The digestive system is considered one of the most complex structures of the human body, which is multifunctional, therefore, malfunctions often occur in its work leading to the development of various diseases of the digestive system. One of these is gastric cardia insufficiency, which will be easier to understand once you understand the concepts. Many people suffering from gastric cardia insufficiency do not even know what it is. This disease refers to pathologies of the motor function of the gastrointestinal tract. Since the occurrence of tumors and inflammation is not observed, insufficiency of the gastric cardia is considered a functional disease.
Description of the pathology
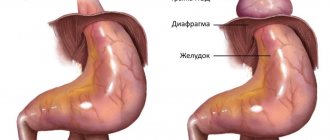
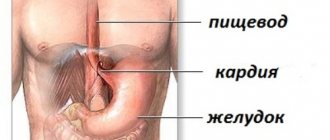
Cardia deficiency refers to disturbances in the functioning of the digestive system that occurred due to the penetration of acidic juice into the esophagus. Every person has sphincters - special valves that filter the passage of contents from one organ to another. If there is a malfunction of the muscular sphincter of the stomach, doctors diagnose cardia insufficiency; only the attending doctor knows what it is and how to get rid of it in an individual case.
During normal functioning of the digestive system, the sphincter opens during food consumption, after which it completely blocks the channel. If functional problems arise, the cardia is not able to retain the acidic contents of the stomach, which then penetrates the esophagus. As a result, cardia insufficiency develops, as well as the inability to close the sphincter, called chalazia in medical practice.
Surgical methods for treating achalasia cardia
Puchkov K.V., Rodichenko D.S. Manual suture in endoscopic surgery: monograph. - M.: MEDPRACTIKA, 2004. - 140 p.
Of the many surgical methods proposed for the treatment of esophageal achalasia, currently only those interventions based on extramucosal cardiomyotomy are mainly performed. One of the main ones is the method of extramucosal cardioplasty, performed according to Heller (E. Heller). The essence of the method is a longitudinal section of the muscular lining of the distal esophagus along its anterior wall for eight to ten centimeters. In this case, the myotomy should cover not only the area of narrowing and the cardiac part of the stomach, but also a partially expanded area of the esophagus. In this case, the edges of the dissected muscular membrane diverge in opposite directions, as a result, the underlying intact mucous membrane begins to bulge into the resulting defect.
According to the literature, good results after this type of surgery are observed in up to 90% of cases. The disadvantages of this technique are associated with leaving the esophageal mucosa unprotected over a large area (8-10 cm x 1 cm). Therefore, in places where the muscular lining of the esophagus is cut, diverticula and scars that deform the cardia can form, causing a relapse of the disease.
Mortality after Heller surgery averages about 1.5% (a number of authors give the figure 4%). The main cause of death is usually overlooked damage to the esophageal mucosa, which leads to mediastinitis (inflammation of the mediastinal tissue), pleurisy (inflammation of the pleura) and peritonitis (inflammation of the peritoneum). Trauma to the mucosa is observed in 6-10% of all operations, therefore, to prevent severe complications, it is extremely important to conduct a very thorough inspection of this area. If the surgeon discovers damage to the mucous membrane, it must be sutured. Also, unsatisfactory results are associated with the destruction of the cardinal sphincter and the development of peptic reflux esophagitis. And due to the possibility of closure and fusion of the dissected walls of the muscle layer, there is a recurrence of the disease, dysphagia and impaired emptying of the esophagus.
Very important!
To reduce mortality and the number of postoperative complications, it is necessary to cover the surgical defect of the esophageal wall with one’s own tissues, which is rarely performed by surgeons due to the technical complexity of this stage of the operation.
Today, there are a variety of ways to cover the mucous membrane. What can the omentum, the anterior wall of the stomach, and a section of the diaphragm be used for? It should be noted that options for closing the defect in the muscular lining of the esophagus with any synthetic materials are not advisable due to the development of bedsores in this place.
Very important!
To prevent the development of cardiac sphincter failure and reflux esophagitis, preserve the natural anatomical relationships of the esophagus, stomach and diaphragm as much as possible.
Reasons for development
Doctors identify several provoking factors for this disease.
- An improperly planned diet, especially overeating, significantly increases the likelihood of pathology.
- Being overweight also increases your risk of developing the disease.
- Various diseases of the gastrointestinal tract, especially ulcers and inflammation of the esophageal mucosa.
- Spasmodic attacks of the pylorus.
- Little physical activity weakens the muscle system, which increases the risk of disease.
- Constantly increased level of pressure in the abdominal area, explained by the process of bearing a child or ascites.
- Increased pressure inside the stomach.
- Surgical interventions to remove the sphincter.
- Excessive physical activity also leads to disturbances in the functioning of the cardia.
The disease develops as a result of the inability of the sphincter to retain acidic substances in the stomach. Food enters the stomach at low pressure, a few millimeters of mercury is enough. Reverse movement requires a load ten times greater. For this reason, with an increased degree of gas formation, reflux of stomach contents into the esophagus is possible, accompanied by characteristic clinical signs.
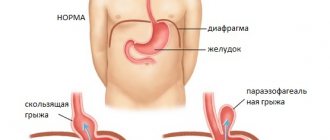
Doctors believe that the main mechanism for the progression of pathology is problems in the functioning of smooth muscle tissue located in the area of the diaphragm. The syndrome is characteristic of a chronic inflammatory process of the pancreas, with gastritis. The risks of pathology also increase with a diaphragmatic hernia.
In a healthy person, the sphincter is completely closed, except when eating. The cardia also blocks the return of contents into the stomach.
The sphincter must work without disturbances and ensure the proper functioning of the gastrointestinal tract. Otherwise, the mucous membrane of the esophagus is not able to regenerate, as a result, a person’s risk of developing gastrointestinal pathologies, for example, pancreatitis or gastritis, increases.
Doctors highlight a list of diseases that increase the likelihood of developing sphincter dysfunction.
- In the case of an anatomical anomaly, which is a hole in the diaphragm. The upper section of the gastrointestinal tract connects to the chest cavity, which in some cases provokes the development of the disease described above.
- Asthmatic disease and diabetes mellitus can also lead to the development of dysfunction of the cardia.
- Syndrome of loss of strength, called adynamia in medical practice.
- Various chronic diseases of the gastrointestinal tract, for example, ulcerative formation of the duodenum.
- Connective tissue pathologies (scleroderma).
Treatment of achalasia cardia. Drug therapy and cardiodilation.
It should be noted that pharmacotherapy (calcium channel blockers, nitrates, myotropic antispasmodics, anesthetics) is effective only in the first stage, in which mild and rare transient dysphagia is noted.
The generally accepted method of treatment is endoscopic bougienage of the esophagus, aimed at expanding the narrowed area, but, unfortunately, this occurs through tissue rupture, with the formation of rough scars in this area, which in the future only worsens the situation. The effect of bougienage of the esophagus is short-lived, repeated manipulations are required and after 4-5 procedures relief does not occur. In this situation, an operation is proposed - esophagomyotomy (dissection of part of the wall of the esophagus to the submucosal layer without opening the lumen of the organ), which allows you to restore normal swallowing and return the patient to a normal lifestyle.
At the same time, the endoscopic dilatation technique can be useful for the treatment of patients in the older age group and people with relapse of achalasia cardia who have previously undergone surgery. That is, for those patients for whom, due to concomitant diseases, surgical intervention is contraindicated or its implementation is technically extremely difficult.
Also, one of the minimally invasive methods of treating achalasia cardia is endoscopic intrasphincteric injection of botulinum toxin A. It is considered as a fairly effective alternative option for people who have absolute contraindications to endoscopic hydro- or pneumatic cardiodilation and surgical intervention, especially when it comes to patients in the older age group , about the presence of pronounced, severe concomitant pathology of the cardiovascular and bronchopulmonary systems. Treatment with botulinum toxin is safe, but it should be borne in mind that the effects on the lower esophageal sphincter often last only 2-3 months, and therefore additional repeated administration of this drug may be required.
Early surgery gives very good results, since in the narrowed area there are no scars from previous cardiodilation, and the muscle strength of the esophageal wall has not yet been depleted. But, even with a distended esophagus, good results are possible when using an adequate laparoscopic method.
Very important!
A feature of my approach to choosing treatment tactics for patients with achalasia cardia is the earlier determination of indications for surgical treatment using the laparoscopic method (through several punctures of the abdominal wall), without waiting for complications to develop and without wasting time on useless conservative treatment methods.
Stages of progression
The severity and prognosis for the outcome of the disease depends on the degree of development of dysfunction, as well as on the amount of gastric juice entering the esophagus.
There are three main degrees in medical practice.
- The first stage of development of the disease is characterized by mild clinical signs. The lower gastric valve has a standard degree of mobility, and a number of signs of the disease are absent.
- At the second stage of pathology progression, the mobility of the cardia decreases significantly. The level of gaping is more than 50% of the total size of the opening that connects the intestinal tract and the gastric tract. Some patients suffering from stage 2 cardiac insufficiency experience prolapse of the esophageal mucosa. Clinical signs of reflux appear.
- The final stage is characterized by absolute non-closure of the sphincter. Hole gaping level is 100%. However, peristalsis of the gastrointestinal tract is preserved. When performing diagnostic procedures, the patient experiences distal esophagitis. The disease affects the lower, 3rd part of the intestine. Pathology of the gastrointestinal tract of a gastroesophageal nature also gradually develops.
Cardiac insufficiency: stages of the disease
Cardia insufficiency occurs in the human body through 3 stages.
Table 2. Stages of the disease
| Stage | Description | Symptoms |
| I | Partial valve closure. The opened space occupies up to 1/3 of the diameter of the esophagus. | Frequently repeated belching of air. |
| II | The sphincter closes only 50%. Such a large gap risks the folds of the esophagus getting into the stomach. | Belching, discomfort in the central part of the peritoneum and prolapse of the mucous membrane. |
| III | Full opening of the sphincter. Despite the fact that the motility of the esophageal tube is preserved, an inflammatory process begins on its walls with the formation of erosions and ulcers. | Severe heartburn, epigastric discomfort, pain while eating, nausea and vomiting. Sometimes there is an increase in body temperature. |
The first degree of cardia insufficiency is mild. If belching occurs, you should immediately consult a specialist doctor.
Main symptoms of the disease
If a person is suspected of insufficiency of the gastric cardia, symptoms may be as follows:
- Heartburn
. The appearance of heartburn is not associated with food intake, that is, it occurs regardless of whether a person has eaten or not. Sometimes an attack of heartburn can be so severe that it deprives a person of peace. - Pain in the stomach area
. The intensity of pain can vary - from dull pain to a strong, intense burning sensation in the esophagus. - Belching of air and stomach contents
. Belching usually has a characteristic sour taste. If there is bile in the contents of the stomach, then the belching will have a bitter taste. - Nausea
. As the intensity of nausea increases, vomiting joins it. - Pain in the epigastric region
. The sensation of rumbling in the stomach arises from stretching of the esophageal mucosa and irritation by the acids contained in the gastric juice. - Dizziness, general weakness
. Fickle companions of gastric cardia insufficiency. Their appearance is associated with general disorders of the digestive tract. - With distal reflux, a whitish coating appears on the tongue
. This symptom is also accompanied by burning pain in the hypochondrium and a feeling of “transfusion” in the abdominal area. If a person develops gastroesophageal disease, the patient usually washes his food down with water. Smokers may want to pay attention to the fact that they wash down their cigarette with water. With a severe degree of esophagitis, problems with swallowing appear - precisely because the esophagus narrows slightly.
Features of treatment
In many cases, this pathology cannot be completely cured. You can only slow down its progression and improve the patient’s condition. But for this it is necessary to diagnose the disease in time and begin treatment. Cardia insufficiency is detected during a comprehensive examination. First of all, fibrogastroduodenoscopy is prescribed, which allows us to examine the condition of the mucous membrane of the esophagus and stomach. X-rays are used to evaluate the presence of a hernia or tumors, and daily pH measurements measure the acidity of gastric juice. To determine the quality of the sphincter itself and the degree of its contraction, manometry of the esophagus is performed.
Based on the results of this examination, treatment is prescribed. It is usually conservative, only in the presence of a hiatal hernia or tumors is surgical intervention indicated. But in order to prevent serious complications, treatment for gastric cardia insufficiency must be comprehensive. To do this, in addition to drug therapy, traditional methods and a special diet, it is necessary to cure or at least put into remission the gastrointestinal diseases that provoked the pathology. You also need to change your behavior and lifestyle.
Causes of burping air after eating
There are several recommendations that you can follow to reduce discomfort:
- do not overeat, reduce portions, and eat more often;
- wear loose, non-tightening clothing;
- sleep on a high pillow;
- walk more and do exercises that strengthen the abdominal muscles;
- avoid increased physical activity, especially on a full stomach;
- do not eat before bed, do not lie down during the day after eating;
- try to avoid weight gain;
- do not drink alcoholic beverages, soda, coffee, chocolate, fatty and spicy foods;
- be sure to quit smoking.
Drug therapy
In the complex treatment of pathology, different medications are necessarily used. First of all, these are means for the treatment of gastrointestinal pathologies that cause disruption of the sphincter. These can be gastroprotectors, antisecretory agents, enzymes to improve food digestion. Sometimes you need to take antibiotics to help get rid of Helicobacter, the main cause of gastritis.
There are also special drugs aimed at protecting the mucous membrane of the digestive tract, reducing the acidity of gastric juice, and relieving inflammation. These are Almagel, Maalox, Phosphalugel, Rennie, Ranitidine, Omeprazole. Sometimes prokinetics are prescribed, which help empty the stomach faster and increase the tone of the pylorus. These are Metoclopramide, Cerucal, Domperidone. They also help relieve nausea and vomiting. And to eliminate bloating and increased gas formation, defoamers are used, for example, Espumisan.
Diet
In the mildest cases, the patient’s condition can be corrected only with the help of proper nutrition. But a special diet is necessary at any stage of the pathology. The most important thing is to avoid filling your stomach and consuming gas-forming foods. To do this, you need to eat in small portions, 4-5 times a day. You should not eat before bed; at least 3 hours must pass after eating. It is also undesirable to eat food that is too hot or cold.
You should avoid drinking alcohol, carbonated drinks, fatty, spicy and fried foods, legumes, mushrooms, smoked meats, chocolate, coffee and strong tea. It is undesirable to eat onions, garlic, cabbage, sour fruits, fresh baked goods and sweets. The diet should contain a sufficient amount of animal proteins, which not only help accelerate tissue regeneration processes, but also increase the tone of the cardiac sphincter. It is recommended to boil or puree all food so that it does not linger in the stomach.
To alleviate the symptoms of cardia insufficiency, it is necessary to follow a certain diet, eliminating all foods that provoke reflux
Exercises
It is believed that exercise can strengthen the esophageal sphincter muscles. Strelnikova’s breathing exercises are considered especially effective. In addition, it is useful to walk, ride a bike, and swim. Any physical exercise is acceptable, except bending forward and lifting weights.
Traditional methods
Traditional treatment can be supplemented with folk remedies. Usually these are juices or decoctions of various medicinal plants. It is advisable to use them only on the recommendation of a doctor during remission. Most often it is recommended to drink decoctions of mint, valerian, St. John's wort, yarrow, and chamomile. Dill water effectively relieves bloating. In addition, the following recipes are used:
- in summer you can take juice from fresh plantain leaves, a tablespoon before each meal;
- A decoction of calamus root is taken half a glass half an hour before meals;
- mix dandelion flowers with sugar, leave, rub and strain, then dilute the syrup with warm water and drink before meals.
Diagnosis of gastric cardia insufficiency
To diagnose cardia deficiency, you need:
- X-ray of the upper part of the digestive system;
- endoscopy (examination of the inside of the esophagus);
- daily ambulatory pH-metry of the esophagus (test to determine the amount of acid in the esophagus);
- gastrofibroscopy (determines pathologies of the gastrointestinal tract);
- biopsy followed by histological examination;
fibrogastroduadenoscopy (FGDS) - examination of the gastric mucosa
Diagnosis of the disease
Due to mild symptoms, determining the stage of chalazia by external signs is quite problematic. The most effective way is endoscopic examination.
Endoscopy is a technique that is widely used to diagnose diseases of the gastrointestinal tract. An endoscope is a device consisting of a probe equipped with a camera and a monitor showing an image of the internal organs.
In addition to endoscopy, FGDS, ultrasound diagnostics, radiography with the use of a contrast agent and pH-metry are prescribed to make an accurate diagnosis. A comprehensive examination allows the gastroenterologist to adequately assess the condition of the esophageal mucosa, determine the degree of cardia insufficiency and identify concomitant pathologies.
Possible complications
Most people do not notice changes in the body as the pathology progresses. However, lack of timely treatment will lead to serious complications. These include the formation of ulcerative lesions in the gastrointestinal tract, inflammation of the mucous membrane of the esophagus, stricture of the esophagus, possible discomfort during swallowing, as well as prolapse of the digestive tract.
Once an acidic substance enters the throat, there is a possibility of developing problems with the respiratory system. Long-term development of cardia failure significantly increases the risk of cancer cells in the esophagus. Over time, Barrett's syndrome develops, characterized by the appearance of tissue-like formations in the body. Also, disorders in the functionality of the sphincter increase the likelihood of developing a malignant tumor of the esophagus - adenocarcinoma.
Traditional medicine
Pharmacists have in their arsenal a large number of drugs aimed at treating chalazia. Depending on the stage of the disease, appropriate medications are prescribed.
Table 1. The most common drugs
| A drug | Description |
| The action of the emulsion is based on inhibition of gastric juice production. Thanks to this, the content of hydrochloric acid in it is reduced to the required limit. Has an anesthetic effect. Due to the fact that it is a choleretic drug, a slight laxative effect is possible. | |
| Naturally based adsorbent. Stabilizes the microflora of mucous membranes and increases the gastroprotective functions of mucus. | |
| Antiemetic drug. Relieves hiccups, normalizes the activity of the gastrointestinal tract and enhances peristalsis. Promotes healing of ulcers. | |
| In addition to the antiemetic effect, the drug stimulates the muscle tone of the gastrointestinal tract. Normalizes the activity of the gastrointestinal tract and reduces the motor activity of the esophagus. Increases the tone of the lower valve of the esophagus, improves bowel movements without causing diarrhea. |
You should take medications only as prescribed by your doctor. In addition to taking medications, it is important to lead a healthy lifestyle and adhere to a diet.
How to treat the disease?
Treatment of this disease is carried out only comprehensively. The first thing that needs to be done is to treat the disease that provoked the development of cardia failure. If a person is overweight, then he needs to eat right or go on a diet. The second step of treatment is to reduce pressure in the abdominal cavity, especially in the case of ascites. The patient must visit a nutritionist to be prescribed specialized nutrition or a therapeutic diet.
Treatment of chalazia with the help of synthetic medications consists of regular use of regulators of motor activity of the lower valve of esophagitis. Domperidone and Metoclopramide are widely used. With their help, you can quickly eliminate the main symptoms of the disease and alleviate the patient’s general condition. The patient must also adhere to certain rules of behavior so as not to provoke an exacerbation of chalazia. He is advised to sleep with his head slightly elevated and not to wear tight clothing.
Increased physical activity should be completely avoided for some time. Gradually they can be increased, but with caution and under the supervision of the attending physician. In some cases, patients will need to change jobs. Surgical treatment of the disease is indicated only for advanced stages of the disease. The operation consists of suturing the muscles that form the cardia. After it is carried out, all symptoms of the disease, as a rule, decrease and soon completely disappear.
Symptoms of the disease can be eliminated with the help of some folk remedies. But before using them, it is recommended to visit a gastroenterologist to agree on this method of treatment. After all, not all traditional medicines are completely safe.
Questions most often asked by patients with achalasia cardia
What anesthesia do you use for laparoscopic treatment of achalasia cardia?
If you would like to learn in more detail about the methods of pain relief used in the surgical treatment of achalasia cardia, please carefully read the information posted on the website.
Is it necessary to somehow prepare for surgery for laparoscopic treatment of achalasia cardia?
If you are planning surgical treatment for achalasia cardia, I ask you to carefully study the preoperative preparation section.
Is it possible to simultaneously perform laparoscopic surgery for achalasia cardia and, for example, fibroids?
Minimally invasive surgery techniques allow two and sometimes three operations to be performed simultaneously during one anesthesia by a team of several surgeons. The issue of simultaneous operations is discussed in more detail in a special section of the site. Simultaneous performance of several surgical interventions will reduce the load on the body, reduce hospitalization time, and speed up the body’s recovery compared to performing several operations with an interval of 5-6 weeks.
Where can I undergo surgery for achalasia cardia?
I conduct the initial consultation with all patients in Moscow at the Swiss University Clinic. Get acquainted in more detail with my main clinical sites in Moscow and Switzerland.
Dietary recommendations
Proper and healthy nutrition for gastric sphincter insufficiency is the basis of the entire therapeutic approach. In order to quickly recover and prevent exacerbations of the disease, you should:
- Avoid consuming foods that can cause a decrease in tone. These include: chocolate products, carbonated drinks, pepper, tea, coffee, seasoned foods.
- Avoid spicy and fatty foods.
- Completely eliminate the consumption of alcohol and tobacco products.
- Meat protein, on the contrary, helps to increase the tone of the LES and reduce symptoms.
The main condition for the complete absorption of food is its frequent consumption in small portions. A minimum 4-hour interval should be observed between main meals. At the end of the meal, refuse to take a lying position, and preferably sleep with the head end raised.
When diagnosing cardia insufficiency, it is recommended to consult a nutritionist to create the right diet. Adjusting your diet will significantly speed up the healing process.
| Measure | Description |
| Diet | The state of the gastrointestinal tract largely depends on the diet. Fasting is strictly contraindicated. The last time of the day you need to eat 3-4 hours before your expected bedtime. You should also avoid foods that negatively affect the esophagus. These include smoked and spicy dishes |
| Eliminating obesity | Avoid weight gain, respond promptly to negative changes in weight and take appropriate measures to correct the situation. Excess weight negatively affects the condition of the entire body. |
| Workout | Physical activity without overexertion is a prerequisite for maintaining a healthy state of the gastrointestinal tract. |
| Doctor visits | If clinical signs of gastrointestinal diseases occur, promptly contact a medical institution for advice and undergo diagnostic procedures |
| Bad habits | Drinking alcoholic beverages, smoking, and taking narcotic drugs negatively affects the functioning of not only the gastrointestinal tract, but also the entire body. |
| Overvoltage | Excessive physical activity should be avoided |
| Self-treatment | If clinical signs of the disease occur, you should not take medications to relieve symptoms. Independent use of antibacterial and other agents is also not recommended. There is a high risk of aggravating the course of the disease. Doctors recommend that if the first signs of cardia insufficiency occur, you should contact a medical facility. |
Causes of the disease: organic factors
There are many reasons for the occurrence of cardiac insufficiency. It is customary to divide them into two large groups:
- organic causes;
- functional reasons.
Organic factors in the occurrence of the disease are those phenomena that are not directly related to disruption of the muscle ring. Organic factors cause negative operating conditions for the gastric valve, which is the impetus for their disruption. They are:
- compression deficiency resulting from improper diet, as a result of overeating or infrequent consumption of food, but in large portions;
- complete lack of physical activity;
- formation of a diaphragmatic hernia;
- the presence of chronic diseases of the digestive system such as gastritis, pancreatitis, etc.;
- consumption of food before going to bed in large quantities;
- excess weight.
In addition, an inflammatory disease of the walls of the esophagus - esophagitis - can provoke the appearance of cardiac sphincter. Cardia failure will develop as the underlying disease progresses.
But there is an important nuance. It is worth understanding that any disease of the digestive system can provoke cardia insufficiency: atrophic gastritis, ulcers, pancreatitis, etc.
Therapeutic exercises for pathology
The muscular structures of the gastric cardia can be easily strengthened. For this purpose, specially designed breathing exercises are used. Particularly popular is Strelnikova’s gymnastic method, which involves performing training twice during the day: in the morning and in the evening before a meal, and also after an hour and a half after its end, for 1500 breaths.
As a preventive measure, gymnastics is performed in the morning or evening period. Such breathing exercises help strengthen the body and improve the health of internal organs due to increased blood flow. Regular breathing exercises for insufficiency of the gastric cardia will be no less useful:
- The training should be carried out on an empty stomach, since any activity performed on a full digestive organ weakens the sphincter, which is explained by the pressure of gastric contents on the valve.
- The lungs are perhaps the only organ that can be controlled externally. For this reason, you need to start gymnastics with normal inhalations and exhalations.
- Exercises should be performed simultaneously with thoracic and abdominal breathing, when the muscular structures of the abdominal cavity become involved in the respiratory process.
- Inhalations and exhalations must be carried out in compliance with different speed limits.
If the disease occurs in the final stages, then the listed gymnastic exercises become useless.
Etiology
In most cases, cardia failure occurs against the background of functional disorders. Less commonly, the cause is organic abnormalities.
Table 1. Causes of cardia failure
| Nature of the disorder | Description |
| Functional | Sphincter spasm leads to an increase in intra-abdominal pressure, which is fraught with increased gas formation and fermentation. |
| Organic | The disease occurs against the background of a hernia. The lower sphincter is displaced into the chest, which leads to smoothing of the esophagogastric angle and loose closure of the valve. Chronic pancreatitis can also provoke cardial insufficiency. |
This disease can also appear for more “prosaic” reasons:
- eating disorder;
- obesity;
- decreased immunity;
- eating a lot of food before bedtime;
- sedentary lifestyle;
- excessive physical activity.
Tumors of the stomach, ulcers, gastritis and abdominal surgery are also at risk.