Treatment of hiatal hernia under the guidance of Doctor of Medical Sciences, Professor Mikhail Andreevich Agapov, at the University Clinic of the Moscow State University named after M.V. Lomonosov
Author:
- Agapov Mikhail Andreevich Head of the surgical department, surgeon, oncologist, coloproctologist
4.5 (Votes: 5)
What is a hiatal hernia?
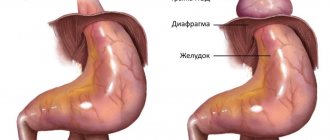
Hiatal hernia
is a pathology in which the internal organs, which are physiologically located under the diaphragm, are displaced into the chest cavity.
Modern medicine notes a trend toward an increase in the number of gastroenterological pathologies. Along with gastritis and peptic ulcers, a hiatal hernia (HH) is often diagnosed, treatment of which is necessary to prevent life-threatening complications. The appearance of the hiatal hernia is considered as an exclusively surgical disease, since there is a change in the diaphragmatic ligaments, muscle stretching and expansion of the lumen of the diaphragm, which are most optimally eliminated surgically.
A hiatal hernia is when part of the stomach or part of the intestine gets into an overly enlarged hole in the diaphragm. The disease is common and causes patients a lot of pain and difficulty eating. Acquired hiatal hernias (HHH) appear more often in women, the risk of their occurrence increases significantly after 50 years (from 0.7% at an earlier age to 4.7% after reaching 50-60 years). Irregular symptoms of a hiatal hernia can be eliminated with medications and a certain diet. If a hernia in the esophagus begins to constantly make itself felt with heartburn, pain, reflux (reflux of food from the stomach), then the most effective treatment in such a situation is surgery. Proper surgical treatment will relieve the patient of the signs of a hiatal hernia without the need for additional medications.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a gastroenterologist (primary) | 4 200 |
| Fluoroscopy and radiography of the esophagus | 2 600 |
| Gastroscopy (videoesophagogastroduodenoscopy) | 6 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
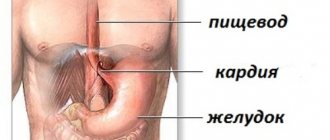
Causes of development of hiatal hernia disease
The esophagus has the shape of an elastic tube and consists of several layers (mucous, muscular and serous membranes). It is located mostly in the chest cavity. Passing between the lungs, large blood vessels and the heart, the esophagus enters the abdominal cavity through the esophageal hiatus in the diaphragm. The chest and abdominal cavities are separated from each other by a muscular horizontal septum (diaphragm), through which the esophagus passes. The normal dimensions of the opening in the diaphragm correspond exactly to the diameter of the passing esophagus, no more and no less. When the diameter of the hole changes, problems begin, one of which is called a hernia in the esophagus.
This phenomenon is quite common, but at small sizes it does not cause any particular problems and can only be noticed during a targeted examination. Medium and large hernias lead to the reflux of aggressive gastric juice into the esophagus and the appearance of clinical symptoms.
The most common causes of acquired hiatal hernia:
- Consequences of injuries to the thoracic and abdominal organs;
- Constant increase in intra-abdominal pressure, due to ascites (fluid in the abdominal cavity); with multiple or repeat pregnancies, chronic constipation, intense physical activity, due to frequent persistent cough (for example, with COPD - chronic obstructive pulmonary disease);
- Age-related decrease in tone (weakening) of the esophageal ligaments (the condition is more common in patients over 50 years old);
- Significant, sharp weight loss, disappearance of adipose tissue under the diaphragm;
- Previous operations on the esophagus;
- Obesity;
- Poor physical shape and tone of the diaphragmatic ligaments;
- Disturbances in the passage of food through the esophagus (esophageal motility disorders);
- Chronic diseases of the stomach, gall bladder, small intestine, leading to disruption of their motility (a situation where the normal contraction of organs and the process of passing food through them is disrupted) - often peptic ulcer of the stomach and duodenum, cholecystitis, pancreatitis.
Congenital hiatal hernia occurs in children with too short an esophagus, when the stomach (or part of it) is located abnormally high (in the chest cavity) due to insufficient length of the esophageal tube.
Recovery after surgery
After the operation is completed, the patient is transferred to the inpatient department, where doctors monitor his condition. If the patient feels well, he or she may be discharged the next morning. The rehabilitation period after removal of a gastric hernia is 3-4 weeks. The patient’s main task at this time is to follow the doctor’s recommendations for a quick recovery and return to their normal lifestyle. In order for the body to quickly recover after surgery, you need to follow the following rules:
- Stick to bed rest.
- Do not lift heavy objects, put off physical activity for a while.
- Go on a diet - your diet should include low-fat, fresh food in pureed or liquid form.
- Take medications - analgesics, proton pump blockers.
If symptoms such as bleeding, pain, or suppuration of wounds appear, you should immediately consult a doctor. After laparoscopic repair with fundoplication, recurrence of the disease is unlikely.
Esophageal hernia: symptoms and causes of their appearance
There are asymptomatic hiatal hernias, which can only be identified through instrumental studies. They are usually discovered by chance. But more often the disease makes itself felt by one or more signs with varying degrees of severity.
- Heartburn
The main reason for its occurrence is compression of the stomach or intestines in the diaphragmatic opening. Intragastric pressure increases, and food is thrown back into the esophagus. The condition is called gastroesophageal reflux disease (GERD). Food from the stomach contains a lot of gastric juice (acid), which irritates the mucous membrane of the esophagus and causes a burning sensation (heartburn).
- Belching
Belching air or acidic contents from the stomach (regurgitation). Hiatal Hernia (HH): The symptom of belching occurs for the same reasons as heartburn. The symptom is quite common, noted in 70% of cases.
- Pain
The nature and intensity of pain can be different: from aching, limited pain behind the sternum, to sharp, burning, stabbing pain of a girdling, diffuse nature. Pain occurs due to irritation of the esophageal mucosa by acidic food entering there from the stomach. Pain can also appear due to compression of the vagus nerves in the esophageal opening of the diaphragm. The anterior branches of which pass from the chest to the abdominal cavity along with the esophagus. Often, painful signs of a hiatal hernia are mistaken for heart pain (for example, confused with angina or even myocardial infarction). Pain accompanies half of patients with hiatal hernia; in time it is associated with eating, the patient remaining in a horizontal position or bending forward.
- Swallowing difficulty (dysphagia)
Patients are concerned about difficulty after swallowing food, a feeling of “lump” appears behind the sternum after eating (especially after eating too hot, cold or too much). Sometimes there is a paradoxical situation when solid food in a patient with hiatal hernia (hiatal hernia) passes more easily than liquid food. However, as the disease worsens, dysphagia appears even when eating food of any consistency and temperature.
- Tongue pain (glossalgia)
- Hoarseness of voice
The last 2 symptoms appear due to peptic burn (stomach acid burn) of the oral mucosa, tongue and larynx.
- Hiccups
- Heart rhythm disturbances
- Dry cough
- Attacks of suffocation similar to those of bronchial asthma
The group of the 4 symptoms listed above occurs due to the “fault” of the vagus nerve, which is compressed together with the esophagus in the opening of the diaphragm.
Combined pathologies and complications
Often, a hiatal hernia is combined with diseases of the biliary tract, peptic ulcer, intestinal diverticulosis, and is an anatomical substrate of gastroesophageal reflux disease.
Complications of hiatal hernia may include:
- inflammation of the lower esophagus (esophagitis),
- erosions and ulcers in this part of the esophagus,
- rarely bleeding,
- strangulated hernia.
Types of hernias UNDER
- Sliding. Another name – floating hiatal hernia – reflects the essence of the disease. The stomach, intestines or omentum enter the chest cavity periodically (freely passing back and forth). Manifestations of the disease may at times be absent and appear spontaneously when food refluxes from the stomach into the esophagus. Typically, heartburn, belching, and pain are a concern. How to relieve pain from a hiatal hernia (sliding)? Taking antacids (acid-reducing agents – Maalox, Smecta, Rennie, Almagel, etc.) helps;
- Paraesophageal (paraesophageal). Constantly located on the side of the esophagus in the chest cavity is the upper part of the stomach. The food that gets there stagnates, causing patients an extremely unpleasant, bursting sensation in the chest after eating. Therefore, they first try to eat less, and then they may even refuse to eat (for fear of pain). This behavior leads to exhaustion of the patient;
- Complicated hernias. The most dangerous thing is a strangulated hernia. The hernial sac becomes motionless in the hole, its contents cannot be evacuated. Signs of intoxication appear (high temperature, pallor, weakness, increased pulse and heart rate), vomiting of undigested food, bile and even blood. There is a high probability of rupture of the hernial sac, which can lead to mediastinitis or peritonitis, and then sepsis. Less serious complications are anemia, bleeding from the esophagus, gastritis and stomach ulcers (where it enters the hernial sac), prolapse of the stomach into the esophagus (prolapse).
It is precisely because of the risk of complications that patients need a thorough examination and decision on the issue of surgical treatment of hernia.
Authorized Products
Patients with a hernia and after surgery spend a long time on Diet No. 1 , which includes:
- Premium quality dried wheat bread.
- Soups with vegetable broth (cereals and vegetables are pureed), seasoned with butter or egg flakes.
- Steamed dishes made from beef, lamb, lean pork, turkey and chicken.
- Steam dishes from lean fish without skin (pieces or cutlets).
- Milk, cream, non-acidic kefir, cottage cheese in the form of soufflé, pudding, fermented milk products with high acidity are excluded.
- Semolina, buckwheat and rice, cooked in water or milk. The porridge is pureed and its consistency should be semi-viscous.
- Vegetables (potatoes, cauliflower, pumpkin, carrots, beets) are steamed and served as purees or puddings.
- Fruit puree, jelly, jelly, compotes, sugar, honey.
- Tea with milk, sweet juices.
- Butter and sunflower oil (refined) - in dishes.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| potato | 2,0 | 0,4 | 18,1 | 80 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| beet | 1,5 | 0,1 | 8,8 | 40 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| cereals | 11,9 | 7,2 | 69,3 | 366 |
| white rice | 6,7 | 0,7 | 78,9 | 344 |
Bakery products | ||||
| wheat bread | 8,1 | 1,0 | 48,8 | 242 |
Confectionery | ||||
| jelly | 2,7 | 0,0 | 17,9 | 79 |
Raw materials and seasonings | ||||
| honey | 0,8 | 0,0 | 81,5 | 329 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
| milk sauce | 2,0 | 7,1 | 5,2 | 84 |
| sour cream sauce | 1,9 | 5,7 | 5,2 | 78 |
Dairy | ||||
| milk | 3,2 | 3,6 | 4,8 | 64 |
| cream | 2,8 | 20,0 | 3,7 | 205 |
Cheeses and cottage cheese | ||||
| cottage cheese | 17,2 | 5,0 | 1,8 | 121 |
Meat products | ||||
| boiled beef | 25,8 | 16,8 | 0,0 | 254 |
| boiled veal | 30,7 | 0,9 | 0,0 | 131 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken | 25,2 | 7,4 | 0,0 | 170 |
| turkey | 19,2 | 0,7 | 0,0 | 84 |
Eggs | ||||
| chicken eggs | 12,7 | 10,9 | 0,7 | 157 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
Juices and compotes | ||||
| juice | 0,3 | 0,1 | 9,2 | 40 |
| jelly | 0,2 | 0,0 | 16,7 | 68 |
| rose hip juice | 0,1 | 0,0 | 17,6 | 70 |
| * data is per 100 g of product | ||||
Treatment of hiatal hernia
There is a common belief that patients diagnosed with hiatal hernia mainly suffer from gastroesophageal reflux, and this is indeed the case. Gastroesophageal reflux disease (GERD) is a disease accompanied by the reflux of acidic, aggressive stomach contents into the esophagus. Today, GERD is recognized as a disease of the 21st century, which is confirmed by its high prevalence along with other diseases of the gastrointestinal tract. The main symptom of this disease is heartburn, which is detected in our country and other countries in 40% of the population. The causes of this disease may coincide with the causes of hiatal hernia. The danger of these diseases lies not only in discomfort and pain, but also in constant inflammation of the mucous membrane of the esophagus, which can ultimately lead to erosive esophagitis, Barrett's esophagus, and esophageal cancer.
The conservative treatment method is used after consultation with a gastroenterologist and surgeon and after all necessary examinations. In addition to examination and questioning, this is an FGDS (fibrogastroduodenoscopy, examination of the esophagus and stomach from the inside with a special instrument). X-ray examination (survey images and images after taking a barium suspension). pH-metry of the esophagus and stomach (study of the acidity level of their contents). Esophagogododenometry (measurement of pressure inside the esophagus and stomach).
Esophageal hernia, how to cure it with medications. Treatment without surgery can be carried out for small hernias, uncomplicated and not accompanied by pronounced symptoms. The goal of treatment is to reduce the intensity of symptoms and avoid the risk of disease progression. It is impossible to eliminate a defect in the diaphragm using therapeutic methods. Treatment begins with lifestyle and nutrition correction. It is necessary to eliminate the factors leading to increased intra-abdominal pressure: lose weight, treat chronic diseases, quit smoking and other bad habits, strictly follow a diet. It is mandatory to prescribe pharmaceuticals that reduce the acidity of the stomach (antacids) and agents that protect the mucous membrane of the esophagus and stomach from the aggressive effects of acidic contents (gastroprotectors),
Recommendations for hiatus hernia
- eat small meals several times a day;
- eat food 2-3 hours before bedtime;
- eat food of gentle temperature and consistency (chopped, pureed);
- if you have symptoms, avoid eating chocolate, onions, citrus fruits, tomatoes, spicy foods and other foods that cause heartburn;
- eliminate alcohol consumption;
- stop smoking!;
- normalize weight;
- sleep with the head of the bed raised 15 cm.
For patients with a hiatal hernia, there are a lot of taboos: you can’t eat fried, salty, smoked, carbonated drinks, spicy food, fast food, alcohol, smoked meats or sweets. In general, everything that stimulates increased production of digestive enzymes and can cause heartburn.
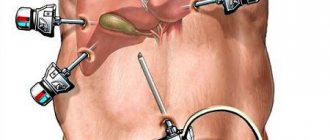
Surgical treatment of hiatal hernia
Surgery for a hiatal hernia is the main radical way to restore the correct anatomical relationship and location of organs and relieve the patient from the unpleasant symptoms of the disease.
Preoperative examination for hiatal hernia includes:
- conducting a general blood test;
- X-ray of the esophagus using barium fluid to ensure a clear silhouette of the esophagus and stomach;
- esophagogastroduodenoscopy, during which the upper part of the gastrointestinal tract is examined using an endoscope;
- esophagomanometry to measure pressure inside the esophagus and stomach.
In each specific case, taking into account concomitant diseases, the attending physician may prescribe additional tests and studies.
Now, in most cases, laparoscopic methods for correcting the esophageal opening of the diaphragm and the esophagogastric junction are the best choice.
Laparoscopic treatment of hiatal hernia has a number of advantages:
- Preservation of the natural anatomy of the thoracic cavity and upper abdominal cavity;
- Less traumatic;
- Fast patient recovery after surgery;
- No cosmetic defects after the intervention (no scars).
During the operation, surgeons see an image from the magnifying optics of the laparoscope on an external monitor. Magnification makes it possible to distinguish fine branches of nerves, fascial spaces and vessels. Mini-instruments inserted through small punctures carry out surgical treatment according to the chosen technique. It could be:
- Modification of the classic Nissen operation (fundoplication). When the lower part of the esophagus is strengthened with a kind of coupling (a cuff several centimeters wide, taken from the tissues of the fundus of the stomach and wrapped around the esophagus 360 degrees. After the operation, the frequency of reflux of food from the stomach is reduced, its motility is normalized, and the tone of the esophagus is strengthened.
- Toupet method. The difference between the method is the amount of coverage of the esophagus with a reinforcing cuff - 270 degrees instead of 360 according to the classical method. The advantages of this method: preservation of the natural mechanisms of belching and the ability to realize the gag reflex.
During the operation, the lower part of the esophagus and the fundus of the stomach are isolated from the adhesions, brought down into the abdominal cavity and fixed in an anatomically based position.
Then crurorrhaphy (reduction of the diaphragmatic opening) and fundoplication (strengthening the lower part of the esophagus with a cuff from stomach tissue) are performed. Sometimes the patient may undergo the Esophyx method of surgery. When there are no punctures, a flexible endoscope and the necessary instruments are inserted through the oral cavity into the esophagus. And they change the angle of the stomach to the esophagus to the correct value. Then the cuff strengthens the transition between the organs.
New laparoscopic surgical techniques have reduced the relapse rate to 3.5% over a five-year period. That is, almost 97 patients out of 100 after 5 years retain the positive effect of treatment, without additional use of medications.
There are different options for fundoplications. The type of operation is determined individually.
Antireflux surgical methods are aimed at eliminating the hernial orifice, forming a physiological mechanism that prevents stomach contents from entering the esophagus, and preventing displacement of the stomach and esophagus. Fundopletion is such an effective, recognized method. This operation has been performed since 1955 and is based on wrapping the fundus of the stomach around the esophagus 360 degrees. This creates a cuff that prevents gastric juice from refluxing into the esophagus. This operation has different execution options. Considering the presence of a large number of anatomical and physiological features in each patient, the cost of the operation is determined individually.
Laparoscopic surgery for hiatal hernia, laparoscopic surgery for cholecystitis (scientific Simultaneous surgery - laparoscopic fundoplication and laparoscopic cholecystectomy).
How to treat
Hernia treatment is carried out both conservatively and surgically. It is necessary to seek advice from both a gastroenterologist and a surgeon. Therapy is often complex. Here it is worth understanding that after detecting a formation, it is necessary to begin therapy as quickly as possible in order to reduce the risk of complications. If we are talking about non-surgical treatment, then the following measures are used. Firstly, it's diet. It is recommended to eat split meals, every 3 hours, but the portions should be small - about 200-300 g. Naturally, it is necessary to exclude potentially dangerous and always classified as dangerous foods - fried, fatty, pickled, smoked and other foods. After all, they irritate the mucous membranes and further increase the production of gastric juice. The optimal solution would be to shift the diet towards the consumption of boiled and steamed dishes, fresh fruits, lean meat, etc. Depending on the severity of the situation, they may be advised to eat pureed food or dishes with a liquid consistency.
In this situation, the normalization of the regime and lifestyle is also of no small importance. Naturally, and this is not even subject to discussion, you need to give up bad habits, get proper rest and engage in physical activity in moderation. Abdominal exercises - various loads and bending - are contraindicated in this situation.
If we talk about drug therapy, antacids may be offered to reduce acidity, drugs that suppress the production of hydrochloric acid, drugs for belching and heartburn, drugs to relieve pain, drugs to restore the protective properties of the mucous membrane of the digestive system.
If there are serious complications, such as bleeding, doctors prescribe additional therapy. These may be means to restore iron balance, etc. The issue of surgical intervention may also be considered.
Therapy must be carried out in consultation with a doctor and exclusively according to his recommendations - this is the only way to guarantee a high-quality result.
Fully or partially limited products
- Fatty and stringy meat, fatty duck and goose, meat and fish broths, canned food, smoked meats, pickled vegetables.
- Fried dishes, mushroom decoctions, tomato and mushroom sauces, fish and meat stewed in their own juices.
- Fresh bread and pastry.
- Tomatoes, radishes, white cabbage, sorrel, cucumbers, onions, mushrooms, sour fruits and berries.
- Spices and seasonings.
- Millet, barley and pearl barley cereals, pasta, legumes.
- Fermented milk products with high acidity.
- Carbonated drinks, sour juices.
The list of products may expand due to individual poor tolerance. Foods that cause heartburn , epigastric discomfort, and vomiting should be avoided.
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| vegetables legumes | 9,1 | 1,6 | 27,0 | 168 |
| canned vegetables | 1,5 | 0,2 | 5,5 | 30 |
| radish | 1,2 | 0,1 | 3,4 | 19 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| black radish | 1,9 | 0,2 | 6,7 | 35 |
| turnip | 1,5 | 0,1 | 6,2 | 30 |
| asparagus | 1,9 | 0,1 | 3,1 | 20 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
Berries | ||||
| grape | 0,6 | 0,2 | 16,8 | 65 |
| gooseberry | 0,7 | 0,2 | 12,0 | 43 |
| currant | 1,0 | 0,4 | 7,5 | 43 |
Cereals and porridges | ||||
| corn grits | 8,3 | 1,2 | 75,0 | 337 |
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
| barley grits | 10,4 | 1,3 | 66,3 | 324 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
Bakery products | ||||
| vysivkovy bread | 9,0 | 2,2 | 36,0 | 217 |
| oatmeal bread | 10,1 | 5,4 | 49,0 | 289 |
| bran bread | 7,5 | 1,3 | 45,2 | 227 |
| whole grain bread | 10,1 | 2,3 | 57,1 | 295 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| candies | 4,3 | 19,8 | 67,5 | 453 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Raw materials and seasonings | ||||
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| ketchup | 1,8 | 1,0 | 22,2 | 93 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
| ground black pepper | 10,4 | 3,3 | 38,7 | 251 |
| chilli | 2,0 | 0,2 | 9,5 | 40 |
| tomato sauce | 1,7 | 7,8 | 4,5 | 80 |
| spicy tomato sauce | 2,5 | 0,0 | 21,8 | 98 |
Dairy | ||||
| kefir | 3,4 | 2,0 | 4,7 | 51 |
| sour cream | 2,8 | 20,0 | 3,2 | 206 |
| curdled milk | 2,9 | 2,5 | 4,1 | 53 |
Sausages | ||||
| dry-cured sausage | 24,1 | 38,3 | 1,0 | 455 |
Bird | ||||
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| dried fish | 17,5 | 4,6 | 0,0 | 139 |
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
Oils and fats | ||||
| creamy margarine | 0,5 | 82,0 | 0,0 | 745 |
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Non-alcoholic drinks | ||||
| green tea | 0,0 | 0,0 | 0,0 | — |
| black tea | 20,0 | 5,1 | 6,9 | 152 |
| * data is per 100 g of product | ||||
Menu (Power Mode)
Patients tolerate milk well, which coats the mucous membrane and eliminates discomfort and heartburn, so drinking milk for second breakfast and at night is recommended. The same applies to milk jelly, which can be recommended for breakfast and afternoon snack. Milk porridges, which are usually consumed for breakfast and dinner, are also useful. Breakfast and dinner are complemented with omelettes or low-sour cottage cheese.
Meat or fish dishes are served for lunch with side dishes of cereals or vegetables. You can add separately cooked and twisted meat, meatballs or an egg mixture to a variety of soups (vegetable and cereal). If desired, milk cereal soups can be served as a first course for lunch.
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Postoperative period
In cases of uncomplicated course of the disease and successful laparoscopic surgery, postoperative management of patients does not go beyond standard measures (pain relief according to indications, antibiotic prophylaxis during surgery and on the 1st day after it, nutrition with liquid food from the 1st day, removal of safety drainage through 12-24 hours). The duration of hospitalization is on average from 2 to 5 days.
If complications develop, appropriate therapy is provided. To evaluate the results of treatment, it is recommended after 3-6 months. perform gastric X-ray, endoscopy and pH monitoring.
Gymnastics
For hiatal hernia, physical therapy is recommended. The following exercises help a lot:
- Lie on your side and rest your head on the cushion. Inhale deeply and inflate your stomach as much as possible, then exhale slowly and relax. Repeat 4-5 times.
- Get on your knees, straighten your back, inhale and slowly bend to the right, exhale and return to the starting position, repeat the exercise 6-7 times.
- Lie on your back. Breathing is even and calm. Slowly turn to your left and then to your right side, trying not to lose your breath.
Diagnostic methods
Diagnosis is based on the clinical picture described above and instrumental examination methods. Instrumental examination methods used to diagnose hiatal hernia and endothelial hernia include:
- fibrogastroscopy - during which the condition of the mucous membrane of the esophagus, stomach and duodenum is assessed, and prolapse of the gastric mucosa into the esophagus is detected,
- X-ray examination of the esophagus and stomach, during which the hiatal hernia itself is revealed, its size, fixation, and the motility of the esophagus and stomach and the presence of reflux of barium suspension into the esophagus are assessed,
- The third study, which helps the surgeon in determining the indications for surgery and choosing the method of surgical correction, is daily pH-metry of the esophagus and stomach, during which the level of gastric secretion and the presence of pathological refluxes from the stomach into the esophagus are determined. The most important criterion for the presence and severity of reflux esophagitis is the total time at which the pH is less than 4 units. Increased number of refluxes lasting more than 5 minutes. and an increase in the duration of the most prolonged reflux indicates a decrease in esophageal clearance and suggests the presence of hypomotor dyskinesia of the esophagus.
To identify the hiatal hernia and determine the extent of damage to the esophagus, as well as select the correct surgical treatment tactics, you must send me a complete description of gastroscopy, x-ray of the esophagus and stomach with barium for the hiatus, preferably an ultrasound of the abdominal organs, indicating your age and main complaints. In rare cases, if there is a discrepancy between complaints, X-ray data and FGS, it is necessary to perform daily pH measurements and manometry of the esophagus. Then I will be able to give a more accurate answer to your situation.