Post-injection abscess is a complication that occurs after intravenous or intramuscular administration (injection) of drugs. It progresses and is treated differently from other abscesses. The essence of the process is that a purulent inflammatory focus is formed with tissue melting in the place where the injection was given.
- Causes
- Places of occurrence of post-injection abscesses
- Symptoms
- Features and complications
- Diagnostics
- Treatment (therapy)
- Prevention
Causes
The reason in most cases is that the rules of antisepsis and asepsis were violated when administering the injection. Ways of infection entering tissues with compromised integrity:
- dirty hands of doctors and nurses
- contaminated medicine, syringe, cotton wool or other injection equipment
- the patient's skin, if it has not been treated before and after the injection
Other possible, but rarer, causes:
- the medicine was administered by mistake (for example, a drug for intravenous administration was injected into the patient’s buttock. In this case, the medicine does not dissolve or occurs slowly, which leads to the formation of an aseptic infiltrate. After which fluid stagnates in the tissues, which causes further complications)
- violation of the injection technique (the needle did not reach the muscle, the needle was not inserted completely, a needle was used that was too short, for example, from a syringe for injecting insulin)
- long-term administration of drugs that cause tissue irritation (mainly magnesium sulfate or antibacterial solutions)
- many injections in one area (long therapy)
- obesity in humans (the layer of fat is so thick that the drug does not enter the muscle, but into the fat, not reaching the muscle layer)
- needle entering a vessel
- infection with dirty hands (a person scratches or scratches the injection site)
- HIV
- old age, as a result of which the body’s defenses weaken
- bedsores
- purulent skin infections
- autoimmune pathologies
- increased allergy status
How to behave after surgery?
After the operation, you will remain in the hospital for 1 to 5 days, depending on the complexity of the operation. You will be prescribed, if necessary, antibacterial therapy and dressings with wound-healing ointments will be performed. After surgery, you may need to hold stool to allow the wound to heal.
Your doctor will teach you how to care for the wound, and it is extremely important to follow these recommendations strictly. One of the important recommendations is to irrigate the wound with a stream of water 3-4 times a day for the purpose of mechanical cleaning and periodic medical monitoring of proper healing in the direction “from the bottom of the wound.” After training, as a rule, you will be able to perform dressings yourself at home.
Places of occurrence of post-injection abscesses
Basically, injections are given in the buttock, because the complication in question often occurs there. This area under the skin contains a large amount of fat. Therefore, if infection occurs, the infection will actively develop in this layer.
The second most common area for abscess development after an injection is the thighs. In such cases, patients prefer to give injections themselves, so they inject the medicine not into the buttock, but into the thigh. If they do not follow the rules of asepsis, the soft tissues may become infected.
General information
Post-injection abscesses are purulent-inflammatory localized foci that arise in soft tissues as a result of non-compliance with the rules of asepsis and administration technique during intravenous, intramuscular and other injections. In this case, the sharpness and length of the needle, the accuracy of choosing the injection site and the frequency of injections in the same place are important. In addition, the cause may be the introduction of various irritants, which, even if all instructions are followed, do not lead to resorption, these include Diclofenac , Reopirin (mainly when administered into the subcutaneous tissue layer).
Most often, the development of an abscess is caused by intramuscular injections into the buttocks, in more rare cases - into the forearm, into the paravertebral and subscapular region.
ICD-10 code for post-injection abscess
Skin abscesses, carbuncles and boils of various origins are assigned the ICD-10 code: L02. Further division takes into account their localization:
- L02.0 Abscess on the face.
- L02.1 Abscess on the neck.
- L02.2 Abscess on the trunk.
- L02.3 Abscess of the buttock.
- L02.4 Abscess of extremities.
- L02.8 Abscess of other locations.
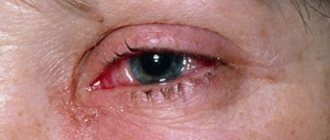
Symptoms
Symptoms may be more or less severe. It depends on how deep the inflammation began. If the depth is large, then the symptoms will not be externally noticeable. But if you press on the affected area, you may feel pain (even if the injection area is not red or swollen).
Local symptoms:
- the drug administration area is hyperemic
- swelling of the injection area
- painful sensations when touching the injection site
- After some time, pain occurs, even if you do not press on the injection site
- symptom of fluctuation (fingers are placed on the swelling, when pressing on the skin with the fingers of one limb, the tissue and fingers on the other limb are raised, because excess fluid collects in the tissues)
- the skin of the affected leg is hot, which indicates an increase in temperature
- in the absence of treatment, the process generalizes: fistulas are formed inside and outside, which aggravates the infection
General symptoms of an abscess after an injection:
- weakness in the body
- fatigue
- low appetite
- increased sweating
- temperature rise 37-38-39-40˚ in different cases
- low performance
Even if you become infected during the injection, the abscess will develop gradually. First, the infiltrate accumulates, and only then purulent processes begin. To prevent the complication from getting worse, it is important to get treatment on time.
How to treat an abscess
The abscess is removed by a surgeon. If you do not seek medical help in a timely manner, this can lead to even more serious consequences for the patient.
- If the inflammatory process is infiltrative and non-purulent, conservative treatment is used. Physiotherapy, absorbable medications, and warm compresses are prescribed. It is recommended to lubricate the injection site with an alcohol solution of iodine.
- If pus begins to form at the site of inflammation, the doctor at our clinic will perform a puncture, remove the accumulated pus and rinse the cavity.
- If the abscess is deep, surgical treatment is performed. An incision is made at the site of the abscess, the cavity is washed and drained.
- In case of an extensive process and symptoms of general intoxication, treatment with antibiotics, immunomodulators, and vitamins is prescribed.
Qualified specialists at our clinic treat purulent inflammatory diseases using the most effective and safe methods and medications.
Diagnostic methods in surgery:
- Doppler in surgery
- Colonoscopy
- Angiography
- CT scan
- Gastroscopy
- MRI
- Abdominal ultrasound
- X-ray
- Endoscopy
Prices:
| Code | Name of service | Prices |
| 1 | Initial appointment | 1200 |
| 2 | Repeated appointment | 900 |
| 3 | Calling a surgeon to your home | 3500 |
| 4 | Abdominal ultrasound | 2200 |
| 5 | Ultrasound of veins and vessels | 2400 |
| 6 | Doppler 2-3 trimester | 1200 |
| 7 | Rectoscopy | 1500 |
Features and complications
Post-injection abscesses differ from abscesses of other etiologies in that there is an infiltrative capsule and a pyogenic membrane. The capsule may rupture if there is a lot of pus in it (untreated), and then nearby tissues will become infected. This leads to the formation of fistulas and extensive phlegmon. This is the complication that is recorded in most cases of neglected treatment. Also in rare cases, doctors detect osteomyelitis and sepsis.
Pathogenesis
An abscess after injection is a complication that is caused by the formation of a purulent inflammatory infiltrate in the cavity in the soft tissue layers, most often as a result of infection. The cavity is formed by the pyogenic membrane, and on the inner wall there is a lining layer of granulocytes, which prevents the pus from “resolving.”
Abscess structure
In the pathogenesis of complications after injections, the physicochemical properties of the administered drugs, the frequency and duration of their exposure, and compliance with the recommendations of the method of administration are of greatest importance. Tissue damage is chemical or occurs during repeated administration of drugs in one place, disrupting tissue trophism and promoting the development of pathogenic microflora, and is also possible as a result of an accidental needle entering a vessel or a complication of infusion therapy, causing the subsequent occurrence of a hematoma in which microorganisms can begin to multiply.
At the stage of infiltration, cell damage and death stimulate the release of many lysosomal enzymes into the extracellular space, changing the metabolism in the lesion - slowing it down in the area of necrosis and increasing it in adjacent areas. This is expressed in an increase in oxygen consumption and various nutrients, the development of acidosis and the accumulation of under-oxidized products such as lactic, pyruvic acid, etc. Due to increased blood flow, dilation of blood vessels and increased permeability, the release of leukocytes and macrophages occurs. Swelling is caused by a local influx of fluid, and pain is caused by pressure on the nerve endings. Abscess formation leads to the formation of pus, consisting of dead tissue and dead cells of the immune system, which is located in the center of the inflammation and is not eliminated until there is an opportunity for its outflow, for example, by drainage.
Diagnostics
The diagnosis is made when a patient comes to the doctor with complaints. History helps in accurate diagnosis. But the doctor may prescribe the following studies:
- general blood analysis
- OA urine
- blood biochemistry
- culture of infiltrate for microflora
If the complication is chronic, then ultrasound diagnostics is done in order to understand how far the inflammation has spread. In the most advanced situations, a CT or MRI will be prescribed.
What studies should be performed in preparation for surgical treatment?
Before the operation, you need to perform a number of standard tests, however, if the disease worsens with the formation of an abscess, the operation is performed for emergency reasons, so waiting for test results should not delay surgical treatment.
In addition to general clinical standard laboratory tests, if a complex fistula or deep-seated abscess is suspected, a number of additional diagnostic procedures may be needed: MRI of the pelvis, ultrasound examination of the pelvis and perineal tissue.
As a rule, the external fistula opening is detected during examination, the internal one - during digital examination of the rectum or anoscopy. However, in some cases - with recurrent, complex fistulas - there is a need to trace the fistula tract along its entire length, evaluate its relationship with the structures of the perineum, and determine the presence of additional tracts or leaks. Today, only MRI of the pelvic organs has this capability, due to its high specificity and sensitivity. That is why this study is the main method for diagnosing complex rectal fistulas.
To objectively assess the functional state of the sphincter (that is, how well it contracts and performs its function), in some cases it is necessary to perform anorectal manometry. The indications and need for it in your case will be determined by your attending physician.
In addition, the patient is usually asked to fill out a special questionnaire, the results of which can be used to determine the degree of continentness (retention of solid and liquid stools and gases) before surgery.
In women, it is often necessary to conduct a vaginal examination to exclude communication between the fistula tract and the vagina when the fistula is located anteriorly.
To exclude other diseases of the colon (in patients over 45 years of age, in cases of colon cancer in relatives, in the presence of two or more fistula tracts), a colonoscopy may be necessary.
Treatment (therapy)
As soon as you discover that there is something wrong with the injection site, immediately go for an in-person consultation with a doctor. Soft tissues are subject to melting by dead cells, which increases the area of spread of the pathological process. Surgical necrectomy with enzymatic necrolysis, formation of a primary suture and vacuum aspiration of purulent masses through drainages are mainly used. After this, flow-wash drainage is performed. The wounds will heal faster this way than if the drug is administered openly.
Washing wounds is done with proteolytic enzymes and sodium hypochlorite. This makes it possible to avoid secondary infection. Previously, the attachment of Pseudomonas aeruginosa often occurred until the procedure described above was developed.
An abscess on the gluteal muscle is treated with puncture. But in recent years, doctors are increasingly less likely to give preference to this method, because purulent streaks and phlegmon often form, or the process becomes chronic. This is very undesirable, therefore the puncture is gradually abandoned.
When developing general therapy for a patient, the severity of the abscess and the nature of the pathogen that multiplies, causing the pathological process, are taken into account. Broad-spectrum antibiotics are relevant. Along with this, painkillers and detoxification drugs are used. But general therapy does not in all cases make it possible to get rid of the problem. Sometimes more and more tissue begins to die, which can result in sepsis. The pus must be drained out so that the process does not progress.
If an infiltrate appears, they stop injecting drugs into the affected area and actively treat the inflammatory process. Physiotherapy with dynamic currents, electrophoresis of proteolytic enzymes and gamma globulin are relevant. If the patient has undergone three or four such sessions, but he does not feel better, and there is pain, then surgical treatment is appropriate. The need for more serious therapy is also determined using ultrasound.
What is a fistula
A fistula is a pathological, normally non-existent, passage in the form of a tube connecting the lumen of a hollow organ with the external environment or the lumen of another organ. A rectal fistula, a kind of “tunnel,” connects the lumen of the rectum with the skin of the perineum, buttocks or (rarely) other hollow organs, sharply reducing the patient’s quality of life. This pathological process can involve a large portion of sphincter muscles, which initially characterizes such a fistula as complex and does not allow for “minimally invasive” treatment. In such a situation, a careful assessment of the degree of involvement of muscle structures and planning of special techniques for economical excision of the fistula with subsequent plastic closure of the resulting defect are required.
Important! Such operations must be performed by expert surgeons with extensive experience in such interventions, otherwise the likelihood of relapse (recurrence of the disease) increases several times.
Fistulas have the following structure:
- internal opening: it is usually the affected anal crypt (that is, the most terminal part of the gland duct). The crypt is connected by a duct to the anal gland, located in the space between the sphincters. It is the inflammation of this gland that in the vast majority of cases leads to the development of the disease (Fig. 2).
Figure 2. Stages of fistula formation: a) - anal gland with an excretory duct, b) - inflammatory process in the gland, with a forming abscess (abscess) c) - formed fistula tract.
- fistula tract, which can be tortuous, have cavities and branches
- external opening: but most often located on the skin of the perineum near the anus (Fig. 3), sometimes in the vagina or urethra (urethra).
Important! If you have the slightest suspicion of a rectal fistula, you should immediately consult a specialist. If treatment is untimely or inadequate, the disease can be complicated by acute inflammation and additional purulent leaks, which significantly worsens the prognosis!
However, it also happens that the fistula tract ends blindly in the pararectal (peri-rectal) tissue, tissues of the perineum, buttocks, that is, it has only an internal opening of the fistula, which opens from the mucous membrane of the rectum and has no “exit” to the outside.
Figure 3. External opening of the fistula
Prevention
After an abscess of the muscle layer (even if the person is cured in time), a scar remains on the skin. Since there was deformation of the fat layer, a dimple remains in that place. Therefore, it is important to follow the rules of prevention. It is important to administer medications correctly, taking into account the frequency, speed and dosage of drug administration. You also need to know whether the medications that are taken into the same syringe are compatible.
When an injection is given, the needle must reach the muscle, passing through the fat. In order for the drug to be absorbed well, you need to lightly massage the area where it was injected. And it is important to do this with a disinfected cotton swab and not with dirty hands. If you need to give several injections (on one day and on subsequent days), try not to fall into the same area, deviate at least a couple of mm.
Follow the rules of asepsis and antiseptics. Before giving the injection, the hands of the person giving it should be thoroughly washed and wiped with a disinfectant. Before and after the injection, the area should be treated with an antiseptic. Syringes and other consumables should be disposable, this greatly reduces the risk of infection.
It is necessary to correctly determine the points where the drug can be administered. It is difficult to give injections to patients with a high body mass index. It is difficult for them to get a needle through the fat to the muscle. In this case, the injection should be given where there is less fat.
Anatomy of the rectum and perianal region, functions of the obturator apparatus
The rectum and anal canal are the final sections of the digestive tract. The immediate tasks of the rectum are the accumulation, formation and excretion of intestinal contents and gases. The functions of the anal canal are unique: a system of nervous reflexes and a complex muscle complex provide one of the most important functions of the body - control of bowel movements, as well as differentiation of the composition of intestinal contents without the need for conscious assessment and subsequent “smart” control of evacuation. In other words, a healthy person most of the time does not think about what kind of contents are in the rectum, whether it is necessary and whether it is possible to retain it in a given situation. All this is controlled unconsciously, thanks to multi-level neuromuscular self-regulation of the holding process.
The approximate boundary between the rectum and the anal canal on the side of the mucous membrane (lumen) of the intestine is formed by the so-called dentate line. There are vertical folds on it, alternating with depressions - crypts. The ducts of the anal glands open into the crypts. The mucus produced by these glands facilitates the sliding of intestinal contents as they pass through the anal canal. Circumstances such as trauma, swelling of the mucous membrane due to defecation disorders, chronic intestinal diseases can lead to inflammatory changes in the crypts and anal glands.
Outside the mucous membrane there is a complex of muscles - these are the sphincter muscles mentioned above, which provide the function of retention and excretion. There are internal and external sphincters. The internal sphincter forms the so-called resting tone, uninterruptedly ensuring the tightness of the anal canal. Its regulation and reduction occur unconsciously, that is, without our will. The external sphincter surrounds the internal one and consists of several layers (portions). Its reduction occurs due to our volitional effort (Fig. 1).
Figure 1. Schematic representation of the rectal sphincters
What to do if an abscess forms?
An abscess is not only painful, but also quite a dangerous condition. It does not always break out; in some cases, pus pours out under the skin, causing severe inflammation. Therefore, when the first signs appear, you should call a surgeon to your home.
or come for a consultation with this specialist yourself.
And if you don’t know which Moscow clinics provide such services, you can collect the necessary data on the “Your Doctor” website. This resource also allows you to make an appointment at a convenient time.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Author:
Mumladze Koba Vazhaevich Anesthesiology and resuscitation
Back to section