Causes of pityriasis rosea
Currently, the exact cause of the pathology is not clear. Many representatives of the medical community believe that the development of pityriasis rosea occurs under the influence of the herpes virus, but this opinion has not yet been confirmed. It is believed that the disease can be triggered by taking certain medications.
Risk factors also include:
- Decreased immunity due to acute respiratory viral infections, sore throat, colds;
- Presence of chronic diseases;
- Stressful situations;
- Disruptions in the metabolic process;
- Illiterate skin care;
- Allergic manifestations;
- Hypovitaminosis;
- Injuries and damage to the skin, including insect bites.
Pityriasis rosea develops due to hypothermia or as a consequence of vaccination. Sometimes the cause is pathologies of the digestive system.
Make an appointment with a dermatologist by phone or by filling out the online form
| Select a clinic | Skin rash | Dermatologist at the clinic | Dermatologist at home |
Symptoms of pityriasis rosea
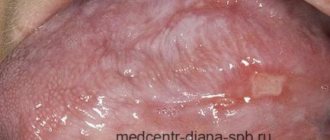
The beginning of pityriasis rosea is the formation of a maternal plaque - a single spot of a fairly large size and a round shape. Its diameter is from 2 cm, the color is pinkish, but gradually the central part of the spot turns yellow. Over time, peeling begins here.
After 7-10 days, multiple oval-shaped spots form on the surface of the skin. They are smaller than the maternal plaque - about 0.5-1 cm in diameter. For the most part, the rash spreads along the back and shoulders, covers the sides of the body, and runs along the lines of skin tension. In the center of all spots, the skin peels off, and a red border appears along the edges of the rash.
The spots that appear do not merge with each other. The pathology may be accompanied by itching. Sometimes the disease manifests itself in an atypical form - without the appearance of a maternal plaque. Pityriasis rosea lasts for several weeks, after which the rash goes away on its own. However, there is also a longer course – up to six months. Pityriasis rosea may be accompanied by weakness and malaise, drowsiness and fever.
Useful information on the topic:
- Calling a dermatologist to your home
- Fungal infections
- Rash on the body
- Sexually transmitted diseases
- How to get tested
- Wart removal
- Removal of condylomas
- Tests for STIs
- Removal of papillomas
- Skin rash
- Pyoderma
- Skin structure
- Mushroom tests
- Diagnosis of sexually transmitted infections
How does the disease manifest itself?
For no apparent reason, a single bright pink spot or plaque appears on the skin. This plaque is called “maternal.” It quickly increases in diameter, reaching 1.5-3 cm. Then, within a few days, similar but smaller rashes appear. They can quickly spread over the skin of the torso, upper and lower extremities, and groin area. Sometimes they appear on the neck. It must be said that pityriasis rosea occurs in those areas of the skin where sunlight reaches the least. Therefore, it never appears on the hands and feet. All elements of the rash are located along the skin lines, on their surface the skin slightly peels off in the form of a “collar”.
Most patients are only bothered by rashes. Some patients experience itching. The disease progresses over several weeks. Tight clothing, water procedures and sweating contribute to the appearance of new plaques. After 2-4 months, spontaneous recovery occurs.
To make a correct diagnosis, you need to consult a dermatologist. Examination of the skin is usually sufficient. In rare cases, skin flakes may need to be scraped for fungal microscopy.
Pityriasis rosea in children
In childhood, pityriasis rosea manifests itself mainly after acute respiratory viral infection. The scales on the rash are usually sparse or absent altogether. The spots most often form in the inguinal folds and armpits. With this disease, the child can continue to live a normal life, the only limitation concerns water procedures. Do not use washcloths or rub the skin with hard towels. During the period of exacerbation of the disease, excessive sweating should be prevented, so physical activity will have to be limited.
It is important to follow all doctor's recommendations. As a rule, drug treatment is not required, but special attention should be paid to restoring the body's immune defenses. In this regard, a balanced diet, room ventilation, and adherence to general hygiene rules play an important role. If there is itching or an atypical course of the pathology, the doctor prescribes medications. But it is not recommended to use folk remedies.
Pityriasis rosea in pregnant women
In pregnant women, pityriasis rosea can develop due to hormonal changes in the body (deficiency of female sex hormones) or a weakening of the immune system due to toxicosis. The disease does not affect the condition of the fetus and does not cause pathologies. However, it is necessary to identify the causes of the disease and eliminate them, since the health of the mother depends on the health of her baby.
The main treatment in such circumstances will be restorative methods. Doctors categorically prohibit the ingestion of decoctions of medicinal herbs, especially St. John's wort, sage, and oregano. Interferons are used to strengthen the immune system, but they should be taken with caution so that your own protective functions do not decrease even further. Multivitamin complexes are often prescribed.
When the disease develops, pregnant women should pay attention to their diet and do special gymnastic exercises. For those who are concerned about itching, doctors recommend treating the rash with vegetable oil, chamomile infusion, and calendula decoction. It is very important to avoid stress, which has an extremely negative effect on the body, including causing pityriasis rosea.
Pityriasis versicolor
Pityriasis versicolor (syn.: versicolor, pityriasis versicolor, pityriasis furfuracea) is a fungal skin disease characterized by damage to the stratum corneum of the epidermis. The causative agent of this disease is the fungus Pityrosporum orbiculare or P. ovale. However, the question of whether both of these forms represent one organism at different stages of its development or are separate species has not been fully resolved. It is currently accepted that both micromorphological varieties P. orbiculare and P. ovale represent different stages in the life cycle of the fungus. Moreover, its oval shape - P. ovale - is more often found on the skin of the scalp, and its round shape - P. orbiculare - on the skin of the body [25]. The correct taxonomic identification of the lipophilic yeasts causing this disease is still a matter of debate. Some scientists prefer the name Pityrosporum orbiculare, while others prefer Malassezia furfur. Thanks to molecular technologies, 10 species of the genus Malassezia have now been identified. Ogunbiyi AO and George AO (2005) identified the most common Malassezia species: M. furfur, M. symboidalis, M. obtusa, M. globosa, M. restricta, M. slooffie and M. pachydermatis [12, 15, 17].
As a result of their analysis, it was established that the cause of pityriasis versicolor in humans is most often M. globosa. Hort W. et al. (2006), having examined 112 patients diagnosed with seborrheic dermatitis, atopic dermatitis, lichen versicolor and AIDS, found that these patients had various types of Malassezia fungi. According to the authors, M. globosa was the most pathogenic species and was more often recorded in HIV-positive patients and patients with lichen versicolor. In the group of patients with seborrheic dermatitis, along with M. globosa, M. sympodialis was isolated.
The issue of the contagiousness of the fungus has been discussed in the scientific literature for quite a long time. Previously, it was believed that transmission of infection occurs either through direct contact with a sick person or through contaminated underwear. This observation was based on the high prevalence of this disease among individuals in the same family. However, it has now been proven that lichen versicolor is not contagious, and a genetic predisposition to the development of keratomycosis has been established: known cases of familial disease are explained by similar skin type in family members who are consanguineous [6, 25, 28].
The causative agent of lichen versicolor is isolated from 10–15% of the population, and 2 times more often in men. The disease mainly develops between the ages of 15 and 40 years. This mycosis is characterized by deterioration in the summer, cases of spontaneous recovery are possible. In some patients, the disease becomes chronic and prone to relapse. However, in most cases, P. orbiculare (ovale) exhibits its pathogenic properties only in adolescence [1, 2, 6, 9]. P. orbiculare (ovale) is a lipophilic fungus, so the intensity of skin colonization is related to the function of the sebaceous glands. In particular, in children under 5 years of age the fungus is not detected at all, while in 15-year-olds it is detected in 93% of cases. Further, with age, the percentage of detection of P. orbiculare decreases, which once again confirms the assumption of a relationship between the presence of the fungus and the functional activity of the sebaceous glands [6, 26]. The primary location of keratomycosis is the mouth of the pilosebaceous follicles; here the fungus multiplies, forming colonies in the form of yellowish-brown dots. Fungi concentrate around the sebaceous glands, using their secretions as a source of fatty acids necessary for their growth and development. Increased air humidity also contributes to the pathogenicity of the fungus, as evidenced by the high prevalence of lichen versicolor among the population of tropical and subtropical countries. Thus, the incidence rate in temperate climates is 2%, in tropical and subtropical climates - up to 40% of cases [6, 16, 19, 24, 26].
Being a yeast-like fungus, P. orbiculare has many of the qualities inherent in this group of fungi. In particular, the disease develops when a saprophytic form is transformed into a pathogenic one under special, favorable circumstances. The development of the disease is promoted by: increased sweating, seborrhea, decreased physiological peeling of the skin, decreased nutrition, and pathology of internal organs. Lichen versicolor is a unique marker of diabetes mellitus, tuberculosis, rheumatism, and AIDS. In these diseases it is found in 52–63% of patients. If pityriasis versicolor develops against the background of tuberculosis, lymphogranulomatosis and other diseases accompanied by sweating, there are no age restrictions and clinical signs of this dermatosis can be observed at any age [6]. The literature describes a case of lichen versicolor diagnosed in a three-month-old child with leukemia [23].
In recent decades, hematogenous infections caused by M. furfur have been observed; they have been described in weakened and immunosuppressed patients, especially after organ transplantation, as well as in neonatal children receiving lipids through a central venous catheter [1, 11, 13, 24].
The presence of cross-reacting antigens in P. orbiculare with fungi of the genus Candida provokes the development of allergic reactions of immediate, immunocomplex and delayed types. Studies conducted by various authors have proven that one of the main risk factors for the formation of complicated forms of atopic dermatitis at an early age in children is the predominance of fungi of the genus Malassezia. The addition of an associated fungal infection changes the clinical picture of atopic dermatitis, which is characterized by a more severe course, widespread process and resistance to traditional therapy [10, 16, 27]. According to the observations of Mayser P. et al. (2000) in patients with P. orbiculare colonization on the scalp and neck, specific IgE antibodies were more often recorded than in patients with localization on the skin of the trunk. In addition, the author found that patients with Malassezia more often complained of diffuse hair thinning.
There is evidence to support the role of P. orbiculare in the development of seborrheic dermatitis. As a result of their vital activity, these fungi break down sebum triglycerides into free fatty acids, and these, in turn, are the direct cause of dermatitis on the surface of the skin, but this assumption still requires proof [8]. In particular, an experimental model of seborrheic dermatitis was obtained by rubbing a P. orbiculare culture into the skin of subjects. Subsequently, regression of experimental dermatitis was noted under the influence of various antimycotic drugs, which confirmed the etiological role of P. orbiculare in seborrheic dermatitis. Moreover, if normally the microflora of the scalp contains 46% of this fungus, then with dandruff it consists of 74% of them, and with seborrheic dermatitis the number of fungi reaches 83% [6, 28].
It must be remembered that seborrheic dermatitis associated with P. orbiculare (ovale) may be the single earliest manifestation of AIDS. According to foreign authors, from 30% to 80% of patients with HIV infection have seborrheic dermatitis, compared to healthy young people in whom this dermatosis was diagnosed only in 3–5% of cases. AIDS-associated seborrheic dermatitis is characterized by resistance to therapy and papular rashes resembling psoriasis [1, 8, 9, 13].
Clinical picture of the disease. The onset of the disease is characterized by the appearance of yellowish dots confined to the mouth of the hair follicles. The primary morphological element is a pink-yellow spot, gradually changing to brown-yellow, on the surface of which there are pityriasis scales. The elements are characterized by peripheral growth and, subsequently, fusion into larger lesions with scalloped edges. With a long course of mycosis, the lesions can occupy large areas of the skin. Over time, the color of the lesions can vary from white to dark brown, this served as the basis for the second name for lichen - multi-colored. The surface of the rash is covered with pityriasis-like scales, which are hardly noticeable upon superficial examination, but when scratched, peeling easily occurs (Beignet's symptom). Since the favorite localization is confined to the “seborrheic zones,” the upper half of the body and the scalp are affected. Additional diagnostic criteria, well known to doctors, are the Balzer iodine test and a golden-yellow or brownish glow under a Wood’s lamp, as well as detection of the pathogen during microscopic and cultural studies [1, 2, 5, 6, 9].
A feature of the clinical picture of pityriasis versicolor is the presence of pseudoleukoderma. Scientists have divided opinions about the causes of uneven skin coloring in this dermatosis. Some researchers believe that P. orbiculare (ovale) inhibits tyrosinase activity during the oxidation process, which leads to a decrease in melanin synthesis and is clinically manifested by the occurrence of true leukoderma [6]. According to other authors, the loosened stratum corneum on the lesions prevents the penetration of ultraviolet rays into the depths of the epidermis. Therefore, after removal of scales during water procedures, the affected lesions become lighter than the surrounding healthy skin [2, 9].
As a rule, diagnosis is not difficult, but there are several points that the practitioner needs to pay attention to. Firstly, in individuals who received treatment and were irradiated with ultraviolet rays, the Balzer test will be negative. Secondly, identifying affected areas on the scalp is of practical importance: if the doctor does not pay attention to this localization of keratomycosis, then there is a high probability of relapse. To diagnose lesions on the scalp, a Wood's lamp is used (the lesions have a greenish-yellow, yellowish-brown or brownish glow). Thirdly, pinkish-brown spots are barely noticeable on white skin, so they are often ignored when examined, but in the summer, if you have a tan, they become more noticeable. And the last nuance: in people without immune deficiency, isolated spots do not exceed, as is known, 1–1.5 cm in diameter, but with severe immunodeficiency they can reach 5 cm in diameter. In this case, not only a disseminated character is noted, but also rich pigmentation and infiltration of elements of multi-colored lichen. In patients with AIDS, lichen versicolor more often manifests itself as seborrheic dermatitis, less often as atopic dermatitis and multiple folliculitis in areas of the skin with symptoms of vasculitis and a necrotic component.
The atypical course of lichen versicolor was described by various authors [11, 14]. The rarest manifestations of lichen versicolor include lesions on the skin of the soles. In the domestic literature, such localization is reported by V. M. Rukovishnikova (1999), who in her monograph refers to the observations of V. P. Zhirkova (1977) of a 16-year-old boy with hyperhidrosis, who, along with rashes of multi-colored lichen in typical places (chest , back, neck, face) there were foci of mycosis on the soles. A pronounced torpidity of the lesions of this unusual localization was noted. Even after four months of treatment, non-inflammatory brownish spots of irregular shape and outline remained on the heels and in the transitional fold from the toes to the sole.
Differential diagnosis of pityriasis versicolor is carried out with syphilis (with syphilitic roseola and leucoderma). The diagnosis of syphilis is confirmed by positive results of classical serological tests (CSR), Treponema pallidum immobilization test (TPI), and immunofluorescence test (RIF). In addition, roseola in secondary syphilis has a pinkish-livid tint, disappears with diascopy, does not peel off, does not fluoresce in the light of a fluorescent lamp, and the Balzer test is negative.
In syphilitic leukoderma there are no confluent hyperpigmented spots and micropolycyclic edges. Syphilitic roseola is characterized by a predominant localization on the trunk and upper extremities, which determines some similarity in the clinical picture, however, with syphilitic lesions there is no tendency to growth and fusion of elements. The roseola spot is of vascular origin, there is no peeling, it is not accompanied by subjective sensations, the Balzer test is negative.
Lichen versicolor should be distinguished from pink lichen of Zhiber, in which erythematous spots are acutely inflammatory, round or oval in shape, with a peculiar peeling in, there is a “maternal” plaque. The rashes are located symmetrically along Langer's lines. The edges of the central, flaky part of the plaque are surrounded by a collar of scales. Numerous secondary rashes are visible around the maternal plaque.
Pityrosporum folliculitis (Malassezia folliculitis) is an infection of the hair follicle caused by yeasts, the same ones that cause pityriasis versicolor. This disease is a separately located, sometimes itchy papulosquamous rash, localized mainly on the upper half of the body and shoulders. Pityrosporum folliculitis most often affects young and middle-aged people and women. Follicular occlusion appears initially, which is secondarily accompanied by increased growth of the fungus. Predisposing factors are diabetes mellitus, as well as taking broad-spectrum antibiotics or corticosteroids. The condition can appear on the forehead and mimic persistent acne. The clinical picture consists of asymptomatic or slightly pruritic dome-shaped follicular papules and pustules with a diameter of 2–4 mm. This dermatosis is more common in the tropics, where it manifests itself as follicular papules, pustules, nodules and cysts. A distinctive feature of Pityrosporum folliculitis is the absence of comedones, torpidity to therapy and localization in the forehead. According to Thomas P. Habiff (2006), very often patients with Pityrosporum folliculitis are mistaken for acne patients. According to the author, this disease should be suspected in young and middle-aged patients with follicular lesions located on the trunk and complaints of itching.
Treatment. Since this disease develops when the saprophytic form of the fungus is transformed into a pathogenic one under special, favorable circumstances, it is necessary, first of all, to identify the provoking factors. Lichen versicolor is a marker of diabetes mellitus, tuberculosis, rheumatism, and AIDS. Therefore, when examining a patient, it is necessary to conduct appropriate studies. Particular attention should be paid to persons who do not fall into the age category from 15 to 45 years. Often the development of a persistent clinical picture of pityriasis versicolor is caused by chemotherapy in cancer patients. As a rule, after completing the course of intensive treatment, such patients undergo spontaneous self-healing.
As mentioned above, pityriasis versicolor is characterized by damage to the surface layer of the epidermis - the stratum corneum. Therefore, treatment of keratomycosis should begin with external means. Medicines for the treatment of pityriasis versicolor can be divided into several groups:
- keratolytic agents;
- fungicidal preparations;
- products containing zinc pyrithioneate;
- combined means.
Therapy for lichen versicolor depends on the prevalence and location of the lesions. Previously, keratolytic agents were used in the treatment of this mycosis: 2–5% salicylic alcohol or an alcohol solution of resorcinol 2 times a day. Modern methods of therapy include fungicidal drugs from the azole group. It has been established that under the influence of antimycotic drugs, after 24 hours, dehydration and vacuolization of the cytoplasm in the fungal cell occurs, the cell wall clears, from which after 48 hours only a shadow remains. Therefore, specific antifungal treatment is often preferred over keratolytic drugs.
Considering the superficiality of skin lesions with keratomycosis, it is preferable to use fungicidal agents in the form of solutions (clotrimazole, bifonazole, ciclopirox, naftifine (Exoderil), terbinafine (Lamisil)) or econazole in powder form, sold under the trade name "Ifenek", which is applied to the affected areas of the skin and rub lightly. A more convenient form of using the drug is a spray (Lamisil, Thermikon). All antimycotic solutions for the treatment of pityriasis versicolor are prescribed 2 times a day for 1 week. Ketoconazole has higher activity against P. ovale, inhibiting its growth in concentrations 25–30 times lower than other antifungal drugs and several times lower than any systemic antimycotics. When topical forms of ketoconazole are applied to the skin, effective concentrations remain inside and on the surface of the epidermis for 72 hours after discontinuation of the drug, which is explained by the affinity of the drug for keratinized tissues.
Zinc pyrithione also has a direct antifungal effect. Today, the mechanism of therapeutic effects of zinc pyrithione is associated not only with cytostatic, but also with antifungal and antimicrobial effects. The effectiveness of drugs containing zinc pyrithione against yeast-like fungi has been studied by many authors [1, 3, 4]. These drugs include Psorilom and Skin-cap, produced in two forms: spray and cream. In the future, these drugs can be used by patients as prophylactic agents at least once every 2 weeks. While inferior to ketoconazole, zinc pyrithione has superior antifungal activity to other drugs, including selenium sulfide and some imidazoles. In the last decade, zinc-based shampoos (Head and shoulders, Friederm zinc) have been widely used in the treatment of dandruff. Thus, the most effective drugs in the treatment of pityriasis versicolor are antifungal agents and zinc pyrithione.
When the scalp is affected by fungus, medicated shampoos containing fungicidal agents (Nizoral, Sebazol, Ducre Quelual DS, Ketoconazole) are used, which are prescribed daily with an exposure of 2–5 minutes for 7–10 days. Treatment with shampoos containing tar (Psoril) is effective in the presence of seborrheic dermatitis to eliminate such manifestations as infiltration, swelling, peeling, and erythema.
Combined preparations include shampoos: Node DS plus, which contains salicylic acid, climbazole, zinc pyrithione, and Keto plus based on ketoconazole and zinc pyrithione.
Systemic treatment is indicated for patients with advanced disease who do not respond to topical therapy or who experience frequent relapses. Intraconazole is prescribed at a dose of 200 mg 2 times a day for one day or 200 mg every day for 5 days. The drug is taken with food to improve absorption. Ketoconazole is taken in a dose of 400 mg once or 200 mg daily for 5 days at breakfast with fruit juice. Fluconazole is prescribed at a dose of 150 mg (2 capsules per week for 4 weeks or 2 capsules as an initial dose, repeated after 2 weeks). If the process resolves slowly, the course of systemic antimycotics can be repeated after 2 weeks. The patient is not recommended to take a bath for 12 hours after treatment, since abstaining from water procedures allows the medicine to accumulate in the skin. Some authors recommend changing clothes daily for one month to prevent relapses. Patients must accept that residual hypopigmentation, as a consequence of pseudoleukoderma, lasts for quite a long time.
In the treatment of Pityrosporum folliculitis, one should adhere to the same principles as in the treatment of pityriasis versicolor, but it is preferable to combine systemic ketoconazole (200 mg daily for 4 weeks) with external antifungal agents.
Literature
- Skin Diseases: Diagnosis and Treatment / Thomas P. Habiff; lane from English; Under general ed. acad. RAMS, Prof. A. A. Kubanova. M.: MEDpress-inform, 2006. 672 p.
- Skin and sexually transmitted diseases: Handbook / Ed. O. L. Ivanova. M.: Medicine, 1997. 352 p.
- Mokronosova M.A., Pyzh V.V., Kashaeva O.V., Reznikov O.V. Therapeutic effect of activated zinc pyrithione in patients with atopic dermatitis / eczema syndrome with sensitization to yeast-like fungi // Russian Journal of Allergology. 2004, no. 3. pp. 83–87.
- Moshkalova I. A., Mikheev G. N., Sokolovsky E. V. et al. Blistering dermatoses. Psoriasis. Modern methods of treatment. St. Petersburg: Sotis, 1999. 133 p.
- Novikov A.I., Loginova E.A. Skin diseases of infectious and parasitic origin. M.: Medical book, N. Novgorod: Publishing house of the NGMA, 2001. 283 p.
- Potekaev N. N., Novikov A. G. Multi-colored lichen. A modern look at an old problem // Russian Journal of Skin and Venereal Diseases. 2004, no. 2. pp. 42–45.
- Rukovishnikova V. M. Mycoses of the feet. M.: MSD, 1999. 317 p.
- Sukolin G.I. Seborrheic dermatitis: new in etiology and treatment // Russian Medical Journal. 1998; 6:382–384.
- Khabib O. N. Mycoses of smooth skin // Consilium Medicum, 2002, volume 2, no. 4.
- Khaertdinova L. A. Medical and social aspects of atopic dermatitis in children complicated by secondary infection. Author's abstract. dis. ...cand. honey. Sci. 2006. 22 p.
- Aljabre SH Intertriginous lesions in pityriasis versicolor // J Eur Acad Dermatol Venereol 2003? 17(b): 659–662.
- Crespo-Erchiga V., Florencio VD Malassezia yeasts and pityriasis versicolor // Curr Opion Infect Dis. 2006; 19 (2): 139–147.
- Christian Schnake S., Hector Gutierrez B., Marcos Saez G., Mario Becker C. Tinea versicolor. Pitiriasis versicolor en lactantes menores Rev // Chil. Pediatr. 1988, 59 (1); 50–52.
- Darling M. J, Lambiase M. C, Young RJ Tinea versicolor mimicking pityriasis rubra pilaris // Gutis. 2005; 75(5):265–267.
- Gemmer CM, DeAngelis YM, Theelen B., Boekhout T., Dawson Jr. TL Differentiation of three biotypes of Malassezia species on human normal skin. correspondence with M. globosa, M. sympodialis and M. restricta // Mycopathologia. 1999; 145(2):69–74.
- Hort W., Nilles M., Mayser P., Edward M., DeSimone R. Ph. Common Superficial Fungal Infections // US Pharmacist. 1999, 24 (4).
- Mayser P., Gross A. IgE antibodies to Malassezia furfur, M. sympodialis and Pityrosporum orbiculare in patients with atopic dermatitis, seborrheic eczema or pityriasis versicolor, and identification of respective allergens // Acta Derm Venereol. 2000; 80(5):357–361.
- Naseri M., Namazi MR Fast, noninvasive method for molecular detection and differentiation of Malassezia yeast species on human skin and application of the method to dandruff microbiology // J Clin Microbiol. 2002; 40(9):3350–3357.
- Nematian J., Ravaghi M., Gholamrezanezhad A., Nematian E. Isolated scalp involvement with pityriasis versicolor alba (pityrias versicolor albus capitis) in a patient from a dry, temperate region // Dermatol Online J. 2003; 9 (3): 17.
- Nenoff P., Haustein UF Effect of anti-seborrhea substances against Pityrosporum ovale in vitro // Hautarzt, 1994, v. 45 (7), p. 464–467.
- Ogunbiyi AO, George AO Pityriasis versicolor: Current concepts in Aetiology and Management // Niger Postgrad Med J. 2005; 12 (3): 183–188.
- Parry ME, Sharpe GR Seborrhoeic dermatitis is not caused by an altered immune response to Malassezia yeast // Br. J. Dermatol. 1998; 139:254–263.
- Schoepfer C., Carla H., Bezou MJ // Arch. Pediatr. 1995. Vol. 2, No. 3. P. 245–248.
- Silverberg NB, Sidbury R., Mancini AJ Childhood molluscum contagiosum: experience with cantharidin therapy in 300 patients // J Am Acad Dermatol. 2000; 43:503–507.
- Shuster S. The aetology of dandruff and the mode of action of therapeutic agents // Br. J. Dermatol. 1984; 111:235–242.
- Tarazooie B., Kordbacheh P., Zaini F., Zomorodian K., Saadat F., Zeraati H., Hallaji Z., Rezaie S. Study of the distribution of Malassezia species in patients with pityriasis versicolor and healthy individuals in Tehran, Iran // BMC Dermatol. 2004; 4:5.
- Thoma W., Kramer HJ, Mayser P. Pityriasis versicolor alba // J Eur Acad Dermatol Venereol. 2005; 19 (2): 147–152.
- Wikler JR, Nieboer C., Willemze R. Quantitative skin cultures of Pityrosporum yeasts in patients seropositive for the human immunodeficiency virus with and without seborrhoeic dermatitis // J. Am. Acad. Dermatol. 1992; 27:37–39.
Yu. A. Gallyamova, Doctor of Medical Sciences, Associate Professor
GOU DPO RMAPO, Moscow
Contact information for authors for correspondence
Prevention of pityriasis rosea
Simple preventive measures can prevent the development of the disease. To protect your body from pityriasis rosea, you need:
- Observe the rules of personal hygiene;
- Avoid synthetic and woolen clothing;
- Carefully select cosmetics, paying attention to their composition, quality, expiration dates;
- Adjust your diet so that your diet contains all the necessary substances;
- Avoid products with artificial colors and additives;
- Forget about bad habits;
- Temper yourself;
- Take vitamins as prescribed by your doctor.
It is advisable not to indulge in strong tea and coffee, fatty and fried foods. At the first manifestations of pityriasis rosea, you need to protect the areas of skin with rashes from direct sunlight and consult a doctor.
Contraindications
Patients with pityriasis rosea, depending on the degree of the disease, may be contraindicated for prolonged water procedures - hot baths, showers. This is due to the fact that the spots are predisposed to swelling, and water can provoke swelling. If water is regularly exposed, damaged tissue may respond poorly to treatment.
However, it is impossible to completely abandon the treatment of inflammation - bacterial microflora will cause a deterioration in the condition of damaged tissues. In this case, a quick rinse in cool or slightly warm water is recommended.
The patient must avoid skin irritation so as not to provoke an exacerbation of the disease. Irritants include:
- rough linen, wool or synthetic clothing;
- ultraviolet irradiation;
- cosmetic and medicinal preparations with tar and sulfur;
- hypothermia.
The disease can be complicated if the diet contains:
- citrus;
- smoked meats;
- dairy products;
- marinade, hot seasonings and sauces;
- fish, seafood;
- carbonated drinks;
- dried fruits.
Only a doctor can give precise nutritional recommendations.
If you notice symptoms of pityriasis rosea, immediately consult a dermatovenerologist.
Other articles by the author
- Pyoderma
- Herpes zoster
- Pityriasis rosea
- Shingles
Diagnosis of pityriasis rosea
Diagnosis of the disease is not difficult, since the manifestations of the pathology are quite typical. But the doctor must make sure that the rash is caused by pityriasis rosea, and not by eczema, syphilis, psoriasis or fungal infection of the skin - mycosis.
In addition, the disease can occur in an atypical form, so special studies and tests are carried out to confirm the diagnosis.
| Appointment with a dermatologist at the clinic. Call a dermatologist at home. | Reception is strictly by appointment, make an appointment by phone: +7 | Prices for services | Reviews about the clinic |
Diagnosis of the disease
Determining the correct diagnosis is sometimes difficult due to the absence of a pathogen. The disease can be confused with other lichen and toxicoderma.
The examination is a visual inspection. A qualified dermatovenerologist will take into account the characteristic placement of spots on the body, their appearance, shape, and based on this will make a diagnosis.
Tests that may also be prescribed:
- general urine and blood tests;
- microprecipitation reaction (diagnosis of syphilis);
- scraping from affected areas.
After diagnosis, the specialist will determine how to treat pityriasis rosea and will advise the patient in detail regarding lifestyle.
Make an appointment
Treatment methods for pityriasis rosea
In the typical course of the disease, treatment may not be required, but only a doctor can make such conclusions based on the examination results. In such situations, the patient is recommended to:
- Hypoallergenic diet;
- Limiting water treatments (shower instead of bath), using a soft washcloth;
- Wearing clothes made from natural fabrics;
- Avoiding activities that cause excessive sweating.
In case of protracted course of pityriasis rosea, antiviral medications, treatment of rashes with salicylic alcohol, and topical antibacterial agents - ointments, can be prescribed. Antihistamine medications are used to reduce itching and can also prevent the spread of rashes. In some cases, treatment with antibiotics is required.
Clinical picture
Most patients do not have severe symptoms of the disease; in some cases they complain of mild or severe itching. The problem occurs in emotional people or patients with skin allergies that react inadequately to external stimuli.
The first sign of pathology is the formation of a “mother spot” - a large pink area of dermis with pronounced peeling. After the scales are torn off, the spot acquires a brown tint and clear boundaries. It does not exceed 2-5 cm in diameter. Initially, a single focus of pityriasis rosea is registered, later several additional ones appear on the body.
Secondary spotting forms a few days after the appearance of the mother spot. Changes are recorded on the arms and legs, back, and abdomen. Secondary rashes have a similar shape, with a reddish or pinkish tint. They rarely occur in the neck or face. The appearance of the first spots requires immediate consultation with a doctor and treatment prescribed by a specialist.
Ointments used for pityriasis rosea
For severe, disturbing itching, anti-inflammatory and antiallergic creams and formulations are prescribed. Ointments are used to treat the disease:
- Hydrocortisone – has an anti-inflammatory effect, relieves itching;
- Olettrinovaya is an antibacterial drug;
- Prednisolone - a composition with healing properties that can relieve inflammation;
- Loriden A - ointment with antipruritic, anti-parotid, anti-edematous effects;
- Sinalar – eliminates inflammation due to antibacterial properties;
- Lassara paste is an antiseptic that discolors stains;
- Rioloxol - antibacterial and anti-inflammatory;
- Flucinar – effectively relieves itching, eliminates flaking and inflammation;
- Sulfur – inhibits the inflammatory process.
Tsindol suspension also helps dry the skin, eliminate inflammation and itching. Ointments are applied to the pink plaques in a thin layer in accordance with the instructions and directions of the doctor. The treatment course is 2-3 weeks, the frequency of use of each drug is determined individually. At the same time as using medications, you should be careful with the affected skin.
However, any ointments, like all other medications, should be used exclusively as prescribed by a doctor, so as not to aggravate the situation. In addition, the effectiveness of each of the listed external remedies greatly depends on the patient’s age, the state of his immunity, the degree of spread of lichen, the presence of chronic pathologies and other characteristics of the body.
Calling a dermatologist to your home for pityriasis rosea
When the first signs of pityriasis rosea appear, you should consult a doctor. Today there is a convenient service for calling a doctor to your home, which provides many advantages:
- Saving time - no need to go to a medical facility or wait for your turn at the office door. You can simply arrange a doctor’s visit at a time convenient for you;
- Comfort – communicating with a doctor at home is much easier, because the doctor is not distracted by other patients and clinic staff, he can spend as much time as necessary on examination and consultation;
- Calmness – for children of all ages, a visit to a medical facility is often stressful, which plays a negative role in the development of many diseases, including pityriasis rosea. A doctor’s home visit will save the child from unnecessary worries;
- No risk – the development of pityriasis rosea often occurs against the background of weakened immunity. In such circumstances, contact with other patients is undesirable, but it is almost impossible to avoid it in the corridors of the clinic, as well as in public transport on the way to the medical facility. At home, such a risk is eliminated;
- If the disease is accompanied by fever, calling a doctor at home will be the best solution;
- Examination at home is the most convenient option for older people, mothers with small children, and patients with disabilities.
The quality of medical care at home is no different from that provided in a medical facility. The doctor gives the necessary recommendations, provides full consultation, diagnoses the disease and prescribes adequate treatment.
Common symptoms and manipulations in dermatology:
- Skin rashes
- Calling a dermatologist to your home
- Itching in the urethra
- Itchy skin
- Skin rash
- Prevention of casual sex
- Skin neoplasms
- Pyoderma
- Pityriasis rosea
- Streptoderma
- Scabies
- Peeling skin
- Fungal infections
- Skin infection
- Pus on the skin
- Blisters on the skin
- Papillomas on the foreskin
- Sexually transmitted diseases
- Skin structure
Where to go with pityriasis rosea
Diagnosis and treatment of pityriasis rosea is carried out by a dermatologist. There are at least two important reasons to see a doctor rather than self-medicate. The first is the need to define the disease. Often, pityriasis rosea has some similarities with other skin pathologies such as fungal infections, psoriasis, mycosis of smooth skin or syphilis.
The second reason is to prevent complications. Despite the fact that the disease usually goes away on its own, sometimes lack of treatment or incorrect selection of drugs creates a serious risk of complications. They consist in the spread of rashes, the appearance of prolonged severe itching, and skin pigmentation after recovery.
With a strong decrease in immunity, a complicated course of the disease with an increase in temperature is possible. In people with blood pathologies or cancer who have undergone chemotherapy, the disease can develop again. The use of folk recipes and all kinds of folk remedies can cause contact dermatitis and even chemical burns. When using dyes, for example, celandine, diagnosing the disease is difficult, and a bacterial infection enters the body.
An acute inflammatory skin disease, which manifests itself as characteristic multiple round maculopapular (plaque-like) and maculopapular elements with a “maternal” largest plaque, the causes of which are currently not fully understood. Pityriasis rosea has many synonyms - Gibert's disease, roseola exfoliating, and many others, but the disease has no connection with fungal etiology (which is usually thought of when they hear the name “lichen”). This name is associated to a greater extent with the external manifestations of the disease. The disease is not prone to recurrence, usually goes away on its own and does not lead to the development of complications. In some cases, a severe course is possible with the spread of plaques throughout the body, pronounced inflammatory changes (swelling, addition of “eczematous” changes), the appearance of itching and general allergic symptoms.
The development of the disease is usually associated with a previous infection of viral etiology (suggestions have also been made about streptococcal etiology, when the disease developed after bacterial tonsillitis). Currently, the role of a certain type of herpes virus (6th and 7th) is especially emphasized. There is still no proven cause of the disease. The infectious-allergic mechanism of development of Zhiber's disease allows us to say that the disease is subject to seasonal fluctuations (like infectious ones); most patients experience symptoms of general intoxication preceding skin manifestations - headaches, joint pain, enlarged lymph nodes, rise in temperature). The acute course of the disease with spontaneous recovery, rare relapses are also signs of the presence of a certain factor (microbial), to which immunity develops. The peak incidence occurs at the age of 20-30 years, and pityriasis rosea practically does not occur in elderly people and children.
The clinical picture of the disease is quite specific, but sometimes blurred and atypical forms occur. Features of skin manifestations during the development of pityriasis rosea include: the appearance of a “maternal” plaque - a bright, round spot (which can rise slightly above the skin level) of large size - on average 3-5 cm, which is usually localized on the body and is accompanied by slight peeling in the central parts; the appearance, after a few days or weeks, of multiple daughter elements that are smaller in size compared to the “mother” and are represented by swollen, scaly spots. The spots may appear over time, so they may differ in appearance (polymorphism of lesions). The central sections of the spots may have a characteristic appearance of delicate folded skin, slightly darker than the surrounding sections. The lateral sections have a “fringed” appearance due to peeling. Gradually, the elements of the rash begin to peel off from the central part to the side and turn pale. Gradually, the rash disappears and leaves an area of reduced pigmentation (a pale spot remains at the site of the former rash). Itching is not considered a characteristic manifestation of pityriasis rosea, but in some cases it can occur (for example, with frequent irritation of the rash sites). The rashes are usually located on the stomach, back, neck, and are almost never found on the limbs. Atypical forms may include several large “mother” plaques or the appearance of vesicles or compacted plaques. From the moment the first element appears until the last one disappears, about 1 - 1.5 months pass.
Diagnosis and treatment of pityriasis rosea is carried out by a dermatovenerologist. Differential diagnosis is carried out with eczema, psoriasis, syphilis, mycoses (fungal skin lesions).
Diagnosis does not present any particular difficulties in the case of the classic course of the disease. A previous infection or hypothermia, the appearance of a “maternal” plaque and daughter elements on the body in the projection of Langer’s lines are sufficient to suggest a diagnosis of Gibert’s disease. Microscopic examination of scrapings from the lesion site is also used to exclude fungal etiology. Additionally, a general blood and urine test is prescribed, as well as a study of antibodies to certain viral agents and Treponema pallidum (excluding syphilis).
The prognosis is favorable in all cases.
What tests need to be taken for pityriasis rosea?
The diagnostic method and set of necessary studies are determined by a dermatologist. Typically, the patient takes a blood test to study general indicators. Tests are often ordered to detect antibodies to viral agents, including syphilis and herpes. To exclude fungal damage to the skin, microscopic examination of scrapings from the site of the lesion is carried out.
Additionally, the doctor may prescribe an immunogram if there is a suspicion of a significant decrease in the body's defenses. The cause of pityriasis rosea is an allergic reaction, so testing for allergens is possible. If necessary, the doctor prescribes additional examinations and consultations with specialists. Typically, such measures are taken in case of protracted or atypical course of the pathology.