A rheumatologist is a specialist in the study, examination and treatment of rheumatological diseases, as well as the development of measures for their prevention. Rheumatology, as one of the specializations of internal medicine, deals with the diagnosis and determination of therapy against diseases of the joints and connective tissue associated with rheumatism. This field is closely related to cardiology, endocrinology, nephrology, hematology, and indirectly to immunology, toxicology, infectology, neurosurgery, so a rheumatologist simply needs specialized knowledge in these areas of medicine. A doctor of such a wide profile is able to correctly establish a diagnosis and describe a detailed treatment regimen, taking into account all the features of rheumatic diseases.
Rheumatologist: what does he do?
The main field of activity of this doctor is the fight against rheumatological diseases that affect connective tissues, blood vessels and joints in the human body. When a rheumatologist sees a patient, he first of all collects his life history and medical history, finds out all the symptoms that worry the patient, and prescribes additional tests to make an adequate diagnosis. It is for this reason that a rheumatologist must also be a qualified diagnostician.
Content:
- Rheumatologist: what does he do?
- Body parts and tissues affected by rheumatological diseases
- Diseases treated by a rheumatologist
- Who is a rheumatologist-cardiologist, why should you contact him?
- When to visit a rheumatologist
- Pediatric rheumatology is a separate area of the healthcare industry
- Methods of diagnosis and treatment relevant for rheumatological lesions of the body
Having established which disease is troubling the patient, the doctor prescribes a treatment regimen in order to reduce symptoms, make the patient feel better, and overcome degenerative or dystrophic processes in the body that cause a specific disease.
The development of preventive measures, as well as therapy to support patients with chronic forms of rheumatological diseases, also falls under the responsibility of rheumatologists.
"Old age" is being treated
However, a person may remain exposed to ineffective therapy for a very long time. He has “arthrosis”, everyone has it and it’s “too early” to go to a rheumatologist. This may be explained by the fact that, as a rule, regional clinics do not have their own rheumatologist specialists, and in regional clinics their appointment is limited by the availability of appropriate quotas or the availability of the corresponding doctors. The patient is simply not referred to a rheumatologist. It is quite difficult to determine the need to see a rheumatologist. Although such cases also occur in practice, when patients themselves “find” their way to a rheumatologist.
The process is delayed, the “therapeutic window” is closing. And at some point, a person, especially in old age, is informed that now it is supposedly “too late” to see a rheumatologist and in general “old age cannot be cured.” It is not true. Even if the therapeutic window has been missed, regardless of age, modern medicine has answers to many challenges. The modern level of medicine makes it possible to improve the quality of life at any age.
Diseases treated by a rheumatologist
All diseases with a characteristic rheumatoid nature are classified according to various criteria. So, for example, they distinguish:
- dystrophic and inflammatory joint processes: these include gout, all types of arthritis (idiopathic, reactive, rheumatoid, infectious, juvenile), ankylosing spondylitis, osteoarthritis;
- systemic vasculitis: lesions that differ in etiology, but have the same manifestation - inflammatory processes in blood vessels. Among them, Wegener's granulomatosis, periarteritis nodosa, and Buerger's disease are common;
- systemic autoimmune connective tissue diseases: scleroderma, lupus erythematosus, Behcet's disease;
- acute rheumatic fever: characterized by the development of pathological processes in the membranes of the heart;
- microscopic vasculitis, Horton's arteritis, hypereosinophilic angiitis are classified as a separate group of rheumatoid diseases.
Arthritis is a process of inflammation and deformation of the inner layer of the joint capsule and cartilage tissue. They can develop as a consequence of psoriasis, previous genitourinary and intestinal infections, or as a result of disturbances in the functioning of the immune system. Characterized by restrictions in mobility, pain, curvature of the limbs or spine.
Gout is a pathological condition in which uric acid crystals are deposited in the joints.
Ankylosing spondylitis is an inflammatory process of an autoimmune nature that affects the intervertebral discs.
Osteoarthritis is an inflammatory disease due to which cartilage tissue loses the substances that give it density.
Vasculitis usually occurs due to disturbances in the functioning of the immune system. Wegener's granulomatosis is a process of inflammation of the arteries, arterioles, capillaries and venules of the eyes, kidneys and respiratory tract. At the site of inflammation, a nodule forms, which dies over time. Periarthritis nodosa is an inflammation of the arterial walls with the formation of microaneurysms. Buerger's disease is characterized by partial or complete occlusion of the cavities of the arteries.
Scleroderma or systemic sclerosis is the process of inflammation of small blood vessels, as a result of which fibrous tissue begins to grow around them and collagen accumulates. At the same time, the walls of the vessels thicken, the lumen of their cavities decreases.
Systemic lupus erythematosus is a disease in which the body’s immune system begins to actively produce antibodies to the DNA of its own cells. A rash appears in the cheekbone area, ulcers appear in the mouth, and convulsions, pleurisy, psychosis, anemia, pleurisy, and pericarditis also accompany the lesion.
Behçet's disease is an inflammatory process in the blood vessels of the mucous membranes of the eyes, mouth, gastrointestinal tract and genitals, and causes the development of ulcerative formations.
Microscopic vasculitis is inflammation of the blood vessels of internal organs, mainly the kidneys and lungs.
Horton's arteritis affects the temporal artery and leads to a narrowing of its lumen.
Rheumatism itself has several forms of manifestation:
- rheumatic carditis, which negatively affects the lining of the heart;
- rheumopolyarthritis – inflammatory processes in the joints;
- rheumopleuritis - inflammation of the lining of the lungs, which is autoimmune in nature;
- cutaneous rheumatism with the formation of erythema and nodules in the subcutaneous tissue.
Treatment methods and follow-up features
The course of treatment by a rheumatologist depends on the specific disease and its severity. Unfortunately, in the case of degenerative and inflammatory diseases of bones, joints and connective tissue, treatment is usually long-term.
In most cases, non-steroidal anti-inflammatory drugs are used to relieve rheumatic pain. Sometimes antibiotics and stronger analgesics may be prescribed. In severe cases, glucocorticosteroids are used, which suppress the immune system and have a powerful anti-inflammatory effect.
These and other drugs, which in addition to alleviating the symptoms of the disease, also inhibit the destruction of joints. Reception should be started as early as possible to avoid unpleasant complications and degenerative changes. It should be remembered that the nature of most rheumatic diseases is such that the pills must be taken constantly; withdrawal may cause a relapse.
Physiotherapy is also very important, thanks to which you can stop the progression of the disease, and sometimes even restore some motor functions of damaged joints. The doctor may prescribe procedures such as:
- Kinesitherapy . The technique is based on performing active and passive exercises that are designed to improve the functioning of diseased joints.
- Medical massage . Reduces muscle tension and stiffness, improves local blood circulation and blood supply to tissues.
- Electrophoresis . The procedure is a method of delivering drugs directly to the affected organ. The technology is based on the use of weak electric current discharges and injections. Electrophoresis helps reduce swelling, reduce pain, and speed up cellular metabolism.
- Ultrasound therapy . The method promotes the resorption of swelling and helps in the restoration of damaged tissue.
- Acupuncture . The technique helps to get rid of pain and accelerates regeneration processes.
Along with therapy, the doctor will give recommendations regarding lifestyle. The topic of proper nutrition with limited salt and maintaining a healthy body weight, as well as other preventive measures will be discussed: quitting smoking, maintaining a drinking regime, minimizing stress, etc.
Who is a rheumatologist-cardiologist, why should you contact him?
Having studied the above classification of diseases, you can understand that many rheumatological diseases have a direct effect on the heart and blood vessels.
A cardiologist-rheumatologist, in fact, is a related doctor, and can make the most accurate diagnosis in case of manifestations:
- endocarditis;
- myocardial damage;
- vascular obstruction;
- development of arrhythmias.
All these symptoms can be caused directly by rheumatism, the treatment of which is mainly the activity of a cardiologist-rheumatologist. Systemic lupus erythematosus, vasculitis and scleroderma are also reasons to consult a specialist in these related fields.
How is the first appointment and diagnosis carried out?
No special preparation is required to visit a doctor. It is enough to take with you a medical card and the results of the latest studies, if available (urinalysis, blood tests, ultrasound, etc.).
A visit to a rheumatologist consists of several stages. The first of them is a detailed interview, that is, obtaining information about the declared ailments.
The rheumatologist may ask:
- Where exactly is the pain concentrated (for example, which joints hurt, maybe the pain affects the entire limb or several fingers)?
- Is the pain worst at night or during the day?
- Is morning stiffness accompanied by morning stiffness and how long does it last?
- Was there swelling of the joints or redness?
- Are the symptoms episodic or chronic?
- Does the pain get worse when you are immobile?
- How intense is the pain?
- Was the symptoms preceded by an infection (eg, urinary tract infection, pharyngitis)?
The survey may focus on other symptoms, comorbidities, or even illnesses that run in family members. Questions that seem to be unrelated to the problem that is the reason for consultation (for example, bad habits or intestinal diseases in parents) should not come as a surprise.
The next step is an examination, and the doctor evaluates not only the condition of the joints. Depending on your symptoms, your rheumatologist may also examine your skin, nails, lymph nodes, or abdomen.
Unfortunately, it happens that the first visit does not provide grounds for making a final diagnosis and drawing up a treatment plan. Sometimes, even with the efforts of the doctor and painstaking preparation on the part of the patient, there is not enough information to make decisions. This is due to the fact that some rheumatic diseases take years to develop, and the full picture appears only with time. In any case, you cannot do without additional examinations.
When to visit a rheumatologist
The main symptom that should alert a person and force him to make an appointment with a rheumatologist is systematically recurring pain, concentrated around one or several joints. Other reasons for visiting a doctor are changes in the shape and appearance of the joints, and a decrease in their mobility.
People with a hereditary predisposition need to be constantly monitored by a specialist and undergo special examinations from time to time.
Increasing viral diseases, such as tonsillitis, are also a reason to consult a rheumatologist. The fact is that systemic inflammatory diseases, which are provoked by viral pathogens, affect, among other things, joints and connective tissues. In addition, any tendency to sore throats and infectious diseases indicates the peculiarities of the functioning of the immune system, which the rheumatologist also pays attention to.
A feeling of stiffness in the back, crunching in the joints and spine, accompanied by the appearance of inflammation and swelling also indicates that it is time to make an appointment with a doctor or call a doctor at home.
Constantly elevated body temperature, increased temperature of the skin on the joint, pain, aches and weakness, stiffness in the morning are a sufficient set of symptoms that require consultation with a rheumatologist.
Are joint problems always arthrosis?
Very often, joint pain is associated in patients with arthrosis. The diagnosis is considered universal: if the joints hurt, it means that the cartilage has worn out. In fact, other diseases have similar symptoms. It manifests itself in pathologies of ligaments and tendons, and in injuries to periarticular tissues, for example due to a meniscus tear.
Almost all people over 40 have degenerative changes in cartilage tissue to one degree or another. They do not always lead to arthrosis in full. Therefore, symptoms can indicate anything, even serious systemic diseases. Only an experienced specialist - a rheumatologist or orthopedist - can determine the cause based on the diagnostic results.
Arthrosis is not the only cause of joint pain
Pediatric rheumatology is a separate area of the healthcare industry
Despite the fact that most rheumatoid diseases manifest themselves in adults, the prerequisites for their appearance can be detected in childhood. In addition, inflammatory processes in connective tissues, especially those that have hereditary preconditions, begin to cause concern even in childhood. Such lesions are extremely dangerous, since, if not detected at a very young age, in adult life they can cause serious inconvenience to a person, and sometimes even cause disability.
It is for this reason that a pediatric rheumatologist must be a highly qualified specialist who is well versed in the problem and the characteristics of the child’s body. For example, diseases such as sore throat in children are one of the decisive factors in the development of rheumatism, which a pediatrician must know about.
There are frequent cases of a child being affected by rheumatic fever - such a disease requires the prescription of appropriate antibiotics, otherwise there is a risk of developing heart defects in the form of complications after the disease.
A little about drug blockades
There is a period when basic therapy for the disease is most effective. It is called the “therapeutic window”. With arthritis, for example, it lasts about three months. The inflammatory process is in the primary phase. Sometimes at this stage it is enough to make one blockade and the pain syndrome will disappear forever.
Unfortunately, there is a strong opinion that the body gets used to drug blockades. There are doctors who convey a biased attitude towards this treatment method. The argument is that once you get used to it, the medications won't help anymore. Guided by this opinion, many people who have shoulder or knee pain refuse joint therapy at the initial stage and miss a very important period. The disease is progressing.
In fact, a timely and correctly performed blockade gives positive results. The technique is successfully used in Europe and Israel, and you should not be afraid of it if you trust your specialist. But only a few people trust it, because there are not many specialists in joint diseases.
In what cases should you consult a rheumatologist? We present the TOP 10 reasons in the video below:
Additional diagnostic methods
Despite the enormous progress in medicine, the importance of traditional X-ray examinations of bones and joints cannot be overestimated. If in doubt, more extensive imaging, such as a CT scan or magnetic resonance imaging, may be needed. Ultrasound examination is becoming increasingly important. The study allows us to evaluate early inflammatory changes in joints, periarticular tissues and peripheral nerves.
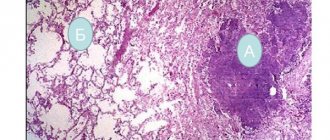
In some cases, histopathological examination of biopsied tissue may be required to make a diagnosis. In this case, hospitalization may be required because some procedures involving tissue collection can only be performed in a hospital setting.
The doctor will also order laboratory tests. Along with a traditional general blood test, a proteinogram (analysis of the protein composition of the blood) and rheumatic tests may be required. In some cases, consultations with specialists in other fields of medicine may be required: pulmonologist, endocrinologist, cardiologist, hepatologist and others.