Sometimes this is the result of inflammation in the scar area, sometimes it is a consequence of the formation of weak connective tissue that makes up the scar (a feature of the patient’s body). As a result, a defect (weak spot) appears at the site of the postoperative scar, through which a protrusion of internal organs is formed - a hernia is formed.
According to statistics, a hernia of this type occurs in every fifth of the operated patients. In half of them, a hernia occurs already in the first year after surgery. For the rest - over the next 5 years.
Causes of postoperative hernia formation
You can never name one single reason why a particular person developed a hernia. There are many factors that contribute to or influence the development of a ventral hernia. Below are the most common conditions that contribute to the formation of a hernia:
Heredity
Some hereditary diseases of connective tissue (for example, Marfan syndrome) are manifested by its weakness, including the weakness of formed scars at the site of damage (surgeries). People with such genetic abnormalities are predisposed to the formation of postoperative hernias.
Impaired regeneration (wound healing).
Inflammation of a postoperative wound can significantly affect the formation of the scar, thereby making it not strong enough, which also increases the risk of a hernia.
Intolerance of the patient's body to suture material.
In this case, an inflammatory reaction of the body to the threads occurs, which can lead to the appearance of defects in the postoperative scar.
Violation of the postoperative regimen by the patient.
Untimely and, most importantly, a sharp increase in physical activity, violation of diet and nutrition with the formation of constipation, during the formation of the scar, leads to a disruption of its structure and a decrease in strength.
Concomitant diseases
Any disease that leads to increased intra-abdominal pressure
- Bronchial asthma
- Bronchitis
- Intestinal disorders, chronic constipation
- Prostate adenoma, chronic urinary retention
- Obesity, etc.
With all these diseases, the edges of the wound experience constant tension, normal microcirculation and innervation are disrupted, which leads to a rapid disruption of the formation of a dense scar.
Technical errors during the operation
Errors in tissue joining techniques can also, over time, cause the formation of defective areas and recurrent hernias.
How do hernias form?
Hernias occur in the area of “weak spots” of the anterior abdominal wall, under the influence of intra-abdominal pressure. Factors that cause its increase are called producing factors and include: physical activity, cough, childbirth and all those cases when the abdominal press tenses.
“Weak spot” is the area of the abdominal wall where the muscular aponeurotic part is most thinned. This may be the place of muscle attachment to the aponeurosis or physiological openings (inguinal rings, umbilical ring).
An increased risk of hernias is observed in people with predisposing factors: connective tissue weakness syndrome, damage to the nerves innervating the abdominal wall, as well as the presence of postoperative scars.
Tests and diagnostics
Making a diagnosis already at the stage of physical examination does not cause difficulties: the presence in a vertical position of an asymmetrical protrusion in the area of the postoperative scar, which increases when the patient coughs/strains and disappears in the lying position, is a reliable symptom of a hernia. Less commonly, peristalsis of intestinal loops is determined through a thinned scar. More detailed information about the size/shape of the hernia, changes in the muscular aponeurotic structures, and the presence of adhesions can be obtained using instrumental examination methods: MRI, CT, ultrasound/radiography of the abdominal cavity, esophagogastroduodenoscopy, colonoscopy.
What does a hernia consist of?
All hernias, regardless of location and size, have a common structure and consist of the following components:
- A hernial orifice is a defect of the anterior abdominal wall, mainly in the aponeurosis. Through them, the internal organs leave the abdomen and end up under the skin. If the hernial orifice is wide, then through it the contents can freely return to the abdominal cavity.
- Hernial sac is a sheet of stretched peritoneum covering organs that extend beyond the abdominal cavity through the hernial orifice. The hernial sac is covered with several membranes, these also include subcutaneous tissue and skin.
- The contents of the hernial sac are the internal organs or their individual parts that extend beyond the abdominal cavity through the hernial orifice.
What types of hernias are there?
Depending on the anatomical location, external and internal hernias are distinguished. External ones include:
- Umbilical hernia.
- Inguinal hernia.
- Hernia of the white line of the abdomen.
- Postoperative hernia.
- Paracolostomy hernia.
- Lumbar hernia.
- Perineal hernia.
- Obturator hernia.
- Hernia of the xiphoid process.
- Sciatic hernia.
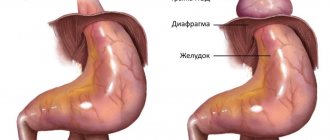
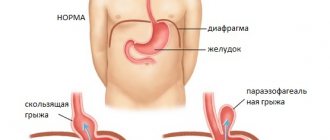
Hernias that form inside the abdominal cavity are considered separately. With such hernias, internal organs can be located in pockets of the peritoneum or penetrate into the chest cavity through the openings of the diaphragm.
Depending on the size of the hernia, they are divided into:
- Small: hernial orifice less than 4 cm
- Medium: hernial orifice from 4 to 10 cm
- Large: hernial orifice larger than 10 cm
Hernias are also classified according to the degree of development:
- initial - a small depression is identified in a weak spot of the abdominal wall - a triggering factor for the formation of a hernia;
- canal - internal organs begin to sink into the hernial opening;
- complete - the internal organs have passed through the hernial orifice and are located under the skin.
According to the clinical course, hernias are divided into:
- reducible - the contents of the hernial sac move freely from the abdominal cavity to the hernial sac and back.
- irredeemable.
- strangulated - a condition in which the hernial orifice puts pressure on the structures of the released organ, which leads to disruption of its blood supply and can lead to necrosis. There are: elastic strangulation, fecal strangulation, parietal strangulation, retrograde strangulation, Meckel's diverticulum strangulation, Broca's hernia.
What are the symptoms of a hernia?
In the initial stages, a hernia may manifest itself as discomfort or slight pain during physical activity at the site of hernia formation. As the aponeurosis thins or the tissues of the anterior abdominal wall weaken, a painless protrusion appears, disappearing when pressure is applied to it. With each new episode of increased intra-abdominal pressure, the hernial orifice will increase in size, and the sac will stretch due to an increase in the volume of contents.
External abdominal hernias that occur without complications are characterized by such general symptoms as: the presence of a hernial protrusion, discomfort in the hernia area, dysfunction of the organs that make up the hernial contents.
Prevention
In order to prevent the development of postoperative hernias, it is recommended:
- wearing the appropriate size bandage;
- restriction of physical activity after abdominal surgery for a period established by the surgeon;
- normalization of body weight;
- a balanced diet to prevent flatulence / constipation ;
- compliance with asepsis rules at all stages of the operation, adequate preoperative preparation of the patient, use of high-quality suture material, proper management of the patient after surgery.
Why is a hernia dangerous?
Any hernia is dangerous for the development of complications. The most serious complication of a hernia is strangulation. It occurs when the blood supply to the contents of the hernial sac is disrupted and tissue necrosis occurs.
An equally serious complication is intestinal obstruction. As a result of the prolonged presence of intestinal loops inside the hernial sac, they are compressed, the movement of intestinal contents through them is disrupted, and intestinal obstruction forms.
It is very important to understand that the development of complications can occur suddenly, against the background of complete well-being: on vacation, at the dacha, while traveling - in situations where qualified medical care is difficult to access or not available at all. Treatment of hernia complications requires emergency intervention, and delay can lead to a sharp deterioration in a person’s condition and significantly worsen the prognosis of delayed treatment.
Therefore, it is better to get rid of the hernia before complications develop.
Classification
Ventral hernias are characterized by a variety of locations, sizes, and shapes, which makes it difficult to create a single classification. According to the characteristic features, there are:
- By size of hernia: small, medium, extensive, giant.
- By localization: lower/upper middle and lower/upper right-sided/left-sided lateral.
- According to the presence of complications: uncomplicated hernia; strangulated hernia; perforating hernia with signs of intestinal obstruction .
According to the composition of the hernial sac: greater omentum, loops of the small intestine, bladder, stomach. By reducibility: reducible/irreducible.
Hernia treatment
It is only possible to completely get rid of a hernia through surgery. There are also conservative methods to alleviate the condition of a hernia, but their use is possible only if there are contraindications to surgery.
Contraindications to elective surgical treatment include severe concomitant diseases, malignant processes in advanced stages, acute diseases and pregnancy. It is important to note that complicated hernias must be operated on urgently for health reasons.
The smaller the size of the hernia, the easier the operation for both the surgeon and the patient. In turn, the treatment of giant hernias represents a major surgical problem and requires the use of non-standard approaches to its elimination.
Hernioplasty (hernia repair) is the name of an operation to “liquidate” a hernia with plastic surgery of a defect in the anterior abdominal wall.
Profitable arithmetic: two operations in one
Cholecystectomy
- Cost: 100,000 - 160,000 rubles.
- Duration: 25-30 minutes
- Hospitalization: 3 days in hospital
More details
We consider performing two or more operations simultaneously for combined surgical diseases as another interesting area of work. There are not so few people suffering from several diseases at once that require surgery. Traditionally, they endure one operation after another, trying to gradually get rid of their ailments. The use of gentle laparoscopic techniques allows you to solve the problem in one step. Our department has accumulated extensive experience when laparoscopic hernioplasty was performed in conjunction with removal of the gallbladder for cholelithiasis, colon resection, gynecological operations, etc. Despite the expansion of the volume, patients tolerate these interventions well, are activated early and are discharged from the hospital in almost the same time frame as after one operation. At the same time, the patient avoids repeated intervention with all the ensuing difficulties and dangers, saving time, effort and money.
What are the methods of anterior abdominal wall plastic surgery?
Plastic methods can be tension or non-tension.
Tension is a type of plastic surgery performed using the patient’s own tissues. This method received this name because, in order to eliminate a hernia defect, the tissues must be “tightened” and sewn together. The resulting tension in the tissues can cause pain after surgery and result in a possible relapse. At the present stage of development of medicine, this method of closing hernias defects is significantly inferior to non-tension methods.
Tension-free plastic surgery involves the use of modern mesh prostheses to strengthen the anterior abdominal wall. The prosthesis is a polypropylene network, which, due to its flexibility, strength and high degree of tissue “germination”, has shown its reliability and safety when used in hernia repair. Mesh prostheses come in different sizes, from small ones with a diameter of 5 cm for umbilical hernias, to large ones of 50 x 50 cm for giant incisional hernias. Modern three-dimensional mesh systems make it possible not only to strengthen the hernia defect in the form of a “patch”, but to completely fill it, significantly reducing the risk of relapse. In some situations, a special mesh is installed, the surface of which is coated with a special composition that allows it to safely contact the abdominal organs and avoid the formation of adhesions between them.
The open hernia repair operation consists of several stages:
- Isolation of the hernial sac. A skin incision is made above the hernial protrusion, the hernial sac is freed from the surrounding subcutaneous fatty tissue. The “hernial orifice” is distinguished.
- The hernial sac is opened, the condition of the contents of the hernial sac is assessed, and if there are no complications, the contents are immersed in the abdominal cavity.
- The hernial sac is excised, stitched and plunged into the abdominal cavity.
- The integrity of the anterior abdominal wall is restored (plasty is performed).
Diet
There is no special diet for postoperative hernias, but the diet should be adjusted towards limiting the amount of food taken at the same time (that is, 5-6 meals in small portions are indicated). constipation are excluded from the diet - saturated meat broths, cabbage, spicy, fatty and spicy foods, legumes, rice, brown bread, milk/dairy products, fresh baked goods, flour products, astringent fruits/berries, carbonated drinks .
The diet should be based on dietary meats, lean fish, chicken eggs, cottage cheese, cereals, baked vegetables, fruits, rosehip decoction, dried fruit compote, weak tea.
Is it possible to operate a hernia without incisions using modern mesh prostheses?
Yes, you can!
At the moment, laparoscopic hernioplasty is the operation of choice for the treatment of various types of hernias. This operation is performed through punctures in the anterior abdominal wall. The surgeon inserts a video camera into the abdominal cavity and, using additionally inserted manipulators, releases the hernial sac from its contents. In the second stage, the surgeon separates the peritoneum of the hernial sac from the tissues of the anterior abdominal wall, dissects it and places a special mesh prosthesis on the hernial orifice. Then, the mesh is reinforced on top with the previously separated peritoneum.
Thanks to this, the prosthesis does not form adhesions with internal organs. This method of plastic surgery avoids tissue tension and greatly reduces the likelihood of relapse. The absence of large incisions on the anterior abdominal wall contributes to a comfortable course of the postoperative period.
Belly patch or new techniques
In recent years, techniques have begun to be used to avoid tissue tension. During the operation, special meshes are inserted through the incision in the projection of the hernial ring to hold the exit of the hernial sac through the aponeurosis defect. The meaning of the action is clear: if a child wipes his pants, then the housewife does not sew up the hole, but sews in a patch. The comparison may be curious for such a serious topic, but it conveys the main idea embedded in the methodology. It should be noted that all “open” operations involve, first of all, an incision, the associated pain syndrome, the danger of inflammation of the suture and, finally, rough scars on the skin. Therefore, in hernia surgery, the search for new operations that would combine not only reliability, but also low trauma does not stop.
How does the postoperative period proceed?
After laparoscopic hernia repair, pain is practically not felt and is therefore easily controlled using tablet painkillers.
The only reminder of the operation was discomfort in the area of small punctures on the anterior abdominal wall.
In uncomplicated cases, discharge from the hospital occurs within 2-3 days. The time frame for returning to work, on average, does not exceed 10-14 days.
Traditional open surgery is characterized by pain in the postoperative period. However, carrying out comprehensive pain relief in a hospital allows you to reduce its severity and feel comfortable throughout the entire recovery period.
After discharge from the hospital, you will be advised to limit physical activity for a period determined by your attending physician based on the complexity of the treatment performed.
Causes
The main reasons for the development of postoperative hernias include:
- Hereditary diseases of connective tissue (Marfan syndrome), manifested by its weakness, including the failure of formed postoperative scars.
- Concomitant diseases leading to increased intra-abdominal pressure (chronic constipation , bronchial asthma , obesity , chronic urinary retention, prostate adenoma , etc.) causing constant tension of the edges of the wound/impaired microcirculation and innervation in this area, which disrupts the formation of a dense scar.
- Inadequate physical activity after surgery, violation of the wearing regime/failure to wear a bandage, which violates the requirements for protecting the scar/supporting the muscular frame in the postoperative period.
- Inflammation of a postoperative wound, accompanied by scar suppuration.
- Violation of nutrition/diet during the formation of the scar, leading to the formation of constipation , which causes a violation of its structure/reduction in strength.
- Errors in the technique of connecting tissues/technical errors of the surgeon during the operation (errors in choosing the method of suturing the wound, excessive tissue tension, poor-quality suture material, suture dehiscence, etc.).
- Factors contributing to the development of ventral hernias include: weakening of the body, vomiting/constipation in the postoperative period, diabetes mellitus , pregnancy /childbirth, systemic diseases that cause disruption of the connective tissue structure.
Who deals with surgical treatment of external abdominal hernias?
You can always contact the clinic of coloproctology and minimally invasive surgery for surgical treatment.
Qualified specialists regularly perform laparoscopic interventions for hernias of the anterior abdominal wall. In some cases, we also use traditional open surgery.
At KKMH, treatment of hernias is carried out both on a paid basis and under the compulsory medical insurance policy.
Sign up for a consultation by phone +7 (499) 11-03-222.