boil is a visible lump or red bump with a purulent head on the surface of the skin. When you touch its surface, you feel relatively severe pain, the skin around it is noticeably inflamed, and its temperature is increased. The most common places of development are the back of the head, the back of the hands, the lower back, and the face. The rash can be single or massive; its symptoms do not depend on the number of points of inflammation.
Why do boils appear?
This question can be answered accurately only after a thorough diagnosis of the boil. Among the most likely causes are infection of the hair follicle of the skin with staphylococcus bacteria against the background of vitamin deficiency, violation of personal hygiene rules, wearing too tight clothes, poor-quality antiseptic treatment of abrasions and skin injuries. The disease can also be caused by intense work of the sebaceous and sweat glands, the secretion of which is a favorable environment for bacteria.
Prognosis and prevention
As a rule, recovery occurs 1-2 weeks after the first symptoms appear. Sometimes a small connective tissue scar appears as a residual phenomenon, which gradually acquires a flesh color and becomes hardly noticeable.
It is not always possible to prevent the development of boils, especially when the immune system is weakened. However, the following recommendations can help avoid the development of the disease:
- Maintain good personal hygiene, including regular hand washing with soap and water or using alcohol-based hand rubs. This will reduce the likelihood of disruption of the normal microflora of the skin and infection by pathogenic bacteria.
- Proper treatment of skin damage. The skin around cuts and abrasions should be treated with antiseptics, and the injuries themselves should be bandaged with clean, sterile, dry bandages until they heal.
- Individual use of personal hygiene products. No sharing of towels, sheets, razors, clothing, sports equipment or other personal items is permitted. Due to these items, pathogenic staphylococci are able to be transmitted from person to person.
- Proper, balanced nutrition.
- Complete treatment of concomitant diseases and conditions that can reduce the body's defenses.
Sources
- Shallcross, Laura J et al. “Incidence and recurrence of boils and abscesses within the first year: a cohort study in UK primary care.” The British journal of general practice: the journal of the Royal College of General Practitioners vol. 65.639 (2015).
- Clinical protocol for diagnosis and treatment of “skin abscess, boil and carbuncle of other localizations” Expert Council of the Republican State Enterprise at the Republican Center for Healthcare Development of the Ministry of Health and Social Development of the Republic of Kazakhstan dated December 12, 2014 protocol No. 9.
- Boils and carbuncles. Mayo Clinic.
- Federal clinical guidelines for the management of patients with pyoderma. Russian Society of Dermatovenereologists and Cosmetologists, 2015.