Symptoms of seizures in the corners of the mouth
Clinical manifestations and symptoms of the lesion depend on many factors and stages. It usually begins with redness of the skin in the corners of the mouth, peeling, and the appearance of bursting blisters. Areas of erosion appear on the mucous membrane and skin of the corner, which become covered with a crust, when ruptured, cracks of varying depths can form.
In areas of inflammation, constant itching is felt, pain appears when opening the mouth, pain when eating spicy food. It is especially typical that a sharp pain appears in the morning, after sleep, when you first open your mouth.
But in some rare cases, obvious pain symptoms are mild, especially in elderly people, or in people suffering from diabetes mellitus (when seizures appear as a consequence of candidal stomatitis).
Features of therapy and prevention
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Therapy is based on eliminating the root cause of the seizure, but there are also general recommendations for caring for the affected skin. If the cracks are streptococcal in nature, ointments with antibiotics are additionally administered, and if they are fungal, ointments with an antifungal effect are administered. The skin around the crack must be regularly treated with disinfectant solutions to avoid re-development of the source of infection. After eliminating the root cause, therapy continues for another 7-10 days until the skin is completely restored.
Depending on the root cause of angulitis, the course of treatment may include the use of antibiotics, B vitamins or paraffin-based ointments. In most cases, the prognosis is favorable. The main thing is not to self-medicate, consult a doctor in a timely manner and follow all necessary recommendations.
Causes of sticky spots in the corners of the mouth
for the appearance of seizures (more precisely, provoking factors) can be very diverse, although ultimately the cause is the action of microorganisms (i.e., infections) that cause limited inflammatory damage to areas of the skin and mucous membranes.
Bacterial infections. Mainly epidermal streptococci or staphylococci.
Fungal infections. Mainly by fungi of the genus Candida, sometimes against the background of candidal stomatitis.
Viral infections. Mainly by herpes simplex virus type 1, but more often against the background of herpetic stomatitis in the oral cavity. As a direct cause, they are less common.
The corners of the mouth are an almost ideal place for the accumulation and reproduction of microorganisms, which is facilitated by constant humidity, the presence of residual nutrients, and the relative enclosure of the space. But for the appearance of seizures in the corners of the mouth, provoking factors are necessary, which can be conditionally classified as external (for example, mechanical, local allergic, etc.) and internal (seizures as a manifestation of other diseases).
Dry mouth. Cracks in the corners of the mouth can be caused by excessive dryness of the oral mucosa (xerostomia).
Allergic reactions. For example, for cosmetics, for the components of ballpoint pens (if you have a habit of holding the tip in your mouth). But more often - on nickel-containing dentures.
Other external factors. As a rule, they contribute to bacterial infection in the corners of the mouth. Using dirty vegetables and fruits, regularly licking the corners of the mouth (which contributes to local stagnation of saliva), squeezing skin formations (such as pimples) on the lips, scratching this area, hypothermia of the entire facial area. External factors can also include long-term use of certain medications: antibiotics, hormone therapy drugs, as well as prolonged elevated body temperature.
General lesions of the oral mucosa. Inflammations of the oral mucosa of various types can lead to the appearance of jams in the corners of the mouth.
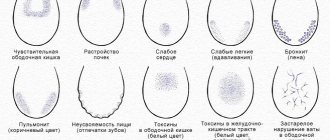
Common diseases as provoking factors. Among them: metabolic pathologies (for example, diabetes mellitus), Down syndrome (with an increased susceptibility to infections), Parkinson's disease (the corners of the mouth are constantly moist), various types of anemia (especially iron deficiency), immunodeficiency conditions, liver pathologies, hypovitaminosis ( deficiency of vitamin B2, B12, B6 or B3), lack of microelements in the body (zinc), pathologies of the gastrointestinal tract.
General characteristics of the condition
Painful cracks around the mouth are colloquially called jams. Zaeda is one of the forms of stomatitis (damage to the oral mucosa) caused by streptococci or yeast-like fungi of the genus Candida. In some cases, doctors diagnose mixed infection (angular stomatitis).
The following angulitis are distinguished: allergic (when using lipstick or other cosmetics), microbial (streptococcal, candidiasis, etc.) and post-traumatic (postoperative, post-manipulation, etc.). Microbial angulitis most often occurs in patients with diabetes mellitus (streptococcal) or in HIV-infected people (candidomycosis). Microbial angulitis in children can occur due to intestinal dysbiosis, vitamin deficiency, decreased immunity and other diseases. Post-traumatic (postoperative) angulitis is cracks in the skin and mucous membranes (linear tears in the skin or mucous membrane) in the area of the corner of the mouth, resulting from excessive (excessive) stretching after intraoral surgical dental operations (removal of dystopic or impacted wisdom teeth) or manipulations associated with treatment of wisdom teeth. Almost after every removal of an impacted or dystopic wisdom tooth, maxillary sinusotomy or other surgical interventions that require wide opening of the mouth, damage (by stretching) to the surface layers of the skin and mucous membrane in the area of the corner of the mouth occurs, i.e. post-traumatic (postoperative) angulitis.
Morphological features
Streptococcal angulitis most often develops in patients of the younger age category. First, a small bubble appears in the corners of the mouth, covered with a thin film. Later, erosion forms at the site of the bubble, covered with a crust of congealed blood and purulent masses. When the blister is opened, moist red skin with traces of minor bleeding is exposed. You can often find a crack in the center of the bubble. Approximately 1-2 hours after opening, the skin again becomes covered with a dense crust.
Content:
- General characteristics of the condition
- Possible reasons for development
- Features of therapy and prevention
Streptococcal infection of the mucous membrane is accompanied by discomfort and pain when opening the mouth.
Seizures of fungal origin are slightly different from streptococcal ones. Initially, a varnish-red erosion forms on the mucosa, surrounded by an additional layer of epithelium. Sometimes erosion is covered with a grayish coating. A specific crust does not form in case of candidiasis angulitis. Most often, the crack is masked by an overhanging skin fold and has a chronic, relapsing course.
Complications of lip jams
At the first, initial stage, the superficial layers of the mucous skin are affected and timely treatment of the jam leads to a quick recovery. But if left untreated, the lesion spreads to the deeper layers of the skin with the formation of a deep crack in the corners of the lips and the participation of lymphatic capillaries. The lesion can spread to neighboring areas of the skin, new cracks form, they combine into a large wound, which requires separate and special treatment.
Treatment
The method of treating angulitis depends on the reasons that provoked its appearance. What to do in the event of the development of a serious pathology - to treat yourself or go to a doctor - is decided by the person himself. In the absence of proper treatment, cheilitis can turn into purulent abscesses.
- Trauma, bad habits. Correct the prosthesis, temporarily avoid going to the dentist, do not perform active actions with the throat and lips, take proper care of the oral cavity, and brush your teeth thoroughly. It is recommended to numb the surface with lidocaine-based solutions. Treat with antiseptics, stimulate healing with rosehip or sea buckthorn oils. It is also not forbidden to use cream for dryness and flaking.
- Leukoplakia. Stop smoking, eliminate spicy foods from your diet. For therapy, use a solution of vitamin A (topically), E, B6 - orally for 30 days.
- Candidiasis. Apply Lamisil cream three times a day to the crack. Consultation with a specialist is recommended.
- Tuberculosis. Treatment against the background of tuberculosis is carried out in conjunction with the main therapy. Cracks in the corners of the lips are eliminated with an antiseptic and anti-tuberculosis drugs. In such a situation, a person complains that the corners of his lips hurt.
- Syphilis. Therapy is similar to tuberculosis. As an addition, agents to eliminate candidiasis can be used.
- Allergy. The use of antiallergic drugs externally and internally. Termination of exposure to the irritating factor.
- Weather. Reducing time spent outdoors, using lip liner. Treatment with Bepanten, Panthenol.
- Hypovitaminosis B2. Taking B vitamins, visiting a specialized doctor. Rosehip oil and Solcoseryl are used for healing.
- Anemia, thyroid disease, HIV infection. Treatment is carried out taking into account the local picture. Similarly with therapy for candidiasis and leukoplakia.
- Atopic cheilitis. A diet excluding alcohol, sweets, and fatty foods. Taking antiallergic drugs, vitamins. Anesthesia, use of antiseptics, use of steroid liniments: adults – Lorinden-S; children - Traumeel-S.
- Chronic recurrent crack. Maintaining oral hygiene, bandages with solcoseryl, correction of emotional background, treatment of concomitant pathologies.
You should forever give up the habit of licking your lips outside in windy weather.
Folk remedies
Many people are treated with folk remedies, which sometimes drive themselves into a serious trap. Despite the harmlessness of irritation in the pharynx area, it can cause irreparable harm to the body.
- Ear wax will help with cracks in the corners of your mouth. You need to take it out with a cotton swab and lubricate the angulite. This method is also effective for herpes.
- Thermal water is also a good helper in the fight against cracks. An analogue of such treatment is hygienic lipstick. 5-6 times a day is enough for the wounds to begin to heal and go away.
- Goose fat, beeswax, and Vaseline are used for angulitis on the corners of the pharynx. Olive, rose hip, tea tree, and sea buckthorn oils are effective. Infusions of chamomile, calendula, and sage help. To soften the surface of the crust on the crack, it is smeared with honey or butter.
- A common folk remedy for wounds on the corners of the mouth is the juice of Kalanchoe leaves, fresh stems of celandine, plantain, and garlic. The disadvantage of this treatment is the possible burning sensation. It shouldn't be scary.
- Use hair that needs to be rubbed every day along the edges of the lips. Perhaps the method helps, to each his own. They also use the dull side of a knife to remove cracks. They are passed over the inflamed area several times a day.
Causes
Cheilitis is a polymorphic and multifactorial disease that can be triggered by infections, physical and chemical environmental factors, as well as internal characteristics of the body. Among them:
- constant exposure to the open air - inflammation and peeling of the lips occurs when chapped by hot or cold air, excessive insolation;
- the presence of chronic diseases with skin manifestations of symptoms - various types of dermatitis, psoriasis, lupus erythematosus, lichen planus, syphilis, etc.;
- allergic reactions of the body - mainly with food allergies;
- tissue irritation from regular exposure to chemicals, including medications (for example, nasal drops);
- various neurological disorders, severe stressful situations, depression, constant anxiety;
- endocrine abnormalities - primarily hyperfunction of the thyroid gland, diabetes mellitus.